Proliferation Response of Leukemic Cells to CD70
advertisement
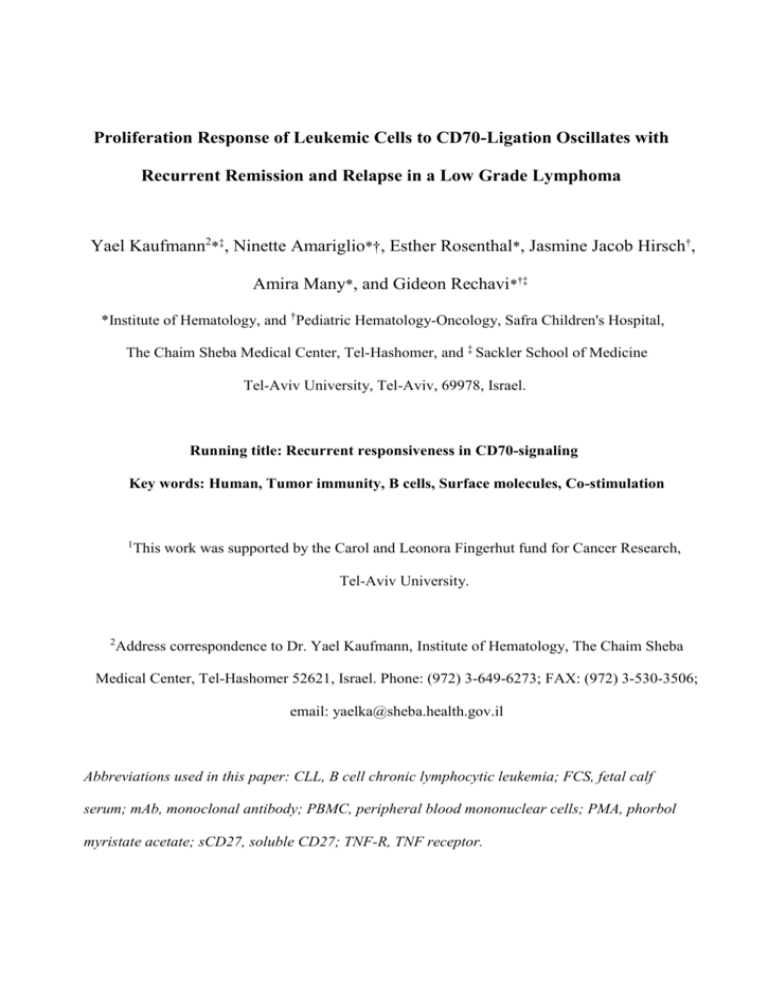
Proliferation Response of Leukemic Cells to CD70-Ligation Oscillates with Recurrent Remission and Relapse in a Low Grade Lymphoma Yael Kaufmann2*‡, Ninette Amariglio*†, Esther Rosenthal*, Jasmine Jacob Hirsch†, Amira Many*, and Gideon Rechavi*†‡ *Institute of Hematology, and †Pediatric Hematology-Oncology, Safra Children's Hospital, The Chaim Sheba Medical Center, Tel-Hashomer, and ‡ Sackler School of Medicine Tel-Aviv University, Tel-Aviv, 69978, Israel. Running title: Recurrent responsiveness in CD70-signaling Key words: Human, Tumor immunity, B cells, Surface molecules, Co-stimulation 1 This work was supported by the Carol and Leonora Fingerhut fund for Cancer Research, Tel-Aviv University. 2 Address correspondence to Dr. Yael Kaufmann, Institute of Hematology, The Chaim Sheba Medical Center, Tel-Hashomer 52621, Israel. Phone: (972) 3-649-6273; FAX: (972) 3-530-3506; email: yaelka@sheba.health.gov.il Abbreviations used in this paper: CLL, B cell chronic lymphocytic leukemia; FCS, fetal calf serum; mAb, monoclonal antibody; PBMC, peripheral blood mononuclear cells; PMA, phorbol myristate acetate; sCD27, soluble CD27; TNF-R, TNF receptor. Abstract Interactions of the tumor necrosis factor-related cell surface ligand CD70 with its receptor CD27 provide a co-stimulatory signal in B- and T- cell activation. Functional CD70-CD27 interactions could contribute to lymphoma and leukemia progression. This possibility was studied using DNA microarrays on a unique case of low-grade lymphoma/leukemia characterized by recurrent cycles of acute leukemic phase alternating with spontaneous remission. Upon induction of the acute phase expression of CD70 and CD27 in the leukemic cells increased 38 and 25 fold, respectively. Co-expression of membrane CD70 and CD27 on the leukemic (CD5+CD19+) cells was maximal 2-3 days following initiation of the attack. Soluble CD27 in the patient's serum was elevated during remission and further increased in the attack. Functional tests showed that neither anti-CD70 nor anti-CD27 antibodies affect the rate of apoptosis. However, the anti-CD70 antibody specifically enhanced proliferation of the remission phase leukemic cells whereas proliferation of the acute-phase counterparts that express higher level of membrane CD70 was unaffected. Hence, in this lymphoma/leukemia, membrane CD70 is presented on the leukemic cells in a responsive state during the remission and a non-responsive state during the attack. Presumably, CD70 in its responsive state provides a co-stimulatory receptor for initiating the next acute phase while its non-responsive state enables the remission. 2 Introduction CD27 and its ligand CD70 are members of the tumor necrosis factor-receptor (TNF-R) family and TNF superfamily, respectively. Interactions between TNF-R family members and their ligands control lymphocyte death, survival, proliferation and differentiation (1, 2). Tightly regulated expression of CD70 and CD27 on normal lymphocytes ensures the transient availability of these co-stimulatory signals. CD70 is transiently induced upon activation of B cells (3) and T cells (4). CD27 is absent from immature and mature B cells but is found on memory B cells (5, 6) T cells (7) and NK cells (8). Differentiation to effector T cells is associated to loss of CD27 (9). Cell surface CD27 can be proteolytically cleaved to produce a 32-kDa soluble CD27 (sCD27) molecule, which can be detected in the serum and urine (10). Elevated serum sCD27 levels are seen in a number of infectious and autoimmune disease states and are believed to be a marker of T cell activation. Also, various types of B cell malignancies express the CD27 molecule and elevated serum levels of sCD27. There appeared to be a correlation between tumor load and sCD27 levels (11). Studies on the biological role of this receptor-ligand pair have mainly addressed the ability of CD27 to regulate the immune response. CD27 signaling appears to play a co-stimulatory role promoting T cell expansion and differentiation (7, 12-15) as well as enhancement of NK cell activity (16). CD70 has been generally envisaged as a passive element merely required for specific CD27 engagement. Yet, reverse signaling of CD70 was reported. Thus, anti-CD70 monoclonal antibodies (mAb) were observed to induce proliferation in a subset of B cell chronic lymphocytic leukemia (CLL) (17) and stimulate NK and T cell-mediated redirected killing (18), suggesting that CD70 might be a signaling molecule. Recently Arens et al showed that CD70 has reverse signaling properties in murine B cells, initiating a signaling cascade that regulates expansion and differentiation (19). In contrast to the tightly regulated expression of CD70 on normal cells, constitutive expression of CD70 is found on several human leukemias and lymphomas (17, 20, 21). The finding that cross-linking of CD70 on malignant B cells augments proliferation (17) raised the possibility that CD70 might contribute to progression of these B-cell malignancies. We have previously reported a case of CD5-positive B cell lymphoma, diagnosed as atypical CLL/SLL, which is characterized by recurrent acute waves of active disease (22, 23). The patient experienced within 8 years 27 cycles of leukemic waves followed by spontaneous 3 partial remissions. The first week of the wave characterized by fever, generalized lymphadenopathy and increasing number of clonal IgM-positive leukemic cells usually above 60.000 cells/mm3. After a few days the symptoms of the acute illness disappeared. Following 2-3 weeks most of the transformed leukemic cells disappeared and the white blood cell count returned to almost a normal level. Nonetheless, 10-60% of the peripheral lymphocytes were monoclonal B cells. The remission periods lasted 2-7 months (22). Transient bouts of serum TNF and IL-10 preceded the acute phases, which were characterized by co-existence of CD40-ligand+ T lymphocytes and lymphoma cells in the bone marrow (23). During remissions, residual IgM+ leukemic cells exhibited resting phenotype, low proliferative response to CD40-ligand and delayed apoptosis in culture. In contrast, the acute phase counterparts were phenotypically activated, underwent rapid apoptosis and proliferated extensively in response to membraneanchored CD40-ligand (23, 24). The existence of a clonal leukemic cell population throughout the course of the disease (22) provides a unique opportunity to characterize molecular changes in the neoplastic cells associated with recurrent activation and regression of the disease. Microarray analysis of the leukemic cells done in this study showed consistent pattern of gene expression characterizing different stages of the disease. Because interactions between CD70 and CD27 provide costimulatory signal in B cell activation we examined their involvement in progression of this "cyclic" lymphoma/leukemia. Indeed, CD70 and CD27 were among the genes whose expression transiently increased simultaneously with initiation of the acute phase. The leukemic cells from remission periods, but not those from acute phases, responded to CD70-ligation by increased proliferation response to PMA. The results are consistent with transition of cell surface CD70 from responsive to non-responsive state that occurs concomitantly with initiation of the attack and is coupled to activation and blast transformation of the leukemic cells. 4 Materials and Methods Isolation of leukemic cells and determination of sCD27 in the serum. Peripheral blood mononuclear cells (PBMC) were separated from heparinized blood by Ficol (Nycomed Pharma AS) density gradient centrifugation and stored in liquid nitrogen. Where indicated the patient's leukemic cells were purified from PBMC on CD19 magnetic beads (DynalR, Oslo, Norway) according to the manufacturer's instructions. The purified cells contained 94-98% CD19+CD5+ double positive leukemic cells. Viability of the leukemic cells, examined by trypan blue exclusion, was always above 92%. Sera were analyzed for sCD27 by sandwich ELISA (Sanquin Reagents, CLB, Amsterdam, Netherlands) according to the manufacturer's instructions. This study was approved by the Institutional Review Board, and informed consent was obtained. Microarray cDNA analysis. CDNA analyses were performed using Affymetrix Hu95A oligonucleotide arrays, as described at http://www.affymetrix.com/support/technical/datasheets/human_datasheet.pdf.(URL1). Total RNA was isolated from 1X107 CD19-purified leukemic cells by TrizolTM reagent (Life Technologies). Quality and amount of RNA was confirmed using an agarose gel. Biotinylated target RNA was prepared, with minor modifications from the manufacturer's recommendations. (http://www.affymetrix.com/support/technical/manual/expression_manual.affx)(URL2). When scaled to a target intensity of 100 (using Affymetrix MAS 5.0 array analysis software), scaling factors for all arrays were within acceptable limits. Details of quality control measures can be found at (http://eng.sheba.co.il/genomics)(URL3). Real-time quantitative polymerase chain reaction (RTQ-PCR) assay. RTQ-PCR assays were performed to determine the expression level of CD70 and CD27. Forward and reverse Primers (MWG-Biotech AG), were designed in different exons; CD70 forward primer 5'- TGGGTGGGACGTAGCTGAG-3' and reverse, 5'- TCCTGCTGAGGTCCTGTGTG- 3'. CD27 forward primer 5’-GCCAGGAACATTCCTCGTGA-3’ 5 and reverse, 5’- TTACAGTGCCGACAGCTCTCA-3’. Thymosinbeta was used as an internal standard. The RTQ-PCR reactions were done using Applied Biosystems 7900HT prism realtime PCR instrument, in a total volume of 20l containing 500nM of each forward and reverse primer, QuanTitect SYBR green PCR kit (Quiagen) for CD70 and CD27 assays, with cDNA equivalent to 25ng RNA of each sample. Appropriate negative controls were designed for each run. Ratio was calculated by dividing each gene expression with that of an internal standard. Flow cytometry. For comparison of cell-surface marker expression, cells that had been cryopreserved during different disease phases were thawed, processed, and analyzed simultaneously. 4105 PBMC were incubated in 0.4ml RPMI containing 10% fetal calf serum (FCS) (GIBCO) for 20 min. at 200C with CD19 PerCP, CD5 APC, CD27 R-PE and CD70 FITC, washed in PBS and analyzed on dual laser-FACScalibur-flow cytometer from Becton Dickinson, San Jose, CA. Discrimination of leukemic cells from the normal hematopoitic cells was done by gating on cells expressing CD19 and CD5. CD70 and CD27 expression on the leukemic cells was scored within the gated CD19+ CD5+ cells. The following monoclonal antibodies (mAbs) were used for 4 color FACS analysis; (R-PE)-labeled CD27 (clone M-T271) and (FITC)-labeled CD70 (clone Ki-24) Becton Dickenson (BD) Biosciences Pharmingen, (APC)-labeled CD5 (clone L17F12) and (perCP)-labeled CD19, BD Biosciences, San Jose, CA. Tests of apoptosis and cell proliferation. The patient's PBMC or CD19+ purified leukemic cells were cultured at 2106/ml in RPMI-1640 supplemented by L-glutamine, 10% FCS and gentamycin sulphate 50g/ml (CM medium), at 37oC in 5% CO2. Spontaneous apoptosis of the leukemic cells in culture was examined by Anexin-V-FITC staining. 4105 leukemic cells were cultured in 96-well flat-bottom plates in CM medium in presence or absence of 1-9g/ml azide-free preparation of anti-CD70 mAb. (clone Ki-24, BD Biosciences Pharmingen) or anti-CD27 mAb. (clone 1A4, Immunotech, Marseille, France). Apoptosis of the cultured leukemic cells was determined following 7 or 24 h incubation in CM medium at 37oC in 5% CO2. The cells were washed and resuspended in a buffer containing 10 mM HEPES (pH 7.4), 140 mM NaCl, and 2.5 mM CaCl2. Annexin-V6 FITC 1:50 (Roche, Mannheim, Germany) and Propidium Iodide 50g/ml (Sigma), were added and the cells were stained for 20 min. at 200C and immediately assessed on a Beckman Coulter Epics MCL flow cytometer. Proliferation of the leukemic cells was tested by 3H-thymidine uptake. 2105 cells were cultured in 96-well plates in CM medium in tetraplicates. To examine the effect of the antibodies on proliferation the leukemic cells were first allowed to bind the antibodies by preincubtion at 200C for 30 min. with 1-9g /ml azide-free CD70 mAb.(clone Ki24), or 1-9g/ml CD27 mAb (clone 1A4), followed by addition of 1ng/ml phorbol myristate acetate (PMA, Sigma, St.Louis). To examine the proliferative response of the leukemic cells to CD40L, purified leukemic cells were cultured with -irradiated CD40L-presenting L cell, as detailed previously (23). The cells were incubated at 37oC in 5% CO2 for 4 days. During the last 18 h of the culture 1Ci 3H-thymidine (20 Ci/mmol, PerkinElmer, Boston, MA) was added to measure proliferation. All apoptosis and proliferation assays were repeated three times. Online supplemental material. The results of the microarray analysis representing all probe sets (pivot for supp) and those representing the 216 probe sets which were upregulated upon initiation of the acute phase (216 subcluster gene list) will be accessible at http://eng.sheba.co.il/genomics. 7 Results Transcriptional profiling of the leukemic cells during remission and the acute phase. The recurrent leukemic attacks enabled us to search for changes occurring consistently in the leukemic cells during the spontaneous induction and regression of the acute phase. Thus, initiation of the attacks was indicated by high fever followed by a burst of blast-like lymphocytes in the blood peaking on the third day and decaying spontaneously within 2-3 weeks. During remission periods 10-60% of the mononuclear cells were the clonal IgM-k, CD5+ CD19+ leukemic cells (22). cDNA microarrays, representative of ~12,000 genes, were employed to compare transcriptional profiles of the leukemic cells during remission periods and on day 3, 5, 7 and 11 of the attack. The leukemic cells were purified by magnetic cell separation of CD19+ cells. Expression of hundreds of genes correlated with the phase of the leukemic cycle. Furthermore, each stage of the attack was characterized by a different expression profile (fig. 1A). Figure 1B depicts a cluster of 216 genes including CD70 and CD27, which were upregulated during transition from remission to the third day of the leukemic attack. This cluster of stimulated genes includes among others genes related to immune response (16), cell adhesion (14), response to external stimulus (21), signal transduction (30), cell-cell signaling (5), regulation of cell proliferation (5) and cell death (15). Table 1 indicates some selected genes whose expression was elevated during the leukemic attack. The first and second groups include genes implicated in cell activation, signal transduction and proliferation. Specific examples of these gene classes are (i) the CD80 antigen involved in the co-stimulatory signal essential for T cell activation and PBEF1 secreted by activated lymphocytes, (ii) galectin 1, affecting the MEK and PI3K signaling pathways, and MKP2 capable of controlling the MEK pathway, (iii) CD70 and CD137 ligand reported to promote reverse signaling in activated B cells and (iv) cyclin B1 and M-phase phosphprotein 1 required for control of the cell cycle. The third and fourth groups of genes whose expression increased during the attack include the growth inhibiting genes TGFRIII, CDK2AP1, and calgizzarin and the pro-apoptotic genes BIK, BAX, MCG10, PIG3, DNASE1L3 and caspase 9. It is interesting that elevated expression of both cell growth enhancers and inhibitors was evident at an early stage of the acute phase. Here we chose to focus on CD70 and CD27 and investigate their possible involvement in the induction and regression of the recurrent leukemic attacks. 8 Expression of CD70 and CD27 oscillates in correlation with the leukemic phase. The expression level of CD70 and CD27 in the purified leukemic cells was verified by RTQPCR analysis. In an attempt to obtain expression ratios that more reliably reflect the transition from remission to acute phase, leukemic cells from three different remission periods were used as reference for comparison of gene expression during the attack. Three days following the burst of the attack the level of CD70 and CD27 increased 38 and 25 fold, respectively. During the next 8 days, in parallel with the spontaneous decay of the attack, expression of CD70 and CD27 gradually decreased approaching the remission phase level (Fig. 2). The higher folds of expression compared to those indicated in Table 1 (7 and 2.6, respectively) probably reflect the use of a different remission cell reference. Higher folds of expression were also found in this assay for TGFRIII and BIK (240 and 150 vs. 42.2 and 32.0, respectively). The time of maximal expression of TGFRIII and BIK remained the 5th day of the attack (not shown). Cell surface expression of CD70 and CD27 was determined on CD19+ CD5+ leukemic cells by 4 colors FACS analysis. Flow cytometric dot plots show that expression of CD70 and CD27 on the majority of the leukemic cells increased upon induction of the attack (Fig. 3A). The cells were examined during 4 different remission periods and 5 out of 9 leukemic attacks occurred during the first 3 years of the disease. CD70 was expressed on the majority of CD19+CD5+ leukemic cells during the attack but on less than 10% of them during remission periods while CD27 was consistently expressed on all the leukemic cells. The level of both CD70 and CD27 expression was maximal on the second-third day of the attack (Fig. 3B). Thus, during the peak of the acute phase 80% of the leukemic cells co-expressed high levels of membrane CD70 and CD27 while during remission periods 90% of the leukemic cells expressed CD27 but no detectable CD70 and 5-10% of them co-expressed CD70 and CD27. The intensity of CD70 staining during remission indicates that the small fraction of leukemic cells included in the CD70-positive subpopulation express high levels of CD70. This oscillation pattern of membrane CD70 and CD27 expression was consistent during the first 3 years of the disease while the patient did not receive any specific medication. Later on, following the 9th leukemic attack, prednisone at 30 mg/day was instituted at the onset of the attack and the dose was subsequently tapered off over a period of 30 days. The stimulation of membrane CD70 9 expression during the attack was inhibited by the prednisone treatment while elevated expression of membrane CD27 was stabilized (Fig. 4). Soluble CD27 in the patient's serum. Soluble CD27 (sCD27), which is capable of binding cell surface CD70, may impede the cellular response of membrane CD27 to CD70 presenting cells (25). Hence, examination of the involvement of CD70-CD27 interaction in progression of the disease requires determination of sCD27 levels in the patient's serum during different phases of the disease. The concentration of sCD27 was determined by ELISA and was expressed as units per milliliter in reference to sera of 11 healthy blood donors. The concentration of sCD27 in the sera of normal donors was 185±80 (U/ml). The patient's sera were examined while prednisone treatment was given during the attack, as no sera were available prior to this period. The patient's sera were taken on the 6th or 7th day of 4 different attacks, during a regression period (on day 20 of the attack), and during 3 remission periods (30, 90 and 150 days from initiation of the recent attack). During the 6th and 7th day of the attack the levels of sCD27 were 1600-3500 U/ml. These levels decreased to 600 (U/ml) during regression of the attack in the next 2 weeks and remained at the same level during remission periods (Fig. 5). Thus, the level of sCD27 in the patient's serum oscillates with the leukemic cycle being 3-5 folds of normal level during remission periods and further increased 35 folds during the attacks. Functional analysis of CD70 and CD27 ligation on the leukemic cells. Ligation of CD70 or CD27 on the leukemic cells membrane does not affect the rate of apoptosis. Extreme changes in the rate of apoptosis of the leukemic cells during the leukemic cycle (22, 23) and oscillation in expression of some BCL-2 family genes (24) prompted us to examine the possible involvement of membrane CD70 and CD27 in apoptosis. Leukemic cells from acute phases and remission periods were incubated with 1-9g/ml mAb directed to CD70 or CD27, (KI-24 or 1A4, respectively). The effect of the antibodies on spontaneous apoptosis of the leukemic cells in culture was examined by Annexin-PI analysis. The indicated mAbs were previously reported to affect some lymphocyte activities. Binding of KI-24 anti CD70 mAb to 10 CD70-positive glioblastoma cells increased allo-proliferation and decreased apoptosis of T lymphocytes in a mixed tumor-T lymphocyte reaction (25), while 1A4 anti CD27 mAb inhibited lympohcytes activation and proliferation (26, 27). Figure 6 shows that the bound CD70 and CD27 mAbs did not affect the rate of apoptosis, either that of the acute phase leukemic cells exhibiting rapid apoptosis or that of the remission phase leukemic cells exhibiting slower apoptosis. This result suggests that cell surface CD70 and CD27 are not directly involved in apoptosis of the leukemic cells. Ligation of CD70 enhances proliferation of the leukemic cells from remission but not those from the acute phase. The leukemic cells of this patient do not proliferate in culture spontaneously. CD70 ligation with anti-CD70 mAb strongly enhanced proliferation of the remission phase leukemic cells submitogenically stimulated with PMA. In contrast, leukemic cells from the acute phase did not exhibit such CD70-mediated proliferation. Ligation of CD27 on the leukemic cells from either remission or the acute phase had no significant effect on proliferation (Fig. 7). The enhancement of proliferation by CD70-ligation resulted from response of the leukemic cells rather than that of normal lymphocytes. Thus, leukemic cells from 3 different remission periods were examined following selection of CD19+ cells on magnetic beads. The purified cells, containing 94-98% CD19+CD5+ leukemic cells, exhibited elevated proliferation as a result of CD70 ligation (Fig. 8). CD70 mAb did not induce proliferation in absence of PMA (data not shown). Ligation of CD70 on leukemic cells from 4 different acute phases at different stages of the attack did not enhance proliferation. In contrast, ligation of CD40 on the leukemic cells from acute phases, but not remission periods, enhanced proliferation (Fig. 8). Thus, during remission the leukemic cells proliferate in response to CD70 ligation; with induction of the acute phase they lose this property and acquire the ability to proliferate in response to CD40 ligaton. 11 Discussion In this study we have investigated a possible contribution of CD70 and CD27 to progression of an unusual B cell lymphoma/leukemia characterized by cycles of leukemic phase alternating with spontaneous remission. We focused here on CD70 and CD27 because the interaction between them may affect lymphocyte activation, proliferation, and death (1, 2) raising the possibility that they are involved in the induction and regression of the recurrent acute attacks. The results presented herein were mostly obtained during the first 3 years of the disease during which the patient experienced 9 leukemic cycles without any specific therapy. However, Cell surface expression of CD70 and CD27 and sCD27 in the serum, were also examined during a later stage of the disease while the patient received prednisone during the attack. Ttranscriptional profiling of the leukemic cells by microarray analysis showed massive changes in gene expression between different stages of the disease. Increased expression of cell growth enhancers and inhibitors as well as apoptosis enhancers was observed at an early stage of the leukemic attack. For example, initiation of the attack was followed by highly increased expression of galectin 1, implicated in enhancements of the Ras signal transduced to ERK (28) via the MEK pathway and PKB activity (29) via the PI3K pathway. Relevant to this may be the observation of Arens et al (19) who have reported that CD70 signaling in murine B cells depends on initiation of MEK and PI3K pathways. On the other hand, termination of the MEK signal could be affected by elevated expression of MKP2 that dephosphorylates MAP kinases ERK1 and ERK2. This in turn could downregulate the MEK pathway during decay of the attack. As for the suppressors of cell growth, the elevated expression of TGFRIII (and CDK2AP1, which is induced by TGF could be relevant to the regression of the attack. This possibility is suggested by two observations. First, TGF functions in CLL as an auto-reactive growth inhibitor accounting for reduced proliferative response of the leukemic cells to CD40L (30). Second, increased expression of TGFRIII is sufficient to enhance TGF signaling (31). CD70 and CD27 were among the 216 genes whose expression consistently increased upon induction of the acute phase concurrently with activation and blast transformation of the leukemic cells. A detailed 4 colors FACS analysis showed that the level of membrane CD70 and CD27 on the CD19+CD5+ leukemic cells was maximal 2-3 days following initiation of the leukemic attack. CD27 was consistently expressed on all the leukemic cells while CD70 was 12 expressed on 80% of the cells at the peak of the acute phase and on less than 10% of them during remission. The fluctuations in cell surface expression of CD70 and CD27 characterized the 9 leukemic cycles that occurred without specific therapy. A different situation was observed during the second stage of the disease, in which prednisone treatment was given throughout the acute phase. The prednisone treatment did not prevent the appearance of 18 additional attacks but they were shorter and the lymphadenopathy less prominent (23). Cell surface CD70 levels in presence of prednisone were not elevated during the attack while increased levels of CD27 were attenuated. The stimulation in CD70 expression occurring in this atypical CLL patient concomitantly with cell activation and blastoid transformation is reminiscence of mantle cell lymphoma in which up-regulation of CD70 coincides with blastoid transformation (32). The consistent up and down regulation of cell surface CD70 and CD27 along the recurrent leukemic attacks and remission periods, is compatible with a functional role of these proteins in the cyclic nature of the disease. CD70 and CD27 mAbs were applied to examine the possible involvement of cell surface CD70 and CD27 in activation and regression of the leukemic attacks. We have found that the rate of apoptosis of the leukemic cells was not affected by either CD70 or CD27 mAb, suggesting that cell surface CD70 and CD27 are not involved in the accelerated apoptosis of the acute phase cells or the slow apoptosis of the remission phase cells (22). However, PMA-mediated proliferation of the leukemic cells from remission phases, but not that of the acute phase cells, was considerably enhanced by CD70 mAb. This augmented proliferation of the remission phase cells was specific for CD70-ligation as mAbs directed to several other membrane molecules, including CD27 mAb, had no effect on proliferation. The finding that the remission phase cells respond to CD70 while the acute phase cells expressing higher level of cell-surface CD70 are none-responsive, raises the possibility that other factors determine whether ligation of CD70 may result in proliferation. A similar phenomenon has been observed in CLL where, in addition to expression of surface Ig, the integrity of the BCRcoupled signaling complex determines the functional outcome of BCR-ligation (33). Our finding is in agreement with that of Lens et al (17) who reported that leukemic cells of 4/18 CLL patients proliferated in response to CD70 mAb. However, CD70 expression per se did not predict whether CLL cells would proliferate in response to CD70 Ab. Expression of CD70 together with CD27 on the leukemic cells raises the possibility that this interaction may 13 constitute an autocrine circuit regulating the malignant cells proliferation. Alternatively, the T cells infiltrating the lymphoid stroma in this patient (23) could as well provide the CD27 as ligand for CD70 on the tumor cells. We have previously found that the patient’s cells exhibited resting state during remission periods and activated state at the initiation of the leukemic attack. Cell activation became apparent by blast-transformation and elevated expression of CD23, CD25, ICAM-1, and LFA-3 (22, 23). The cell activation, the bouts of TNF and IL-10 detected in the serum during early acute phases and the production of TNF and IL-10 by activated leukemic cells in culture (23) suggested that the neoplastic cells responded to an activation signal at the onset of each leukemic attack. The leukemic cells from the attack but not those from remission exhibited high proliferative response to CD40L. The potent responsiveness of the acute phase leukemic cells to CD40L is compatible with the finding that during acute phase the patient’s bone marrow was heavily infiltrated with both CD40L-positive T cells and the neoplastic cells (23). These results suggested that CD40L+, reactive T lymphocytes residing in the patient’s bone marrow support proliferation of the neoplastic cells during the acute leukemic phases. Notably, however, the proliferation response of the resting, remission phase cells to CD40L was significantly lower than that of activated, acute phase cells (23). This observation implied that initiation of extensive proliferation of the resting neoplastic cells at onset of acute phases requires an additional activation signal. The finding herein that the remission phase leukemic cells proliferate effectively in response to CD70-ligation and less effectively in response to CD40L while the acute phase cells do not respond to CD70-ligation but proliferate in response to CD40L, suggests that signaling via CD70 precedes that of CD40 in promoting the leukemic attack. The recurrent change in CD70 responsiveness of the leukemic cells could be explained by several ways: 1. The CD70 unresponsiveness of the acute phase cells could result from binding of sCD27 to cell surface CD70 making it unavailable to the stimulating CD70 Ab. This possibility seems however unlikely since the ratio of sCD27 to membrane CD70 is 3-5 times higher during remission periods while the cells respond effectively to CD70 signaling. 2. The second interpretation is based on a previous observation (22) that two B-cell clones with differently rearranged heavy-chain genes consistently appeared in the blood of this patient during recurrent acute phases. During the spontaneous remissions, one clone (termed the "acute 14 clone") regressed while the second clone (the "remission clone"), remained relatively stable. Thus, the 2 clones of the leukemic cells may differ in their CD70 responsiveness as follows; the remission clone which comprise the majority of leukemic cells during remission respond to CD70-ligation by enhanced proliferation while the second clone which dominates the acute phase do not respond to CD70. However, preferential proliferation of the remission clone cells, contradicts the previous results which demonstrated that proliferation and death of the acute clone cells and not that of the remission clone cells, determine the cyclic nature of the disease (22). 3. The overall results suggest that the leukemic cells of the acute clone and not those of the remission clone, consistently express cell surface CD70 and respond to its ligation during remission but not during the attack. We do not know what may cause this switch between responsive and none-responsive state of cell surface CD70. A possible explanation will be a change in the signaling cascade. An alternative explanation could be a conformational change of membrane CD70 affecting its responsiveness. A structural rearrangement of cell surface integrins resulting in change of their ligand binding activity was previously described (34). In conclusion, we have found that in this lymphoma/leukemia case a switch from responsiveness to unresponsiveness of CD70 occurs on the leukemic cells during initiation of the acute phase. Prior to this transition, cell surface CD70 could supply a co-stimulatory receptor for cell proliferation and thus provide a growth advantage to the responder leukemic clone. Termination of this CD70 response concurrently with cell activation and blast transformation of the leukemic cells could contribute to regression of the acute phase in this 'cyclic' disease. The finding that spontaneous remission follows the acute phase in spite of elevated proliferation response to CD40 ligation, support the notion that continuous growth of the leukemic cells requires CD70 response in this case. In human leukemias and lymphomas that constitutively express cell surface CD70 it may provide a co-stimulator receptor for tumor cells proliferation. Whether this responsiveness is required for tumor cell growth and could be regulated by a switch in CD70 reactivity should be examined in a future study. Acknowledgments We thank R. Pinkas-Kramarsky, R. Dardik and A. Simon for valuable advices and G. Kaufmann for critical reading of the manuscript. 15 References 1. Smith, C. A., T. Farrah, and R. G. Goodwin. 1994. The TNF receptor superfamily of cellular and viral proteins: activation, costimulation, and death. Cell 76:959. 2. Gruss, H. J., and S. K. Dower. 1995. Tumor necrosis factor ligand superfamily: involvement in the pathology of malignant lymphomas. Blood 85:3378. 3. Lens, S. M., R. de Jong, B. Hooibrink, G. Koopman, S. T. Pals, M. H. van Oers, and R. A. van Lier. 1996. Phenotype and function of human B cells expressing CD70 (CD27 ligand). Eur J Immunol 26:2964. 4. Oshima, H., H. Nakano, C. Nohara, T. Kobata, A. Nakajima, N. A. Jenkins, D. J. Gilbert, N. G. Copeland, T. Muto, H. Yagita, and K. Okumura. 1998. Characterization of murine CD70 by molecular cloning and mAb. Int Immunol 10:517. 5. Klein, U., K. Rajewsky, and R. Kuppers. 1998. Human immunoglobulin (Ig)M+IgD+ peripheral blood B cells expressing the CD27 cell surface antigen carry somatically mutated variable region genes: CD27 as a general marker for somatically mutated (memory) B cells. J Exp Med 188:1679. 6. Agematsu, K., S. Hokibara, H. Nagumo, and A. Komiyama. 2000. CD27: a memory Bcell marker. Immunol Today 21:204. 7. Gravestein, L. A., J. D. Nieland, A. M. Kruisbeek, and J. Borst. 1995. Novel mAbs reveal potent co-stimulatory activity of murine CD27. Int Immunol 7:551. 8. Sugita, K., M. J. Robertson, Y. Torimoto, J. Ritz, S. F. Schlossman, and C. Morimoto. 1992. Participation of the CD27 antigen in the regulation of IL-2-activated human natural killer cells. J Immunol 149:1199. 9. Hamann, D., P. A. Baars, M. H. Rep, B. Hooibrink, S. R. Kerkhof-Garde, M. R. Klein, and R. A. van Lier. 1997. Phenotypic and functional separation of memory and effector human CD8+ T cells. J Exp Med 186:1407. 10. Loenen, W. A., E. De Vries, L. A. Gravestein, R. Q. Hintzen, R. A. Van Lier, and J. Borst. 1992. The CD27 membrane receptor, a lymphocyte-specific member of the nerve growth factor receptor family, gives rise to a soluble form by protein processing that does not involve receptor endocytosis. Eur J Immunol 22:447. 16 11. Lens, S. M., K. Tesselaar, M. H. van Oers, and R. A. van Lier. 1998. Control of lymphocyte function through CD27-CD70 interactions. Semin Immunol 10:491. 12. Arens, R., K. Tesselaar, P. A. Baars, G. M. van Schijndel, J. Hendriks, S. T. Pals, P. Krimpenfort, J. Borst, M. H. van Oers, and R. A. van Lier. 2001. Constitutive CD27/CD70 interaction induces expansion of effector-type T cells and results in IFNgamma-mediated B cell depletion. Immunity 15:801. 13. Yamada, S., K. Shinozaki, and K. Agematsu. 2002. Involvement of CD27/CD70 interactions in antigen-specific cytotoxic T-lymphocyte (CTL) activity by perforinmediated cytotoxicity. Clin Exp Immunol 130:424. 14. Taraban, V. Y., T. F. Rowley, and A. Al-Shamkhani. 2004. Cutting edge: a critical role for CD70 in CD8 T cell priming by CD40-licensed APCs. J Immunol 173:6542. 15. Bullock, T. N., and H. Yagita. 2005. Induction of CD70 on dendritic cells through CD40 or TLR stimulation contributes to the development of CD8+ T cell responses in the absence of CD4+ T cells. J Immunol 174:710. 16. Yang, F. C., K. Agematsu, T. Nakazawa, T. Mori, S. Ito, T. Kobata, C. Morimoto, and A. Komiyama. 1996. CD27/CD70 interaction directly induces natural killer cell killing activity. Immunology 88:289. 17. Lens, S. M., P. Drillenburg, B. F. den Drijver, G. van Schijndel, S. T. Pals, R. A. van Lier, and M. H. van Oers. 1999. Aberrant expression and reverse signalling of CD70 on malignant B cells. Br J Haematol 106:491. 18. Orengo, A. M., C. Cantoni, F. Neglia, R. Biassoni, and S. Ferrini. 1997. Reciprocal expression of CD70 and of its receptor, CD27, in human long term-activated T and natural killer (NK) cells: inverse regulation by cytokines and role in induction of cytotoxicity. Clin Exp Immunol 107:608. 19. Arens, R., M. A. Nolte, K. Tesselaar, B. Heemskerk, K. A. Reedquist, R. A. van Lier, and M. H. van Oers. 2004. Signaling through CD70 regulates B cell activation and IgG production. J Immunol 173:3901. 20. Stein, H., H. Herbst, I. Anagnostopoulos, G. Niedobitek, F. Dallenbach, and H. C. Kratzsch. 1991. The nature of Hodgkin and Reed-Sternberg cells, their association with EBV, and their relationship to anaplastic large-cell lymphoma. Ann Oncol 2 Suppl 2:33. 17 21. Ranheim, E. A., M. J. Cantwell, and T. J. Kipps. 1995. Expression of CD27 and its ligand, CD70, on chronic lymphocytic leukemia B cells. Blood 85:3556. 22. Kaufmann, Y., A. Many, G. Rechavi, O. Mor, M. Biniaminov, E. Rosenthal, M. Levanon, J. Davidsohn, I. Aizman, Z. Mark, and et al. 1995. Brief report: lymphoma with recurrent cycles of spontaneous remission and relapse--possible role of apoptosis. N Engl J Med 332:507. 23. Aizman, I., A. Many, E. Rosenthal, G. Schiby, I. Goldberg, V. Barak, B. Ramot, and Y. Kaufmann. 2000. Neoplastic cell activation and proliferative response to CD40-ligand characterize recurrent leukemic bouts in an unusual case of low grade lymphoma. Leuk Lymphoma 36:613. 24. Aizman, I., A. Many, S. Peller, B. Ramot, and Y. Kaufmann. 2000. Expression of wildtype p53 and Bcl-2 family genes oscillates with recurrent remission and relapse in an unusual case of low-grade lymphoma. Acta Haematol 103:177. 25. Wischhusen, J., G. Jung, I. Radovanovic, C. Beier, J. P. Steinbach, A. Rimner, H. Huang, J. B. Schulz, H. Ohgaki, A. Aguzzi, H. G. Rammensee, and M. Weller. 2002. Identification of CD70-mediated apoptosis of immune effector cells as a novel immune escape pathway of human glioblastoma. Cancer Res 62:2592. 26. Sugita, K., Y. Torimoto, Y. Nojima, J. F. Daley, S. F. Schlossman, and C. Morimoto. 1991. The 1A4 molecule (CD27) is involved in T cell activation. J Immunol 147:1477. 27. Kobayashi, N., H. Nagumo, and K. Agematsu. 2002. IL-10 enhances B-cell IgE synthesis by promoting differentiation into plasma cells, a process that is inhibited by CD27/CD70 interaction. Clin Exp Immunol 129:446. 28. Paz, A., R. Haklai, G. Elad-Sfadia, E. Ballan, and Y. Kloog. 2001. Galectin-1 binds oncogenic H-Ras to mediate Ras membrane anchorage and cell transformation. Oncogene 20:7486. 29. Baran, C. P., S. Tridandapani, C. D. Helgason, R. K. Humphries, G. Krystal, and C. B. Marsh. 2003. The inositol 5'-phosphatase SHIP-1 and the Src kinase Lyn negatively regulate macrophage colony-stimulating factor-induced Akt activity. J Biol Chem 278:38628. 18 30. Lotz, M., E. Ranheim, and T. J. Kipps. 1994. Transforming growth factor beta as endogenous growth inhibitor of chronic lymphocytic leukemia B cells. J Exp Med 179:999. 31. Blobe, G. C., X. Liu, S. J. Fang, T. How, and H. F. Lodish. 2001. A novel mechanism for regulating transforming growth factor beta (TGF-beta) signaling. Functional modulation of type III TGF-beta receptor expression through interaction with the PDZ domain protein, GIPC. J Biol Chem 276:39608. 32. Zhu, Y., J. Hollmen, R. Raty, Y. Aalto, B. Nagy, E. Elonen, J. Kere, H. Mannila, K. Franssila, and S. Knuutila. 2002. Investigatory and analytical approaches to differential gene expression profiling in mantle cell lymphoma. Br J Haematol 119:905. 33. Lankester, A. C., G. M. van Schijndel, C. E. van der Schoot, M. H. van Oers, C. J. van Noesel, and R. A. van Lier. 1995. Antigen receptor nonresponsiveness in chronic lymphocytic leukemia B cells. Blood 86:1090. 34. Takagi, J., and T. A. Springer. 2002. Integrin activation and structural rearrangement. Immunol Rev 186:141. 19 Figure Legends Figure 1. Comparative gene expression profiles of purified leukemic cells obtained from the atypical B-CLL patient during remission and different stages of the acute phase. The leukemic cells were taken on day 3, 5, 7 and 11 of the acute phase and during a remission phase and purified on CD19 beads. Transcriptional profiles of purified leukemic cells containing 94-98% CD5+CD19+ cells was obtained by microarray analysis. Figure 1A shows an unsupervised hierarchal clustering of 5963 valid probe sets out of the total 12625 probe sets. A distinction was made between the samples taken close to the onset of the attack (day 3 and day 5) as compared to the samples taken later (day 7 and day 11) which exhibited expression profile closer to that of the remission period. This is emphasized in the enlarged subcluster (figure 1B) representing 216 probe sets which are up regulated in the samples taken on the third and fifth day of the attack and down regulated in the samples taken later in the attack (day 7 and day 11) and in the remission sample. Included in the 216 genes subcluster are: (a) CD70, TNFligand (TNFSF7) (AffID 34054-at Acc L08096) and (b) CD27, TNF-receptor (TNFRSF7) (AffID 38578-at Acc M63928). Yellow indicates high relative expression and blue low expression. Each column represents a sample and each row a gene. Figure 2. RTQ-PCR analysis of CD70 and CD27 gene expression in the leukemic cells during remission and the leukemic attack. Comparative ratio analysis by RTQ-PCR of CD70 (TNFSF7) and CD27 (TNFRSF7) gene expression in purified leukemic cells during the leukemic cycle. The Y axis shows relative gene expression. The average expression level of CD70 and CD27 during 3 different remission periods (R) was taken as 1. Expression level of CD70 and CD27 increased 37 and 25 folds, respectively, during transition from remission to the third day of the attack followed by gradual decrease to the remission phase level. Figure 3. Cell surface expression of CD70 and CD27 on the leukemic cells is increased concomitantly with transition from remission to the acute phase. Four colors FACS analysis shows cell surface expression of CD70 and CD27 gated on CD19+CD5+ double positive leukemic cells. A. Flow cytometric dot plots illustrate labeling of CD19+CD5+ cells with 20 antibodies to CD70 and CD27 during remission and on the third day of the leukemic attack. The percentage of cells in the upper right quadrant (CD70+CD27+) is indicated. B. Accumulated data represent staining intensity and percentage of CD70+CD27+ and CD70CD27+ leukemic cells during early (R1) and late (R2 and R3) remission periods and on different days (2nd-11th) following the initiation of the leukemic attack. The percentage of CD70+CD27+ cells increased from 5-10% during remission periods to 80-90% on the second-third day of the attack. Maximal density of cell surface CD70 and CD27 was observed at an early stage of the attack. Figure 4. Prednisone treatment during the attack prevents elevation of cell surface CD70 expression on the leukemic cells. Comparative expression of cell surface CD70 and CD27 on the leukemic cells in absence and presence of prednisone. Four colors FACS analysis of CD19+CD5+ leukemic cells shows that prednisone treatment inhibited stimulation of cell surface CD70 during the attack. In contrast, elevation of cell surface CD27 at the initiation of the attack was unaffected by prednisone treatment and its reduction during regression was attenuated. Figure 5. Elevated levels of sCD27 in the patient's Serum. Serum samples were examined for sCD27 on the day indicated following the initiation of the attack. Sera representing 2 different "leukemic cycles" were analyzed. Sera of 11 normal controls contained 185±80 U/ml sCD27. The levels of sCD27 in the patient's serum were elevated during remission and were further increased during the attack. Figure 6. cells. Antibodies to CD70 and CD27 do not affect the rate of apoptosis of the leukemic Spontaneous apoptosis of the leukemic cells in culture was examined. The results expressed by annexin positive cells show the percent of apoptotic cells following 7 h or 24 h incubation. Leukemic cells from the peak of the acute phase exhibiting rapid spontaneous apoptosis (39% in 7h and 94% in 24h ) or leukemic cells from remission period exhibiting slower apoptosis (23% in 7h and 36% in 24h ), were incubated in absence or presence of 6 g/ml of either anti CD70 mAb (clone ki-24) or CD27 mAb (clone 1A4). Data are expressed as 21 average values of 4 different experiments with cells from 2 different "leukemic cycles". The rate of spontaneous apoptosis of the leukemic cells was not affected by either mAb. Figure 7. The effect of CD70 and CD27 mAbs on proliferation of leukemic cells obtained during remission and acute phase. The patient's leukemic cells obtained during remission period or on the fifth day of the acute phase were preincubated for 30 min at 200C in the absence or presence of 1- g/ml of either anti CD70 mAb (clone ki-24) or CD27 mAb (clone 1A4). PMA (1ng/ml) was added and cell proliferation was tested after 4 days of culturing. The data of one representative experiment of three are displayed as average cpm (SE values ranged between 1-5%). Cells from 3 different "leukemic cycles" were analyzed. Proliferation of leukemic cells from the remission phase but not that of the acute phase cells was enhanced by CD70 mAb. CD27 mAb did not significantly affect proliferation of the leukemic cells. Figure 8. CD70 mAb enhances proliferation of purified leukemic cells obtained during remission whereas CD40L enhances proliferation of those obtained during the attack. The leukemic cells were taken on the third and fifth day of the acute phase and during two different remission periods and purified on CD19 beads. The purified leukemic cells were cultured in g/ml of either anti CD70 mAb (clone ki-24) or CD27 mAb (clone 1A4). To examine the effect of CD40 triggering, the leukemic cells were cultured with -irradiated CD40L-presenting cells. Shown is one representative experiment out of three. CD70 mAb enhanced proliferation of the leukemic cells obtained during remission and did not affect the acute phase cells. CD40L induced proliferation of the leukemic cells obtained during the attack and did not affect the remission phase cells. 22 Table I. Differentially expressed genes during the leukemic attack Functional category/Gene name GenBank Acc No.a Fold Change relative to Remission Day in the attack Cell activation and signal transduction CD80 antigen pre-B-cell colony-enhancing factor, PBEF1 galectin 1 dual specificity phosphatase 4, MKP2 Proliferation CD70, TNFSF7 CD137 ligand, TNFSF9 cyclin B1 M-phase phosphoprotein 1 Growth inhibition transforming growth factor receptor III CDK2-associated protein 1, CDK2AP1 S100 Ca-binding protein A11, calgizzarin Apoptosis BCL2 interacting killer, BIK poly(rc) binding protein 4, MCG10 quinone oxidoreductase homolog, PIG3 deoxyribonuclease I-like 3, DNASE1L3 caspase 9 BCL2 associated protein, BAX CD27, TNFRSF7 M27533 U02020 AI535946 U48807 3 5 7 11 ___________________ 3.3 4.0 3.5 2.8 4.0 3.0 1.4 2.5 48.5 27.9 19.7 8.6 8.6 3.2 2.6 5.7 L08096 U03398 M25753 L16782 7.5 4.3 4.3 1.6 3.0 1.6 1.6 3.0 3.5 3.2 1.4 3.5 L07594 AF006484 D38583 22.6 42.2 18.4 3.5 5.7 3.7 5.7 7.5 2.8 21.1 2.3 1.9 U34584 W22541 AF010309 U75744 U60521 U19599 M63928 13.9 32.0 6.5 4.6 4.6 3.5 4.0 4.0 3.0 3.7 1.6 3.5 2.6 2.6 -1.1 4.9 -1.6 2.3 1.3 1.7 1.3 a GenBank accession number. 23 4.6 2.6 7.5 4.0 5.7 3.7 1.1 1.1 1.2 2.1 1.5