Anastasio_dissertation - Institutional Repositories
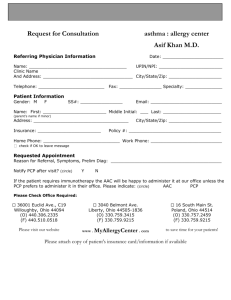
advertisement

The committee for Noelle Catherine Anastasio certifies that this is the approved version of the following dissertation: Effects of Perinatal Phencyclidine Treatment on Neuronal Viability, N-Methyl-D-Aspartate Receptor Regulation and Schizophrenic-like Behaviors Committee: Kenneth M. Johnson, Ph.D. ,Supervisor Kathryn A. Cunningham, Ph.D. Kelly T. Dineley, Ph.D. Joel P. Gallagher, Ph.D. Geoffrey T. Swanson, Ph.D. ______________________________ Dean, Graduate School Effects of Perinatal Phencyclidine Treatment on Neuronal Viability, N-Methyl-D-Aspartate Receptor Regulation and Schizophrenic-like Behaviors By Noelle Catherine Anastasio, M.S. Dissertation Presented to the Faculty of the Graduate School of Biomedical Sciences of The University of Texas Medical Branch at Galveston in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy The University of Texas Medical Branch March, 2009 for my grandfather Acknowledgements I would like to express my gratitude to my advisor, Dr. Ken Johnson, for his support and encouragement. He pushed and challenged me to always do my best and his trust in me allowed me to develop in to the independent scientist that I am today. I wish to also thank the members of my committee, Drs. Kathryn Cunningham, Kelly Dineley, Joel Gallagher and Geoffrey Swanson for their expertise and advice, both in and out of the laboratory. This work was supported by a Ruth L. Kirschstein NRSA F31 Fellowship from the National Institute on Drug Abuse. I would also like to thank Dr. Cheng Z. Wang and Dr. Gang Lei for their technical expertise and countless scientific discussions concerning not only my studies, but the field of schizophrenia animal models as well. I must of course mention Yan Xia, aka “Sunshine”; with her there was never a dull moment in the lab. Her ability to make me laugh and her constant support and encouragement made coming to work a joy. I must also thank Dr. Marcy Jordan for her friendship, ability to answer any question I had about the inner workings of UTMB, the endless science discussions, and most importantly, for always being there when I needed her most. On a personal note, I must thank Tad Conaty for his love, encouragement and patience throughout this process. To my parents, thank you for nurturing the inner scientist in me as a child by encouraging me to always ask questions and when the answer was unknown to discover a way to answer it myself. I must also thank you for being my biggest fans and for supporting me every step of the way as I pursued a higher education. A special thanks to my sister, Bethany, who has taught me to not take it all so seriously. iv Effects of Perinatal Phencyclidine Treatment on Neuronal Viability, N-Methyl-D-Aspartate Receptor Regulation and Schizophrenic-like Behaviors Publication No._____________ Noelle Catherine Anastasio, Ph.D. The University of Texas Medical Branch, 2009 Supervisor: Kenneth M. Johnson Clinical use of phencyclidine (PCP), a potent dissociative anesthetic, was abandoned as a result of reports of post-operative hallucinations and disoriented behavior; further, illicit use has substantially diminished because of its psychotomimetic properties. PCP intoxication in humans has also been shown to mimic both the positive and negative symptoms of schizophrenia as well as exacerbate psychoses in schizophrenics. PCP elicits its major actions as a noncompetitive NMDA receptor (NMDAR) antagonist. Administration to immature rats has been shown to cause neurotoxicity in a regional and treatment dependent manner and development of schizophrenic-like behaviors later in life. The purpose of this study is to determine the mechanism and functional consequences of PCP-induced regulation of the NMDAR in association with neurotoxicity in the frontal cortex and if there is a causal relationship between cell death and the development of aberrant behaviors in perinatal rats. The first specific aim of this project will focus on delineating the mechanisms of regulation of the NMDAR, specifically the role of synthesis and trafficking of the receptor following acute and sub-chronic PCP administration. Specific aim 2 is designed to determine the functionality of the cortical NMDAR following both acute and sub-chronic PCP treatment by assessing NMDA- and glycine-dependent activation of 3H-MK-801 binding. The subunit composition of the NMDAR that mediates PCP-induced neuronal neurotoxicity is currently unknown; therefore, we designed specific aim 3 to show that the synaptic or extrasynaptic localization of NMDA NR2A and 2B receptors may dictate function and neuronal susceptibility to cell death. Finally, the purpose of specific aim 4 is to demonstrate that neurotoxicity underlies the development of behaviors which model several aspects of schizophrenia, including the positive symptoms (locomotor sensitization), the negative symptoms (social interaction and social discrimination) and deficits in sensorimotor gating (PPI of acoustic startle). Work v within this dissertation discovered that PCP induces neurotoxicity in developing pups in a manner that is highly regulated affecting the distribution, composition, number, and function of NMDAR and that this loss of cortical neurons and altered cortical landscape is associated with behavioral deficits that are similar to both the positive and negative symptoms of schizophrenia. vi Table of Contents List of Tables ..................................................................................................... xi List of Figures ................................................................................................... xii List of Figures ................................................................................................... xii List of Abbreviations ........................................................................................ xv Chapter 1: Introduction ...................................................................................... 1 Phencyclidine (PCP) and noncompetitive NMDA receptor antagonists ......... 1 The NMDA Receptor ..................................................................................... 3 Schizophrenia................................................................................................ 4 Pathophysiology of schizophrenia ................................................................. 5 NMDAR-mediated neurotoxicity and aberrant behaviors in rodent models of schizophrenia ................................................................................................ 7 Hypothesis 1 .............................................................................................. 12 Specific Aim 1a ............................................................................................ 13 Specific Aim 1b ............................................................................................ 14 Hypothesis 2. ............................................................................................. 14 Specific Aim 2 .............................................................................................. 15 Hypothesis 3 .............................................................................................. 16 Specific Aim 3a ............................................................................................ 16 Specific Aim 3b ............................................................................................ 17 Specific Aim 3c ............................................................................................ 17 Hypothesis 4 .............................................................................................. 18 Specific Aim 4a ............................................................................................ 18 Specific Aim 4b ............................................................................................ 19 vii Chapter 2: NR2A-Containing Synaptic NMDARs Mediate PCP-Induced Cortical Neurotoxicity and the Subsequent Development of Schizophrenialike Behaviors ................................................................................................... 20 Introduction ............................................................................................... 20 Materials and Methods .............................................................................. 23 Animals .................................................................................................... 23 Drugs. ...................................................................................................... 23 Organotypic slice culture.......................................................................... 24 In vivo experimental design. .................................................................... 24 Terminal dUTP Nick-End Labeling (TUNEL)............................................ 25 Caspase-3 Activity. .................................................................................. 25 Co-Immunoprecipitation and Western Blotting. ........................................ 26 Antibodies. ............................................................................................... 27 Locomotor Activity. .................................................................................. 28 Statistical Analysis ................................................................................... 28 Results ....................................................................................................... 28 Discussion ................................................................................................. 41 Chapter 3: Differential Regulation of the NMDAR by Acute and Sub-chronic Phencyclidine Administration ......................................................................... 48 Introduction ............................................................................................... 49 Materials and methods.............................................................................. 51 Animals. ................................................................................................... 51 Drugs. ...................................................................................................... 51 Experimental design. ............................................................................... 52 Sub-cellular fractionation. ........................................................................ 52 Western blot analysis. .............................................................................. 53 Antibodies. ............................................................................................... 53 Results ....................................................................................................... 54 Discussion ................................................................................................. 63 Chapter 4: Alterations in NMDAR Binding of 3H-MK-801 in Response to Postnatal PCP Administration ......................................................................... 67 Introduction ............................................................................................... 68 viii Materials and methods.............................................................................. 71 Animals. ................................................................................................... 71 Drugs. ...................................................................................................... 71 Experimental design. ............................................................................... 72 3H-MK-801 binding. .................................................................................. 72 Results ....................................................................................................... 74 Discussion ................................................................................................. 82 Chapter 5: Atypical Antischizophrenic Drugs Prevent Changes in Cortical NMDARs and Behavior Following Sub-chronic PCP Administration .......... 86 Introduction ............................................................................................... 86 Materials and Methods .............................................................................. 89 Animals. ................................................................................................... 89 Drugs. ...................................................................................................... 89 Experimental design. ............................................................................... 90 Sub-cellular fractionation. ........................................................................ 90 Western blot analysis. .............................................................................. 91 Antibodies. ............................................................................................... 92 Pre-pulse inhibition (PPI) of acoustic startle. ........................................... 92 Locomotor Activity. .................................................................................. 92 Statistical analysis. .................................................................................. 93 Results ....................................................................................................... 93 Discussion ............................................................................................... 106 Chapter 6: Modeling the Negative Symptoms of Schizophrenia ............... 113 Introduction ............................................................................................. 113 Materials and Methods ............................................................................ 116 Animals. ................................................................................................. 116 Drugs. .................................................................................................... 116 Experimental design. ............................................................................. 116 Social Interaction Test. .......................................................................... 117 Social Discrimination Task. .................................................................... 117 Statistical Analysis. ................................................................................ 118 ix Results ..................................................................................................... 118 Discussion ............................................................................................... 123 Chapter 7: Conclusions and Future Directions .......................................... 127 General Conclusions............................................................................... 127 Specific Aim 1 ............................................................................................ 130 Specific Aim 2 ............................................................................................ 134 Specific Aim 3 ............................................................................................ 135 Specific Aim 4 ............................................................................................ 138 Future Directions ..................................................................................... 139 References ...................................................................................................... 144 x List of Tables Table 5.1 Effects of PCP (10 mg/kg) on weight (g) gain in developing rats ..... 94 xi List of Figures Figure 2.1. Representative photomicrographs showing TUNEL-positive staining in corticostriatal organotypic slice cultures. ........................................................ 30 Figure 2.2. Effects of PCP administration on neurotoxicity in corticostriatal slice cultures. .............................................................................................................. 31 Figure 2.3. Effects of neonatal PCP and selective NR2A and NR2B antagonists on frontal cortex neurotoxicity in PN7 rats. ......................................................... 32 Figure 2.4. Effects of neonatal PCP and selective NR2A and NR2B antagonists on striatal neurotoxicity in PN7 rats. ................................................................... 33 Figure 2.5. Effects of neonatal PCP and selective NR2A and NR2B antagonists on frontal cortex neurotoxicity in young rats. ...................................................... 34 Figure 2.6. Effects of neonatal PCP and selective NR2A and NR2B antagonists on striatal neurotoxicity in young rats. ................................................................ 35 Figure 2.7. Effects of PCP administration on the localization of NR2A and NR2B in the synaptic or extrasynaptic milieu. ............................................................... 37 Figure 2.8. Locomotor sensitization induced by a 4 mg/kg PCP challenge to either sub-chronic PCP or PEAQX treated animals. ........................................... 39 Figure 2.9. Effect of selective blockade of NR2A and NR2B subunits on locomotor sensitization. ...................................................................................... 40 Figure 3.1. Acute PCP administration selectively up-regulates NR1/NR2B in the frontal cortex of perinatal rats. ............................................................................ 56 Figure 3.2. Sub-chronic PCP treatment up-regulates NR1/NR2A in the frontal cortex of perinatal rats. ....................................................................................... 57 Figure 3.3. Effects of acute and sub-chronic PCP administration on the NMDAR subunits in the cortical ER fraction. .................................................................... 58 Figure 3.4. Acute PCP treatment selectively alters levels of PSD-95 in the frontal cortex of perinatal rats. ............................................................................ 59 Figure 3.5. Effects of acute and sub-chronic PCP administration on the activation of calpain in the frontal cortex. ............................................................ 61 xii Figure 3.6. Effects of MDL28170 (calpain inhibitor) on the cortical membrane expression of NMDAR subunits following acute PCP treatment. ........................ 62 Figure 4.1. Effects of agonist stimulation (100 µM NMDA + 30 µM glycine) on 3H-MK-801 binding in the frontal cortex of saline and PN7 PCP treated rat pups. ........................................................................................................................... 75 Figure 4.2. Effects of agonist (100 µM NMDA + 30 µM glycine) stimulation on 3H-MK-801 binding in the frontal cortex of PN7, 9, & 11 PCP treated rat pups. . 76 Figure 4.3. 3H-MK-801 displacement by the NR2B selective antagonist ifenprodil in acute PCP treated animals. ............................................................................ 78 Figure 4.4. 3H-MK-801 displacement by the NR2B selective antagonist ifenprodil in sub-chronic PCP treated animals. .................................................................. 79 Figure 4.5. 3H-MK-801 displacement by the NR2A selective antagonist NVPAAM007 .............................................................................................................. 80 Figure 4.6. 3H-MK-801 displacement by the NR2A preferring antagonist PEAQX ........................................................................................................................... 81 Figure 5.1. Effects of PCP administration (PN7 only) on PPI of acoustic startle. ........................................................................................................................... 96 Figure 5.2. Effects of PCP administration (PN7 only) the development of locomotor sensitization. ...................................................................................... 97 Figure 5.3. Effects of subchronic PCP administration (PN7, 9 & 11) on PPI of acoustic startle.................................................................................................... 98 Figure 5.4. Effects of subchronic PCP administration (PN7, 9 & 11) on the development of locomotor sensitization. ............................................................. 99 Figure 5.5. Pharmacological antagonism of PCP treatment on PN7 effects on NR1 and NR2B in the frontal cortex. ................................................................ 102 Figure 5.6. Pharmacological antagonism of PCP treatment on PN7, 9, & 11induced up-regulation on NR1 and NR2A in the frontal cortex. ........................ 103 Figure 5.7. Effects of a single injection of PCP on PN7 on the membrane protein expression of NR1 and NR2B in the striatum. .................................................. 104 Figure 5.8. Antagonism of PCP treatment on PN7, 9, & 11-induced downregulation on NR1 in the striatum. .................................................................... 105 xiii Figure 6.1. Effects of neonatal PCP administration on social interaction and locomotor activity in pre-and post-pubescent male pups. ................................. 120 Figure 6.2. Effects of neonatal PCP administration on social interaction and locomotor activity in pre- and post-pubescent females. .................................... 121 Figure 6.3. Effects of perinatal PCP treatment on PN7, 9, & 11 on social discrimination in adult (PN56-58) animals. ....................................................... 122 xiv List of Abbreviations 5-HT Serotonin 7-Cl KYNA 7-chloro Kynurenic Acid ACh Acetylcholine AChE Acetyl cholinesterase AMPA α-amino-3-hydroxyl-5-methyl-4-isoxazole-propionate ANOVA Analysis of Variance APV (2R)-Amino-5-phosphonovaleric Acid BDNF Brain Derived Neurotrophic Factor Bmax Maximum bound CB Calbindin CHX Cycloheximide CR Calretinin CRE cAMP Response Element CREB cAMP Response Element Binding DA Dopamine DAG Diacylglycerol DAOA D-amino Acid Oxidase Activator DIV Day in vitro DTNBP1 Dystrobrevin Binding Protein 1 ER Endoplasmic Reticulum ERK Extracellular Signal-Regulated Kinase GABA Gamma-Aminobutyric Acid xv GK Guanylate Kinase GRM3 Metabotropic Glutamate Receptor 3 Gene GSK Glycogen Synthase Kinase i.p. Intraperitoneal IC50 Concentration of inhibitor that inhibits 50% response KA Kainate LTD Long-term depression LTP Long-term potentiation MAGUK Membrane-Associated Guanylate Kinase MDL28170 Calpain Inhibitor III MK-801 Dizocilpine NE Norepinephrine NF-κB Nuclear Factor kappa B NMDAR N-methyl-D-aspartate receptor NR1 NMDA receptor subunit 1 NR2 NMDA receptor subunit 2 NRG1 Neuregulin-1 NVP-AAM007 [(R)-[(S)-1-(4-bromo-phenyl)-ethylamino]-(2,3-dioxo-1,2,3,4tetrahydro-quinoxalin-5-yl)-methyl]-phosphonic acid PCP Phencyclidine OR 1-(1-phenylcyclohexyl) piperidine hydrochloride PDI Protein Disulfide Isomerase PEAQX [[(1S)-1-(4-Bromophenyl) ethyl] amino] (1, 2, 3, 4-tetrahydro-2, 3dioxo-5-quinoxalinyl) methyl PI3K Phosphotidylinositide-3 Kinase xvi PKC Protein Kinase C PLC Phospholipase C PN Postnatal Day PPI Pre-pulse Inhibition PSD-95 Post-Synaptic Density 95 PV Parvalbumin RGS4 Regulator of G-protein Signaling 4 s.c. Subcutaneous SAP102 Synapse Associated Protein 102 SAP97 Synapse Associated Protein 97 SBP α-II spectrin specific breakdown products SH3 Src Homology Domain 3 TUNEL Terminal d-UTP Nick End Labeling xvii Chapter 1: Introduction Phencyclidine (PCP) and noncompetitive NMDA receptor antagonists Phencyclidine [1-(1-phenylcyclohexyl) piperidine hydrochloride or PCP] was originally developed in the 1950s for use as a surgical anesthetic (Johnson & Jones 1990). Despite its effectiveness at producing a state of dissociative anesthesia with little cardio-respiratory depression, clinical use was abandoned because patients reported post-surgical hallucinations, delirium and disoriented behavior (Morris et al. 2005). Due to its hallucinogenic effects and availability, PCP appeared on the drug of abuse scene in the mid-1960’s and was known as “angel dust”, “hog” or the PeaCe Pill (Morris et al. 2005, Johnson & Jones 1990). However, illicit use of PCP fell out of favor because of its psychotomimetic properties (Johnson & Jones 1990). PCP intoxication in humans has been shown to induce a psychotic state in healthy individuals which mimics both the positive and negative symptoms of schizophrenia as well as exacerbates psychoses in schizophrenics (Luby et al. 1962, Javitt & Zukin 1991, Steinpreis 1996). Ketamine, a structurally related arylcycloalkylamine, is a shorter acting dissociative anesthetic that is still used clinically in veterinary medicine and as a pediatric anesthetic in the treatment of burn victims during wound dressing changes (Hirsch et al. 1997). Like PCP, ketamine is also abused illegally and is known on the street as “special K” or “vitamin K” (Morris et al. 2005). Users report dream-like states and hallucinations; however, high doses can result in respiratory depression, delirium and amnesia and schizomimetic liked effects (Krystal et al. 1994). Dizocilpine (MK-801) is a noncompetitive N-methyl-D- aspartate receptor (NMDAR) antagonist that possesses a higher affinity and specificity for the NMDAR compared to PCP and was originally developed to serve as a neuroprotectant following stroke and can also serve as an anticonvulsant (Kochhar et al. 1991, Vanderschuren et al. 1998, Olney et al. 1 1989b). Neither the abuse potential of MK-801 nor its intoxication effect in humans is known, but it is self-administered by animals (Beardsley et al. 1990). PCP possesses a complex and broad pharmacology, affecting various neurotransmitter systems and ion channels (Lodge & Johnson 1990, Johnson & Jones 1990, Morris et al. 2005), including voltage-dependent sodium and potassium channels (French-Mullen & Rogawski 1992, Vincent et al. 1983). PCP appears to largely act as a noncompetitive NMDAR antagonist (Ki of 50-100 nM) (Anis et al. 1983) as an open channel blocker, binding within the channel pore in a voltage and use-dependent manner (Honey et al. 1985, MacDonald et al. 1987, Johnson & Jones 1990). PCP also has been shown to act behaviorally as an anticholinergic in locomotor activity and stereotypy (Johnson & Jones 1990, Finnegan et al. 1976, Murray & Horita 1979). Interestingly, it has also been shown dose-dependently to act as a cholinomimetic and a weak inhibitor of acetyl cholinesterase (AChE) and butyryl cholinesterase (Maayani et al. 1974, Snell et al. 1988); however, this was not well correlated with rotorod activity or the discriminative stimulus properties of PCP (Johnson & Jones 1990, Johnson 1982). PCP also inhibits the σ binding site (Largent et al. 1984), norepinephrine (NE) reuptake (Taube et al. 1975, Garey & Heath 1976), and serotonin (5-HT) reuptake as well as reduces 5-HT turnover (Smith et al. 1977). PCP blockade of the NMDAR can also lead to the release of 5-HT in the prefrontal cortex and hippocampus. The subsequent activation of 5-HT receptors, specifically 5-HT2A, results in the increased release of glutamate (Adams & Moghaddam 2001) and may also underlie the hallucinatory aspects of PCP intoxication (Martin et al. 1998). In addition, PCP blocks dopamine (DA) reuptake (Ki = 0.1µM) (Steinpreis & Salamone 1993, Garey & Heath 1976, Johnson & Jones 1990) and facilitates its release [albeit ten times less potent than amphetamine] (Johnson & Jones 1990, Verma & Moghaddam 1996). DA antagonists are able to antagonize behavioral effects produced by PCP such as cognitive tasks involving working memory in addition to hyperlocomotor activity (Castellani & Adams 1981, Verma 2 & Moghaddam 1996), suggesting a role for DA in the expression of these behaviors. However, these varying actions of PCP are less potent than its actions on the NMDAR; therefore, it is likely that the psychotomimetic actions of PCP are mostly due to its blockade of the NMDAR (Johnson & Jones 1990, Morris et al. 2005), but inhibition of monoamine transport may also play a role. The NMDA Receptor The NMDAR is a member of the ionotropic glutamate family of receptors, which also includes α-amino-3-hydroxyl-5-methyl-4-isoxazole-propionate (AMPA) and kainate (KA) receptors. These receptors act in concert to mediate excitatory neurotransmission in the mammalian brain. The NMDAR is unique among the glutamate receptors in that it requires binding of glutamate to the NR2 subunit and binding of the co-agonist glycine to the NR1 subunit as well as alleviation of the voltage-dependent Mg2+ block in order for the receptor to be open and functionally active. Glutamate receptors promote various phases of neuronal development, including neuronal migration, differentiation, and synaptogenesis (Komuro & Rakic 1993). Further, in the developing brain, specifically during a stage of rapid neurite growth and synapse formation known as the brain growth spurt (Olney et al. 2002), the NMDAR is one of the primary mediators of glutamatergic excitatory neurotransmission and synaptic plasticity and is intricately linked to the development of long-term depression (LTD) and long-term potentiation (LTP) in learning and memory models (Lynch & Guttmann 2002). Nevertheless, in a process known as excitotoxicity, overactivation of NMDA receptors triggers a rapid rise of internal calcium resulting in the activation of prodeath signaling cascades as well as phospholipases, endonucleases, and proteases which can lead to cytoskeletal, membrane and DNA damage and ultimately apoptosis and/or necrosis (Rothman & Olney 1995). 3 Schizophrenia Schizophrenia is a complex neuropsychiatric disorder, characterized by the presence of both positive (paranoia, hallucinations, delusions) and negative symptoms (emotional and social withdrawal, anhedonia, depression) as well as cognitive impairments, such as working memory and attention deficits (McGlashan 1996b). 2000). The etiology currently remains unknown (Weinberger It afflicts around 1% of the population worldwide and shows strong genetic tendencies (Lewis & Lieberman 2000, Bromet & Fennig 1999). It has been described as a neurodevelopmental disorder since symptoms of the first psychotic break do not appear until early adulthood and may result from a combination of susceptible genes as well as unknown environmental factors (Weinberger 1987, Weinberger 1996, Pilowsky et al. 1993, Harrison & Owen 2003). The primary pathological insult, in at least some cases of schizophrenia, is thought to originate in the late second to early third trimester in utero; a stage of brain development in the human that corresponds to the first three weeks of postnatal life in the rat (Benes 1991, Murray et al. 1992, Pilowsky et al. 1993). The functional consequences of this insult do not become evident until after puberty, a time at which many of the affected neural networks reach maturity (Weinberger 1987). That is, damage to the brain remains relatively clinically silent until normal development and neuronal maturity (e.g. dendritic pruning and alterations in cytoarchitecture) unmasks behavioral abnormalities caused by the affected structures (Marenco & Weinberger 2000). Schizophrenia occurs equally in males and females, although onset typically appears earlier in men than women (peak ages of onset are 20–28 years and 26–32, respectively) (Castle et al. 1991). Interestingly, those diagnosed with schizophrenia are more likely to have been born in winter or spring (Davies et al. 2003), delivered during obstetric complications (Geddes & Lawrie 1995), or had a prenatal exposure to infections (e.g. influenza), all of 4 which provide additional support for a link between in utero pathology and risk of developing the disease (Brown 2006). Pathophysiology of schizophrenia A hyper-dopaminergic state is thought to underlie the pathophysiology of schizophrenia and is based on evidence that indirect-acting DA agonists, such as amphetamine, are capable of mimicking the positive symptoms of schizophrenia (Carlsson 1988). In further support of this DA hypothesis of the disease, the clinical potency of all of the early “typical” antipsychotics (e.g. haloperidol and the phenothiazines) to effectively alleviate the hallucinations, paranoia, and delusions associated with schizophrenia is strongly correlated with their affinity for DA D2 receptors (Bunney et al. 2000, Moghaddam 1994). However, typical antipsychotics are not effective at alleviating or controlling the negative symptoms or cognitive deficits of the disease. antipsychotics, termed “atypical” Thus, introduction of newer antipsychotics (clozapine, olanzapine, risperidone), which are effective at treating both positive and negative symptoms, suggested that DA may not be the only player in schizophrenia, since atypical antipsychotics possess relatively high affinity for DA, 5-HT, histamine, α1 noradrenergic, and muscarinic ACh receptors (Bondolfi et al. 1998, Large 2007). The NMDA hypofunction (reduced channel function) theory of schizophrenia is based on the major finding that noncompetitive NMDAR antagonists, including PCP, ketamine, and MK-801 mimic multiple aspects of schizophrenia. Transient inactivation of NMDA receptors by administration of PCP or MK-801 to rodents results in neurotoxicity and structural damage in brain regions somewhat similar to those in which damage is present in schizophrenics (Olney et al. 1989b, Olney & Farber 1995b). Structural damage to the cingulate cortex, hippocampus, parahippocampal gyrus and entorhinal cortex has been observed in postmortem analysis of schizophrenic brains (Kovelman & Scheibel 1984, Bogerts 1993). Further, it was reported that high doses of PCP or MK-801 5 cause neuronal vacuolization in the adult rat retrosplenial and posterior cingulate cortices (Olney et al. 1989b). Also, repeated administration of either MK-801 or PCP in adult rats has been reported to cause neurodegeneration (silver-positive) in the anterior cingulate, parietal, temporal, piriform, and entorhinal cortices, as well as the hippocampus and amygdala (Olney & Farber 1995b). In schizophrenics, there is also evidence for a reduction in mismatch negativity responses following a sensory cue [ketamine has also been reported to reduce mismatch negativity (Umbricht et al. 2000)]; this response has been shown to be mediated by the NMDAR and is an additional indication of NMDAR hypofunction (Javitt et al. 1996, Shelley et al. 1991). Normally, activation of NMDARs on GABAergic interneurons (primarily parvalbumin (PV)-containing basket cells) in the basal ganglia results in an inhibition of excitatory neurotransmission to cortical pyramidal neurons; however, PCP-induced inhibition of the NMDAR on these interneurons results in a disinhibition of neurotransmission, producing an increase in excitation of pyramidal cells in the cortex [confirmed in the rat by electrophysiology (Jackson et al. 2004), metabolic imaging (Sharp et al. 2001, Vaisanen et al. 2004) as well as elevated glutamate release (Moghaddam et al. 1997)]. The subsequent and prolonged overactivation of glutamate receptors on the pyramidal neurons leads to cellular stress and ultimately excitotoxic cell death, (Olney & Farber 1995a, Large 2007). Cortical disinhibition has been reported in schizophrenia as evident by an increase in brain metabolic activity (Friston 1992, Friston et al. 1992, Lisman et al. 2008). Further, examination of post-mortem brain tissue from schizophrenics shows a loss of PV-containing interneurons, with no effect on calbindin- or calretinin-containing interneurons in the frontal cortex (and hippocampus) (Beasley & Reynolds 1997, Beasley et al. 2002, Danos et al. 1998, Reynolds & Beasley 2001). Malfunctioning communication between pyramidal neurons and PV-containing interneurons has been proposed to also affect DA neurotransmission, linking the hyper-dopaminergic theory and the 6 NMDA hypofunction theory (Lisman et al. 2008). In fact, NMDAR antagonists have been shown to stimulate dopamine release in animal models (Pawlowski et al. 1990, Verma & Moghaddam 1996) suggesting that the hyper-dopaminergic state in schizophrenia is indeed a consequence of NMDA hypofunction (Grace 1991, Carlsson & Carlsson 1990), most likely originating in the hippocampus (Floresco et al. 2001, Legault et al. 2000), a brain region implicated in the manifestation of psychosis and deficits in working and short-term memory characteristic of schizophrenia (Lisman et al. 2008). NMDAR-mediated neurotoxicity and aberrant behaviors in rodent models of schizophrenia Based on Olney’s hypothesis and clinical evidence linking deficits in NMDAR synaptic transmission and disinhibition or neurotransmission to the pathophysiology of schizophrenia (Mouri et al. 2007), the effects of acute and chronic PCP or MK-801 treatment has been extensively studied in the adult rat as an animal model of the disease (Andine et al. 1999, Hanania et al. 1999, Hargreaves & Cain 1995, Jentsch et al. 1997, Johnson et al. 1998, Moghaddam et al. 1997, Ogren & Goldstein 1994, Phillips et al. 2001). However, since symptoms of the disease do not typically manifest in the human until late adolescence or early adulthood, many researchers, including those in this laboratory, investigate the effects of NMDAR blockade in developing rodents (Weinberger 1987, Ikonomidou et al. 1999, Wang et al. 2001, Wang & Johnson 2005). Neurodegeneration during early stages of brain development has been shown following PCP or MK-801 treatment in the cortex, hippocampus, and striatum, all of which are regions of the brain implicated in schizophrenia (Ikonomidou et al. 1999). In addition, acute PCP treatment on postnatal day (PN) 7, results in neurodegeneration (positive silver staining) in the frontal cortex, striatum, and hippocampus within 9 hours of treatment (Wang & Johnson 2005). This laboratory has also reported the presence of both non-specific 7 neurodegeneration (positive silver staining) and apoptotic neurons (terminal dUTP nick end labeling (TUNEL) positive) in the cortex, but not the in the striatum or hippocampus, following sub-chronic PCP administration on PN7, 9, & 11 (Wang et al. 2001, Wang & Johnson 2005), thereby suggesting either a developmental or pharmacological tolerance in these regions. Pretreatment with olanzapine was able to prevent the appearance of neurotoxic indices following sub-chronic postnatal PCP administration, suggesting that this treatment paradigm may model certain aspects of schizophrenia in rats (Wang et al. 2001) Schizophrenics have an impaired ability to filter external sensory information, a process known as sensorimotor gating (Bunney et al. 2000). Deficits in sensorimotor gating are thought to contribute to thought disorder and cognitive fragmentation characteristic of the disease (Braff & Geyer 1990). Prepulse inhibition (PPI) of acoustic startle response in animals is used as an animal model of sensorimotor gating. PPI of acoustic startle is a measure of the reduction of the startle response when a smaller non-startling acoustic stimulus (pre-pulse) is presented 80-120 ms prior to the startling stimulus (pulse) (Swerdlow et al. 1994). Acute PCP treatment produces an inhibition in PPI in adult rats, similar to that seen in schizophrenic patients (Martinez et al. 2000a). Typical antipsychotics, such as haloperidol, are not able to reverse deficits in PPI caused by acute PCP treatment in adult rats (Geyer et al. 2001) or in prepubertal rats (Martinez et al. 2002), but can reverse the effects of DA agonists, e.g. apomorphine. However, atypical antipsychotics, including clozapine, olanzapine, and quetiapine, are effective at alleviating acute PCP inhibition of PPI in adult rats (Geyer et al. 2001, Ballmaier et al. 2001, Martinez et al. 2002) as well as pre-pubescent rats (PN24-28, 10 mg/kg PCP on PN PN7, 9, & 11 (Wang et al. 2001), but not following acute PCP treatment to pups (PN16-19) or pre-pubertal (PN45) rats (Martinez et al. 2002). Additional behavioral consequences of acute PCP administration to adult rats include increases in locomotor activity, stereotypy, ataxia, circling, head8 weaving and walking backwards (Steinpreis 1996, Castellani & Adams 1981, Geyer & Ellenbroek 2003). In general, alterations in motoric behaviors such as these are thought to be mediated by DA and model the positive symptoms of schizophrenia, since they can be blocked by typical antipsychotics such as haloperidol (Geyer & Ellenbroek 2003, Steinpreis 1996). DA antagonists have been shown to inhibit PCP-induced locomotor activity, turning, and ataxia (Tsutsumi et al. 1995); more specifically, D1 and D2 receptors may play a role in acute PCP-induced hyperlocomotion, while only D2 receptors appear to regulate chronic PCP-induced hyperlocomotor activity (Phillips et al. 2001). Chronic administration of PCP to adult rats results in locomotor sensitization (Hanania et al. 1999, Johnson et al. 1998). Locomotor sensitization induced by chronic PCP can be inhibited by pretreatment with the atypical antipsychotic clozapine (Johnson et al. 1998), which possesses affinity for D2 and D4 receptors, 5-HT2, 5-HT3, 5-HT6 and 5-HT7 receptors, α1 noradrenergic receptors, muscarinic ACh receptors and histamine receptors (Lieberman 1993). Atropine, a selective muscarinic antagonist, was able to partially inhibit chronic PCP-induced locomotor sensitization; however, ketanserin, a 5-HT2A/2C receptor antagonist, had no effect (Phillips et al. 2001). These results suggest a regulatory role for ACh and DA in the manifestations of PCP-induced hyperlocomotor activity in adult rats. We have previously reported that sub-chronic PCP administration (PN7, 9, & 11) to developing rat pups can enhance locomotor activity and induce the development of locomotor sensitization following PCP challenge as well as deficits in PPI of acoustic startle (Anastasio & Johnson 2008a, Wang et al. 2001), both of which can be alleviated by treatment with atypical antipsychotics. Acute and repeated PCP treatment, but not amphetamine, of rats also results in deficits in social interaction (a hallmark of the negative symptoms of schizophrenia) and cognitive deficits as measured by the social interaction test and delayed spatial alternation task, respectively (Sams-Dodd 1999, Koros et al. 2007, Sams-Dodd 1998, Wang et al. 2001). Chronic treatment (21 days) with the atypical 9 antipsychotic, clozapine, but not the typical antipsychotic haloperidol reversed the PCP-induced deficits in social behavior (Sams-Dodd 1996). Deficits in selective attention and information processing, i.e. the inability to differentiate relevant from irrelevant information is an additional debilitating negative symptom of schizophrenia (Goldberg & Gold 1995). Acute PCP administration to adult rats has been reported to produce a reduced novelty discrimination index [time spent investigating the familiar juvenile compared to time spent investigating novel juvenile] (Terranova et al. 2005). Further, adult rats which received PCP during the perinatal stage (PN7, 9, & 11) also present with a deficit in the novelty discrimination index (Depoortere et al. 2005, Terranova et al. 2005, Harich et al. 2007a). These deficits could be reversed with the atypical antipsychotic clozapine (Terranova et al. 2005), supporting this behavior model as a suitable model of the attention processing deficits present in schizophrenia. Several studies from this laboratory have investigated the possible mechanisms by which PCP may elicit its neurotoxic effects and produce alterations in behavior in rats, specifically by measuring the effects of PCP on the expression of the NMDAR. The NMDAR is composed of multiple subunits including NR1, NR2A-D and NR3A/B; a functional receptor is typically composed of a NR1 subunit with one of the four NR2 subunits, forming a heterotetrameric complex. The NR1/NR2 complex differs in regard to its regional pattern of expression in the brain, its regulation by phosphorylation, proteases, polyamines or protons, its electrophysiological and functional properties, and its affinity for cytoskeletal post-synaptic density proteins (Paoletti & Neyton 2007, Kohr 2006, Waxman & Lynch 2005, Westbrook et al. 1997, Cull-Candy et al. 2001). Each subunit of the NMDAR contains an extracellular N-terminal region, three membrane spanning domains, one intramembrane loop and an intracellular Cterminal region. The C-terminal region of the NR2 subunit serves as a binding site for intracellular anchoring and trafficking proteins such as post-synaptic density 95 (PSD-95), synapse associated protein 102 (SAP102), and synapse 10 associated protein 97 (SAP97) and also links second messenger cascades to the NMDAR, thereby modulating the interaction of the receptor with various intracellular signaling cascades (Niethammer et al. 1996, Bi et al. 1998b, Wechsler & Teichberg 1998, Wu & Lynch 2006, Bi et al. 1998a, Guttmann et al. 2001, Guttmann et al. 2002, Zheng et al. 1999). Chronic PCP treatment of adult rats (20 mg/kg x 5 days) resulted in increases in the NMDAR subunit NR1 mRNA in the olfactory tubercle, piriform cortex, frontal cortex and anterior striatum (Wang et al. 1999). In addition, this treatment of adult rats also produced locomotor sensitization that was accompanied by an increase in NMDA-induced release of striatal 14C-GABA and 3H-ACh, which was correlated with an increase in NR1 immunoreactivity, suggesting that alterations in NMDAR function in the striatum may underlie PCP-induced locomotor sensitization (Hanania & Johnson 1999). In developing rats, sub-chronic PCP treatment of pups on PN7, 9, & 11 resulted in increased expression of NR1 mRNA in the frontal cortex, striatum, nucleus accumbens and olfactory cortex that was inhibited by pretreatment with the atypical antipsychotic olanzapine (Wang et al. 2001). This confirmed that increases in NR1 protein levels in the frontal cortex of PCP-treated pups coincided with increases in NR1 protein that was observed in PCP-treated adult rats (Hanania et al. 1999). Up-regulation of NR1 protein in the frontal cortex caused by sub-chronic PCP administration was associated with increases in TUNEL positive cells as well as an increase in the Bax (pro-apoptotic protein) to Bcl-XL (anti-apoptotic protein) ratio, both of which were inhibited by olanzapine pretreatment (Wang et al. 2001). These results parallel studies using 3H-MK-801 binding to show increases in NMDAR density (McDonald et al. 1990b, Gao & Tamminga 1994) as well as studies showing the delayed occurrence of cortical and striatal neurotoxicity induced by MK-801 or PCP (Ikonomidou et al. 1999, Wang et al. 2001, Wang & Johnson 2005). The exact mechanisms underlying the regulation of the NMDAR following acute or sub-chronic PCP administration 11 and the relationship between neurotoxicity have yet to be established and merit further investigation. The overall purpose of the present study was to characterize the regulation, function, and localization of NMDAR subunits (NR1, NR2A, and NR2B) following both acute (PN7) and sub-chronic (PN7, 9, & 11) PCP treatment in order to gain insight into the mechanism of neurotoxicity and the behavioral alterations caused by perinatal PCP administration in a developmental animal model of schizophrenia. The following hypotheses were addressed: Hypothesis 1: Differential regulation of NR1 and NR2 subunits in the frontal cortex following acute or sub-chronic PCP administration results from differences in synthesis and/or intracellular trafficking of the subunits. NMDA antagonists including PCP, MK-801 and ethanol have been shown to regulate the membrane expression levels of the NMDAR through changes in protein synthesis or trafficking of the NMDAR complex from intracellular compartments to the membrane (Dong et al. 2004, Sircar et al. 1996, Suvarna et al. 2005, Wenthold et al. 2003). Alterations in the trafficking of the NMDAR have been hypothesized to be dependent on its interactions with members of the post synaptic complex, specifically PSD-95 (Yamada et al. 1999b, Suvarna et al. 2005, Lu et al. 2000, Dong et al. 2004). PSD-95 plays a major role in the cell surface expression of assembled NR1/NR2 receptor complexes by anchoring the functional NR1/NR2 complex to the membrane through its interactions with the terminal four amino acid residues of the NR2 subunit (Wenthold et al. 2003, Yamada et al. 1999b). It has also been reported that MK-801 treatment to neonatal rats increases mRNA levels of NR1, NR2A, and NR2D mRNA in the frontal cortex and striatum (Sircar et al. 1996, Wilson et al. 1998). Sub-chronic PCP administration has been shown to result in the nuclear translocation of the transcription factor NF-κB (Wang et al. 2001), which has been shown to lead to 12 the up-regulation of the NR1 promotor and subsequent transcription of the gene (Liu et al. 2004a). My previous studies reported that acute PCP treatment increased membrane levels of NR1 and NR2B protein in the frontal cortex, while no effect on NR2A levels was detected. Furthermore, NR1 and NR2B protein levels in the endoplasmic reticulum (ER) fraction were decreased by acute PCP, suggesting an increased trafficking of NR1/NR2B from the ER to the membrane. Pretreatment with various antipsychotics had no effect on changes in protein expression induced by acute PCP. On the other hand, sub-chronic PCP treatment caused an increase in NR1 and NR2A expression in both the ER and membrane fractions of the frontal cortex, while no effect on NR2B expression was measured in either fraction. The increase in NR1/NR2A in the membrane fraction was blocked by pretreatment with antipsychotics. Therefore, I proposed to determine the mechanisms underlying the differences between acute and subchronic PCP-induced regulation of the NMDAR by assessing the synthesis and trafficking of NR1, NR2A, and NR2B subunits in the frontal cortex and striatum in vivo as well as the role of DA and 5-HT systems in regulation of the NMDAR. Specific Aim 1a Preliminary data shows that acute and sub-chronic PCP administration results in modest increases in the mRNA of NR1, NR2A, or NR2B in the frontal cortex 24 hrs later; however, these changes are not well correlated with the protein expression levels measured at this time point. It has been suggested that mRNA may be a poor indicator of protein levels, since expression of protein is not only dependent on transcription of the gene, but also nuclear export of mRNA, mRNA stability, translational regulation and protein degradation/turnover (Pradet-Balade et al. 2001). Thus, to address this concern we will use a protein synthesis inhibitor, cycloheximide (CHX), in order to clarify the role of protein synthesis in PCP-mediated regulation of the NMDAR subunits. CHX is a broad 13 protein synthesis inhibitor whose mechanism of action involves the reduction of the elongation rate via an eEF2-independent mechanism (Liu et al. 1997). To determine the role of protein synthesis in acute and sub-chronic PCP-induced regulation of the NMDAR, we will measure the protein expression levels of membrane bound NMDAR subunits in the presence and absence of the protein synthesis inhibitor, CHX following PCP administration. Specific Aim 1b Alterations in the trafficking of the NMDAR from intracellular compartments to the membrane are suggested to be mediated through activation of the calcium-dependent neutral cysteine protease, calpain (Dong et al. 2004, Yamashima 2004).To establish the role of calpain-mediated cleavage and trafficking of the NMDAR from intracellular compartments to the membrane, tissue from the frontal cortex of acute and sub-chronic PCP treated animals will be collected and the expression of α-II spectrin (a member of the post-synaptic density that is enzymatically cleaved directly by calpain) and its calpain specific breakdown products (SBP) which migrates at 145 and 150 kDa. In addition, to further clarify the role of calpain in the trafficking of the NMDAR, we will utilize MDL28170, a selective calpain inhibitor, following acute or sub-chronic PCP administration, and measure the membrane expression levels of NR1, NR2A, and NR2B in the frontal cortex and striatum. MDL28170 is a potent calpain inhibitor (Ki=10 nM in vitro) that has been shown to cross the blood brain barrier following systemic administration (Li et al. 1998). Hypothesis 2: Up-regulation of the NMDAR in the frontal cortex by either acute or sub-chronic PCP treatment of perinatal rats results in a hyperfunctional receptor and is dependent on the subunit composition of the receptor. 14 The consequences of PCP-induced neurotoxicity are multifaceted and may involve various compensatory mechanisms, including but not limited to altering the synaptic expression levels and functional properties of the NMDAR. It has been reported that postnatal PCP administration (1 and 5 mg/kg on PN515) increased membrane expression levels of the NMDAR as well as maximal 3H-MK-801 binding in the frontal cortex (Sircar 2003). The exact mechanisms underlying the differential regulation of the NMDAR following acute or subchronic PCP administration and the relationship between NMDAR density and function are unknown in this animal model of schizophrenia; therefore, the present study seeks to determine whether the apparent treatment dependent upregulation of the NMDAR subunits corresponds to an increase in its functionality using a 3H-MK-801 binding assay. Glutamate and glycine, which promote opening and activation of the NMDA channel, stimulate radioligand binding in a well washed membrane preparation, and inhibition by noncompetitive NMDAR antagonists is dependent on the presence of both agonists (Johnson et al. 1989, MacDonald et al. 1987). Further, MK-801 binds deep within the NMDAR channel and binding is influenced by the open state of the channel; therefore, it is possible to study the regulation and function of the NMDAR by measuring the binding of radiolabeled MK-801(Johnson et al. 1989). Specific Aim 2 The functionality of the NMDAR following both acute and sub-chronic PCP treatment will be determined in the frontal cortex by assessing NMDA- and glycine-dependent activation of 3H-MK-801 binding. Preliminary data suggest that in the frontal cortex acute PCP treatment selectively affects the NR1/NR2B complex, while the NR1/NR2A complex appears to be sensitive to sub-chronic PCP treatment (Anastasio & Johnson 2008b). Thus, it is anticipated that the sensitivity of 3H-MK-801 binding to NR2A and NR2B selective antagonists such 15 as NVP-AAM077 and ifenprodil, respectively, will be altered following either acute or sub-chronic PCP treatment. Hypothesis 3: Neuroprotection from PCP administration is mediated through activation of NR1/NR2A receptors (synaptic) while PCP-induced neurotoxicity is dependent on blockade of NR1/NR2B receptors (extrasynaptic), suggesting that localization of NMDA NR2A and NR2B receptors may dictate different neurotoxic functions in response to PCP. The subunit composition of the NMDAR that mediates PCP-induced neuronal neurotoxicity is currently unknown. Work from the Bading laboratory has proposed that activation of synaptic NMDARs lead to neuronal survival while activation of extrasynaptic receptors may lead to neuronal death (Hardingham et al. 2002). The subunit composition of synaptic and extrasynaptic NMDARs is not entirely clear and may depend on the stage of development. Early in development, NR2B receptors dominate in expression compared to NR2A, but a “switch” occurs later in development and NR2A are then expressed at a higher level. However, this switch does not rule out the role of NR2B receptors in either synaptic or extrasynaptic transmission. Recent work from our laboratory suggests that activation of synaptic receptors, which are thought to be NR1/NR2A, protects neurons from PCP-induced neurotoxicity (Lei et al. 2008). Further, we have hypothesized that aberrant behaviors induced by PCP are due to its neurotoxic effects; therefore, the purpose of this study is to show a relationship between NR2-blockade mediated neurotoxicity and development of locomotor sensitization. Specific Aim 3a We plan to investigate the role of synaptic and extrasynaptic NMDARs in PCP-induced neurotoxicity in vitro and in vivo. Selective antagonists at various doses for NR2A (NVP-AAM007 and PEAQX) and NR2B (ifenprodil) will be 16 administered to organotypic corticostriatal slice cultures as well as developing rat pups and apoptosis estimated by measurement of caspase-3 enzymatic activity and histochemical assessment of terminal dUTP nick-end labeling (TUNEL) of apoptotic neurons. Specific Aim 3b The membrane associated guanylate kinase (MAGUK) family of proteins includes PSD-95 (post-synaptic density 95), SAP102 (synapse associated protein 102), and SAP97 (synapse associated protein 97). PSD-95 is thought to bind to the PDZ domain in the C-terminal region of synaptic NR2A or NR2B subunits (Lu et al. 2000, Wu et al. 2007), while SAP102 is linked to NR2B subunits either in the synaptic or extrasynaptic space (Wu et al. 2007, Sans et al. 2003) To determine the differential “synaptic” localization of NR2A and NR2B following either acute or sub-chronic PCP administration in vivo, we will perform immunoprecipitation studies in washed cortical synaptic membranes and crude membrane fractions from animals treated with PCP on PN7 (acute studies) or on PN7, 9, & 11 (sub-chronic studies). First, we will determine the composition of the NMDAR (NR1+NR2A and/or NR2B) via pull down assays. determine the synaptic localization of the NR2 In order to subunits we will immunoprecipitate PSD-95 or SAP102 and then immunoblot with anti-NR1, antiNR2A, anti-NR2B, or anti-actin. To confirm our results, we will pull-down with NR2A or NR2B and immunoblot for actin, NR1, PSD-95 or SAP102. Specific Aim 3c So as to determine the effects of blockade of NR2 subunits on the development of locomotor sensitization and establish a relationship between neurotoxicity and development of this behavioral phenomenon, animals will be treated either acutely or sub-chronically with saline, PCP, PEAQX (NR2Apreferring antagonist) or ifenprodil (NR2B-selective antagonist) on PN7, 9, & 11, 17 allowed to develop and locomotor activity measured following challenge with either PCP, PEAQX, or ifenprodil on PN28-35. Hypothesis 4: Sub-chronic PCP administration to developing rats will induce locomotor sensitization in response to PCP challenge, deficits in PPI of acoustic startle as well as deficits in social interaction and social discrimination, thereby mimicking multiple symptoms of schizophrenia. PCP intoxication in humans has been shown to mimic both the positive and negative symptoms of schizophrenia as well as exacerbate psychosis in schizophrenics. In general, alterations in motoric behaviors are thought to model the positive symptoms of schizophrenia. Further, PCP disrupts PPI of acoustic startle in animals and is routinely used to model the sensorimotor gating deficits of schizophrenia (Geyer et al. 2001, Rasmussen et al. 2007). Hypofunction in the prefrontal cortex is thought to underlie the origins of the negative symptoms of the disease (Goff & Evins 1998). Clinical observations have shown that PCP intoxicated humans repeatedly present with symptoms which mimic several negative symptoms of schizophrenia, including social withdrawal. There is a paucity of studies investigating the PCP perinatal model and its ability to mimic the negative symptoms of schizophrenia. Therefore, in this study we sought to determine the effect of PN7 and PN7, 9, 11 PCP administration on multiple behaviors thought to model different aspects of schizophrenia; specifically locomotor sensitization, PPI of acoustic startle, social interaction as well as its effect on social discrimination. Specific Aim 4a Measurement of PPI of acoustic startle will performed according to previously published procedures with minor modifications (Wang et al. 2001, Wang et al. 2003). Animals will be treated on PN7 or PN7, 9, & 11 with PCP, allowed to age and PPI measured on PN24-26. 18 The ability of atypical antipsychotics to prevent the PCP-induced deficits in PPI will also be determined. Repeated PCP administration causes a progressive augmentation of locomotor activity (Xu & Domino 1994), referred to as sensitization. Sensitization is also thought to be an important index related to psychosis as well as movement and thought disorders in schizophrenia (Robbins 1990); therefore, we will determine if acute or sub-chronic PCP administration results in locomotor sensitization as well as the effects of atypical antipsychotics (e.g. olanzapine and risperidone) to prevent it. Specific Aim 4b Social interaction is best defined as the time a pair of animals spend in an active social interaction (sniffing and grooming its partner, close following, mounting and crawling over or under its partner) with or without direct physical contact (Mouri et al. 2007). Male and female Sprague-Dawley rat pups will be treated on PN 7, 9, and 11 with PCP and then tested for deficits in social interaction on PN28-29 (pre-pubescent) and PN54 (post-pubescent). Deficits in social novelty discrimination, i.e. the inability of an adult rat to discriminate between a familiar and a novel juvenile, is thought to serve as a suitable animal model of the selective attention processing deficits characteristic of schizophrenia (Engelmann et al. 1995). Animals will be treated on PN7, 9, & 11 with saline or PCP allowed to age and tested as adults on PN58-60. The time of investigative behavior of or by the adult (anogenital exploration, sniffing with direct contact, crawling over each other, grooming, play behaviors) towards each of the two juveniles will be recorded. The time spent investigating the familiar juvenile divided by the time spent investigating the novel juvenile is defined as the novelty discrimination index. 19 Chapter 2: NR2A-Containing Synaptic NMDARs Mediate PCP-Induced Cortical Neurotoxicity and the Subsequent Development of Schizophrenia-like Behaviors The relationship between PCP-induced neurotoxicity in perinatal rats and the development of schizophrenic-like behaviors is uncertain, as is the role of NMDAR subunits in both. We used antagonists selective for NR2A- and NR2Bcontaining NMDARs to test the hypothesis that the behavioral and neurotoxic effects of PCP are mediated by blockade of synaptic NMDARs which are thought to predominantly consist of NR1/NR2A subunits, rather than NR1/NR2B subunits. Sprague-Dawley rats were treated on PN7 (acute) or on PN7, 9, & 11 (subchronic) with PCP (10 mg/kg), PEAQX (selective NR2A antagonist, 10, 20, or 40 mg/kg, s.c.), or ifenprodil (selective NR2B antagonists, 1, 5, or 10 mg/kg, s.c.) and sacrificed to measure caspase-3 activity as an index of apoptosis or allowed to age and tested for locomotor sensitization to PCP challenge on PN2835. PCP or PEAQX on both PN7 and PN7, 9, & 11 markedly elevated caspase-3 activity in the cortex while ifenprodil showed no effect. Striatal neurotoxicity was evident after treatment with PCP or PEAQX on PN7 or only after sub-chronic treatment with a high dose of PEAQX (20 mg/kg). Animals treated with PCP or PEAQX on PN7, 9 and 11 showed a sensitized locomotor response to PCP challenge on PN28-35. Ifenprodil treatment had no effect on either measure. Therefore, PCP blockade of cortical synaptic NR1/NR2A, rather than NR1/NR2B, appears to be responsible for PCP-induced neurotoxicity and the development of long-lasting behavioral deficits. Introduction NMDAR antagonists including PCP and ketamine are drugs of abuse that induce amnesia, delirium, and schizophrenia-like symptoms (Luby et al. 1962, Javitt & Zukin 1991). PCP is thought to be one of the most dangerous drugs of 20 abuse; depending on the dose administered it can act as a hallucinogen, stimulant, depressant and/or anesthetic. In addition to the psychotomimetic symptoms produced by PCP, several parallels exist between the effects of PCP administration and schizophrenia, specifically altered cerebral blood flow, glucose utilization and neurotoxicity in brain regions including, but not limited to the frontal cortex, striatum, and hippocampus all of which are thought to be afflicted in schizophrenics (Olney et al. 1989a, Olney & Farber 1995b, Strous & Javitt 1996). The similarities between PCP-induced neurotoxicity in animals and its ability to mimic schizophrenia led to the hypo-glutamatergic hypothesis of schizophrenia (Olney & Farber 1995a). PCP is an open channel blocker of NMDA receptors, binding within the channel pore in a voltage and use dependent manner (Honey et al. 1985, MacDonald et al. 1987, Johnson & Jones 1990). The NMDAR is a voltage-gated channel and member of the glutamate family of excitatory neurotransmitters, which is activated following binding of glutamate and the co-agonist glycine and is permeable to Ca2+ and is chiefly localized to the postsynaptic neuronal membrane. The NMDAR is primarily a heterodimeric complex formed by the combination of two of the obligatory NR1 subunits and two of the four NR2 subunits (A-D) and less commonly, it is also known to form a heterotrimeric complex including NR1, NR2A and NR2B (Kutsuwada et al. 1992, Kohr 2006, Cull-Candy et al. 2001). The composition of the NMDAR complex varies in distribution and possesses unique pharmacological and physiological properties in the brain (Lynch & Guttmann 2001, Cull-Candy et al. 2001). During early postnatal development of the rat, NMDARs are the principal mediator of glutamatergic neurotransmission and are also highly responsive to over-stimulation resulting in excitotoxic neuronal death (Ben-Ari et al. 1997). Extensive evidence indicates that activation of synaptic NMDARs [predominantly NR1/NR2A (Tovar & Westbrook 1999, Cull-Candy et al. 2001)] promote neuronal survival through increased synaptic function and Ca2+ entry leading to activation 21 of the CREB pathway. However, activation of extrasynaptic receptors [predominantly NR1/NR2B (Cull-Candy et al. 2001, Tovar & Westbrook 1999)] leads to neuronal death by shutoff of the pro-survival CREB pathway as well as inactivation of activated ERK and its downstream signaling partners (Soriano & Hardingham 2007, Hardingham et al. 2002, Hardingham & Bading 2002, Ivanov et al. 2006). Although acute blockade of NMDA receptors by MK-801 or PCP results in wide-spread neurotoxicity (Ikonomidou et al. 1999), this laboratory has reported that subchronic PCP treatment of perinatal rats on PN7, 9 and 11 results in a cumulative apoptosis in the frontal cortex (Wang & Johnson 2007, Wang & Johnson 2005, Wang et al. 2001) that is associated with long-lasting behavioral deficits that resemble certain aspects of schizophrenic-like behaviors (Anastasio & Johnson 2008a, Wang et al. 2001). For example, this treatment caused an olanzapine-sensitive deficit in pre-pulse inhibition (PPI) of acoustic startle as measured on PN24-26, as well as a sensitized locomotor response to low-dose PCP (4 mg/kg) measured on PN28-35 (Anastasio & Johnson 2008a). These studies help to establish the validity of perinatal neurodegeneration induced by PCP along with its behavioral sequelae as a potential animal model of schizophrenia. However, the means by which PCP causes neurodegeneration is not completely understood, nor is the relationship between neurotoxicity and the development of abnormal behaviors later in life. The primary goal of this study was to determine whether PCP-induced neurotoxicity and its detrimental behavioral effects could be attributed to blockade of either synaptic or extrasynaptic NMDA receptors. Since NR2A receptors are thought to be localized predominantly in the synapse and NR2B receptors are believed to be mostly extrasynaptic (Cull-Candy et al. 2001), we proposed that if PCP-induced neurodegeneration and behavioral deficits were the consequence of blockade of synaptic, rather than extrasynaptic NMDA receptors, then the effects of PCP would be mimicked by the NR2A antagonists 22 NVP-AAM007 and PEAQX (Feng et al. 2004), but not by the NR2B antagonist, ifenprodil (Williams 2001). To this end, we compared the effects of PEAQX, or its stereomer NVP-AAM007 (Auberson et al. 2002) and ifenprodil to PCP treatment in measures of apoptosis (both in organotypic corticostriatal slices and in vivo) and the development of locomotor sensitization to PCP challenge on PN28-35. The results of these experiments allow us to propose that neurotoxicity and the subsequent alterations in early adolescence behavior that results from PCP administration during a critical stage of brain development in the rat is predominantly due to blockade of synaptic NR2A-containing, rather than NR2Bcontaining receptors. Materials and Methods Animals. Timed, day 14 pregnant female Sprague-Dawley rats were obtained from Charles River Laboratories (Wilmington, MA). The dams were housed individually with a regular 12h light-dark cycle (lights on 0700, off at 1900) with food and water ad libitum. Following parturition, male and female pups from four dams were combined and randomly cross-fostered to one of the four lactating dams. Each litter consisted of ten to twelve pups. On postnatal (PN) day 2.5, some animals were sacrificed by decapitation and their brains used for organotypic brain slice culture. Other pups were treated on PN7 or on PN7, 9 and 11 and killed by decapitation in experiments described below or allowed to age and used for behavioral studies. All experiments were conducted in accordance with NIH regulations and with approval of the University of Texas Medical Branch at Galveston Institutional Animal Care and Use Committee. Drugs. PCP was acquired from the National Institute on Drug Abuse (NIDA, Rockville, MD) and dissolved in 0.9% NaCl. NVP-AAM007 was a generous gift 23 provided to us by Dr. Yves Auberson (Novartis Institute for Biomedical Research, Basel, Switzerland). [[[(1S)-1-(4-Bromophenyl) ethyl] amino] (1, 2, 3, 4- tetrahydro-2, 3-dioxo-5-quinoxalinyl) methyl] phosphonic acid tetrasodium hydrate (PEAQX) and ifenprodil (+)-tartrate salt were purchased from SigmaAldrich (St. Louis, MO) and dissolved in 0.9% NaCl. Doses were chosen based on our own work with these compounds as well as the published ED50 values. Organotypic slice culture. Corticostriatal slice cultures were prepared as previously prescribed (Xia et al. 2008) In brief, 2.5 day-old rat pups were sacrificed by decapitation. The brains were removed quickly and cut into 400-μm-thick coronal sections by a McIlwain tissue chopper under sterile conditions. Three adjacent frontal corticostriatal slices with morphology comparable to levels between A5.3 and A6.8 mm in P10 rats (Sherwood & Timiras 1970) were placed and cultured in inserts with a porous and translucent membrane (Culture Plate Insert, MILLIPORE Co, Bedford, MA) at the interface between medium and CO 2enriched atmosphere. The initial culture medium was a mixture of 25% inactivated horse serum, 25% Hank's balanced salt solution, and 50% OPTIMEM culture medium, supplemented with 25 mM D-glucose and 1% penicillin/streptomycin. On DIV 3, the medium was switched to serum-free Neurobasal medium supplemented with 25 mM D-glucose, 1 mM glutamine, 2% B-27, and 1% penicillin/streptomycin. The medium was changed twice a week thereafter. Slices were used in experiments on DIV9. In vivo experimental design. Male and female rat pups were treated on PN 7 (acute) or on PN 7, 9, and 11 (sub-chronic) with 10 mg/kg PCP (s.c.), 10, 20 or 40 mg/kg PEAQX (s.c.), 10 mg/kg NVP-AAM007 (s.c.), or 1, 5, or 10 mg/kg ifenprodil (i.p.). For the neurotoxicity studies, animals were sacrificed and the brains were processed for 24 measurement of caspase-3 activity as described below. For the behavioral studies, animals were assessed for locomotor sensitization in response to PCP challenge (4 mg/kg, i.p.) on PN28-35. Terminal dUTP Nick-End Labeling (TUNEL). Slices used for TUNEL labeling were collected 12 hours [(time of peak cell death in the slice (Wang & Johnson 2007)] after PCP treatment. Slices were first rinsed with 0.01 M PBS (pH 7.2) and then fixed with ice-cold 2% paraformaldehyde in 0.1 M PBS (pH 7.2) at room temperature for 1 hour. After washing with 0.01M PBS (pH 7.2), slices were dehydrated and rehydrated in ethanol (70%, 90%, 100%, 90%, 70%, PBS), incubated with pepsin (0.04% in 10 mM HCl) for 15 min followed by quenching of endogenous peroxidase with 3.0% hydrogen peroxide in methanol for 10 min. After washing with PBS and pre-incubation with TdT (terminal deoxynucleotidyl transferase) reaction buffer (30 mM Tris-HCl, pH 7.2, 140 mM Na cacodylate and 1 mM CoCl2) for 15 min, slices were incubated with biotin-16-dUTP (10 nmoles/ml) and TdT (200 U/ml) in the TdT buffer in a humidified chamber for 2 hours at 37°C. Slices were then washed in PBS, incubated with the Vectastain ABC reagents for 60 min and stained with a filtered mixture of Vector SG peroxidase substrate. Caspase-3 Activity. Organotypic slice samples used for caspase-3 activity measurement were always collected 12 hours after PCP treatment; in vivo samples were collected 8 hrs [peak time point for PCP-induced caspase-3 activation in the frontal cortex and striatum (Wang & Johnson 2007, Wang & Johnson 2005)] after the injection on PN7 or 8 hrs after the last of the three injections on PN7, 9, & 11. Measurement of caspase-3 activity was carried out as previously described (Wang & Johnson 2007). Briefly, samples were sonicated in ice-cold lysis buffer containing 25 mM HEPES (pH 7.4), 5 mM MgCl2, 1.5 mM EDTA, 1.0 mM EGTA, 1 mM DTT, 0.1% Triton X-100 25 and 1% protease inhibitor cocktail. After cooling on ice for 15 min, the sonicates were centrifuged at 13,000 x g for 5 min at 4°C. The supernatants were then collected for measurement of caspase-3 activity. Protein concentration was measured by using a bicinchoninic acid protein assay kit (Pierce, Rockford, IL). To measure the enzyme activity, each sample was prepared in two parallel sets. One set consisted of an equal volume of supernatant and assay buffer (100 mM HEPES, pH 7.4, containing 2 mM dithiothreitol, 0.1% CHAPS, and 1% sucrose). The other set was a mix of equal volume of the same supernatant and assay buffer containing the selective caspase-3 inhibitor, Z-DEVD-FMK (0.5 µM). After incubation at room temperature for 15 min, the caspase-3 substrate, Ac-DEVD-AFC (25 µM), was added and the samples were then incubated at 37°C for 60 min. Fluorescence resulting from cleavage of the substrate was measured using a microplate fluorometer (Fluoroskan Ascent, Labsystems, Helsinki, Finland) at excitation and emission wavelengths of 405 and 510 nm, respectively. 7-Amino-4-trifluoromethylcumarin (AFC) was used as a fluorescent standard. Caspase-3 activity was calculated as the difference of enzyme activities in samples incubated without and with the caspase-3 inhibitor and then normalized to the total protein concentration. Co-Immunoprecipitation and Western Blotting. Crude synaptosomal protein extracts were prepared from 2 mm sections corresponding to 4.7 to 2.7 mm anterior to Bregma for the frontal cortex and 0.7 mm to -1.3 mm for the striatum as previously described (Anastasio & Johnson 2008b) with minor modifications Brain sections were homogenized (10 times w/v) in ice cold Krebs-sucrose solution (125 mM NaCl, 1.2 mM KCl, 1.2 mM MgSO4, 1.2 mM CaCl2, 22 mM Na2CO3, 1 mM NaH2PO4, 10 mM glucose, 0.32 M sucrose). Just prior to use, a protease inhibitor cocktail, consisting of 4-(2aminoethyl) benzenesulfonyl fluoride (AEBSF), pepstatin A, E-64, bestatin, leupeptin, and aprotinin without metal chelators (Sigma-Aldrich, St Louis, MO) at a concentration of 10 μL/mL was added to the lysis buffer. The homogenate was 26 then centrifuged at 1000 x g at 4oC. The supernatant (S1) was collected and centrifuged at 16,000 x g at 4oC for 20 minutes to pellet the crude synaptosomes; the resultant pellet was re-suspended in buffer and stored at -80oC. Total protein concentrations were determined using the BCA (bicinchoninic acid) protein assay© (Pierce Chemical, Rockford, IL). In immunoprecipitation experiments, 100 µg membrane protein was incubated with antibodies (2 µg) against PSD-95, SAP102, NR2A, or NR2B and the immune complexes were collected with 50 µl of protein A/G–Sepharose beads (gently shaken overnight at 4°C). Immunoprecipitates were then washed 3 times with ice-cold PBS, and resuspended in 2x Laemmli sample buffer, incubated in 90 0C water for 5 min, and centrifuged at 15,000 x g for 1 min. The supernatant was subjected to SDSPAGE and transferred to polyvinylidene difluoride (PVDF) membranes (0.2 μm) in a Mini Electrotransfer Unit (Bio-Rad, Hercules, CA) overnight. The blotting was performed by repeated stripping and reprobing with anti-NR1, anti-NR2A, anti-NR2B, anti-PSD-95, and anti-SAP102. Analysis was carried out using enhanced chemiluminescence (ECL) plus Western blotting detection reagents (Amersham Biosciences, Piscataway, NJ). The bands corresponding to the various proteins of interest were scanned and densitometrically analyzed by using an automatic imaging analysis system (Alpha Innotech Corporation, San Leandro, CA). All quantitative analyses were normalized to β-actin (after stripping [Reblot mild, Chemicon International, Temecula, CA]). Antibodies. Monoclonal anti-NR1, anti-NR2A, and anti-NR2B antibodies were purchased from BD Biosciences (San Jose, CA). Monoclonal anti-PSD-95 and anti-SAP102 were purchased from Cell Signaling (Danvers, MA). Primary antibody dilution was 1:500-1:1000. Secondary antibodies were purchased from Zymed (Invitrogen Corporation, Carlsbad, CA) and used at a concentration of 1:5000. 27 Locomotor Activity. On the day of testing, animals were placed in locomotor activity chambers and allowed to habituate for 30 minutes prior to a challenge dose of PCP (4 mg/kg, i.p.), PEAQX (4 mg/kg, i.p.) or ifenprodil (5 mg/kg, i.p.). Locomotor activity was measured for an additional 90 minutes in an open-field activity system (San Diego Instruments, San Diego, CA) which consisted of a square enclosure with Plexiglas walls (40 x 40 x 40 cm). Horizontal activity was measured with a 4 x 4 photobeam matrix which recorded both central and peripheral activity in 5 min bins as previously described (Anastasio & Johnson 2008a). Statistical Analysis. Group comparisons were specifically defined before the beginning of each experiment; therefore, planned comparisons were performed instead of an overall F test in a multifactorial ANOVA (Keppel 1982). Statistical comparisons for each biochemical and for locomotor sensitization experiments were conducted using a one-way ANOVA. All values are presented as mean ± SEM. The null hypothesis was rejected at p<0.05. Results Inasmuch as this laboratory has previously characterized PCP-induced neurotoxicity in the corticostriatal slice culture (Wang & Johnson 2005, Xia et al. 2008) we decided to build on these studies and to investigate which NMDAR subunit may mediate cell death. Organotypic brain slices can serve as an in vitro model that conserves the biologically relevant structural and functional features of in vivo tissues (Vickers & Fisher 2004), while also allowing easier manipulation of drugs than possible in vivo. PCP (3 µM) and the NR2A antagonist NVPAAM007 (100 nM, 1µM, and 10 µM) caused robust TUNEL-positive staining compared to control (Figure 2.1). No apoptosis was evident in slices treated 28 with 100 nM, 1 µM, or 10 µM ifenprodil (Figure 2.1). Measurement of caspase-3 activity also showed that 3 µM PCP and 3 µM PEAQX produced similar caspase3 activation, while NVP-AAM007 was approximately three-fold more potent (Figure 2.2). Ifenprodil had no effect on caspase-3 activity in the slice culture (Figure 2.2). As previously reported, PCP (10 mg/kg) treatment on either PN7 or on PN7, 9, & 11 results in robust caspase-3 activation in the frontal cortex (Figures 2.3 and 2.5, respectively) (Wang & Johnson 2007). NVP-AAM007 (10 mg/kg) also significantly increased cleaved caspase-3 compared to control (data not shown) and blockade of NR2A subunits with PEAQX dose dependently increased cortical caspase-3 activity following both acute (Figure 2.3) and subchronic administration (Figure 2.5). In contrast, as observed in vitro, blockade of NR2B subunits with ifenprodil on PN7 (Figure 2.3) or on PN7, 9, & 11 had no significant effect on cleavage of caspase-3 at 1, 5 or 10 mg/kg in the frontal cortex (Figure 2.5). PCP administration or PEAQX (20 mg/kg and 40 mg/kg) on PN7 resulted in a 6-8 fold increase in caspase-3 activity in the striatum, but no effect of ifenprodil was observed (Figure 2.4). Similarly, subchronic administration of 20 mg/kg PEAQX treatment on PN7, 9, & 11 caused an 8-fold increase in caspase-3 activity in the striatum, but no effect of PCP or ifenprodil was observed in this brain region (Figure 2.6). The highest dose of PEAQX (40 mg/kg) was toxic to the animals when administered on PN7, 9, & 11, i.e. 8 hrs after the third injection all of the pups had lost ~33% of their starting body weight suggesting a failure to thrive. 29 Figure 2.1. Representative photomicrographs showing TUNEL-positive staining in corticostriatal organotypic slice cultures. Cultures were treated on DIV 9 for 12 hrs with 3 μM PCP, various doses of NVP-AAM007, or various doses of ifenprodil. PCP and NVP-AAM007 dose dependently caused robust apoptosis compared to control; no cell death was evident in ifenprodil treated cultures. N=3/treatment 30 Figure 2.2. Effects of PCP administration on neurotoxicity in corticostriatal slice cultures. 3 μM PCP (DIV 9 for 12 hrs) to corticostriatal organotypic slice cultures activates caspase-3. NVP-AAM007 and PEAQX dose-dependently activate caspase-3 while ifenprodil does not. control (one-way ANOVA with Dunnett’s method) 31 N=5-7/treatment, *p<0.05 vs. PN7-Frontal Cortex Figure 2.3. Effects of neonatal PCP and selective NR2A and NR2B antagonists on frontal cortex neurotoxicity in PN7 rats. Sprague-Dawley rat pups were treated on PN7 with saline, 10 mg/kg PCP (s.c.), various doses of PEAQX (s.c.), or various doses of ifenprodil (i.p.). PCP and PEAQX resulted in caspase-3 activation in the frontal cortex 8 hrs after treatment. N=5-7/treatment, *p<0.05 vs. saline (one-way ANOVA with Holm-Sidak method) 32 PN7-Striatum Figure 2.4. Effects of neonatal PCP and selective NR2A and NR2B antagonists on striatal neurotoxicity in PN7 rats. Sprague-Dawley rat pups were treated on PN7 with saline, 10 mg/kg PCP (s.c.), various doses of PEAQX (s.c.), or various doses of ifenprodil (i.p.). PCP and PEAQX resulted in caspase-3 activation in the striatum 8 hrs after treatment. N=5-7/treatment, *p<0.05 vs. saline (one-way ANOVA with Holm-Sidak method) 33 PN7, 9, &11-Frontal Cortex Figure 2.5. Effects of neonatal PCP and selective NR2A and NR2B antagonists on frontal cortex neurotoxicity in young rats. Sprague-Dawley rat pups were treated on PN7, 9, & 11 with saline, 10 mg/kg PCP (s.c.), various doses of PEAQX (s.c.), or various doses of ifenprodil (i.p.). PCP and PEAQX resulted in caspase-3 activation in the frontal cortex 8 hrs after the last of 3 injections. N=5-7/treatment, *p<0.05 Bonferroni's post hoc test) 34 vs. saline (one-way ANOVA with PN7, 9, & 11-Striatum Figure 2.6. Effects of neonatal PCP and selective NR2A and NR2B antagonists on striatal neurotoxicity in young rats. Sprague-Dawley rat pups were treated on PN7, 9, & 11 with saline, 10 mg/kg PCP (s.c.), various doses of PEAQX (s.c.), or various doses of ifenprodil (i.p.). PCP and PEAQX resulted in caspase-3 activation in the striatum 8 hrs after the last of three injections. N=57/treatment,*p<0.05 vs. saline (one-way ANOVA with Holm-Sidak method) 35 Since, the sub-chronic paradigm more closely models the schizophrenic disease state (Anastasio & Johnson 2008a), this treatment paradigm was carried through for the remaining experiments in this study. In order to determine the subunit composition of synaptic and extrasynaptic NMDAR receptors following sub-chronic PCP administration, we took advantage of the predominately synaptic localization of PSD-95 and the extrasynaptic localization of SAP102 and performed co-immunoprecipitation (Sans et al. 2000, van Zundert et al. 2004). Quantification of these results indicate that PCP treatment on PN7, 9, & 11 increases the association of PSD-95 with NR2A, but not NR2B (Figure 2.7A). Sub-chronic PCP administration results in a significant increase in the association of both NR2A and NR2B with SAP102 in the cortical synaptosomal fraction (Figure 2.7B). To verify these results, reverse pull-down assays were performed by precipitating with the NR2 subunit antibodies and subsequent probing for PSD-95 and SAP102 with specific antibodies for these proteins. These experiments yielded results similar to those obtained above (data not shown). Further, to authenticate the presence of fully assembled and functional NMDARs, all membranes were probed for the obligatory NR1 subunit. The NR1 subunit was associated with NR2A and NR2B in both synaptic and extrasynaptic fractions (data not shown). 36 Figure 2.7. Effects of PCP administration on the localization of NR2A and NR2B in the synaptic or extrasynaptic milieu. Cortical crude synaptosomal extract (100 µg) from rat pups 8 hrs after treatment were incubated with 2 µg antibody against PSD-95 or SAP102. The blots were probed sequentially, after stripping, with antibodies against NR2A or NR2B. Quantified results indicate in A) PCP treatment on PN7, 9, & 11 increases the association of NR2A with PSD95. B) Sub-chronic PCP treatment results in an increase in the association of NR2A and NR2B with SAP102. Values shown are mean ± SEM n=4/treatment group, * p < 0.05 (Student’s t- test) 37 To better understand the relationship between PCP-induced neurotoxicity and the development of adverse behaviors in the rat, we extended our previous study (Anastasio & Johnson 2008a) and investigated the effects of selective NR2A and NR2B antagonists on the development of locomotor sensitization. Sub-chronic PCP and PEAQX (10 and 20 mg/kg) showed enhanced locomotor activity in response to PCP challenge (4 mg/kg) compared to saline pretreatment (F3, 73=4.99) (Figure 2.8A); however, pretreatment with either dose of ifenprodil (1 or 5 mg/kg) did not enhance the locomotor response to PCP challenge. The time courses of the locomotor responses to PCP challenge for all treatment groups are shown in Figure 2.8B. We did not determine the effects of 10 mg/kg ifenprodil in the behavior studies because the lower doses had no effect on cortical neurotoxicity or locomotor sensitization. The reciprocal locomotor sensitization experiments were also performed in order to determine whether blockade of either the NR2A or NR2B subunits alone can activate a sensitized locomotor response similar to PCP challenge. The effects of PEAQX or ifenprodil challenge on locomotor activity following treatment during development with either saline, PCP, PEAQX, or ifenprodil are shown in Figures 2.9A and 2.9C. Acute challenge with either PEAQX (4 mg/kg) (F2,23=2.098) or ifenprodil (5 mg/kg) (F2,32=1.342) on PN28-35 did not significantly increase locomotor activity in rats treated sub-chronically with either PCP, PEAQX or ifenprodil on PN7, 9 and 11. Similarly treated rats were also co-challenged with both PEAQX and ifenprodil on PN28-35 and no alterations in locomotor activity were observed (data not shown). 38 Figure 2.8. Locomotor sensitization induced by a 4 mg/kg PCP challenge to either sub-chronic PCP or PEAQX treated animals. Animals treated sub- chronically with ifenprodil do not show a sensitized response to PCP challenge. (left) Time course of locomotor activity (right) N=8-26/treatment group *p<0.05 vs. saline (one-way ANOVA with Holm-Sidak method) 39 Figure 2.9. Effect of selective blockade of NR2A and NR2B subunits on locomotor sensitization. Neither PEAQX nor ifenprodil challenge results in locomotor sensitization as measured on PN28-35 (A and C). The time course of locomotor activity is shown in panels B and D. N=8/treatment group. 40 Discussion Neither the mechanism of PCP-induced neurotoxicity in perinatal rats, nor the association between neurotoxicity and the development of behavioral deficits as the animal matures, is completely understood. Further, the role played by specific NMDAR subunits in either is undefined. Therefore, the focus of this study was to investigate the role of NR2A and NR2B receptors in PCP-induced neurotoxicity and the development of aberrant behaviors in the immature rat. Through a pharmacological approach, we discovered that administration of NR2A-preferring antagonists mimicked PCP-induced neurotoxicity in the frontal cortex, while administration of a selective NR2B antagonist had no effect. This strongly suggests that cortical neurotoxicity following PCP administration is due to blockade of NMDA receptors that contain NR2A subunits, rather than those that contain NR2B subunits. Moreover, blockade of NR1/NR2A receptors during the early postnatal period results in locomotor sensitization in response to PCP challenge. During the embryonic stage and shortly after birth, neurons primarily express NR1/NR2B-containing NMDARs (Monyer et al. 1994, Akazawa et al. 1994). Within the first postnatal week, NR2A subunit mRNA expression is up- regulated during a period of rapid synapse formation (Akazawa et al. 1994, Monyer et al. 1994). The increase in synaptic NR2A-containing NMDARs is thought to correlate with a gradual decrease of NR2B-containing synaptic NMDARs. Generally, NR2B-containing receptors translocate during early development to the extrasynaptic space; however, depending on the brain region, some may remain in the synaptic space (Cull-Candy et al. 2001, Thomas et al. 2006). Excessive over-activation of synaptic NMDARs results in Ca2+ overload and neuronal excitotoxicity. Blockade of synaptic NMDAR activation has been shown to be neuroprotective in animal models of stroke and seizure (Lei et al. 2008, Lee et al. 1999, Hardingham & Bading 2002, Hardingham et al. 2002). Generally, it appears that synaptic NMDARs induce a coordinate up41 regulation of newly identified pro-survival genes and down-regulation of prodeath genes while extrasynaptic NMDARs appear not to activate pro-survival genes, but instead induce a putative Ca2+ activated Cl- channel that kills neurons (Hardingham & Bading 2003, Hardingham & Bading 2002, Hardingham et al. 2002). Further, it has been suggested that it is the spatial distribution and not the subunit composition per se that determines the NMDAR-dependent signaling (Ivanov et al. 2006) and its downstream consequences. Conversely, the division of function between synaptic and extrasynaptic NMDARs has been challenged by data showing that excitotoxic insults are preferentially mediated by NR2B containing receptors, regardless of localization, while NR2A receptors exerted a neuroprotective effect against both NMDAR-mediated and non-NMDARmediated toxic insults (Liu et al. 2007, Zhang et al. 2007). Here, we hypothesized that PCP-induced neurotoxicity is in part mediated through blockade of synaptic NR1/NR2A receptors. We compared two NR2A preferential antagonists, NVP-AAM007 and PEAQX, to ifenprodil, a selective NR2B subunit antagonist. NVP-AAM007 and PEAQX have greater than 10-fold selectivity for NR2A (Ki=5.4 nM) compared to NR2B (Ki=67 nM), though only a 2fold selectivity over the NR2C subunit (Ki=11.6 nM), which is sparingly found in the frontal cortex (Feng et al. 2004). Ifenprodil is a relatively selective inhibitor of the polyamine binding site on the NR2B subunit and has a 400-fold lower IC50 for NR2B-containing receptors compared to NR2A or NR2C-containing receptors (Williams 2001). We first compared these antagonists in cultured organotypic slices and observed robust neurotoxicity following incubation with either PCP or the NR2A-preferring antagonists, NVP-AAM007 and PEAQX. However, no effect of the NR2B-selective antagonist, ifenprodil, was observed. Although PEAQX and NVP-AAM007 are not truly specific for the NR2A subunit over the NR2B subunit, the lack of effect of ifenprodil strongly support the hypothesis that PCPinduced neurotoxicity is mediated largely through its blockade of NR2Acontaining receptors. At this time in our model system it is not possible to 42 definitively state that the NR1/NR2A receptors that are blocked and mediate PCP-induced neurotoxicity are located only in the synapse. Nevertheless, pharmacological manipulation with preferential NR2A and NR2B antagonists suggests that the subunit composition does play a prominent role in neurotoxicity in the frontal cortex of the developing rat, though PCP-induced neurotoxicity may be dependent on both the spatial distribution and subunit composition. This laboratory has previously reported that acute PCP administration on PN7 causes apoptosis in the cortex and striatum, but evidence of toxicity following PCP administration on PN7, 9 and 11 is found only in the cortex (Wang & Johnson, 2005; Wang & Johnson 2007). In the current experiments, we again observed a developmental and pharmacological specific PCP-mediated neurotoxicity; such that caspase-3 activation was observed in the striatum following a single injection on PN7, yet no PCP-mediated neurotoxicity was observed in the striatum following treatment on PN7, 9, & 11. We have previously attributed this to “tolerance” or an undefined, developmentally regulated, susceptibility mechanism. Interestingly, in the current study, unlike PCP, the NR2A-preferring antagonist, PEAQX, induced neurotoxicity following sub-chronic treatment on PN7, 9, & 11. At this time, the reason for this discrepancy between PEAQX and PCPmediated neurotoxicity is unknown; however, we speculate that the difference between PCP and PEAQX may be related to the neuronal type, specifically the striatal interneurons, affected by these compounds. This laboratory has reported that a single injection of PCP on PN7 does not cause a loss of GABAergic interneurons containing either parvalbumin (PV), calretinin (CR) or calbindin (CB) in the adult striatum (PN56), but does cause a loss of PVcontaining interneurons in the frontal cortex (Wang et al. 2008). Chen and Reiner (1996) demonstrated that there is a differential distribution of NR2A/NR2B subunits on striatal neuron types, such that somatostatin- and about half of the PV-containing interneurons do not possess either NR2A or NR2B subunits 43 (somatostatin and PV-containing interneurons account for approximately onepercent of all striatal neurons). Cholinergic interneurons and the majority of the identified striatal projection, striatonigral, enkephalin-containing, and striatal matrix neurons do express both NR2A or NR2B (Chen & Reiner 1996); therefore, PEAQX-induced neurotoxicity may be due to its blockade of these striatal neurons which express the NR2A subunit, e.g. cholinergic interneurons and striatal projection neurons. Further, these cholinergic interneurons have been reported to possess a greater resistance to NMDA-mediated toxicity compared to the striatal projection neurons (Araki et al. 1994, FigueredoCardenas et al. 1994). It has been postulated that these cholinergic interneurons do not express AMPA receptors (Cheng et al. 1996); therefore, without AMPA receptor activation and depolarization, it would not be possible to alleviate the voltage-dependent Mg2+ block of NMDARs and the open channel blocker, PCP, would not be able to gain entry to the NMDA channel or inhibit its function, thereby sparing these neurons. Thus, this may explain the temporal neurotoxic effects of PCP, i.e. a single injection of PCP results in the death and clearance of the projection neurons leaving behind the heartier cholinergic interneurons which are resistant to PCP-induced neurotoxicity, but are sensitive to PEAQX blockade. While division of NR2A and NR2B receptors into synaptic and extrasynaptic pools, respectively, is not completely true in all instances, it provides a framework for this study. Furthermore, although the biological relevance of the segregation of NMDARs into synaptic and extrasynaptic locales is incompletely understood, the mechanism of targeting the NMDAR to these different sites is thought to involve the C-terminal tail of the NR2 subunit and its interactions with PDZ domain proteins in the postsynaptic density (Prybylowski et al. 2005). The PDZ proteins play a fundamental role in linking the NMDAR to intracellular signaling cascades (Prybylowski et al. 2005). Further, the differential association with the MAGUK (membrane-associated guanylate kinase) family members may be vital not only for the regulation and expression of the NMDAR, 44 but also for the localization of NMDAR subtypes during development and subsequently, the response to noxious agents, such as PCP (Kim & Sheng 2004, Cousins et al. 2008). PSD-95 is the most highly enriched PDZ protein in the postsynaptic density and is thought to predominantly associate in vivo with NR2A, while SAP102 is commonly expressed in dendrites, axons and cytoplasm as well as the synaptic and extrasynaptic spaces and associates with primarily with NR2B (Kim & Sheng 2004, Sans et al. 2000). There is also a developmental expression pattern for SAP102 and PSD-95, whereby SAP102 predominates in the synapse early in postnatal life and then PSD-95 gradually increases in the synaptic space as the animal matures (Kim & Sheng 2004). Interestingly, this developmental pattern mirrors the developmental “switch” in expression pattern of NR2B to NR2A, supporting earlier reports that in immature synapses NR2BSAP102 complexes are predominant, but as the animals age, NR2B subunits may be translocated to the extrasynaptic space as NR2A-PSD-95 expression increases in the mature synaptic milieu (Sans et al. 2000, Kim & Sheng 2004, Cull-Candy et al. 2001) . We performed co-immunoprecipitation studies to determine the localization of cortical NMDARs in a crude synaptoneurosomal preparation from postnatal cortex. Several studies have shown the number of NMDARs, their subunit composition, as well as their postsynaptic linkers can be altered following administration of NMDA antagonists including MK-801, ethanol and PCP (Dong et al. 2004, Anastasio & Johnson 2008b, Sircar et al. 1996, Suvarna et al. 2005, du Bois et al. 2009). These alterations in expression of the NMDAR have been suggested to be due to changes in synthesis, trafficking of the receptor from intracellular compartments to the membrane, or lateral diffusion within the membrane (Anastasio & Johnson 2008b, Tovar & Westbrook 2002, Choquet & Triller 2003). We demonstrated that following PCP treatment on PN7, 9, & 11, there is an apparent compensatory up-regulation in the surviving neurons of NR1/NR2A/PSD-95, while no statistically significant effect on NR1/NR2B/PSD-95 45 was measured. This response to PCP-induced neurotoxicity by neighboring neurons may represent a protective mechanism to prevent further damage to the brain and/or restore cortical NMDA-mediated neurotransmission and synaptic communication. An increase in the association of both NR2A and NR2B with SAP102 following PCP administration was also observed. While it is reasonable to postulate that these receptors exists as functional heterodimers, the segregation of these subunits into a heterotrimeric receptors in either the synaptic or extrasynaptic space cannot be ruled out. Interestingly, we observed no effect of PCP treatment on the relationship between NR1 and SAP102 (data not shown). An alternative explanation of this is that in the extrasynaptic space there is an increase in NR2A or NR2B subunits that is not associated with NR1, suggesting the possibility of an effect on the composition of the NMDAR resulting in the insertion and expression of a nonfunctional NMDAR linked to SAP102 most likely in the extrasynaptic milieu, but may also be in the synaptic locale. This would also represent an alternative, pro-survival compensatory mechanism rendering the neuron less susceptible to glutamate toxicity (Vanhoutte & Bading 2003). The neurotoxicity evident in the frontal cortex following either a single injection or multiple injections suggests a role for altered cortical function in either the poor performance of certain behavioral tasks or the development of aberrant behaviors (Wang & Johnson 2007, Wang & Johnson 2005, Wang et al. 2001). The neurodevelopmental theory of schizophrenia states that damage to the brain during a critical stage of brain maturity (PN7-11 in the rat) may account for the development of mental illness later in life due to impaired synapse formation and neurite outgrowth (Olney et al. 2002, du Bois & Huang 2007). Therefore, we tested the hypothesis that PCP-induced cortical neurotoxicity plays a role in the development of locomotor sensitization and that both involve blockade of synaptic NR1/NR2A subunits during a critical stage in brain development. This study established that PCP administration on PN7, 9, & 11 resulted in an 46 enhanced locomotor response to PCP challenge on PN28-35, and a similar result was observed following treatment with the NR2A antagonist, PEAQX. On the other hand, animals treated with ifenprodil on PN7, 9, & 11 exhibited no change in locomotor activity in response to PCP challenge. Thus, these data strongly support the hypothesis that blockade of NR2A receptors by PCP treatment on PN7, 9 and 11 and the subsequent cell death alters the architecture of the cortex as well as glutamatergic and GABAergic synaptic transmission (du Bois et al. 2009, Olney & Farber 1995a) resulting in the development of a sensitized locomotor response to PCP challenge. Interestingly, these experiments demonstrate that the effect of the PCP challenge on test day (PN28-35) to either developmentally treated PCP or PEAQX animals is not due to the immediate blockade of either NR2A or NR2B by PCP. That is, since challenge with either PEAQX or ifenprodil, or a combination of the two, did not result in an enhanced locomotor response, then it follows that blockade of either NR2A or NR2B alone or in combination is insufficient to produce an increased behavioral response and suggests that the expression of PCP-induced sensitization requires activation of mechanisms apart from blocking either NR2A or NR2B independently or simultaneously. It is quite possible that the actual expression of sensitization requires NMDA receptorindependent effects of PCP such as blockade of DA or 5-HT uptake or inhibition of cholinergic receptors or K+ channels (Verma & Moghaddam 1996, Johnson & Jones 1990, Lodge & Johnson 1990). In summary, PCP induces neurotoxicity in developing pups in a manner that is highly regulated and is dependent on the distribution as well as the composition of the NMDAR. The consequences of this loss of cortical neurons and altered cortical landscape are associated with behavioral deficits that are similar to the positive symptoms of schizophrenia. Further, future work delineating the role of NR2 subunits in the neurotoxic process may lead to the development of future pharmacotherapeutics for schizophrenia. 47 Chapter 3: Differential Regulation of the NMDAR by Acute and Sub-chronic Phencyclidine Administration Neurodegeneration induced by the NMDAR antagonist phencyclidine (PCP) has been used to model the pathogenesis of schizophrenia in the developing rat. Acute and sub-chronic administration of PCP in perinatal rats results in different patterns of neurodegeneration. The potential role of an alteration in the membrane expression of NMDARs in PCP-induced degeneration is unknown. Acute PCP treatment on PN7 increased membrane levels of both NR1 and NR2B proteins in the frontal cortex; conversely, NR1 and NR2B protein levels in the endoplasmic reticulum (ER) fraction were decreased. Acute PCP administration also resulted in increased membrane cortical protein levels of postsynaptic density-95 (PSD-95), as well as the activation of calpain, which paralleled the observed increase in membrane expression of NR1 and NR2B. Further, administration of the calpain inhibitor, MDL28170, prevented PCPinduced up-regulation of NR1 and NR2B. On the other hand, sub-chronic PCP treatment on PN 7, 9 and 11 caused an increase in NR1 and NR2A expression, which was accompanied by an increase in both NR1 and NR2A in the ER fraction. Sub-chronic PCP administration did not alter levels of PSD-95 and had no effect on activation of calpain. These data suggest that increased trafficking accounts for up-regulation of cortical NR1/NR2B subunits following acute PCP administration, while increased protein synthesis likely accounts for the increased expression of NR1/NR2A following sub-chronic PCP treatment of the developing rat. These results are discussed in the context of the differential neurodegeneration caused by acute and subchronic PCP administration in the developing rat brain. 48 Introduction PCP is a potent noncompetitive NMDAR antagonist [Ki~100 nM (Anis et al. 1983)] that has been shown to mimic both the positive and negative symptoms of schizophrenia in humans and to exacerbate psychosis in schizophrenics (Luby et al. 1962, Javitt & Zukin 1991). Since the symptoms of schizophrenia do not appear until early adulthood, Weinberger (1987) postulated that the etiology of schizophrenia may be developmental in nature and that the primary pathological insult may occur in utero or early in postnatal development (Benes 1991, Murray et al. 1992, Pilowsky et al. 1993). The nature of this insult is unknown, but it could involve glutamatergic hypofunction and may involve a loss of certain cortical interneurons and/or an altered organization of cortical connectivity (Benes 1991, Benes 1995, Lewis 1997). This led to investigation of the neurotoxic effects of acute PCP or MK-801 during development in the rat (Lei et al. 2008, Ikonomidou et al. 1999, Wang & Johnson 2005, Wang & Johnson 2007). While acute PCP administration on PN7 causes wide-spread apoptosis (Ikonomidou et al. 1999, Wang et al. 2005, Wang & Johnson 2007) evidence of apoptosis including positive caspase-3 immunoreactivity and TUNEL staining is restricted to the cortex following sub-chronic PCP administration on postnatal day (PN) 7, 9, and 11 (Wang et al. 2001, Wang & Johnson 2007, Wang & Johnson 2005). These data suggest the presence of a developmentally regulated tolerance in these regions (Wang et al. 2001, Wang & Johnson 2007, Wang & Johnson 2005). Over activation of NMDARs has been shown to cause damage that will eventually kill neurons in a process known as excitotoxicity (Lynch & Guttmann 2002). It is generally agreed that activation of NMDARs causes an increase in Ca2+ influx leading to intracellular Ca2+ overload (Abdel-Hamid & Tymianski 1997, Garthwaite & Garthwaite 1986, Lei et al. 1992), activation of pro-death proteins including caspase-3 and ultimately neurotoxicity. Other studies have shown that NMDAR-mediated neurotoxicity involves increased superoxide formation and the 49 activation of the proteolytic enzyme caspase-3 resulting in increased NF-κB nuclear transport. These mechanisms are activated by excessive intracellular Ca2+ levels (McInnis et al. 2002, Qin et al. 2000, Takadera et al. 1999), most likely secondary to increased NMDAR function and support the hypothesis that PCP-induced neurotoxicity may be mediated by increases in the NMDAR density (Wang et al. 2005). Thus, further investigation of PCP-induced regulation of the NMDAR in conjunction with neurotoxicity may shed light on the molecular mechanisms underlying the psychotomimetic properties of PCP, particularly those mediating the schizophrenia-like symptoms following perinatal administration (Wang et al. 2001). The NMDAR is composed of multiple subunits including NR1, NR2A-D and NR3A/B. The NR1 subunit forms a heteromeric complex with one of the four NR2 (A-D) subunits (Kutsuwada et al. 1992, Monyer et al. 1994). The composition of the NR1/NR2 complex differs in regard to their regional pattern of expression, their regulation by phosphorylation, polyamines or protons, their electrophysiological properties, and their affinity for cytoskeletal proteins (Paoletti & Neyton 2007, Kohr 2006, Waxman & Lynch 2005, Westbrook et al. 1997). Each subunit of the NMDAR contains an extracellular N-terminal region, three membrane spanning domains, one intramembrane loop and an intracellular Cterminal region. The C-terminal region of the NR2 subunit is thought to be a substrate for the calcium-activated neutral protease calpain (Wu & Lynch 2006, Wechsler & Teichberg 1998, Guttmann et al. 2001, Guttmann et al. 2002, Bi et al. 1998a, Bi et al. 1998b). Further, this region serves as a binding site for intracellular anchoring proteins such as PSD-95, SAP102, and SAP97 and also links second messenger cascades to the NMDAR, thereby modulating the relations of the receptor with various intracellular signaling cascades (Niethammer et al. 1996, Bi et al. 1998b, Wechsler & Teichberg 1998, Wu & Lynch 2006, Bi et al. 1998a, Guttmann et al. 2001, Guttmann et al. 2002, Zheng et al. 1999)). Furthermore, the C terminus has been suggested to play a strong 50 role in regulating trafficking of the NR1 subunit (Wenthold et al. 2003) and posttranslational modifications of this region play a role in the activity of the NMDAR localization and function (Guttmann et al. 2002). Therefore, the purpose of the present study was to characterize the effect of both acute (PN7) and sub-chronic (PN7, 9, & 11) PCP treatment on the regulation of the NMDAR subunits (NR1, NR2A, and NR2B) as well as PSD-95, a member of the NMDAR postsynaptic density complex, in the frontal cortex in order to determine the possible role of NMDAR trafficking and expression in PCP-induced neurodegeneration and later behavioral deficits. Materials and methods Animals. Timed, day 14 pregnant female Sprague-Dawley rats were obtained from Charles River Laboratories (Wilmington, MA). The dams were housed individually with a regular 12h light-dark cycle (lights on 0700, off at 1900) with food and water ad libitum. Following parturition, male and female pups from four dams were combined and randomly cross-fostered to one of the four lactating dams. Each litter consisted of ten to twelve pups. All experiments were conducted in accordance with the NIH and the Institutional Animal Care and Use Committee. Drugs. Phencyclidine was acquired from the National Institute on Drug Abuse (NIDA, Rockville, MD) and dissolved in 0.9% NaCl. MDL28170 (10 mg/kg, Sigma-Aldrich, St. Louis, MO) was dissolved in 1% DMSO. Doses were chosen based on prior experiments that addressed PCP-induced regulation of the NMDAR (Wang et al. 2001) and our own work with the compounds. Injections were administered i.p. or s.c. in 1 mL/kg of vehicle. 51 Experimental design. Male and female rat pups were treated on either PN7 (acute) or on PN 7, 9, and 11 (sub-chronic) with 10 mg/kg subcutaneous (s.c.) PCP or saline. In the acute studies, pups were sacrificed by decapitation on PN7 at 0, 4, 8, or 24 hours following saline/vehicle (control, time=0 hours), PCP/vehicle treatment. In the acute MDL28170 studies, pups were treated with PCP on PN7 or post-treatment with MDL28170 (10 mg/kg, i.p., every 2 hours for 8 hours) and then sacrificed by decapitation 24 hours following saline/ vehicle, PCP/vehicle, MDL28170/vehicle, MDL28170+PCP/vehicle treatment. In the sub-chronic studies, pups were sacrificed by decapitation 24 hours following the last injection of the aforementioned drug regimens on PN7, 9 and 11. For both acute and subchronic biochemical studies, the frontal cortex was dissected as described below and used for Western blot analysis. Sub-cellular fractionation. Protein extracts were prepared from 2 mm sections corresponding to 4.7 to 2.7 mm anterior to Bregma for the frontal cortex as previously described with some modifications (Wang et al. 2001, Paxinos & Watson 1986). Cortical brain sections were homogenized in 500 μL of lysis buffer with the aid of an automatic tissue grinder (Kontes Pellet Pestle Motor, Kimble / Kontes, Vineland, New Jersey). The lysis buffer consisted of 10 mM HEPES (pH 7.4), 1 mM EDTA, 2 mM EGTA, and 500 μM DTT. Just prior to use, protease inhibitor cocktail [4-(2aminoethyl) benzenesulfonyl fluoride (AEBSF), pepstatin A, E-64, bestatin, leupeptin, and aprotinin without metal chelators (Sigma-Aldrich, St Louis, MO)] at a concentration of 10 μL/mL was added to the lysis buffer. The homogenate was then centrifuged at 1000 x g at 4oC for 10 minutes to pellet the nuclear protein fraction (P1). The supernatant (S1) was collected and centrifuged at 8000 x g at 4oC for 30 minutes to pellet the membrane bound protein fraction (P2). The cytoplasmic fraction (S2) was collected and stored at -80oC. P2 (membrane 52 fraction) was re-suspended in homogenization buffer and centrifuged at 20,000 x g at 4oC for 30 minutes; the resultant pellet was re-suspended in lysis buffer + 1% SDS, boiled for 10 minutes and stored at -80oC. To isolate endoplasmic reticulum (ER) protein, the S2 fraction was centrifuged at 100,000 x g at 4 oC for 60 minutes. P3 (ER fraction) was re-suspended in lysis buffer and stored at 80oC. Total protein concentrations were determined using the BCA (bicinchoninic acid) protein assay© (Pierce Chemical, Rockford, IL). Western blot analysis. Equal amounts of protein were separated on 10% Bis-Tris gels (Invitrogen, NY) using SDS-PAGE with a MES-SDS running buffer system, pH 7.4. Following electrophoresis (110 V for 2 hours), proteins were transferred to polyvinylidene difluoride (PVDF) membranes (0.2 μm) in a Mini Electrotransfer Unit (Bio-Rad, Hercules, CA) overnight. The membrane was blocked in 5% nonfat milk, followed by incubation with the primary antibody in 1% milk for 2 hours at room temperature. Following washes (3 x 10 minutes) in TBS+0.1% Tween 20 (TBST), the membrane was incubated with horseradish peroxidase conjugated secondary antibodies for 1 hour at room temperature. Analysis was carried out using the enhanced chemiluminescence (ECL) plus Western blotting detection reagents (Amersham Biosciences, Piscataway, NJ). corresponding to the various proteins of interest were The bands scanned and densitometrically analyzed by using an automatic imaging analysis system (Alpha Innotech Corporation, San Leandro, CA). All quantitative analyses were normalized to β-actin (after stripping [Reblot mild, Chemicon International, Temecula, CA]). Antibodies. The monoclonal anti-NR1, anti-NR2A, anti-NR2B, and anti-protein disulfide isomerase (PDI) were purchased from BD Biosciences (San Jose, CA). 53 The monoclonal anti-PSD-95 and anti-αII spectrin antibodies were purchased from Chemicon International (Temecula, CA). Primary antibody dilution was 1:500-1:1000. Secondary antibodies were purchased from Zymed (Invitrogen Corporation, Carlsbad, CA) and used at a concentration of 1:5000. Results It has been reported that neurotoxicity caused by non-competitive NMDAR antagonists is dependent on development with the most vulnerable time existing in the early postnatal period in rats (Ikonomidou et al. 1999, Wang & Johnson 2007, Wang & Johnson 2005). In order to ascertain the effects of acute PCP (10 mg/kg) treatment on the expression of NMDAR subunits, membrane protein from the frontal cortex was extracted on PN 7 at 0, 4, 8 and 24 hours after saline or PCP treatment. Saline treated animals sacrificed immediately after administration (t=0 hour) on PN7 served as the control in the biochemical studies of the time course of acute PCP effects. Figure 3.1A shows representative Western blots of NR1 and NR2B from the frontal cortex of acute PCP or saline treated perinatal rats at all time points examined on PN7. Quantitative analysis revealed that acute PCP treatment produced a 3-fold increase in membrane bound NR1 and NR2B subunits in the frontal cortex at 8 hours and this persisted for 24 hours (Figure 3.1B). The calpain-degraded NR2B breakdown product, molecular weight 140 kDa, was increased 80% following acute PCP treatment (saline 0.485 ± 0.161; PCP 0.868 ± 0.216, n=6 for both groups, p<0.05 paired ttest). There was no effect of acute PCP treatment on membrane bound NR2A protein levels in the frontal cortex (Figure 3.1B). To investigate the effects of sub-chronic PCP administration on the concentration of the membrane NR1, NR2A, and NR2B in the frontal cortex, rat pups were treated with either saline or PCP on PN7, 9, & 11 and were sacrificed on PN12 (24 hours following the last injection). Cortical membrane bound protein extracts were then subjected to Western blot analysis. 54 Figure 3.2A shows representative Western blots of NR1 and NR2A subunits from the frontal cortex. Sub-chronic PCP treatment caused a 3-fold increase in membrane NR1 and a 10-fold increase in NR2A protein levels in the frontal cortex with no effect on NR2B protein expression (Figure 3.2B). To determine the possible mechanism by which PCP regulates the expression of cortical NMDAR subunits, protein residing in the endoplasmic reticulum (ER) fraction was isolated from saline and acute PCP or sub-chronic PCP treated animals and subjected to Western blot analysis. To verify that the ER fraction was successfully isolated, we probed for protein disulfide isomerase (PDI, an ER housekeeping protein); no changes in ER PDI protein levels were measured following acute or sub-chronic PCP administration and PDI was not detected in the membrane protein fraction (data not shown). Acute PCP treatment produced a decrease in NR1 and NR2B protein levels in the ER fraction of the frontal cortex on PN7 at 24 hours following administration (Figure 3.3). Conversely, sub-chronic PCP treatment produced an increase in NR1 and NR2A protein levels in the ER fraction measured 24 hours following the last of the three injections (Figure 3.3). These results indicate that acute PCP administration may cause an increase in trafficking of the NR1 and NR2B subunits from intracellular compartments to the membrane while sub-chronic PCP treatment induces new synthesis of the NR1 and NR2A subunits. In addition, PSD-95 protein expression levels in the membrane fraction of frontal cortex were also increased following 8 hours of PCP treatment and remained elevated 24 hours after treatment (Figure 3.4B). However, following sub-chronic PCP administration, the β-actin normalized values for cortical membrane PSD-95 protein (0.973 ± 0.214, N=4) were not significantly different from saline treated animals (0.717 ± 0.0781, N=4, p=0.306, Figure 3.4B). Figure 3.4A shows representative Western blots of cortical PSD-95 protein expression from acute and sub-chronic PCP treated animals. 55 Figure 3.1. Acute PCP administration selectively up-regulates NR1/NR2B in the frontal cortex of perinatal rats. A) Representative western blots from the frontal cortex of saline or acute PCP treated animals at all time points examined on PN7. B) Quantitative analysis of the effects of acute PCP treatment on NR1, NR2A and NR2B membrane bound protein levels in the frontal cortex (N=15/group). *p<0.05 vs. SAL NR1 (one-way ANOVA with Bonferroni's post hoc test) #p<0.05 vs. SAL NR2B (one-way ANOVA with Bonferroni's post hoc test) 56 Figure 3.2. Sub-chronic PCP treatment up-regulates NR1/NR2A in the frontal cortex of perinatal rats. A) Representative western blots from the frontal cortex of saline or sub-chronic PCP (10 mg/kg, N=15) treated animals. B) Quantitative analysis of the effect of sub-chronic PCP on NMDAR subunit proteins in the frontal cortex. (N=15/group) *p<0.05 vs. SAL NR1 (one-way ANOVA with Bonferroni’s post hoc test) ^p<0.05 vs. SAL NR2A (one-way ANOVA with Bonferroni’s post hoc test) 57 Figure 3.3. Effects of acute and sub-chronic PCP administration on the NMDAR subunits in the cortical ER fraction. Quantitative analysis of the effect of acute and sub-chronic PCP (10 mg/kg) on ER protein levels of NMDAR subunits in the frontal cortex. *p<0.05 vs. acute saline (Student’s t-test) ^p<0.05 vs. sub-chronic saline (Student’s t-test) 58 Figure 3.4. Acute PCP treatment selectively alters levels of PSD-95 in the frontal cortex of perinatal rats. A) Representative western blot showing acute PCP treatment (10 mg/kg, n=4) produced a time-dependent increase in membrane levels of PSD-95 while sub-chronic PCP treatment has no effect on the levels of membrane PSD-95 protein in the frontal cortex. B) Quantitative analysis of protein expression from acute and sub-chronic PCP treatment on PSD-95 protein levels in the frontal cortex. (N=4/group) *p<0.05 vs. acute SAL (one-way ANOVA with Bonferroni’s post hoc test) 59 To further define the mechanism of PCP-induced regulation of the NMDAR, we examined the role of calpain (calcium-dependent neutral cysteine protease). Cleavage of the cytoskeletal proteins alpha-II spectrin by calpain between Tyr1176 and Gly1177 produces two αII spectrin specific breakdown products (SBP) of molecular weights 150 and 145 kDa, which are calpainspecific spectrin breakdown products and antibodies to these fragments are available commercially; therefore, one can indirectly measure calpain activation through Western blot analysis of SBPs (Zhou & Baudry 2006, Nath et al. 1996, Bi et al. 1997, Wu & Lynch 2006). Acute PCP treatment resulted in an increase in the αII-spectrin calpain SBP while sub-chronic PCP treatment had no effect on αII-spectrin calpain SBP expression levels (Figure 3.5B). To further clarify the role of calpain in PCP-induced trafficking of the NMDAR subunits, we treated animals following acute PCP administration with the selective calpain inhibitor, MDL28170 (10 mg/kg, every 2 hrs for 8 hrs, i.p.). MDL28170 is a potent calpain inhibitor (Ki=10 nM in vitro) that has been shown to cross the blood brain barrier following systemic administration (Li et al. 1998). Animals were sacrificed 24 hours after the PCP injection and Western blot analysis of cortical membrane NR1 and NR2B was performed. PCP administration resulted in an up-regulation of both NR1 and NR2B, which was blocked by post-treatment with MDL28170 (Figure 3.6). These data lend support for the role of calpain activation in acute PCP-induced changes in the trafficking of NR1/NR2B. 60 Figure 3.5. Effects of acute and sub-chronic PCP administration on the activation of calpain in the frontal cortex. A) Representative western blot showing acute PCP treatment (10 mg/kg, n=4) produced an increase in membrane levels of calpain SBP (145/150 kDa) while sub-chronic PCP treatment has no effect on the levels of calpain SBP (145/150 kDa) protein in the frontal cortex. B) Quantitative analysis shows that acute PCP treatment causes an increase in the activation of calpain as measured by the cleavage of αII-spectrin while sub-chronic PCP has no effect. *p<0.05 vs. acute saline (Student’s t-test) 61 Figure 3.6. Effects of MDL28170 (calpain inhibitor) on the cortical membrane expression of NMDAR subunits following acute PCP treatment. Quantitative analysis shows that acute PCP (10 mg/kg, 24 hrs after treatment) treatment causes an increase in membrane levels of NR1 and NR2B and that administration of the calpain inhibitor, MDL28170 (10 mg/kg i.p.), blocks upregulation of both NR1 and NR2B. MDL28170 was administered on PN7 every 2 hrs following PCP treatment for 8 hrs. (N=6/group) *p<0.05 vs. NR1 SAL (One way ANOVA with Tukey’s test) ^p<0.05 vs. NR2B SAL (One way ANOVA with Student-Newman-Keuls method) 62 Discussion NMDAR antagonists including PCP, MK-801 and ethanol have been shown to regulate the membrane expression levels of the NMDAR through changes in protein synthesis or trafficking of the complex from intracellular compartments to the membrane (Dong et al. 2004, Sircar et al. 1996, Suvarna et al. 2005). Previous studies reported an increase in NR1 and NR2A mRNA in the cortex and striatum of the neonatal rat 4 hours after MK-801 treatment (Wilson et al. 1998). These results are consistent with an increase in NMDAR membrane protein (McDonald et al. 1990a, Gao & Tamminga 1994) and the delayed occurrence of toxicity induced by MK-801 or PCP (Ikonomidou et al. 1999, Wang et al. 2001, Wang & Johnson 2005). The present study demonstrated that acute PCP treatment on PN7 increased the levels of membrane NR1 and NR2B protein expression in the frontal cortex at 8 and 24 hours following PCP administration. Further, analysis of the cortical ER fraction demonstrated a decrease in NR1 and NR2B protein following acute PCP administration. To understand the mechanism by which the up-regulation of NR1 and NR2B occurs, we first examined PCP-induced changes in the expression of PSD-95. The membrane associated guanylate kinase family (MAGUK) of proteins, specifically PSD-95, play key roles in NMDAR trafficking to the membrane (Dong et al. 2004, Lu et al. 2000, Suvarna et al. 2005), clustering at the membrane, and stabilization of the NMDAR complex and organization of the post-synaptic architecture (Mauceri et al. 2007, Wu et al. 2007, Lu et al. 2000, Yamada et al. 1999a). Acute PCP administration produced an increase in membrane cortical protein levels of PSD-95, which paralleled the observed increase in membrane NR1 and NR2B expression in the frontal cortex. Therefore, increased trafficking of assembled NMDAR from the ER to the membrane in conjunction with intact PSD-95 following acute PCP administration would account for the apparent up-regulation of NR1/NR2B composed receptors in the frontal cortex. 63 Activation of the NMDA receptor results in the influx of Ca 2+ which in turn activates the calcium-dependent neutral cysteine protease, calpain, among many other key calcium-dependent signaling molecules. Calpain activation has been suggested to play a role in excitotoxic neuronal death (Saido et al. 1994, Brorson et al. 1995, Araujo et al. 2004, Zhou & Baudry 2006) as well as neurodegenerative disorders such as Parkinson’s and Alzheimer’s diseases (Etienne & Baudry 1987, Crocker et al. 2003, Vanderklish & Bahr 2000). Excessive activation of calpain results in the enzymatic cleavage of cytoskeletal proteins, loss of structural integrity and disturbances in axonal transport (Yamashima 2004). The C-terminal regions of the NR2A (cleavage position Phe1279; Ser1330) and NR2B subunits have been shown to be substrates of calpain (Bi et al. 1998a, Bi et al. 1998b, Guttmann et al. 2001), both in vivo and in vitro (Wu et al. 2007, Wu & Lynch 2006). Here we report that acute PCP administration results in a robust activation of calpain 24 hrs following treatment. Wu and colleagues (2005) suggested that after overactivation of NMDARs, calpain will cleave and degrade the NMDAR, resulting in downregulation of its function and protection of the neuron from excitotoxic cell death; on the other hand, it is possible that following acute PCP administration the protective effects of calpain are abolished; therefore, the cell death cascade is activated. Based on functional studies using I 125-MK-801 binding to NR1/NR2B, it has been suggested that in excitotoxic settings, calpain cleavage of NR2B creates novel, active fragments (140, 130, and 115-120 kDa) which remain on the extracellular surface and function similar to the native receptor (Liao et al. 2001, Simpkins et al. 2003). Taken together, our results support the possibility that cortical neurotoxicity measured on PN7 in perinatal rats is due to a hyperfunctional NR1/NR2B complex; however, this interpretation is complicated by recent time course studies from this laboratory. It has been shown that following a single injection of PCP on PN7, caspase-3 is activated by 2 hrs in the frontal cortex; furthermore, TUNEL staining appears 6 hrs after treatment, peaks at 16 64 hrs and is cleared by 24 hrs (Wang & Johnson 2007, Wang & Johnson 2005). This study reports that the time course of up-regulation of NR1 and NR2B in the frontal cortex following acute PCP treatment occurs after neuronal neurodegeneration has been initiated (Wang & Johnson 2007, Wang & Johnson 2005), suggesting that the up-regulation of NR1 and NR2B must also arise in surviving neurons where up-regulation potentially could play a compensatory role in these neurons. Nonetheless, it is also possible that NR1 and NR2B up- regulation plays a significant role in neurotoxicity following acute administration of PCP. Sub-chronic PCP treatment of pups resulted in increased expression of NR1 mRNA and polypeptide in the frontal cortex (Wang et al. 2001). In addition to up-regulation of NR1, the current study found that sub-chronic PCP administration resulted in increased expression of membrane NR2A in the frontal cortex, with no change in NR2B levels. Furthermore, analysis of the cortical ER protein fraction revealed increased NR1 and NR2A protein levels following subchronic PCP treatment, suggesting that up-regulation may be due to increased synthesis of these subunits. While the mechanism underlying this up-regulation is unknown, it is known that the NR1 gene contains a binding site for the transcription factor NF-κB (Liu et al. 2004a). Further, it has been reported that binding to the NR1 NF-κB site up-regulates the NR1 promotor and subsequent transcription of the gene through interactions with Sp1/Sp3 factors. This is relevant in that this laboratory previously reported that sub-chronic PCP treatment increased nuclear translocation of NF-κB (Wang et al. 2001). Therefore, PCP-induced activation of NF-κB may signal increased synthesis of the NR1 subunit, resulting in the observed up-regulation of the protein. These data along with the neurotoxic effects of sub-chronic PCP treatment in vivo support the possibility that up-regulation of NR1 and NR2A in the frontal cortex may be due to an increase in new protein synthesis. 65 We suggest that the mechanism of regulation of the NMDAR is treatmentdependent. This is supported by our observation of the lack of effect of subchronic PCP administration on the levels of PSD-95 and calpain activation. Disruption of the NR2A-PSD-95 interface by either palmitoylation of PSD-95 or elimination of the PSD-95 binding site on NR2A leaves NR2A susceptible to cleavage by calpain (Wu & Lynch 2006, Dong et al. 2004). Alternatively, it has been suggested that PSD-95 may also be a substrate for calpain and it has been shown that NMDA treatment of organotypic hippocampal cultures produced activation of calpain and the subsequent cleavage of PSD-95 (Lu et al. 2000). Truncation of PSD-95 would then lead to an unstable NR1/NR2A/PSD-95 complex in the membrane and cause the internalization and down-regulation of the assembled NMDAR (Dong et al., 2004). It is reasonable then to predict that the up-regulation of NR1/NR2B following acute PCP administration is due to activation of calpain-mediated trafficking while up-regulation of NR1/NR2A following sub-chronic PCP administration is due to an increase in protein synthesis as well as a stable NR1/NR2A/PSD-95 complex and the subsequent forward trafficking of this complex into the synapse. These conclusions are consistent with recent studies suggesting that calpain mediated regulation of the NMDAR is dependent on the NR2 subunit present (2A resistant, 2B sensitive) as well as the developmental age and brain region examined (Dong et al. 2006). Furthermore, it has been recently reported that NMDA-induced protein synthesis is dependent on the presence of the NR2A, but not the NR2B subunit (Tran et al. 2007). In summary, this study provides evidence that two distinct mechanisms are likely involved in the differential regulation of NMDAR subunits following perinatal acute and sub-chronic PCP administration. These data are consistent with the hypothesis that changes in NMDAR density may play a role in PCPinduced neurotoxicity in the frontal cortex in the developing rat. 66 Chapter 4: Alterations in NMDAR Binding of 3H-MK-801 in Response to Postnatal PCP Administration PCP is known to block the function of N-methyl-D-aspartate receptors (NMDAR) through binding to the interior of the open ion channel. We have previously reported that the NR1/NR2B receptor is up-regulated following a single injection of PCP while the NR1/NR2A receptor is up-regulated in response to sub-chronic PCP treatment (see chapter 3). It is hypothesized that up- regulation of the NMDAR protein is associated with increased receptor function. To test this hypothesis, NMDAR function was estimated by measuring the binding of 3H-MK-801, a high-affinity open channel blocker, that binds to the NMDAR channel interior in a manner that reflects the relative degree of channel opening (Jones et al. 1989) Rat pups were treated on PN7 (acute) or on PN 7, 9, 11 (sub-chronic) with 10 mg/kg PCP or saline. Twenty-four hours later, the rats were sacrificed; the frontal cortex was harvested and subsequently prepared for binding by homogenization and differential centrifugation so as to isolate a crude, well-washed synaptosomal fraction. 3H-MK-801 binding was estimated in the presence of maximally activating concentrations of NMDA and the co-agonist, glycine. Under these conditions, both acute and sub-chronic PCP produced a robust increase in agonist stimulated 3H-MK-801 binding compared to saline. Inhibition studies with selective NR2A and NR2B antagonists were performed to determine the subunit composition of the NMDAR species responsible for its enhanced function. Because of the disruption by Hurricane Ike, this series of experiments was not completed and at this time it is difficult to interpret these results. Nevertheless, these data are presented in their current form in hopes that these experiments will be completed before finalization of this dissertation project. At this point, 3H-MK-801 binding in the presence of glutamate and glycine confirms that PCP treatment increases NMDAR function, most likely as a result of an increase in receptor density. In summary, the use of radioligand 67 binding as a measure of open channel function has been partially successful in elucidating the relationship between PCP-induced up-regulation of the NMDAR and its functionality. Introduction PCP is a drug of abuse known to cause neurological effects, such as a reversible psychotic state which includes the full range of positive and negative symptoms of schizophrenia in healthy individuals (Mechri et al. 2001, Javitt & Zukin 1991), a disease that is thought to be associated with a developmental insult (Weinberger 1996). The NMDAR hypofunction theory of schizophrenia is supported by the selectivity of PCP for the NMDAR as well as the recent findings linking several putative schizophrenia genes to glutamatergic neurotransmission and the NMDAR (Harrison & Weinberger 2005). Glutamate, the primary mediator of excitatory neurotransmission at central nervous system synapses, plays an important role in synaptic plasticity, predominantly through its actions at the NMDAR. The NMDAR is a ligand-gated ion channel which requires the binding of glutamate and the co-agonist glycine, as well as removal of a voltage-dependent Mg2+ block, in order to be functionally active (Johnson & Jones 1990, MacDonald et al. 1987). Cloning studies have identified several NMDA receptor subunits: the obligatory NR1, NR2A-D, and NR3A-B (McBain & Mayer 1994). The NR1 subunit forms a heteromeric complex with NR2 or NR3 subunits. The most abundant receptor combinations in the forebrain are thought to be diheteromeric (NR1/NR2A, NR1/NR2B) or triheteromeric (NR1/NR2A/2B) with the physiology and pharmacology of the NMDAR dependent on its subunit composition and localization (Cull-Candy et al. 2001). PCP is an open channel blocker of the NMDAR, inhibiting the channel in a use and voltage-dependent manner. MK-801 is a high-affinity, noncompetitive NMDAR open-channel antagonist which has proven to be an effective tool to examine the functional properties of the NMDAR 68 as well as the effects of PCP or ketamine in animal models of drug abuse and mental diseases (Vanderschuren et al. 1998, Beardsley et al. 1990). Noncompetitive NMDA antagonists, including PCP and MK-801, are routinely used to model schizophrenia in adult and young animals (Wang et al. 2001, Hargreaves & Cain 1995, Jentsch et al. 1997, Moghaddam et al. 1997, Ogren & Goldstein 1994, Ikonomidou et al. 1999). Blockade of the NMDAR results in increased release of glutamate in the frontal cortex (Moghaddam et al. 1997), which leads to the subsequent overactivation of either AMPA or KA receptors, resulting in excitotoxic cell death (Large 2007). Additionally, blockade of trophic NMDAR function with MK-801 or PCP causes widespread neurotoxicity in various brain regions in developing rodents, including the frontal cortex, hippocampus, and striatum (Lei et al. 2008, Xia et al. 2008, Ikonomidou et al. 1999). This laboratory has also reported the presence of apoptotic (TUNELpositive) neurons in the cortex of perinatal rats, following sub-chronic PCP (10 mg/kg) administration on postnatal day (PN)7, 9, and 11; however, neurotoxicity is not evident in the striatum or hippocampus, thereby suggesting developmental tolerance or limited susceptibility in these regions (Wang et al. 2001, Wang & Johnson 2005). Thus, further investigation of PCP-induced regulation of the NMDAR in conjunction with neurotoxicity may shed light on the molecular mechanisms underlying the psychotomimetic properties of PCP, particularly those mediating the schizophrenia-like symptoms following perinatal administration. The consequences of PCP-induced neurotoxicity could be multifaceted, involving various compensatory and signaling mechanisms, including but not limited to altering the expression levels of the NMDAR in the membrane of surviving neurons. Several studies have reported that NMDA antagonists including PCP, MK-801 and ethanol are able to regulate the synaptic membrane expression levels of the NMDAR through changes in protein synthesis or trafficking of the NMDAR complex from intracellular compartments to the 69 membrane (Suvarna et al. 2005, Dong et al. 2004, Sircar et al. 1996, Anastasio & Johnson 2008b). Specifically, we have discovered that in developing rats, the membrane expression of NMDAR is up-regulated and that the composition of the receptor subunits is dependent on the treatment paradigm, i.e. PCP administration on PN7 causes NR1/NR2B to be up-regulated while PCP administration on PN7, 9, & 11 results in up-regulation of NR1/NR2A receptor protein (Anastasio & Johnson 2008b). These results parallel studies using 3Hglutamate binding to show increases in NMDAR density in the cingulate cortex, striatum, and hippocampus in PN7 rats 24 hrs following MK-801 (1mg/kg) administration (Gao & Tamminga 1994, McDonald et al. 1990b). Glutamate and glycine which promote opening and activation of the NMDA channel stimulate radioligand binding in well washed membrane preparations and inhibition by noncompetitive NMDAR antagonists is dependent on the presence of both agonists (Johnson et al. 1989, MacDonald et al. 1987). Therefore, since MK-801 binds deep within the NMDAR channel, which is influenced by the open state of the channel, it is possible to study the regulation and function of the NMDAR by measuring the binding of radiolabeled MK-801 (Johnson et al. 1989). Postnatal PCP administration (1 and 5 mg/kg on PN5-15) increased maximal agonist stimulated (100 µM glutamate + 100 µM glycine) 3HMK-801 binding in the hippocampus (~2 fold) and in the frontal cortex (~1.5 fold) compared to the saline control (Sircar 2003). Ethanol (2 g/kg x 5 days) increased the cortical expression of NR2B and agonist stimulated (100 µM glutamate + 100 µM glycine) 3H-MK-801binding in the frontal cortex, but not the hippocampus (Sircar & Sircar 2006). Further, the PCP-induced alterations in NMDAR expression and function may play a role in the development of adverse behaviors later in life, such as impairing the acquisition of spatial learning or the development of locomotor sensitization in response to PCP challenge (Anastasio & Johnson 2008a, Sircar 2003). 70 The exact mechanisms underlying the differential regulation of the NMDAR following acute or sub-chronic PCP administration and the relationship between NMDAR density and function are unknown in this animal model of schizophrenia. Therefore, the present study seeks to determine whether the apparent treatment dependent up-regulation of the NMDAR subunits corresponds to an increase in its functionality using a 3H-MK-801 binding assay. This study also sought to determine the subunit composition of the NMDAR responsible for changes in its function by measuring the inhibition of 3H-MK-801 binding by NR2A and NR2B selective inhibitors in saline and PCP-treated rats. Materials and methods Animals. Timed, day 14 pregnant female Sprague-Dawley rats were obtained from Charles River Laboratories (Wilmington, MA). The dams were housed individually with a regular 12h light-dark cycle (lights on 0700, off at 1900) with food and water ad libitum. Following parturition, male and female pups from four dams were combined and randomly cross-fostered to one of the four lactating dams. Each litter consisted of ten to twelve pups. Pups were treated with 10 mg/kg PCP on PN7 or on PN7, 9 and 11 and killed by decapitation in experiments described below. All experiments were conducted in accordance with the NIH and the University of Texas Medical Branch at Galveston Institutional Animal Care and Use Committee. Drugs. PCP was acquired from the National Institute on Drug Abuse (NIDA, Rockville, MD) and dissolved in 0.9% NaCl. NVP-AAM007 was a generous gift provided to us by Dr. Yves Auberson (Novartis Institute for Biomedical Research, Basel, Switzerland). [[[(1S)-1-(4-Bromophenyl) ethyl] amino] (1, 2, 3, 4- tetrahydro-2, 3-dioxo-5-quinoxalinyl) methyl] phosphonic acid tetrasodium 71 hydrate (PEAQX) and ifenprodil (+)-tartrate salt were purchased from SigmaAldrich (St. Louis, MO) and dissolved in 0.9% NaCl. Injections were administered s.c. in 1 mL/kg of vehicle. 3H-MK-801 was purchased from Perkin Elmer (Waltham, MA) with a specific activity of 22 Ci/mmol. Experimental design. Male and female rat pups were treated on either PN7 (acute) or on PN 7, 9, and 11 (sub-chronic) with 10 mg/kg subcutaneous (s.c.) PCP or saline. In the acute studies, pups were sacrificed by decapitation 24 hours following saline or PCP on PN7. In the sub-chronic studies, pups were sacrificed by decapitation 24 hours following the last injection of the aforementioned drug regimens on PN7, 9 and 11. The frontal cortex was dissected from 2 mm sections corresponding to 4.7 to 2.7 mm anterior to Bregma. 3H-MK-801 binding. The buffy coat preparation exhibits pharmacological characteristics similar to the electrophysiologically defined NMDAR; therefore, agonist stimulated 3HMK-801 binding represents a biochemical assay that allows a partial characterization of functional properties of the NMDAR complex (Jones et al. 1989). Since the glutamate and glycine binding sites exist on the NR2 and NR1 subunits, respectively, it was anticipated that increased functionality (increased channel opening associated with increased effects of either glutamate or glycine on ligand binding) will reflect changes in NR1 and NR2 subunit function. Buffy coat membranes from the frontal cortex were prepared according to previous publications with minor modifications (Jones et al. 1989, Johnson et al. 1993). The tissue was homogenized in 20 vol 0.32 M sucrose and centrifuged at 1000 x g for 10 min. The supernatant was collected and centrifuged at 20,000 x g for 10 min. The P2 pellet was resuspended in 20 vol ice cold dH 2O and centrifuged at 8000 x g for 10 min. The supernatant and buffy coat were 72 collected and centrifuged at 48,000 x g for 20 min. The P4 pellet was resuspended in 20 vol of ice cold dH2O and centrifuged at 48,000 x g for 20 min. This pellet (P5) was frozen at -20oC and stored for 1-7 days. On the day of use, the pellet was thawed and resuspended in 40 vol dH2O, incubated at 37oC for 20 min and centrifuged at 48,000 x g for 10 min. This pellet (P6) was resuspended in 40 vol dH2O and centrifuged at 48,000 x g for 10 min two more times before final resuspension in 10 mM HEPES. For the 3H-MK-801 binding assay, aliquots of the homogenate (40 µg protein/tube) were added to tubes containing 5 nM 3H-MK-801 (Perkin Elmer, Boston, MA) and the appropriate concentrations of test drugs in 10 mM HEPES (pH 7.4, 25oC) for a total volume of 1mL per tube. Basal binding was determined in the presence of 30 µM 7-chlorokynurenic acid (7-Cl KYNA, a glycine antagonist) and 1 mM (2R)-amino-5-phosphonovaleric acid (APV, a specific NMDAR antagonist); nonspecific binding was determined in the presence of 100 µM PCP. Samples were incubated for 2 hrs at 25 oC and the binding reaction was terminated by vacuum filtration over GF/C glass fiber filters. The filters were soaked in 0.03% polyethylenimine to reduce filter binding. Filtration was followed by two 5 mL washes of ice-cold buffer and retained radioactivity was measured by liquid scintillation spectrometry. Total protein concentrations were determined using the BCA (bicinchoninic acid) protein assay© (Pierce Chemical, Rockford, IL). Experiments were repeated a minimum of three times. Possible differences in specific binding values between saline and treatment were determined by Student’s t-test; statistical values of p<0.05 were considered significant. Preliminary studies determined that it was necessary to pool two frontal cortices from PN8 or PN12 pups in order to obtain adequate CPM (counts per minute) and binding levels similar to that obtained from adult cortical synaptosomal preparations. Further, tissue preparation involved multiple washes to facilitate removal of endogenous glutamate, Mg2+, and glycine so that the effects of exogenously added glutamate and glycine could be detected. 73 Specificity of radioligand binding was verified through MK-801 and PCP competition assays. The concentration of 3H-MK-801 used is near the Kd value most commonly reported (4.92 nM) and as such, changes in binding could be the result of changes in the Kd or Bmax for the MK-801 binding site. Under these conditions, this, in turn, could be influenced by changes in the K d or Bmax of either the glutamate or glycine receptor sites. Results In order to determine potential changes in NMDAR functionality following PCP administration, 3H-MK-801 binding was studied under different conditions and with different inhibitors, selective for either NR2A or NR2B. In rats acutely treated with PCP, maximal 3H-MK-801 binding following agonist stimulation (100 µM NMDA + 30 µM glycine) was significantly higher (approximately three-fold) than in saline treated controls (Figure 4.1). following 100 µM NMDA + 30 µM glycine Maximal 3H-MK-801 binding stimulation was also significantly greater in the sub-chronic PCP treated animals compared to their saline controls (1113.93 ± 121.79 pmol/mg protein versus 760.14 ± 75.57 pmol/mg protein, respectively), albeit to a lesser extent than in the acute treated animals (Figure 4.2). 74 Figure 4.1. Effects of agonist stimulation (100 µM NMDA + 30 µM glycine) on 3H-MK-801 binding in the frontal cortex of saline and PN7 PCP treated rat pups. PCP treatment resulted in a significant increase in agonist stimulated 3H-MK-801 binding in the frontal cortex of PN7 treated rat pups compared to saline treated animals. Animals were sacrificed 24 hours after treatment. Samples were run in triplicate, N=4/treatment group. *p<0.05 vs. saline stimulated (Student’s t-test) 75 Figure 4.2. Effects of agonist (100 µM NMDA + 30 µM glycine) stimulation on 3H-MK-801 binding in the frontal cortex of PN7, 9, & 11 PCP treated rat pups. PCP treatment resulted in a significant increase in agonist stimulated 3HMK-801 binding in the frontal cortex of PN7, 9, & 11 treated rat pups compared to saline control animals. Animals were sacrificed 24 hours after treatment. Samples run in triplicate, N=7/treatment group. *p<0.05 vs. saline stimulated (Student’s t-test) 76 To determine the subunit composition which underlies the observed increase in maximal 3H-MK-801 binding, we performed inhibition studies with selective NR2B (ifenprodil, 10 nM-100 µM) and NR2A antagonists [NVP-AAM007 (1 nM-10 µM) and PEAQX (10 nM-100 µM)]. The rationale for this experiment was that if increased binding following treatment was mostly due to increases in either NR2A or NR2B, then the 3H-MK-801 binding would be more susceptible to either a selective NR2A or NR2B antagonist. No difference in ifenprodil IC50 values due to acute PCP treatment was measured (Figure 4.3); however, specific 3H-MK-801 binding in the presence of 10 nM ifenprodil shows that there is a significant decrease (~57%) in specific binding compared to control (no inhibitor) experiments in the animals administered PCP on PN7, while no effect on specific binding was observed in the saline treated animals compared to control (Figures 4.3). For the sub-chronic PCP treated animals, maximal 3H- MK-801 binding was not different between saline or PCP treated animals compared to control experiments; also, no difference in IC 50 values (saline=10.32 µM; PCP=15.87 µM) was measured (Figures 4.4). Inhibition of 3H-MK-801 binding by the NR2A-preferring antagonist NVP-AAM007 caused no significant difference in specific binding in saline treated animals compared to control, but did cause a ~34% decrease in inhibition in maximal binding in the PCP treated group compared to control binding. Since there was not a dose response, an IC50 could not be determined (Figure 4.5). Similar results were obtained with PEAQX inhibition, an additional NR2A-preferring antagonist (Figure 4.6). 77 Figure 4.3. 3H-MK-801 binding inhibition by the NR2B selective antagonist ifenprodil in acute PCP treated animals. Agonist stimulated (100 µM NMDA + 30 µM glycine) 3H-MK-801 binding detected no significant difference in apparent affinity for ifenprodil between saline and acute PCP treatment (IC50=10.71 µM and 8.05 µM, respectively). Control binding was determined in the presence of 100 µM NMDA + 30 µM glycine without ifenprodil. N=4/treatment group. 78 Samples run in triplicate, Figure 4.4. 3H-MK-801 binding inhibition by the NR2B selective antagonist ifenprodil in sub-chronic PCP treated animals. Agonist stimulated (100 µM NMDA + 30 µM glycine) 3H-MK-801 binding detected no significant difference in apparent affinity for ifenprodil between saline and sub-chronic PCP treatment (saline IC50=10.32 µM; PCP IC50=15.87 µM). Control binding was determined in the presence of 100 µM NMDA + 30 µM glycine without ifenprodil. Samples were run in triplicate, N=4/treatment group. 79 Figure 4.5. 3H-MK-801 binding inhibition by the NR2A selective antagonist NVP-AAM007. Agonist stimulated (100 µM NMDA + 30 µM glycine) 3H-MK-801 binding detected no NVP-AAM007 dose response in both saline and sub-chronic PCP treatment. Control binding was determined in the presence of 100 µM NMDA + 30 µM glycine without NVP-AAM007. Samples were run in triplicate, N=4/treatment group. 80 Figure 4.6. PEAQX. 3H-MK-801 displacement by the NR2A preferring antagonist Agonist stimulated (100 µM NMDA + 30 µM glycine) 3H-MK-801 binding detected no PEAQX dose response in either saline or sub-chronic PCP treated rat pups. Control binding was determined in the presence of 100 µM NMDA + 30 µM glycine without PEAQX. Samples run in triplicate, N=4/treatment group. 81 Discussion Glutamatergic neurotransmission during early postnatal development is primarily mediated by the NMDAR in the frontal cortex (Ben-Ari et al. 1997). Blockade of the NMDAR during this stage of development with PCP causes a robust increase in cortical neurotoxicity (Wang et al. 2001, Wang & Johnson 2005), presumably resulting in a compensatory response to maintain synaptic transmission in the surviving neurons, such as an increase in synaptic expression of the NMDAR. We have previously observed that acute PCP treatment increased membrane levels of NR1 and NR2B protein in the frontal cortex, while no effect on NR2A levels was detected (Anastasio & Johnson 2008b). Conversely, sub-chronic PCP treatment stimulated an increase in NR1 and NR2A expression in membrane fractions of the frontal cortex, while no effect on NR2B expression was measured (Anastasio & Johnson 2008b) . Here we investigated whether this apparent up-regulation in receptor density corresponds to an alteration in receptor function as measured by glutamate and glycinestimulated 3H-MK-801 binding. We discovered that upon agonist stimulation, there was a significant increase in the maximal binding 3H-MK-801 binding in the frontal cortex of both acute (~ 3 fold) and sub-chronic PCP (~1.5 fold) treated rat pups. The difference between 3H-MK-801 binding levels between the day 8 controls and day 12 controls is most likely due to maturation of the brain and/or the NMDAR, e.g. changes in the probability of channel opening. Nonetheless, the increase in binding in the PCP treated animals is consistent with acute PCPinduced up-regulation of membrane NR1/NR2B protein expression as well as the increase in NR1/NR2A membrane protein levels measured following sub-chronic PCP administration (Anastasio & Johnson 2008b). Thus, this supports the hypothesis that the newly inserted NMDAR subunits in the membrane following PCP administration are functionally active. Next, to determine the NMDAR subunit composition responsible for the increase in receptor function and to verify previous Western blot experiments 82 (Anastasio & Johnson 2008b), we performed inhibition studies with selective NR2 subunit antagonists. Ifenprodil is a neuroprotectant which acts as an NMDAR antagonist by blocking the polyamine site on the NR2B subunit (Williams 2001, Reynolds & Miller 1989). Ifenprodil has been shown to inhibit 3H-MK-801 binding in a biphasic fashion (Reynolds & Miller 1989). The high affinity phase (Ki ~ 15nM) represents binding to the polyamine site and accounts for 50-60% of total 3H-MK-801 binding in the presence of 100 µM glutamate; however, the addition of 30 µM glycine reduces total binding due to the high affinity phase to 20% without altering ifenprodil affinity for the polyamine site (Reynolds & Miller 1989). The low affinity phase (Ki ~ 20-40 µM) is regulated by binding to the Zn2+ site on the NR2B subunit (Reynolds & Miller 1989). Inhibition of 3H-MK-801 binding by the lowest concentration of ifenprodil tested (10nM) decreased maximal binding in the PCP treated animals to 43% of control experiments. The design of this experiment limits our interpretation of these data such that we cannot definitively determine if this effect is due to alterations in the polyamine site or the Zn 2+ site; therefore, experiments which address these concerns are currently ongoing and are designed to test a greater range of ifenprodil concentrations with the goal of elucidating the mechanism of ifenprodil inhibition in this assay. Nevertheless, due to the stark difference in ifenprodil inhibition in the acutely treated animals, this study may provide preliminary evidence that acute PCP administration alters the high affinity polyamine binding site on the NR2B for ifenprodil such that the newly inserted NR1/NR2B receptor function is more sensitive to ifenprodil inhibition. Additionally, this study may provide preliminary evidence for the presence of an increase in the triheteromeric NMDAR following a single injection of PCP. The presence of a single copy of NR2B (or NR2A) is adequate for ifenprodil binding (or selective NR2A antagonists) albeit to a lesser extent than in the presence of two copies of the NR2B subunit; therefore, no change in ifenprodil IC50 values following PCP administration does not signify that the 83 NR2B subunit is absent or nonfunctional, but suggests that it may have coassembled with NR2A (Hatton & Paoletti 2005). Interestingly, in the sub-chronic paradigm, ifenprodil maximally inhibited 3H-MK-801 binding in both the saline and PCP treated animals with no difference in IC50 values. This suggests that the increase in sub-chronic PCP specific binding is not mediated through NR2B-containing receptors and is most likely through the NR2A-containing receptors, since this is the most commonly expressed NMDAR composition in the frontal cortex (Cull-Candy et al. 2001). This is supported by our previous study which reported that sub-chronic PCP administration up-regulates the membrane levels of NR1/NR2A subunit in the cortex three-fold, but does not alter the protein expression levels of NR2B (Anastasio & Johnson 2008b). Further, inhibition by the NR2A antagonist should produce a lower IC50 in the sub-chronic PCP treated animals compared to saline (Anastasio & Johnson 2008b); however, no dose response was observed with the NR2A antagonists, NVP-AAM007 or its diastereomer PEAQX; therefore, no IC50 values could be determined. NVP-AAM007 and PEAQX are considered to be competitive antagonists for the glutamate site on the NR2A subunit; therefore, the lack of a dose response may in part be due to the concentration of NMDA applied in this assay (Neyton & Paoletti 2006). Future experiments are currently ongoing which tests a lower concentration of NMDA that still activates the receptor, but does not compete with and inhibit the actions of NVP-AAM007 or PEAQX as well as experiments which are designed to test a greater range of NR2A antagonist concentrations. We also plan to determine the effects of NR2A inhibition on 3H-MK-801 binding in the cortex of animals treated with PCP on PN7. We anticipate no effect of NR2A inhibition on maximal binding because acute PCP selectively up-regulates NR1/NR2B membrane protein levels (Anastasio & Johnson 2008b). We must also acknowledge that while NVP-AAM007 and PEAQX are thought to be potent inhibitors of the NR2A-containing NMDARs, their ability to 84 discriminate between NR2A and NR2B-containing receptors in an in vitro assay is actually much smaller than originally reported by Liu et al., (2004b). In fact, several more recent studies have reported that the NVP-AAM007 IC50 values for NR2A and NR2B differ by approximately 9-fold and that PEAQX is ~12-fold more selective for NR2A than NR2B, far from the original 130-fold difference originally described (Feng et al. 2004, Neyton & Paoletti 2006, Frizelle et al. 2006, Liu et al. 2004b). The reason for this discrepancy is most likely due to differences in the level of glutamate occupancy of both NR2A and NR2B. Glutamate has a higher affinity for NR1/NR2B compared to NR1/NR2A (Cull-Candy et al. 2001, Laurie & Seeburg 1994, Neyton & Paoletti 2006), thus, to achieve a similar level of activation a higher level of glutamate should be applied at NR1/NR2A receptors than at NR1/NR2B (Neyton & Paoletti 2006). To study the effects of NVP-AAM007, a competitive and irreversible inhibitor of the glutamate site (Frizelle et al. 2006), Liu et al. (2004b) stimulated NR1/NR2A receptors with 2 µM glutamate and NR1/NR2B receptors with 5 µM glutamate resulting in their report of a greater subunit selectivity for NR2A than NR2B. However, NR1/NR2A receptors were most likely not fully activated in that experiment; therefore, the interpretation of the results is biased. Thus, precaution must be taken in to account when interpreting results from experiments obtained with these incompletely understood pharmacological tools. The development of a highly selective and potent NR2A antagonist is desperately needed and would exponentially advance this field. In conclusion, postnatal PCP administration results in a compensatory increase in functional NMDARs in the synaptic membrane in the frontal cortex of developing rat pups. The functional consequences of this up-regulation and role it plays in altering cortical function, as well as the development of abnormal schizophrenic-like behaviors will be addressed in subsequent studies. 85 Chapter 5: Atypical Antischizophrenic Drugs Prevent Changes in Cortical NMDARs and Behavior Following Sub-chronic PCP Administration We sought to determine the relationship between PCP-induced alterations in behavior and NMDAR expression in the cortex by examining the effect of antischizophrenic drug treatment on both. Sprague-Dawley rat pups were pretreated with risperidone or olanzapine 30 min prior to treatment with PCP on PN7 or sub-chronically on PN7, 9, & 11. Pre-pulse inhibition (PPI) of acoustic startle was measured on PN24-26 and following a challenge dose of 4 mg/kg PCP, locomotor activity was measured on PN28-35. PCP treatment on PN7 did not cause a deficit in PPI, but did cause locomotor sensitization. This was prevented by both antipsychotics. Further, PCP treatment on PN7 caused an upregulation of NR1 and NR2B, but this was not affected by either antischizophrenic drug. On the other hand, PCP treatment on PN7, 9, & 11 caused a deficit in PPI and a sensitized locomotor response to PCP challenge as well as an up-regulation of NR1 and NR2A, all of which were prevented by both atypical antischizophrenic drugs. These data support the hypothesis that subchronic, but not single injection PCP treatment to developing rats results in behavioral alterations that are sensitive to antipsychotic drugs and these behavioral changes observed could be related to up-regulation of cortical NR1 and NR2A receptors. Introduction Schizophrenia is a severe neuropsychiatric disorder which afflicts approximately 1% of the population worldwide and shows strong genetic tendencies, with symptoms first presenting in early adulthood (Lewis & Lieberman 2000, Bromet & Fennig 1999). The disease is characterized by the presence of both positive, e.g. paranoia, hallucinations, delusions, and negative 86 symptoms, including but not limited to emotional and social withdrawal, anhedonia, and depression, as well as cognitive impairments such as memory and attention deficits (McGlashan 1996a). PCP intoxication in humans has been shown to mimic both the positive and negative symptoms of schizophrenia as well as exacerbate psychosis in schizophrenics. These psychotomimetic properties led researchers to examine the effects of PCP in animals (Luby et al. 1962, Javitt & Zukin 1991). PCP administration to rats results in increased locomotor activity, stereotypy, ataxia, head-weaving, circling and walking backwards (Steinpreis 1996, Castellani & Adams 1981, Braff & Geyer 1990, Martinez et al. 2000b, Geyer & Ellenbroek 2003). In general, alterations in motoric behaviors such as these are thought to model the positive symptoms of schizophrenia. N-methyl-D-aspartate receptor (NMDAR) antagonists (PCP and MK-801) have been shown to reproducibly disrupt PPI of acoustic startle in animals and are routinely used to model the sensorimotor gating deficits of schizophrenia (Geyer et al. 2001, Rasmussen et al. 2007). PPI of acoustic startle is a gauge for information processing in specific pathways that are known to be abnormal in schizophrenia (Bunney et al. 2000, Adams & Moghaddam 1998, Castellani & Adams 1981, Wang et al. 2001, Ellenbroek & Cools 2000). This deficit may contribute to the thought disorder and cognitive fragmentation characteristic of this disease (Braff & Geyer 1990). It is a measure of the reduction of the startle response when a smaller non-startling acoustic stimulus (pre-pulse) is presented 80-120 ms prior to the startling stimulus (pulse) (Swerdlow et al. 1994). The etiology of schizophrenia has been described as a neurodevelopmental disorder (Weinberger 1987, Weinberger 1996, Pilowsky et al. 1993). Neurodegeneration during early stages of development has been shown following PCP or MK-801 treatment in the cortex, hippocampus, and striatum, all of which are regions of the brain implicated in schizophrenia (Wang & Johnson 2005, Wang & Johnson 2007, Ikonomidou et al. 1999). In addition, 87 PCP treatment on PN7, results in neurodegeneration (positive silver staining) in the frontal cortex, striatum, and hippocampus within 9 hours of treatment (Wang & Johnson 2005, Wang & Johnson 2007). Accompanying increases in caspase3 immunoreactivity and terminal dUTP nick-end labeling (TUNEL) of broken DNA show this degeneration to be apoptotic in nature. Furthermore, administration of MK-801 and/or PCP to the neonate has been shown to produce aberrant behaviors later in development (Beninger et al. 2002, Wang et al. 2001) specifically, locomotor sensitization and deficits in PPI of acoustic startle were reported in postnatal (PN24-28) rats treated with PCP on PN7, 9, & 11 (Wang et al. 2001). While it is generally acknowledged that the schizophrenic “break” does not often occur before puberty, there is evidence that this does occur in some cases (Ross et al. 2006b, Nicolson et al. 2000). Further, when examined retrospectively, there is ample evidence of abnormalities such as poor academic performance and poor social interaction skills in children who are eventually diagnosed as schizophrenic. This laboratory and others have demonstrated that this model (PCP treatment on PN7, 9, & 11) has face validity in that it results in behavioral deficits in rats similar to those seen in schizophrenia, including deficits in spatial learning, PPI of acoustic startle and social behavior (Wiley et al. 2003a, Wiley et al. 2003b, Wang et al. 2001, Rasmussen et al. 2007, Harich et al. 2007a). Further, pretreatment with olanzapine was able to prevent both behavioral and cytotoxic indices of postnatal PCP administration, suggesting that this treatment paradigm is a suitable model of schizophrenia in rats (Wang et al. 2001) Up-regulation of the NR1 subunit of the NMDAR has been reported to be associated with PCP-induced behavioral changes (Wang et al., 2001); however, it is not known whether this is accompanied by commiserate increases in NR2 subunits, which would be necessary for altered receptor function (Kutsuwada et al. 1992, Monyer et al. 1994, Paoletti & Neyton 2007). Further, it is not known 88 whether behavioral changes following single dose PCP treatment on PN7 administration are associated with NMDAR up-regulation, and if so, whether these changes can also be modulated by antischizophrenic drugs. Therefore, in this study we determined the effect of PN7 and PN7, 9, 11 PCP administration on two behaviors thought to model different aspects of schizophrenia as well as on the levels of the three most abundant cortical and striatal NMDAR subunits (NR1, NR2A and NR2B). Finally, the relevance of the changes in behavior and NMDAR subunit protein as a model of schizophrenia was challenged by determining the effect of pretreatment with two anti-schizophrenic drugs, risperidone and olanzapine. Materials and Methods Animals. Timed, day 14 pregnant female Sprague-Dawley rats were obtained from Charles River Laboratories (Wilmington, MA). The dams were housed individually with a regular 12h light-dark cycle (lights on 0700, off at 1900) with food and water ad libitum. Following parturition, male and female pups from four dams were combined and randomly cross-fostered to one of the four lactating dams. Each litter consisted of ten to twelve pups with approximately equal numbers of each gender. All experiments were conducted in accordance with the NIH and the Institutional Animal Care and Use Committee. Drugs. Phencyclidine was acquired from the National Institute on Drug Abuse (NIDA, Rockville, MD) and dissolved in 0.9% NaCl. Risperidone was obtained as a solution from Janssen Pharmaceutica (Titusville, NJ) and dissolved in 0.9% NaCl. Olanzapine was a generous gift from Eli Lilly and Company (Indianapolis, IN) and was dissolved in 0.1 N HCl and titrated to pH 7.0 with 0.1 N NaOH and finally diluted with 0.9% NaCl. Doses were chosen based on prior experiments 89 that addressed PCP-induced regulation of the NMDAR (Wang et al. 2001) and our own preliminary experiments. Experimental design. Male and female rat pups were treated on either PN7 or on PN 7, 9, and 11 (sub-chronic) with 10 mg/kg PCP or saline vehicle (s.c). Olanzapine (1 mg/kg, s.c.) or risperidone (0.25 mg/kg, s.c.) were administered 30 minutes prior to PCP or saline administration on PN7 or on PN 7, 9, 11. Pups were sacrificed by decapitation on PN7 at 24 hours following saline/vehicle (control, time=0 hours), PCP/vehicle, antagonist/vehicle, or antagonist/PCP treatment. In a separate experiment, pups were sacrificed by decapitation 24 hours following the last injection of the aforementioned drug regimens on PN7, 9 and 11 (on PN12). For biochemical studies, the frontal cortex or striatum was dissected as described below and used for Western blot analysis. In behavioral experiments, animals were assessed for PPI of acoustic startle on PN24-26 and then tested for locomotor activity following a 4 mg/kg PCP (i.p.) challenge on PN28-35. We chose to investigate the frontal cortex and striatum because of the prominent role these two brain regions play in the pathophysiology of schizophrenia. Furthermore, the frontal cortex and striatum are part of the brain circuitry involved in the expression of both PPI (Koch & Bubser 1994, Swerdlow et al. 1995, Ellenbroek et al. 1996) and locomotor sensitization (Pierce & Kalivas 1997). Sub-cellular fractionation. Protein extracts were prepared from the frontal cortex or striatal brain tissue as previously described with some modifications (Wang et al. 2001, Anastasio & Johnson 2008b). Briefly, 2 mm sections corresponding to 4.7 to 2.7 mm anterior to Bregma for the frontal cortex and 0.7 mm to -1.3 mm for the striatum (Paxinos & Watson 1986) were cut with the aid of an aluminum brain mold. Cortical brain sections were homogenized in 500 μL of lysis buffer with 90 the aid of an automatic tissue grinder (Kontes Pellet Pestle Motor, Kimble / Kontes, Vineland, New Jersey). The lysis buffer consisted of 10 mM HEPES (pH 7.4), 1 mM EDTA, 2 mM EGTA, and 500 μM DTT. Just prior to use, protease inhibitor cocktail [4-(2-aminoethyl) benzenesulfonyl fluoride (AEBSF), pepstatin A, E-64, bestatin, leupeptin, and aprotinin without metal chelators (Sigma-Aldrich, St Louis, MO)] at a concentration of 10 μL/mL was added to the lysis buffer. The homogenate was then centrifuged at 1000 x g at 4oC for 10 minutes to pellet the nuclear protein fraction (P1). The supernatant (S1) was collected and centrifuged at 8000 x g at 4oC for 30 minutes to pellet the membrane protein fraction (P2). The membrane fraction was re-suspended in homogenization buffer and centrifuged at 20,000 x g at 4oC for 30 minutes; the resultant pellet was re-suspended in lysis buffer + 1% SDS, boiled for 10 minutes and stored at 80oC. Western blot analysis. Equal amounts of protein were separated on 10% Bis-Tris gels (Invitrogen, NY) using SDS-PAGE with a MES-SDS running buffer system, pH 7.4. Following electrophoresis (110 V for 2 hours), proteins were transferred to polyvinylidene difluoride (PVDF) membranes (0.2 μm) in a Mini Electrotransfer Unit (Bio-Rad, Hercules, CA) overnight. The membrane was blocked in 5% nonfat milk, followed by incubation with the primary antibody in 1% milk for 2 hours at room temperature. Following washes (3 x 10 minutes) in TBS+0.1% Tween 20 (TBST), the membrane was incubated with horseradish peroxidase conjugated secondary antibodies for 1 hour at room temperature. Analysis was carried out using the enhanced chemiluminescence (ECL) plus Western blotting detection reagents (Amersham Biosciences, Piscataway, NJ). corresponding to the various proteins of The bands interest were scanned and densitometrically analyzed by using an automatic imaging analysis system (Alpha Innotech Corporation, San Leandro, CA). All quantitative analyses were 91 normalized to β-actin (after stripping [Reblot mild, Chemicon International, Temecula, CA]). Antibodies. The monoclonal anti-NR1, anti-NR2A, and anti-NR2B were purchased from BD Biosciences (San Jose, CA). Anti-actin antibody was obtained from Chemicon International (Temecula, CA). Primary antibody dilution was 1:5001:1000. Secondary antibodies were purchased from Zymed (Invitrogen Corporation, Carlsbad, CA) and used at a concentration of 1:5000. Pre-pulse inhibition (PPI) of acoustic startle. Measurement of PPI of acoustic startle was performed according to previously published procedures with minor modifications (Wang et al. 2001, Wang et al. 2003). Testing was performed between 0900 and 1600 hours as described below. Male and female rat pups (PN24-26) were transferred into a small sound-attenuated, dedicated behavior room on the day of testing and allowed to acclimate to the room for 20 minutes. Animals were then placed into one of three startle chambers (SR-Lab, San Diego Instruments, San Diego, CA) with a background noise level of 65 dB. Following a 10 minute acclimation period, rats were exposed to three randomly administered stimuli: no stimulus, a 73 dB 20 ms pre-pulse 100 ms prior to a 120 dB pulse, or a 120 dB 40 ms pulse alone with a variable inter-trial interval (5-20 sec) for a total of 63 trials (21 no stimulus, 21 pulse alone, and 21 pre-pulse + pulse). % PPI of acoustic startle was calculated as the [pulse-(pre-pulse + pulse)]/pulse x 100. Locomotor Activity. On the day of testing animals were placed in locomotor chamber boxes and allowed to habituate for 30 minutes prior to a 4 mg/kg challenge dose of PCP (i.p.). Locomotor activity was measured for an additional 90 minutes via an 92 open-field activity system (San Diego Instruments, San Diego, CA) which consisted of a square enclosure with Plexiglas walls (40 x 40 x 40 cm). Horizontal activity was measured with a 16 x 16 photobeam matrix which recorded both central and peripheral activity in 5 min bins. Statistical analysis. Group comparisons were specifically defined before the beginning of each experiment; therefore, planned comparisons were performed instead of an overall F test in a multifactorial ANOVA (Keppel 1982). Statistical comparisons for each experiment were conducted using a one-way ANOVA. All values are presented as mean ± SEM. The null hypothesis was rejected at p<0.05. Results PCP administration in adult rats causes substantial impairments in normal behavior (Hanania et al. 1999, Phillips et al. 2001, Geyer et al. 2001). In perinatal rats, 10 mg/kg PCP results in significant reduction of normal behaviors, most notably, a reduction of suckling behavior. This lasts approximately 6-8 hours and causes a concomitant weight loss, especially in male pups. While females regain the lost weight within 24 hrs, the males do not; however, at the time of behavioral testing, there is no significant difference in weight between saline and PCP treated animals of either gender (Table 5.1). All experimental groups consisted of equal numbers of males and females. 93 Table 5.1 Effects of PCP (10 mg/kg) on weight (g) gain in developing rats PN7 PN8 PN9 PN10 PN11 PN12 PN28 14.3±0.7 19.7±0.2 17.4±1.2 23.7±0.5 20.9±1.5 29.1±0.7 81.1±2. 8 14.7±0.8 17.3±0.6* 16.5±0.8 21.4±0.4* 19.9±1.3 24.9±1.5 79.2±4 16.2±0.6 21.2±0.4 20.7±0.8 26.4±0.6 25.5±1.1 31.5±0.6 91.2±3.5 15.9±0.8 17.7±0.5^ 17.5±0.8^ 21.9±0.7^ Data presented as mean (g) ±SEM *p<0.05 vs. saline female N=6-11/group (Student’s t-test) ^p<0.05 vs. saline male N=6-13/ group (Student’s t-test) 20.6±1.1^ 23.8±0.3^ 85.6±4.6 Saline female PCP female Saline male PCP male 94 PCP treatment on PN7 had no significant effect on PPI (F 3, 31=2.264, NS), suggesting that acute neurotoxicity previously observed (Wang & Johnson 2007) is not sufficient to alter this behavior (Figure 5.1). Further, PCP treatment on PN7 had no effect on the startle amplitude (data not shown). However, we found that PCP treatment on PN7 caused a significantly sensitized locomotor response to PCP challenge on PN28-35 that was prevented by either olanzapine (F3,31=8.071, p<0.05) or risperidone (F3,31=10.001, p<0.05) (Figure 5.2). As with PCP treatment on PN7, treatment on PN7, 9, & 11 produced no significant effect on startle amplitude (data not shown). On the other hand, PCP treatment on PN7, 9, & 11 resulted in a significant deficit in PPI of acoustic startle measured on PN24-26, which was blocked by pretreatment with either olanzapine (F3,31=4.194, p<0.05) or risperidone (F3,31=2.852, p<0.05) (Figure 5.3). Previous studies from this laboratory reported that the atypical antipsychotic drug, olanzapine, prevented sensitization to the locomotor activating effects of PCP challenge with 2 mg/kg on PN42 as well as the inhibition of baseline pre-pulse inhibition of acoustic startle on PN24-28 in female pups (Wang et al. 2001). This experiment was repeated using the present design which also included male pups in order to exclude any gender related differences. Further, this design was extended to risperidone, which has some atypical properties at low doses. For these studies, animals treated sub- chronically with PCP and then challenged with 4 mg/kg PCP on PN28-35, showed enhanced locomotor activity compared to saline treated animals (Figure 5.4). p<0.05) Both olanzapine (F3,31=5.920, p<0.05) and risperidone (F3,31=5.044, pretreatment on PN7, 9, & 11 prevented PCP-induced locomotor sensitization measured on PN28-35 with no effect of their own (Figure 5.4). 95 Figure 5.1. Effects of PCP administration (PN7 only) on PPI of acoustic startle. PCP (10 mg/kg) treatment on PN7 does not produce a significant deficit in PPI of acoustic startle as measured on PN24-26. N=8 in both control and experimental groups. 96 Figure 5.2. Effects of PCP administration (PN7 only) the development of locomotor sensitization. Locomotor sensitization induced by a 4 mg/kg challenge to PCP treatment on PN7 treated animals as measured on PN28-35. Pretreatment on PN7 with olanzapine (1 mg/kg) or risperidone (0.25 mg/kg) inhibits the development of locomotor sensitization N=8/group (top). Time- course of locomotor activity (bottom) *p<0.05 vs. saline (one-way ANOVA with Bonferroni’s post hoc test). N=8 in both control and experimental groups. ●-saline; ○-10 mg/kg PCP; ▼-1 mg/kg olanzapine; ∆-olanzapine + PCP; ■-0.25 mg/kg risperidone; □-risperidone + PCP 97 Figure 5.3. Effects of subchronic PCP administration (PN7, 9 & 11) on PPI of acoustic startle. PCP treatment (10 mg/kg) treatment on PN7, 9, & 11 results in a deficit in PPI of acoustic startle as measured on PN24-26. Pretreatment on PN7, 9, & 11 with olanzapine (1 mg/kg) or risperidone (0.25 mg/kg) inhibits the PCP-induced deficit in PPI of acoustic startle. *p<0.05 vs. saline (one-way ANOVA with Bonferroni’s post hoc test). N=8 in both control and experimental groups. 98 Figure 5.4. Effects of subchronic PCP administration (PN7, 9 & 11) on the development of locomotor sensitization. Locomotor sensitization induced by a 4 mg/kg challenge to PCP treatment on PN7, 9, & 11 treated animals as measured on PN28-35. Pretreatment on PN7, 9, & 11 with olanzapine (1 mg/kg) or risperidone (0.25 mg/kg) inhibits the development of locomotor sensitization. (top) Time course of locomotor activity (bottom) *p<0.05 vs. saline (one-way ANOVA with Bonferroni’s post hoc test). N=8 in both control and experimental groups. ●-saline; ○-10 mg/kg PCP; ▼-1 mg/kg olanzapine; ∆-olanzapine + PCP; ■-0.25 mg/kg risperidone; □-risperidone + PCP 99 In order to delineate one possible biochemical mechanism underlying the above mentioned behavioral changes, we determined the effects of PCP treatment on PN7 or on PN7, 9, & 11 on the density of NR1, NR2A, and NR2B in the synaptosomal membrane fraction of the frontal cortex and striatum. Quantitative western analysis revealed that PCP treatment on PN7 produced a 3fold increase in membrane bound NR1 and NR2B subunits in the frontal cortex 24 hours after PCP administration, while no effect on NR2A was observed (Anastasio & Johnson 2008b). In another experiment, perinatal animals were treated with either olanzapine (1 mg/kg) or risperidone (0.25 mg/kg) 30 minutes prior to PCP treatment on PN7. Twenty-four hours after the PCP injection, the rats were killed and the density of NMDARs was determined in the cortical membrane fraction. Pretreatment with either olanzapine or risperidone did not inhibit the up-regulation of membrane cortical NR1 or NR2B induced by PCP treatment on PN7 (Figure 5.5). Furthermore, treatment with olanzapine or risperidone alone had no effect on the concentration of membrane NR1 or NR2B in the frontal cortex compared to saline controls (data not shown). PCP treatment on PN7, 9, & 11 treatment caused a 3-fold increase in membrane NR1 and a 10-fold increase in NR2A protein levels in the frontal cortex with no effect on NR2B protein expression (Anastasio & Johnson 2008b). To analyze the actions of atypical antipsychotics on PCP-induced changes in the membrane protein levels of NMDAR subunits in the frontal cortex, animals were treated with olanzapine or risperidone 30 minutes prior to PCP on PN7, 9, & 11 and sacrificed 24 hours after the last of 3 injections. Each of the antipsychotics investigated inhibited PCP-induced up-regulation of the NR1 subunit in the membrane protein fraction of the frontal cortex (Figure 5.6), while having no effect on NR1 subunit expression on their own (data not shown). Pre-treatment with either olanzapine or risperidone also was able to completely block the increase in membrane cortical NR2A protein levels caused by PCP treatment on PN7, 9, & 11 treatment (Figure 5.6) with no effect on their own (data not shown). 100 PCP treatment on PN7 had no significant effect on NR1 or NR2B protein expression levels in the striatum at 24 hours following treatment (Figure 5.7). The effects of pretreatment with the antipsychotics on NR1 and NR2B protein levels in the striatum were also investigated following a single injection of PCP. Treatment with olanzapine or risperidone did not significantly alter expression of NR1 or NR2B protein levels in the striatum prior to PCP on PN7 at 24 hours following treatment (Figure 5.7) or when administered alone (data not shown). Similarly, treatment with either PCP or atypical antipsychotics did not alter striatal NR2A protein expression levels (data not shown). Unlike the up-regulation of NR1 observed in the frontal cortex, Western blot analysis of membrane bound protein showed that levels of striatal NR1 protein were significantly decreased following sub-chronic PCP treatment on PN7, 9, & 11 (Figure 5.8), with no effect on regulation of striatal NR2A (Figure 5.8) or NR2B (data not shown). Pretreatment with the anti-schizophrenic drug olanzapine, but not risperidone, prevented the down-regulation of NR1 protein expression in the striatum caused by sub-chronic PCP administration (Figure 5.8). Administration of these drugs alone had no effect on NR1 or NR2A protein levels in the striatum (data not shown). We also measured the levels of NR1, NR2A, and NR2B in the frontal cortex of animals following PCP challenge on PN28-35. No alterations in the protein levels of any of the subunits in the frontal cortex were evident in the animals treated sub-chronically with PCP (data not shown). 101 Figure 5.5. Pharmacological antagonism of PCP treatment on PN7 effects on NR1 and NR2B in the frontal cortex. Quantitative analysis reveals that antipsychotics pretreatment has no effect on PCP treatment on PN7-induced upregulation of NR1 or NR2B protein levels in the frontal cortex 24 hours following PCP (10 mg/kg, N=5-15/treatment). *p<0.05 vs. SAL NR1 (one-way ANOVA with Bonferroni's post hoc test) ^p<0.05 vs. SAL NR2B (one way ANOVA with Bonferroni’s post hoc test). 102 Figure 5.6. Pharmacological antagonism of PCP treatment on PN7, 9, & 11induced up-regulation on NR1 and NR2A in the frontal cortex. Quantitative analysis reveals that pretreatment with antipsychotics prevents PCP-induced (10 mg/kg, N=5-15/treatment) up-regulation of NR1 or NR2A protein in the frontal cortex. *p<0.05 vs. SAL NR1 (one-way ANOVA with Bonferroni's post hoc test) ^p<0.05 vs. SAL NR2A (one way ANOVA with Bonferroni’s post hoc test). 103 Figure 5.7. Effects of a single injection of PCP on PN7 on the membrane protein expression of NR1 and NR2B in the striatum. Quantitative analysis reveals that PCP treatment on PN7 has no effects on the expression of striatal NR1 or NR2B (10 mg/kg, N=5-15/treatment). 104 Figure 5.8. Antagonism of PCP treatment on PN7, 9, & 11-induced downregulation on NR1 in the striatum. pretreatment with olanzapine prevents Quantitative analysis reveals that PCP-induced (10 mg/kg, N=5- 15/treatment) down-regulation of NR1 in the striatum. PCP treatment had no effect on protein levels of NR2A *p<0.05 vs. SAL NR1 (one-way ANOVA with Bonferroni's post hoc test) 105 Discussion A number of genes related to glutamatergic function have been discovered that are significantly associated with schizophrenia, though in as yet undefined ways. Included in this list is NRG1 (neuregulin-1), which is known to regulate NMDAR expression (Chong et al. 2008, Craddock et al. 2005). DTNBP1 (dystrobrevin binding protein 1) has been shown to modulate glutamate function through up-regulation of presynaptic proteins and neurotrophic effects mediated by the Akt signaling pathway (Duan et al. 2007, Numakawa et al. 2004). DAOA (D-amino acid oxidase activator) activates NMDA receptors through a series of reactions involving the glycine-like molecule, D-serine (Korostishevsky et al. 2004, Ross et al. 2006a). RGS4 (regulator of G-protein signaling 4) is under-expressed in schizophrenic prefrontal cortex in postmortem microarray studies and has been reported to regulate G proteins in glutamate neurons, thereby dampening the effects of neurotransmitter interactions at Gprotein coupled receptors (Chowdari et al. 2002, Chowdari et al. 2008). In addition to the glutamate related genes above found with linkage analysis, several other genes putatively associated with the NMDA synapse have been discovered to be associated with schizophrenia, including GRM3 (mGluR3 a member of the group II metabotropic receptor family, which also includes mGluR2 (Egan et al. 2004); mGluR3 is known to modulate glutamate release. Thus, genetic evidence supports a role for alterations in various glutamatergic genes including those specific to NMDAR function in schizophrenia. Importantly, these data are strongly supported by pharmacological data that also imply a role for altered NMDAR function. However, the complexities of these data do not allow a direct comparison between the data in this model to what may occur in the human brain in schizophrenia. Our view is that animal models may reveal the gross structural features underlying behavioral alterations in rats that are similar to schizophrenia and possibly point to novel pharmacological approaches that may be helpful in treatment of the disease. 106 It is well known that acute PCP treatment produces a disruption in PPI in adult rats, similar to that seen in schizophrenic patients (e.g. (Martinez et al. 2000b, Mansbach & Geyer 1989). Typical antipsychotics, such as haloperidol, are not able to reverse deficits in PPI caused by acute PCP treatment in adult rats (Geyer et al. 2001) or in pre-pubertal rats (Martinez et al. 2002), but in adult rats, they can reverse the effects of dopamine agonists (Geyer et al. 2001). Atypical antipsychotics, including clozapine, olanzapine, and quetiapine, are effective at alleviating acute PCP inhibition of PPI in adult rats (Johansson et al. 1995, Martinez et al. 2002, Geyer et al. 2001, Ballmaier et al. 2001, Johansson et al. 1994), but not in pups (PN16-19) or pre-pubertal (PN45) rats (Martinez et al. 2002). However, olanzapine is effective at preventing the deficits observed in PPI in PN24-28 pups following PCP treatment on PN7, 9 and 11 (Wang et al. 2001). In addition, both olanzapine and risperidone are able to increase PPI in NR1 -/mice (Duncan et al. 2006). The current study shows that both olanzapine and risperidone pretreatment also blocks the PPI deficit observed in both male and female PN24-26 pups following PCP pretreatment on PN7, 9 and 11. In contrast, PCP treatment on PN7 administration did not produce a deficit in PPI in developing rat pups. It is then reasonable to postulate that PCP treatment on PN7, 9, & 11 produces a chronic deficit in NMDA receptor function compared to a single injection of PCP and that this more closely models the disease and the developmental NMDA hypofunction theory of schizophrenia (Duncan et al. 2006). Like other psychomotor stimulants, repeated administration of PCP causes a progressive augmentation of locomotor activity (Xu & Domino 1994), referred to as sensitization. The neuroadaptations associated with sensitization may be linked to the mechanisms underlying addiction (Robinson & Berridge 1993). Sensitization is also thought to be an important index related to psychosis as well as movement and thought disorders in schizophrenia (Robbins 1990). PCP-induced sensitization is blocked by haloperidol and risperidone (Kitaichi et al. 1995) and cross-sensitizes with MK-801 (Pechnick & Hiramatsu 1994), but not 107 with amphetamine (Balster 1989, Balster 1986). In the current study, PCP treatment on PN7 or on PN7, 9, & 11 produced locomotor sensitization in rats at PN28-35 that was blocked by pretreatment with either olanzapine or risperidone. Furthermore, the neurotoxicity evident in the developing frontal cortex following either a single injection or multiple injections suggests a role for altered cortical function in the development of this aberrant behavior (Wang & Johnson 2007, Wang & Johnson 2005, Wang et al. 2001). Our group and others have demonstrated that a single administration of PCP, MK-801 or ketamine to PN7 pups induces widespread neuronal apoptosis (Ikonomidou et al. 1999, Scallet et al. 2004, Young et al. 2005, Wang & Johnson 2007, Wang & Johnson 2005). Other laboratories have also reported that transient NMDAR blockade by acute PCP, MK-801, ketamine, and ethanol to rodents during development causes behavioral, structural, and molecular abnormalities in adulthood (Fredriksson & Archer 2004, Fredriksson & Archer 2003, Fredriksson et al. 2004, Wozniak et al. 2004, Harris et al. 2003). For example, Harris et al (2003) found that PN7 female rat pups administered MK801 (0.5 mg/kg, twice, 8 hours apart, s.c.) showed PPI deficits and increased locomotor activity accompanied by a reduction of brain volume and neuronal number within the hippocampus and altered hippocampal NR1 subunit expression. Several studies from this laboratory have investigated a possible mechanism by which PCP may elicit its neurotoxic effects and produce alterations in behavior in rats. In developing rats, PCP treatment on PN7, 9, & 11 of pups resulted in increased expression of NR1 mRNA in the frontal cortex, striatum, nucleus accumbens and olfactory cortex that was inhibited by pretreatment with the atypical antipsychotic olanzapine (Wang et al. 2001). These data are consistent with our previous report demonstrating that chronic PCP treatment resulted in increased NR1 immunoreactivity in the frontal cortex and striatum of adult rats treated chronically with PCP (Hanania et al. 1999). In 108 addition, recently we reported that PCP treatment on PN7 produces an upregulation of cortical NR1 and NR2B subunits via an increase in trafficking from intracellular compartments to the membrane, while subchronic PCP treatment results in an up-regulation of cortical NR1 and NR2A subunits by increasing new protein synthesis of these subunits (Anastasio & Johnson 2008b). We extended these experiments in this study and show that olanzapine and risperidone pretreatment is unable to prevent the up-regulation of cortical NR1 and NR2B subunits following PCP treatment on PN7 administration. These data suggest that NMDAR up-regulation in the cortex and subsequent locomotor sensitization following a single injection of PCP are independent of each other. This suggests that expression of sensitized behavior is dependent on mechanisms requiring activation of D2 and/or 5-HT2A/2C receptors. Thus, even though a sensitized behavioral response to acute PCP challenge appears to involve activation of D2 and/or 5-HT2 receptors, the increase in NMDAR trafficking appears to be independent of these receptors. Furthermore, the DA and 5-HT mechanisms involved in locomotor sensitization may be downstream of receptor regulation. If so, antipsychotics would be ineffective at preventing PCP-induced changes in receptor trafficking, but still capable of preventing PCP-induced sensitization and other behaviors. In contrast, both olanzapine and risperidone are able to prevent upregulation of NR1 and NR2A subunits in the frontal cortex following sub-chronic PCP treatment. These data suggest that up-regulation of NR1 and NR2A subunits (rather than NR1 and NR2B) may underlie the development of deficits in PPI following PCP treatment on PN7, 9, & 11, though the relative role of NMDAR subunits in locomotor behavior and PPI are not completely understood. Several studies have reported that blockade of NR2B subunits with selective antagonists (eliprodil and Ro63-1908) does not disrupt PPI (Depoortere et al. 1999, Wiley 1998, Higgins et al. 2003) and that it is the combined blockade of NR2A and NR2B subunits which is necessary to induce deficits in PPI as well as 109 hyperactivity in rodents (Spooren et al. 2004). Administration of the selective NR2A antagonist, NVP-AAM007, to adult rats did not disrupt PPI and resulted in hypolocomotor activity, while the NR2B antagonist, Ro 25-6981disrupted PPI and produced a dose-dependent hyperlocomotion (Chaperon et al. 2003). Thus, the role of NR2A and NR2B subunits in the detrimental behavioral effects of PCP merits further investigation. Neither the mechanisms underlying PCP-induced alterations in behavior nor NMDA receptor upregulation nor those responsible for the ability of olanzapine and risperidone to prevent these alterations are clear. Clozapine, olanzapine, and M100907, but not haloperidol, have been reported to prevent the blockade of NMDA responses in the medial prefrontal cortex caused by acute PCP administration (Arvanov & Wang 1999, Wang & Liang 1998). These data suggest a prominent role for 5-HT2A receptors in preventing the acute effect of PCP. Furthermore, clozapine has been shown to inhibit hypersensitive responses to NMDA following subchronic PCP (Arvanov & Wang 1999), suggesting that the expected increase in NMDAR function following PCP upregulation of NR1 and NR2A may also be prevented by olanzapine treatment. It is possible that the ability of olanzapine to inhibit PCP-induced neurotoxicity, NMDAR up-regulation and deficits in PPI following PCP treatment stems from its blockade of both DA and 5-HT2A receptors. Additionally, if PCP-induced neurotoxicity and the subsequent loss of these cortical neurons results in a hypoglutamatergic state, then the ability of antipsychotics to prevent this loss of glutamatergic tone through blockade of DA and 5-HT receptors may be related to their effectiveness in alleviating both positive and negative symptoms of schizophrenia (Jardemark et al. 2000). Understanding the mechanism by which olanzapine and risperidone prevent PCP-induced neuronal apoptosis could provide insights into the molecular and cellular mechanisms involved in the behavioral effects of PCP in rats, which in turn could provide insight into the etiology and pharmacotherapy of schizophrenia. 110 PCP treatment on PN7 had no effect on the expression of either PSD-95 (data not shown) or any of the NMDA receptor subunits in the striatum. PSD-95 interacts with the intracellular tail of NR2 subunits and is thought to be responsible for anchoring the functional NR1/NR2 receptor complex in the membrane (Wenthold et al. 2003). Thus, it is possible that the lack of an observable effect on NMDA receptor expression is related to the lack of effect on PSD-95. This suggests that the striatal neurotoxicity previously reported (Wang and Johnson, 2005) is unrelated to alterations in the expression of NMDAR protein. Similarly, the locomotor sensitization measured following a single injection of PCP must also be due to mechanisms other than changes in striatal NMDAR expression levels. However, this does not rule the possible role that altered NMDAR expression in the frontal cortex may play in the sensitization response. Pretreatment with olanzapine was able to prevent the down-regulation of striatal NR1 polypeptide that was caused by sub-chronic PCP administration; however, pretreatment with risperidone did not. We have recently observed that neither SCH23390 (selective D1 antagonist), sulpiride (selective D2 antagonist), nor M100907 (selective 5-HT2A antagonist) were able to prevent the downregulation of NR1 in the striatum (Anastasio and Johnson, unpublished observations). Thus, this effect of olanzapine may require blockade of both DA and 5-HT receptors. In addition to affinity for DA and 5-HT receptors, olanzapine possesses high affinity for muscarinic ACh receptors (Ki = 1.89 nM), H1 histamine receptors (Ki=7.14 nM), as well as α1 noradrenergic receptors (Ki=19 nM) (Arnt & Skarsfeldt 1998, Raggi et al. 2004); therefore, it is possible that in the striatum, an area rich in muscarinic ACh receptors, olanzapine’s effect of blocking down-regulation of NR1 caused by sub-chronic PCP administration to postnatal rats could also involve an action at these receptors. PN7-11 is a critical stage in brain development, with ample evidence of neurite growth and synapse formation, and is referred to as the brain growth 111 spurt (Olney et al. 2002). Thus, it is reasonable that even temporary changes during this critical period could result in behavioral changes as these animals mature. No variation in the expression of cortical NR1, NR2A, or NR2B was observed in either saline or sub-chronically PCP treated pups as measured immediately following PCP challenge and behavior measurement on PN28-35. Thus, it could be argued that the behavioral effects observed at this time are independent of the effects of PCP challenge on the expression of the NMDAR and that are more likely due to changes in NMDAR expression during an earlier, critical period of development and the subsequent maturation of the brain. Additionally, these results are consistent with the neurodevelopment theory of schizophrenia, which hypothesizes that damage during this early, critical stage of brain development may account for the later manifestation of mental disorders (du Bois & Huang 2007). 112 Chapter 6: Modeling the Negative Symptoms of Schizophrenia Disruptions in the glutamate system are thought to play a causative role in the pathogenesis of schizophrenia. PCP or “angel dust” is a drug of abuse, which blocks the NMDA receptor in several corticolimbic structures responsible for emotions, memory, and higher thought processes. PCP administration in humans has been shown to mimic both the positive and negative symptoms of schizophrenia. PCP administration in immature rats has been shown to cause neuronal cell death and as the rat matures, irregular behaviors become evident. The purpose of this study was to determine the effect of perinatal PCP treatment in rat models of the negative symptoms of schizophrenia. We incorporated two behavior models to accomplish this, the social interaction test and the social discrimination task. Male and female Sprague-Dawley rats were treated with 10 mg/kg PCP on PN7, 9, & 11 and were tested for social interaction on PN28 (prepubescent) and again on PN54 (post-pubescent) or were tested for social discrimination on PN58-60. Pre-pubescent males showed a significant reduction in social interaction, which was no longer evident when measured two weeks after the onset of puberty (PN54). PCP treatment of perinatal females had no effect on social interaction at either age. Both adult male and female rats showed a deficit in social discrimination, as marked by a reduction in the novelty discrimination index. These data support the use of sub-chronic PCP administration in perinatal rats as useful in modeling the negative symptoms of schizophrenia. Introduction Schizophrenia is a severe neuropsychiatric disorder characterized by the presence of both positive, e.g. paranoia, hallucinations, delusions, and negative symptoms, including but not restricted to social and emotional withdrawal, 113 anhedonia, and depression, as well as cognitive impairments such as memory and attention deficits (McGlashan 1996a, Koros et al. 2007). Moreover, the negative symptoms have a propensity to be more enveloping and relentless, and less sensitive to antipsychotic medications (Fenton & McGlashan 1991). PCP is well known to exacerbate psychoses in schizophrenics (Luby et al. 1962, Javitt & Zukin 1991, Lahti et al. 2001). Importantly, clinical observations have shown that PCP and ketamine intoxicated humans repeatedly present with symptoms which mimic the positive as well as several negative symptoms of schizophrenia, including social withdrawal. PCP animal models of this disease have been developed in order to replicate the various symptoms of schizophrenia and serve as investigatory tools for development of future therapeutic compounds. Hypofunction in the prefrontal cortex is thought to underlie the origins of the negative symptoms of the disease (Goff & Evins 1998). In addition, there is anatomical evidence of deficits “hypoglutamatergic” in nature. in cortical function that may be Glutamate promotes various phases of neuronal development, including migration, differentiation, and synaptic plasticity (Komuro & Rakic 1993). In the perinatal rat, the NMDAR is the primary mediator of glutamatergic excitatory neurotransmission in the brain and neurons expressing the NMDAR undergo a period of hypersensitivity to NMDAR blockade in which they are highly prone to excitotoxicity and neurodegeneration (Ben-Ari et al. 1997). Transient inactivation of NMDARs can be lethal for many neurons; administration of PCP or other noncompetitive NMDA antagonists, such as MK801 (dizocilpine), in the adult rat resulted in restricted neurotoxicity and structural damage in brain regions similar to those in which damage is present in schizophrenics (Olney et al., 1989; Olney and Farber, 1995b). PCP-mediated neurotoxicity in the prefrontal cortex, may underlie the aberrant schizophreniclike behaviors reported in various animal models of the disease. This laboratory has previously reported that sub-chronic PCP administration to developing rat pups can model the positive symptoms of 114 schizophrenia (enhanced locomotor activity and development of locomotor sensitization following PCP challenge) as well as deficits in pre-pulse inhibition of acoustic startle (Anastasio & Johnson 2008a, Wang et al. 2001), both of which can be alleviated by treatment with atypical antipsychotics, such as olanzapine and risperidone. Acute and repeated PCP, but not amphetamine treatment of rats, also results in deficits in social interaction (Sams-Dodd 1999, Sams-Dodd 1998) and cognitive deficits as measured by the delayed spatial alternation task (Koros et al. 2007, Wang et al. 2001, Wiley et al. 2003a). Chronic pre-treatment (21 days) with the atypical antipsychotic, clozapine, but not the typical antipsychotic haloperidol reversed the PCP (2 mg/kg x 3 days)-induced deficits in social behavior (Sams-Dodd 1996). An additional symptom characteristic of schizophrenia is a deficit in selective attention and information processing, i.e. the inability to differentiate relevant from irrelevant information (Goldberg & Gold 1995). The capacity of an adult rat to differentiate between a familiar and a novel juvenile in a social environment has been suggested to be a suitable animal model of selective attention deficits (Engelmann et al. 1995). Acute PCP administration to adult rats has been reported to produce a reduced novelty discrimination index [time spent investigating the familiar juvenile compared to time spent investigating novel juvenile] (Terranova et al. 2005). Further, adult rats which received PCP during the perinatal stage (PN7, 9, & 11) also present with a deficit in the novelty discrimination index (Depoortere et al. 2005, Terranova et al. 2005, Harich et al. 2007a). These deficits could be reversed with post-treatment with the atypical antipsychotic clozapine (Terranova et al. 2005), supporting this behavioral test as a suitable model of the attention processing deficits present in schizophrenia. There is a paucity of studies investigating the PCP perinatal model and its ability to mimic the negative symptoms of schizophrenia; therefore, the purpose of this study was to explore whether this specific sub-chronic PCP treatment paradigm models the negative symptoms of schizophrenia. Specifically, the 115 effect of perinatal PCP administration on social interaction was measured in preand post-pubescent rats and its effect on social discrimination was also determined when the pups were adults. Materials and Methods Animals. Timed, day 14 pregnant female Sprague-Dawley rats were obtained from Charles River Laboratories (Wilmington, MA). The dams were housed individually with a regular 12h light-dark cycle (lights on 0700, off at 1900) with food and water ad libitum. Following parturition, male and female pups from four dams were combined and randomly cross-fostered to one of the four lactating dams. Each litter consisted of ten to twelve pups. All experiments were conducted in accordance with NIH regulations and with approval of the University of Texas Medical Branch at Galveston Institutional Animal Care and Use Committee. Drugs. Phencyclidine was acquired from the National Institute on Drug Abuse (NIDA, Rockville, MD) and dissolved in 0.9% NaCl. Experimental design. Male and female Sprague-Dawley rat pups were treated on PN 7, 9, and 11 (sub-chronic) with 10 mg/kg PCP or saline vehicle (s.c). On PN22, littermates were weaned and housed 2 per cage according to treatment and sex. Animals were then tested for deficits in social interaction on PN28 (pre-pubescent) and PN54 (post-pubescent) or deficits in the social discrimination task on PN58-60 (adult). 116 Social Interaction Test. Social interaction is best defined as the time a pair of animals spends in an active social interaction (sniffing and grooming its partner, close following, mounting and crawling over or under its partner) with or without direct physical contact (Mouri et al. 2007). Testing was conducting during the dark cycle in order to decrease anxiogenic behavior and aggressive/territorial behavior as well as increase basal social behavior. The test was performed in open arena (40 x 40 x 40 cm) with bottom and sides made of clear Plexiglass placed in a sound attenuated chamber equipped with video recording capabilities. The light intensity was 30 lx and the bedding had been pre-exposed to other rats in order to maintain a constant odor level in the arena. On the day of testing, unfamiliar rat pairs that were matched for treatment, weight and sex were placed simultaneously in the arena 20 cm apart. Each testing session lasted for 10 minutes. Videos of the testing session were analyzed for % time of direct physical contact as well as types of social interacting behaviors. The types of social behavior measured were: investigative sniffing (anogenital, snout, other body parts), climbing over or under (climbing over the back or pushing head and forepart of body beneath), grooming the partner, following (rat moves after its partner without direct physical contact), avoiding (rat actively turns away or freezes when approached by its partner) (Sams-Dodd 1999, Sams-Dodd 1995). No aggressive or territorial behaviors were noted in any of the test groups. Social Discrimination Task. Social discrimination was measured as described previously with minor modifications (Harich et al. 2007a). All tests were performed during the light period of the night-day cycle under dimmed illumination (30 lx). Animals were treated as previously described with saline or PCP, allowed to age and on the day of testing (PN58-60), they were brought to a designated behavior room and allowed to acclimate for 30 min. They were then placed in an open field (40 x 117 40 x 40 cm) together with a same sex familiar juvenile (40-55 g) for 30 min. At the end of this period, a second unfamiliar juvenile, termed the novel juvenile, was placed in the chamber for an additional 5 min. The entire session was video-recorded and the time of investigative behavior of or by the adult (anogenital exploration, sniffing with direct contact, crawling over each other, grooming, play behaviors) towards each of the two juveniles was analyzed by a trained observer. The time spent investigating the familiar juvenile divided by the time spent investigating the novel juvenile is presented as the novelty discrimination index. Statistical Analysis. Group comparisons were specifically defined before the beginning of each experiment; therefore, planned comparisons were performed instead of an overall F test in a multifactorial ANOVA (Keppel 1982). All values are presented as mean ± SEM. The null hypothesis was rejected at p<0.05. Results The social interaction test we employed was based on previous studies with some modifications and has been shown repeatedly to model the negative symptoms of the disease with face and predictive validity (Snigdha & Neill 2008, Sams-Dodd 1996, Koros et al. 2007). Perinatal PCP treatment of young males (PN28) caused an overall significant 25 % decrease in total time spent in social interaction (from 6.7 min in saline treated pups to 5 min in PCP treated pups). Concomitant with this, we observed that PCP treated pups showed a significant 91% increase in total (central and peripheral) locomotor activity compared to the saline treated controls (Figure 6.1 left). Both the deficit in social interaction and increase in locomotor activity disappeared in mature males aged PN54 (Figure 6.1 right). No deficit in social interaction or alterations in locomotor activity was 118 measured in either pre-or post pubertal (aged PN28 and PN54, respectively) females (Figure 6.2). In order to extend previous work which suggested that PCP treatment can also model the selective attention and information processing deficits seen in schizophrenia (Goldberg & Gold 1995) Deficits in social novelty discrimination, i.e. the inability of an adult rat to discriminate between a familiar and a novel juvenile, is thought to serve as a suitable animal model of this symptom of schizophrenia (Engelmann et al. 1995). Deficits in novelty discrimination have been shown to occur after acute PCP (Terranova et al. 2005) and in adult rats that received PCP treatment during development (Depoortere et al. 2005, Terranova et al. 2005, Harich et al. 2007a). In this study, it was observed that both male and female rats treated on PN7, 9, & 11 with PCP have significant and long-lasting deficits in novelty discrimination as measured on PN58-60 (Figure 6.3). 119 Figure 6.1. Effects of neonatal PCP administration on social interaction and locomotor activity in pre-and post-pubescent male pups. Quantitative analysis of the % total time of social interaction (left) and the total locomotor activity (right) in pre- and post-pubescent saline and PCP-treated males. N=6/treatment group. *p<0.05 vs. saline PN28 male (Student’s t-test). 120 Figure 6.2. Effects of neonatal PCP administration on social interaction and locomotor activity in pre- and post-pubescent females. Neither the percent of total time spent in social interaction (left) nor the total locomotor activity (right) in either pre-pubescent (PN28) or post-pubescent (PN54) was different between saline and PCP-treated females. N=6/treatment group. 121 Figure 6.3. Effects of perinatal PCP treatment on PN7, 9, & 11 on social discrimination in adult (PN56-58) animals. The novelty discrimination index is defined by the time spent investigating the novel juvenile divided by time spent investigating the familiar juvenile) of both adult male and female Sprague-Dawley rats treated during development on PN7, 9 and 11. *p<0.05 vs. saline (Student’s t-test). 122 N=8/treatment group. Discussion It has been observed in the clinical setting that NMDAR antagonists, but not d-amphetamine, repeatedly and reliably induce several negative symptoms of schizophrenia, specifically social isolation and withdrawal (Sams-Dodd 1999). Further, stereotyped behaviors and locomotor hyperactivity, but not social interaction, relates to the positive symptoms of schizophrenia and may also serve as a marker of the psychotomimetic effects of a drug (Mouri et al. 2007). The present study shows that sub-chronic PCP administration to the perinatal rat results in long-lasting deficits in behavior which are thought to represent the negative symptoms of schizophrenia. Repeated PCP administration has been shown to induce deficits in social interaction, some of which have been shown to be persist for at least 28 days after withdrawal from treatment (10 mg/kg/day for 14 days) (Sams-Dodd 1999, Qiao et al. 2001, Sams-Dodd 1996). Here, we report that PCP treatment causes a deficit in the social interaction test in pre-pubertal, but not post-pubertal males. Further, stereotyped behavior, ataxia, and immobility were absent on the day of testing suggesting a specific effect on social behavior and not due to the intoxicating effects of PCP administration. The PCP pharmacokinetic differences between male and female rats are well known and are a significant parameter which must be acknowledged when interpreting PCP-induced behavioral differences between genders. Further, there are important sex differences in social interaction, such that social interaction may play a different role in females compared to males; hence, caution should be exercised when interpreting results from females (File & Seth 2003). The present study reports that PCP treatment to females on PN7, 9, & 11 has no effect on social interaction in either the prepubescent or post-pubescent female. An analogous study which tested social interaction 10 weeks after PCP treatment of females on PN7, 9, & 11 also saw no deficit (du Bois et al. 2008). Alternatively, a study by Snigdha and Neill (2008) treated adult female rats with PCP (2 mg/kg, 2x/day for seven days) reported 123 enduring deficits in social interaction which persisted for at least six weeks after treatment. The discrepancies are most likely due to differences in drug treatment schedules, ages and species of rats used, and/or the test parameters employed. In these experiments the observed hyperlocomotion in pre-pubertal males represents the total locomotor activity of both animals; therefore, it is not possible to draw unequivocal conclusions concerning the PCP treated rats. However, it is reasonable to postulate that the observed hyperactivity in response to the novel environment in the perinatal PCP-treated pre-pubertal males was due to perinatal PCP treatment of the subjects rather than to an unlikely difference in the untreated pups. PCP and MK-801 induce spontaneous hyperactivity in laboratory animals in a novel environment (Ford et al. 1989, Verebey et al. 1981). PCPinduced locomotor activity and the positive symptoms of the disease can be blocked by typical antipsychotics such as haloperidol, a potent and high affinity dopamine D2 antagonist (Moghaddam 1994, Verma & Moghaddam 1996). Synaptic interaction between dopaminergic and glutamatergic systems in the mesocorticolimbic system may underlie spontaneous exploration of a novel environment, a complex behavior which is affected by sensory processing, environmental cues, the animals’ state of arousal and interactions with other animals (Kelley et al. 1989, Clements & Greenshaw 2005). Thus, because of the ability of PCP to block the NMDA glutamate receptor subtype and increase activity in mesolimbic, mesocortical and nigrostriatal dopaminergic pathways (Jentsch et al. 1998, French & Ceci 1990), it is reasonable to expect that perinatal PCP treatment during development could alter exploratory behaviors mediated by these pathways later in life. An additional purpose of this study was to investigate whether sub-chronic PCP treatment of rat pups could model multiple aspects of the deficits in social function characteristic of schizophrenia, specifically by also measuring the effects of PCP on selective attention and information processing deficits. The social discrimination task used in the current study is an animal behavior model for 124 selective attention capacities (Harich et al. 2007a, Terranova et al. 2005). In this task, the adult animal must focus on the relevant juvenile, the novel juvenile, which requires a high level of selective attention since both juveniles move around rapidly playing with each other, i.e. the spatial position of the two stimuli changes constantly. Terranova et al. (2005) determined that this test is not likely to be a measure of impaired short term memory or social recognition abilities since the adult rat’s competence for social discrimination was maintained subsequent to each juvenile being placed into a small mesh cage thereby preventing it from freely moving around in the chamber. Previously it has been established that PCP administration on PN7, 9 and 11 to male rats results in a diminished novelty discrimination index, a deficit that was effectively treated with novel and potential antipsychotics, including a glycine transport inhibitor and mGluR2/3 agonists (Depoortere et al. 2005, Harich et al. 2007a). Further, others have extended our model by showing that a 5-HT1A agonist/D2 antagonist dulled the effects of perinatal PCP on novelty discrimination in a social context (Terranova et al. 2005). Here we demonstrate that sub-chronic PCP administration to both developing male and female rat pups results in long-lasting deficits in the novelty discrimination index, i.e. following treatment with PCP during development, the young adult animals that were treated with PCP appear to lack the ability to focus their attention on the novel juvenile. Similar to Harich et al (2007a), PCP treated animals spent more time investigating the familiar juvenile compared to the saline treated adults, suggesting an incomplete familiarization by the adult PCP treated animal within the first 30 minutes of the test, thereby increasing the exploratory time of the familiar juvenile during the last 5 min of the task. Taken in context with other reductions in information processing as evidenced by deficits in pre-pulse inhibition (Anastasio & Johnson 2008a, Wang et al. 2001) this study further supports the use of perinatal PCP treatment as a 125 useful tool in characterizing and designing pharmacotherapeutics approaches to the multiple symptoms of schizophrenia. 126 Chapter 7: Conclusions and Future Directions General Conclusions Clinical use of PCP, a potent dissociative anesthetic, was abandoned as a result of reports of post-operative hallucinations and disoriented behavior. Due to its hallucinogenic effects, PCP appeared on the drug of abuse scene in the mid-1960’s known as “angel dust”; nevertheless, illicit use of PCP has subsided because of its psychotomimetic properties. In addition to the psychotomimetic symptoms produced by PCP, several parallels exist between PCP administration and schizophrenia. PCP has been reported to increase cerebral metabolic activity in several limbic brain regions including the entorhinal cortex, retrosplenial and anterior cingulate cortex, the subiculum and the nucleus accumbens (Hargreaves et al. 1993, Weissman et al. 1989). Ketamine has also been shown to increase cerebral blood flow in the anterior cingulate cortex (Lahti et al. 1995). In addition, acute PCP administration was reported to cause neurotoxicity in the posterior cingulate/retrosplenial cortex (Olney et al. 1989b). Chronic administration of MK-801 or PCP caused neurodegeneration in additional brain regions including the anterior cingulate, parietal, temporal, piriform, and entorhinal cortices, hippocampus, and amygdala (Olney & Farber 1995b, Olney & Farber 1995a). These brain regions in which PCP and other noncompetitive NMDA antagonists alter cerebral blood flow and glucose utilization as well as produce neurotoxicity are some of the same brain regions that are thought to be affected in schizophrenia (Strous & Javitt 1996). It was postulated that since symptoms of schizophrenia do not appear until early adulthood that the etiology of the disease may be developmental in nature (Weinberger 1987), which led to the investigation of the neurotoxic effects of acute PCP or MK-801 during stages of rodent development (Ikonomidou et al. 1999, Wang et al. 2001, Wang & Johnson 2005). 127 As evidenced by several measures of neurotoxicity (TUNEL positive, cleaved caspase-3, and silver staining) PCP administration on postnatal day (PN)7 causes a robust loss of neurons in layers II-IV of the cingulate, parietal, and retrosplenial cortices, but also in the subiculum/CA1 region, anterior ventral nucleus of the thalamus and striatum (Wang & Johnson 2007, Wang & Johnson 2005). On the other hand, PCP administration on PN7, 9, & 11 shows a neurotoxic regional specificity for the frontal cortex only (Wang et al. 2001, Wang & Johnson 2005). Interestingly, PCP administration on PN7 results in a loss of parvalbumin (PV)-containing, but not calretinin or calbindin-containing neurons in the superficial layers (II–IV) of the primary somatosensory, motor, and retrosplenial cortices, but not in the striatum or hippocampus in PN56 rats (Wang et al. 2008). The effects of PCP on administration on PN7, 9, & 11 on PV expression in the adult animal have yet to be determined. The developmental dependence and neuronal specificity of this effect of PCP is remarkably similar to the damage observed in schizophrenic brains. These data strongly support the importance of determining the precise mechanisms of PCP-induced neurotoxicity and the functional consequences of this neurotoxicity in this model of schizophrenia. The overall purpose of this study is to address the hypotheses that neurotoxicity during a critical stage in brain development and subsequent alterations in cortical function may underlie the expression of aberrant schizophrenic-like behaviors in the developing rat. In summary, this work demonstrates that PCP induces neurotoxicity in developing pups in a manner that is highly regulated affecting the distribution, subunit composition, number, and function of NMDAR and that this loss of cortical neurons and altered cortical landscape is associated with behavioral deficits that are similar to those observed in schizophrenia. Specifically, PCP on PN7 causes cortical neurotoxicity by blocking NR1/NR2A receptors and induces a compensatory upregulation of NR1/NR2B in the synapse and the subsequent activation of calpain. Up-regulation of NR1/NR2B is most likely due to an increase in trafficking of 128 NR1/NR2B from ER to membrane. Further, the simultaneous increase in PSD- 95 most likely protects NR2B from calpain mediated cleavage; therefore, no internalization of the receptor occurs and membrane expression levels remain high. PCP on PN7, 9, & 11 also induces neurotoxicity in the frontal cortex by inhibiting NR1/NR2A-containing receptors resulting in a compensatory upregulation of NR1/NR2A receptors at the synaptic membrane, most likely through an increase in new NMDAR protein synthesis via NFκB nuclear translocation (Wang et al. 2001). We had hypothesized that an increase in NMDAR expression would result in intracellular Ca2+ overload and the activation of the apoptotic cell death cascade (McInnis et al. 2002, Wang et al. 2001, Wang et al. 2003). However, we no longer believe this to be true, since the NMDAR protein measured in these studies must come from live cells and the time course of upregulation of the receptor does not correspond to the time course of cell death. Caspase-3 is activated by 2 hrs in the frontal cortex; furthermore, TUNEL staining appears 6 hrs after treatment, peaks at 16 hrs and is completely cleared by 24 hrs (Wang & Johnson 2005, Wang & Johnson 2007). Therefore, we now propose that the compensatory mechanism of up-regulation occurs in surviving neurons in response to the death of neighboring cells and may serve to “protect” these neurons from PCP-induced neurotoxicity and re-establish NMDARmediated neurotransmission. Further, the newly inserted NMDARs are functionally active receptors and following agonist stimulation those from PCP treated animals (both acute and sub-chronic) function at a higher level compared to their saline counterparts. This change in function and loss of neurons may alter the architecture of the cortex as well as cortical glutamatergic and GABAergic neurotransmission (Olney & Farber 1995a, du Bois et al. 2009), which results in deficits in PPI of acoustic startle, social interaction, social discrimination as well as the development of locomotor sensitization. 129 Specific Aim 1 Specific Aim 1 was designed to determine the mechanism of PCP-induced regulation of the NMDAR in the frontal cortex. Acute PCP treatment (single injection on PN7) increased membrane levels of NR1 and NR2B protein in the frontal cortex, while no change in the expression of NR2A was detected. We next examined the effect of PCP on the expression of PSD-95, a member of the NMDAR post-synaptic density complex. Acute PCP administration produced an increase in membrane cortical protein levels of PSD-95, which paralleled the observed increase in membrane NR1 and NR2B expression in the frontal cortex. On the other hand, NR1 and NR2B protein levels in the ER fraction were decreased by acute PCP, suggesting an increased trafficking of NR1/NR2B from the ER to the membrane. Pretreatment with various antipsychotics and selective D1, D2 or 5-HT2A receptor antagonists had no effect on up-regulation of NMDAR protein expression induced by acute PCP. In distinction from the effects of acute PCP administration, sub-chronic (PN7, 9, & 11) PCP treatment caused an increase in NR1 and NR2A expression in both the ER and membrane fractions of the frontal cortex, while no effect on NR2B expression was evident in either fraction. We also determined that sub-chronic PCP administration did not alter levels of PSD-95 in the cortical membrane fraction. The increase in NR1/NR2A in the membrane fraction was blocked by pretreatment with antipsychotics and selective 5-HT2A, D1, or D2 receptor antagonists. The mechanism(s) of trafficking of NR1, NR2A, and NR2B subunits from intracellular compartments to the membrane and the role of calpain-mediated trafficking in the regulation of the NMDAR was also examined. We examined the role of calpain, a calcium-dependent neutral cysteine protease which is thought to regulate NMDAR trafficking, in both the acute and sub-chronic treatment paradigm. Calpain activation has been shown to play a role in excitotoxicity (Saido et al. 1994, Brorson et al. 1995, Araujo et al. 2004, Zhou & Baudry 2006) in several neurodegenerative disorders including Parkinson’s disease as well as 130 Alzheimer’s disease (Etienne & Baudry 1987, Vanderklish & Bahr 2000, Crocker et al. 2003). Calpain-mediated enzymatic cleavage of cytoskeletal proteins results in the loss of structural integrity and disturbances in axonal transport (Yamashima 2004). Additional substrates for calpain include αII-spectrin (cleavage position Tyr1176 & Gly1177), PSD-95, the NR2A subunit (cleavage position Phe1279; Ser1330), and the NR2B subunit (cleaved fragments of 140, 130, & 115/120 kDa) (Bi et al. 1998a, Bi et al. 1998b, Guttmann et al. 2001). To measure calpain activation, we performed Western blots on membrane cortical tissue from acute or sub-chronic PCP treated animals in order to examine the protein expression levels of αII-spectrin (a member of the post-synaptic density that is enzymatically cleaved directly by calpain) and its calpain specific breakdown products (SBP) which migrates at 145 and 150 kDa. Acute PCP treatment resulted in an increase in the αII-spectrin calpain SBP while subchronic PCP treatment had no effect on αII-spectrin calpain SBP expression levels. In order to add validity to the role of calpain in acute PCP-induced trafficking of the NR1/NR2B, we determined the effect of administering 10 mg/kg MDL28170 (a selective calpain inhibitor every 2 hrs for 8 hrs after PCP on PN7) on the membrane expression levels of NR1/NR2B in the frontal cortex. MDL28170 was able to prevent the up-regulation of NR1and NR2B protein levels and it also prevented cleavage of calpain itself. These data support our hypothesis that a treatment dependent mechanism of calpain-mediated trafficking may underlie the regulation of the NMDAR subunit composition following acute PCP administration to the perinatal rat. The NR1 subunit contains eight splice variants, one in the N terminus and two in the C terminus that possess distinguishing features. The splice variants differ in regard to their regional pattern of expression, their regulation by phosphorylation, polyamines and protons, their electrophysiological properties, and their affinity for cytoskeletal proteins (Cull-Candy et al. 2001). The C terminal splice variant composition affects trafficking of the NR1 subunit. It has been 131 suggested that the C2’ cassette present in four of the NR1 splice variants possesses a PDZ binding domain (STVV) (Wenthold et al. 2003). In addition, the NR1 subunit contains an ER retention signal (RXR) in the C1 cassette that must be masked for the polypeptide to be released from the ER (Wenthold et al. 2003). Thus, an alternative explanation underlying the mechanism of PCP- induced alterations in trafficking of the receptor may exist. It is reasonable to suggest that following acute PCP administration, binding of PSD-95 to the PDZ binding domain of the C2’ cassette of the NR1 subunit may mask the RXR motif in the C1 cassette, resulting in the exit of the NR1 subunit from the ER and insertion in the membrane (Standley et al. 2000); therefore, the robust increase in cortical membrane levels of PSD-95 caused by acute PCP treatment could be due to its persistent binding to the C2’ cassette of the NR1 subunit in conjunction with its presence in the post-synaptic density complex. This suggests that PSD95 interacts early in secretory pathways, perhaps functioning as an export protein that overrides the ER retention signal for the NR1 subunit in addition to serving to anchor the functional, assembled receptor complex in the synapse by binding to the C-terminus of the NR2 subunit (Wenthold et al. 2003). PCP blockade of the NMDA receptor results in the efflux of glutamate in the frontal cortex (Adams & Moghaddam 2001) leading to the subsequent activation of either AMPA/KA receptors or metabotropic glutamate receptors (mGluRs). Investigation of the interactions between mGluRs and NMDARs suggests that stimulation of mGluRs potentiates NMDAR function (Aniksztejn et al. 1991, Bleakman et al. 1992, Harvey & Collingridge 1993). Modulation of NMDAR function by mGluRs is thought to be limited to Group I; both mGluR1 (Lan et al. 2001) and mGluR5 (Pisani et al. 2001) have been implicated. Group I mGluRs are G-protein coupled receptors that are positively coupled to phospholipase C (PLC) resulting in the formation of diacylglycerol (DAG) and activation of protein kinase C (PKC), leading to the release of Ca 2+ from intracellular stores (Conn & Pin 1997). 132 Potentiation of NMDAR function by mGluR5 is dependent on G-protein second messenger signaling cascades, which includes PKC and Src kinase (Benquet et al. 2002). PKC phosphorylation of sites near the RXR motif of the NMDAR NR1 subunit masks the ER retention signal resulting in the trafficking of the subunit to the membrane (Scott et al. 2003). Thus, activation of mGluRs may be an additional compensatory mechanism in response to acute PCP blockade of the NMDAR. Next, we tested the role of protein synthesis in the regulation of the NMDAR. Cycloheximide (CHX) has been shown to cause transient (~12 hrs) suppression of brain protein synthesis in rats (Pavlik & Teisinger 1980). Since, protein synthesis would be intermittently released from inhibition in our subchronic paradigm we anticipated that the rats would tolerate the CHX posttreatment well (Liu et al. 1997). Although the chosen dose and dosing schedule of CHX had been reported to be well tolerated in adult animals (Liu et al. 1997), it was toxic in our experimental paradigm using perinatal rats. Animals treated with PCP (10 mg/kg) + CHX (0.25 mg/kg) on PN7, 9, & 11 died on PN12. Therefore, we administered CHX only on PN7 and PN9 three hours after PCP treatment. No animals in this paradigm died; however, a significant difference in their weight was observed. Since we were not comfortable with the level of toxicity, we decided to not pursue this project further. The ability of atypical antipsychotics as well as selective DA and 5-HT receptor antagonists to block sub-chronic induced alterations in the NMDAR subunits suggests that up-regulation of NR1 and NR2A in the frontal cortex following sub-chronic PCP administration may be due to increased synthesis of protein and mediated in part by D1, D2, and 5-HT2A receptors, which may have been activated by the effects of PCP on dopaminergic and serotonergic neuronal populations (Adams & Moghaddam 2001, Verma & Moghaddam 1996). PCPinduced release of DA in the prefrontal cortex (Verma & Moghaddam 1996) could lead to the activation of D1 receptors resulting in increased levels of cAMP and increased activation of PKA, which would be expected to increase the 133 phosphorylation of the transcription factor CREB (cAMP response element binding protein) (Lau et al. 2004). The NR1 gene contains a CRE (cAMP response element) binding site upstream of its transcription start site (Lau et al. 2004). PCP-induced phosphorylation of CREB by PKA or from activation of the MAP kinase pathway could then lead to increased binding of P-CREB to the NR1 CRE site, resulting in increased transcription of NR1 subunit protein in the frontal cortex. However, preliminary data indicates that the expected increase in cortical levels of P-CREB following both acute and sub-chronic PCP administration is not quite significant (Robeson and Johnson, unpublished observation). In addition, the NR1 gene contains a binding site for the transcription factor NF-κB (Liu et al. 2004a). Liu et al. (2004a) reported that binding to the NR1 NF-κB site up-regulates the NR1 promotor and subsequent transcription of the gene through interactions with Sp1/Sp3 factors. Wang et al. (2001) reported that sub-chronic PCP treatment increased nuclear translocation of NF-κB subunits p50 and p65 as evidenced by electrophoresis mobility shift assay (EMSA); this was prevented by olanzapine pretreatment. Therefore, PCP- induced activation of NF-κB transcription factors may be an alternative explanation for the observed increase in synthesis of NR1 protein. Specific Aim 2 Specific Aim 2 attempted to determine the function of the NMDAR in the frontal cortex using NMDA and glycine stimulated 3H-MK-801 binding. PCP blockade of the NMDAR results in a loss of cortical GABAergic PV-containing interneurons (Wang et al. 2008) and disruption in glutamatergic neurotransmission, resulting in the compensatory up-regulation of the NMDAR in surviving neurons. This aim was designed to test the hypothesis that up- regulation of the NMDAR in the frontal cortex by acute or sub-chronic PCP treatment of perinatal rats results in a hyper-functional receptor and is dependent on the relative NR1/NR2B versus NR1/NR2A composition of the receptor. We 134 determined that both acute and sub-chronic PCP administration causes the insertion of functionally active NMDARs in to the cortical synaptic space as evident by an increase in maximal NMDA and glycine stimulated 3H-MK-801 binding, which paralleled the increase in NMDAR receptor density (Anastasio & Johnson 2008b). However, we were not able to definitively determine the subunit composition responsible. A flaw in the experimental design may underlie the inability to draw conclusions from the ifenprodil and NR2A antagonist (both NVP-AAM007 and PEAQX) inhibition studies; i.e. the dose range tested for these compounds was too narrow and did not produce a full dose response inhibition curve. Experiments are currently ongoing which address this concern. Additionally, it would be useful to perform electrophysiological experiments to verify the binding results as well as to determine whether any changes in synaptic plasticity are evident, such as NMDA-dependent LTP which would underlie the proposed altered cortical function. It has been hypothesized that the NR2A subunit is the main mediator involved in delivering the AMPA GluR1 subunit to the synaptic membrane (via Ras-ERK activation), a critical step in NMDAR-dependent LTP (Kim et al. 2005); therefore, it would be instructional to measure the effect of acute and sub-chronic PCP treatment on synaptic GluR1 content as well as NMDAR-dependent LTP. Specific Aim 3 The subunit composition of the NMDAR that mediates PCP-induced neuronal neurotoxicity is currently unknown; therefore, we designed specific aim 3 to show that the synaptic or extrasynaptic localization of NR2A and 2B receptors may determine function. Over the last several years substantial evidence indicates that activation of synaptic NMDARs promotes neuronal survival, but activation of extrasynaptic receptors leads to cell death (Hardingham et al. 2002, Hardingham & Bading 2002). Thus, we proposed that PCP damages neurons by blocking synaptic NMDA receptors, most of which are thought to 135 contain NR1 and NR2A (Hardingham & Bading 2003, Hardingham et al. 2002). To investigate the role of synaptic and extrasynaptic NMDARs in PCP-induced neurotoxicity in vitro and in vivo we used antagonists at various doses for NR2A (NVP-AAM007 and PEAQX) and NR2B (ifenprodil). NVP-AAM007 and ifenprodil were administered to organotypic corticostriatal slice cultures as well as developing rat pups and apoptosis was estimated by measurement of caspase-3 enzymatic activity and histochemical assessment of TUNEL labeling of apoptotic neurons. In corticostriatal slices and in vivo, we found that both NVP-AAM007 and PEAQX are neurotoxic in the cortex, while ifenprodil is not. These data suggest that neurotoxicity in the frontal cortex of developing rat pups following acute or sub-chronic PCP administration is due to blockade of NR1/NR2A receptors, but not NR1/NR2B receptors. These results implicate synaptic NMDA receptors, rather than non-synaptic receptors as mediators of PCP-induced neuronal death. Although NVP-AAM007 and PEAQX may have a minor capacity for inhibition of NR2B-containing receptors (Frizelle et al. 2006, Neyton & Paoletti 2006), the lack of a neurotoxic effect by ifenprodil (selective NR2B antagonist) strongly argues against a role for the NR2B subunit at this stage of development in this PCP neurotoxicity model of schizophrenia. Cell death in the striatum following a single injection of PCP was induced by high doses of PEAQX, but not ifenprodil. These data suggest that acute PCPmediated neurotoxicity in the striatum is also mediated through blockade of NR1/NR2A receptors. Sub-chronic PCP does not induce noticeable neurotoxicity in the striatum after the last of three doses, but sub-chronic blockade of NR2A receptors in the striatum with PEAQX resulted in neurotoxicity at the highest dose of PEAQX administered. It has been postulated that at high doses this compound will block both NR2A and NR2C subunits (Feng et al. 2004). Therefore, it is reasonable to postulate that PCP selectively blocks NR2A subunits in the frontal cortex inducing neurotoxicity; however blockade of both 136 NR2A and NR2C receptors in the striatum may be necessary to result in neurotoxicity. The differential “synaptic” localization of NR2A and NR2B following either acute or sub-chronic PCP administration in vivo is uncertain, and was thus verified experimentally. All members of the MAGUK family (e.g. PSD-95, SAP102, SAP97) contain three PDZ domains, a Src homology domain 3 (SH3) and a C-terminal guanylate kinase-like (GK) domain. These post-synaptic proteins play key roles in NMDAR trafficking to the membrane, clustering at the membrane, and stabilization of the NMDAR complex organization in the postsynaptic architecture (Mauceri et al. 2007, Wu et al. 2007, Lu et al. 2000). PSD95 is thought to bind to the PDZ domain in the C-terminal region of synaptic NR2A or NR2B subunits (Lu et al. 2000, Wu et al. 2007). SAP102 is linked to extrasynaptic NR2B subunits (Wu et al. 2007, Sans et al. 2003) while SAP97 plays a role in the trafficking and insertion of NR2A subunits in the synaptic membrane (Mauceri et al. 2007). The expression level of NMDARs, their subunit composition as well as postsynaptic linkers can be altered following administration of NMDA antagonists including MK-801, ethanol and PCP (Dong et al. 2004, Anastasio & Johnson 2008b, Sircar et al. 1996, Suvarna et al. 2005) We performed co-immunoprecipitation studies to determine the localization of cortical NMDARs in a crude synaptoneurosomal preparation from postnatal cortex and demonstrated that following PCP treatment on PN7, 9, & 11, there is an apparent compensatory up-regulation in the surviving neurons of NR1/NR2A, but not NR1/NR2B in the synapse. This response to PCP-induced neurotoxicity by neighboring neurons may represent a protective mechanism to prevent further damage to the brain and/or restore cortical synaptic communication. An increase in the association of both NR2A and NR2B with SAP102 following PCP administration was also observed, suggesting a change in the expression levels of extrasynaptic NR2A and NR2B subunits as well as providing further evidence 137 that the localization of NR2A to the synaptic space is not necessarily true in all instances (Cull-Candy et al. 2001) . We have hypothesized that aberrant behaviors induced by PCP are due to its neurotoxic effects; therefore, an additional aspect of specific aim 3 was to show a relationship between NR2-blockade mediated neurotoxicity and the development of locomotor sensitization. As anticipated, PCP challenge to animals treated during development (PN7, 9, & 11) with PCP or PEAQX (an NR2A selective antagonist) resulted in locomotor sensitization associated with the neurotoxicity induced by these agents during a critical age of brain maturation. PEAQX or ifenprodil challenge did not result in locomotor sensitization, suggesting that the expression of this behavioral phenomenon following PCP challenge is not entirely due to blockade of the NMDAR, instead expression of this behavior may be in part due to PCP’s indirect effects on DA transmission (Verma & Moghaddam 1996, Johnson & Jones 1990, Lodge & Johnson 1990). Specific Aim 4 Finally, specific aim 4 was designed to test the validity of our treatment paradigm as a model of schizophrenia. Sub-chronic PCP administration to perinatal rats resulted in deficits of PPI of acoustic startle and the development of locomotor sensitization, which was prevented by olanzapine and risperidone pretreatment. To determine the pharmacological properties of the protective effects of olanzapine and risperidone, we tested the ability of selective receptor antagonists for D1 (SCH23390), D2 (sulpiride), and 5-HT2A (M100907) to prevent the behavioral effects of PCP. Interestingly, pre-treatment on PN7, 9, & 11 with SCH23390 and sulpiride prevented PCP-induced deficits in PPI, while M10907 was ineffective, suggesting that D1 and D2 receptors, but not 5-HT2A receptors may play a role in PCP-induced deficits in PPI. Further, we developed a methodology in our laboratory based on others (Snigdha & Neill 2008, Sams138 Dodd 1996, Koros et al. 2007, Harich et al. 2007a) with the purpose to identify PCP-induced deficits in social behavior, a key component of the negative symptoms of schizophrenia. Here we were able to effectively model the negative symptoms of schizophrenia with our treatment paradigm and report that subchronic PCP administration causes a deficit in social interaction and social discrimination, lending additional credibility to our treatment paradigm as a viable model of schizophrenia. In the future, we propose testing the effects of posttreatment with various antipsychotics in addition to DA and 5-HT receptor antagonists on the PCP-induced deficits in PPI, social behaviors, and development of locomotor sensitization so as to more closely mirror the clinical setting. Future Directions The dose and treatment paradigm employed in this study was designed to induce robust neurotoxicity, and while the this level of cortical neuropil loss does not occur in schizophrenia, the ability of perinatal PCP to kill PV-containing interneurons in cortical layers II-IV (Wang et al. 2008) as well as other neurons in regions similar to those affected in schizophrenia (Wang et al. 2001, Wang & Johnson 2005) is a significant finding. This is made even more important because of the concomitant deficits in social behavior, sensorimotor gating and working memory caused by postnatal PCP administration (Anastasio & Johnson 2008a, Wang et al. 2001, Harich et al. 2007b). However, the detailed molecular signaling mechanism(s) of neuronal death are still largely unknown as are the mechanisms responsible for the ability of antipsychotics and other compounds to provide protection against both the behavioral and neurotoxic effects of PCP (Anastasio & Johnson 2008a, Wang et al. 2001, Wang et al. 2003). The results from the abovementioned neurotoxicity studies are in general agreement with earlier studies which proposed that stimulation of synaptic NMDARs resulted in increased CREB activity, BDNF production and neuronal 139 survival, while stimulation of extrasynaptic receptors leads to a CREB shutoff pathway that prevents BDNF activation resulting in the subsequent neuronal death (Hardingham et al. 2002). It is important to note that some argue that the subunit composition not the localization of the NMDAR underlies the neurotoxicity (Liu et al. 2007). In contradiction, a recent publication by Martel et al. (2009) reports that NR2B subunits can mediate both neuronal survival and survival death. Hence, deciphering this debate between subunit composition versus localization and which determines how a neuron responds to toxic stimuli merits further investigation. To address this controversy, we will perform the following experiments in the organotypic slice culture system because it maintains the cortico-striatal inputs which are present in the whole animal and also allows us to perform many more experimental conditions (e.g. large drug concentration range), which would be difficult to do in whole animal experiments. In organotypic slice cultures synaptic transmission will be activated by blocking GABAA receptors and K+ channels with 50 µM bicuculline and 25 µM 4- aminopyridine, respectively (Lei et al. 2008, Hardingham et al. 2002, Ivanov et al. 2006). A low concentration of NMDA (10 µM) which is thought to be selective for synaptic versus extrasynaptic receptors (Soriano et al. 2006) in the presence of PCP will also be added and neurotoxicity measured with the caspase-3 activity assay. We have previously shown that this concentration of NMDA protects against PCP-induced neurotoxicity in a dissociated neuronal culture (Lei et al. 2008). The addition of a NR2A antagonist (NVP-AAM007 or PEAQX) or NR2B antagonist (ifenprodil) would then determine which subunit was responsible for the synaptic response to PCP-mediated neurotoxicity. Blockade of synaptic NMDARs with a low concentration of PCP and a moderate concentration of NMDA would stimulate extrasynaptic NMDARs and produce cell death. The post-treatment with NR2A antagonists or NR2B antagonists would allow one to distinguish the subunit composition responsible for the extrasynaptic response allowing us to clarify the controversy in our system. 140 PCP addition to organotypic slice cultures results in a long-lasting inhibition of ERK1/2 activity most likely through blockade of Ca 2+ influx and inactivation of ERK1/2 signaling (Xia et al. 2008). Therefore, the actions of PCP can be thought of as inhibiting synaptic activity and inducing cell death by uncoupling of the NMDAR and ERK1/2 signaling which, in turn, leads to a decrease in transcription and translation of the pro-survival proteins CREB and BDNF. As mentioned previously, NR2A-containing receptors are thought to primarily localize to the synaptic space, while NR2B-containing receptors have been found in both the synaptic (possibly in heterotrimeric form) and extrasynaptic milieu, most likely as a heterodimeric NR1/NR2B receptors (CullCandy et al. 2001). Ivanov et al. (2006) reported that extrasynaptic NMDARs inactivate the ERK1/2 pathway, while synaptic NMDARs favor activation of the ERK1/2 signaling cascade. Importantly, it is thought that NMDAR localization, rather than subunit composition alone determines the physiological and pharmacological properties of the receptors. That is, synaptic NR2B has been shown to be responsible for ERK1/2 phosphorylation and activation, while in contrast the extrasynaptic NR2B contributes to ERK1/2 dephosphorylation and inactivation (Ivanov et al. 2006). This laboratory has also demonstrated that activation of synaptic NMDARs prevents both PCP-induced neurotoxicity as well as inhibition of the PI3K/Akt/GSK-3β pathway in primary forebrain cell culture, corticostriatal slice cultures and in neonatal rats (Lei et al. 2008, Xia et al. 2008). This pathway is an additional and well established pro-survival pathway and promotes cell survival by phosphorylation and inhibition of pro-apoptotic proteins such as caspase-9 and GSK-3β (Cardone et al. 1998, Cross et al. 1995). Activating the PI-3K/Akt pathway by enhancing synaptic NMDAR strength prevented PCP-induced apoptosis (Lei et al. 2008). Further, PCP causes neuronal death in the layers IIIV of the cortex by dephosphorylation and activation of GSK-3β (Xia et al. 2008); unphosphorylated GSK-3β is known to activate the pro-death protein, caspase-3 141 (Rubinfeld et al. 1996). Therefore, the actions of PCP can be thought of as inhibiting the neuroprotective effects of Akt signaling as well as promoting the toxic effects of GSK-3β signaling. We propose that this bidirectional control of the ERK1/2 and the PI3K/Akt pathways by different synaptic or extrasynaptic pools of the NMDAR is an early signaling event responsible for neuronal survival or neuronal death following PCP administration and thus, is an important subject for future studies. To test this hypothesis we would first determine the time course of ERK1/2 activation following PCP administration in vivo. Next, we would administer NR2A or NR2B preferring antagonists to perinatal rat pups and measure the effects on ERK1/2 as well as the PI3K/Akt/GSK3-β pathways. We would also perform the reverse experiment in which we administer selective inhibitors for ERK1/2 or the PI3K/Akt/GSK3-β pathway and measure their effects on the expression of synaptic/extrasynaptic NR2A or NR2B subunits as well as neurotoxicity in the frontal cortex of developing rats. Recently, we have demonstrated that activation of D1 receptors in the frontal cortex protects against PCP-induced neurotoxicity by enhancing synaptic strength through synergistic activation of PI3K/Akt/GSK3-β pathways (Lei et al. 2009). PKA/Src kinase and the Interestingly, stimulation of D1 receptors diminishes PCP-induced deficits in PPI of acoustic startle (Lei et al. 2009). These studies demonstrate a novel mechanism for protection against PCP-induced neurotoxicity through enhancement of synaptic NMDAR strength by activation of D1 receptors as well as activation of the MEK/ERK and PI3K/Akt/GSK-3β pathways. Enhancing synaptic strength following PCP administration is thought to be the next step in treatment of schizophrenia. Co-administration of antipsychotics with compounds which enhance NMDAR function, such as glycine, d-cycloserine or glycine transporter 1 (GlyT1) inhibitors, have been somewhat successful in treating schizophrenics (Coyle & Tsai 2004, Lane et al. 2006). Thus, we believe 142 that answers to the aforementioned processes may lead to the discovery of new therapeutic targets for schizophrenia either through elucidating the molecular signaling cascades and the NMDAR subunit composition/localization involved in PCP-induced neurotoxicity or determination of the best mechanism to enhance synaptic NMDAR strength. 143 References Abdel-Hamid, K. M. and Tymianski, M. (1997) Mechanisms and effects of intracellular calcium buffering on neuronal survival in organotypic hippocampal cultures exposed to anoxia/aglycemia or to excitotoxins. J Neurosci, 17, 3538-3553. Adams, B. and Moghaddam, B. (1998) Corticolimbic dopamine neurotransmission is temporally dissociated from the cognitive and locomotor effects of phencyclidine. J Neurosci, 18, 5545-5554. Adams, B. W. and Moghaddam, B. (2001) Effect of clozapine, haloperidol, or M100907 on phencyclidine-activated glutamate efflux in the prefrontal cortex. Biol Psychiatry, 50, 750-757. Akazawa, C., Shigemoto, R., Bessho, Y., Nakanishi, S. and Mizuno, N. (1994) Differential expression of five N-methyl-D-aspartate receptor subunit mRNAs in the cerebellum of developing and adult rats. J Comp Neurol, 347, 150-160. Anastasio, N. C. and Johnson, K. M. (2008a) Atypical anti-schizophrenic drugs prevent changes in cortical N-methyl-D-aspartate receptors and behavior following sub-chronic phencyclidine administration in developing rat pups. Pharmacol Biochem Behav, 90, 569-577. Anastasio, N. C. and Johnson, K. M. (2008b) Differential regulation of the NMDA receptor by acute and sub-chronic phencyclidine administration in the developing rat. J Neurochem, 104, 1210-1218. Andine, P., Widermark, N., Axelsson, R., Nyberg, G., Olofsson, U., Martensson, E. and Sandberg, M. (1999) Characterization of MK-801-induced behavior as a putative rat model of psychosis. J Pharmacol Exp Ther, 290, 13931408. Aniksztejn, L., Bregestovski, P. and Ben-Ari, Y. (1991) Selective activation of quisqualate metabotropic receptor potentiates NMDA but not AMPA responses. Eur J Pharmacol, 205, 327-328. Anis, N. A., Berry, S. C., Burton, N. R. and Lodge, D. (1983) The dissociative anaesthetics, ketamine and phencyclidine, selectively reduce excitation of central mammalian neurones by N-methyl-aspartate. Br J Pharmacol, 79, 565-575. 144 Araki, T., Kato, H., Liu, X. H., Itoyama, Y., Kogure, K. and Kato, K. (1994) Delayed damage of striatal interneurons after cerebral ischemia in the gerbil. Neurosci Lett, 176, 17-20. Araujo, I. M., Verdasca, M. J., Leal, E. C., Bahr, B. A., Ambrosio, A. F., Carvalho, A. P. and Carvalho, C. M. (2004) Early calpain-mediated proteolysis following AMPA receptor activation compromises neuronal survival in cultured hippocampal neurons. J Neurochem, 91, 1322-1331. Arnt, J. and Skarsfeldt, T. (1998) Do novel antipsychotics have similar pharmacological characteristics? A review of the evidence. Neuropsychopharmacology, 18, 63-101. Arvanov, V. L. and Wang, R. Y. (1999) Clozapine, but not haloperidol, prevents the functional hyperactivity of N-methyl-D-aspartate receptors in rat cortical neurons induced by subchronic administration of phencyclidine. J Pharmacol Exp Ther, 289, 1000-1006. Auberson, Y. P., Allgeier, H., Bischoff, S., Lingenhoehl, K., Moretti, R. and Schmutz, M. (2002) 5-Phosphonomethylquinoxalinediones as competitive NMDA receptor antagonists with a preference for the human 1A/2A, rather than 1A/2B receptor composition. Bioorg Med Chem Lett, 12, 1099-1102. Ballmaier, M., Zoli, M., Mazzoncini, R., Gennarelli, M. and Spano, F. (2001) Combined alpha 2-adrenergic/D2 dopamine receptor blockade fails to reproduce the ability of clozapine to reverse phencyclidine-induced deficits in prepulse inhibition of startle. Psychopharmacology (Berl), 159, 105-110. Balster, R. L. (1986) Clinical implications of behavioral pharmacology research on phencyclidine. NIDA Res Monogr, 64, 148-162. Balster, R. L. (1989) Behavioral pharmacology of PCP, NMDA and sigma receptors. NIDA Res Monogr, 95, 270-274. Beardsley, P. M., Hayes, B. A. and Balster, R. L. (1990) The self-administration of MK-801 can depend upon drug-reinforcement history, and its discriminative stimulus properties are phencyclidine-like in rhesus monkeys. J Pharmacol Exp Ther, 252, 953-959. Beasley, C. L. and Reynolds, G. P. (1997) Parvalbumin-immunoreactive neurons are reduced in the prefrontal cortex of schizophrenics. Schizophr Res, 24, 349-355. 145 Beasley, C. L., Zhang, Z. J., Patten, I. and Reynolds, G. P. (2002) Selective deficits in prefrontal cortical GABAergic neurons in schizophrenia defined by the presence of calcium-binding proteins. Biol Psychiatry, 52, 708-715. Ben-Ari, Y., Khazipov, R., Leinekugel, X., Caillard, O. and Gaiarsa, J. L. (1997) GABAA, NMDA and AMPA receptors: a developmentally regulated 'menage a trois'. Trends Neurosci, 20, 523-529. Benes, F. M. (1991) Evidence for neurodevelopment disturbances in anterior cingulate cortex of post-mortem schizophrenic brain. Schizophr Res, 5, 187-188. Benes, F. M. (1995) Altered glutamatergic and GABAergic mechanisms in the cingulate cortex of the schizophrenic brain. Arch Gen Psychiatry, 52, 1015-1018; discussion 1019-1024. Beninger, R. J., Jhamandas, A., Aujla, H., Xue, L., Dagnone, R. V., Boegman, R. J. and Jhamandas, K. (2002) Neonatal exposure to the glutamate receptor antagonist MK-801: effects on locomotor activity and pre-pulse inhibition before and after sexual maturity in rats. Neurotox Res, 4, 477-488. Benquet, P., Gee, C. E. and Gerber, U. (2002) Two distinct signaling pathways upregulate NMDA receptor responses via two distinct metabotropic glutamate receptor subtypes. J Neurosci, 22, 9679-9686. Bi, R., Bi, X. and Baudry, M. (1998a) Phosphorylation regulates calpain-mediated truncation of glutamate ionotropic receptors. Brain Res, 797, 154-158. Bi, X., Chen, J., Dang, S., Wenthold, R. J., Tocco, G. and Baudry, M. (1997) Characterization of calpain-mediated proteolysis of GluR1 subunits of alpha-amino-3-hydroxy-5-methylisoxazole-4-propionate receptors in rat brain. J Neurochem, 68, 1484-1494. Bi, X., Rong, Y., Chen, J., Dang, S., Wang, Z. and Baudry, M. (1998b) Calpainmediated regulation of NMDA receptor structure and function. Brain Res, 790, 245-253. Bleakman, D., Rusin, K. I., Chard, P. S., Glaum, S. R. and Miller, R. J. (1992) Metabotropic glutamate receptors potentiate ionotropic glutamate responses in the rat dorsal horn. Mol Pharmacol, 42, 192-196. Bogerts, B. (1993) Recent advances in the neuropathology of schizophrenia. Schizophr Bull, 19, 431-445. 146 Bondolfi, G., Dufour, H., Patris, M., May, J. P., Billeter, U., Eap, C. B. and Baumann, P. (1998) Risperidone versus clozapine in treatment-resistant chronic schizophrenia: a randomized double-blind study. The Risperidone Study Group. Am J Psychiatry, 155, 499-504. Braff, D. L. and Geyer, M. A. (1990) Sensorimotor gating and schizophrenia. Human and animal model studies. Arch Gen Psychiatry, 47, 181-188. Bromet, E. J. and Fennig, S. (1999) Epidemiology and natural history of schizophrenia. Biol Psychiatry, 46, 871-881. Brorson, J. R., Marcuccilli, C. J. and Miller, R. J. (1995) Delayed antagonism of calpain reduces excitotoxicity in cultured neurons. Stroke, 26, 1259-1266; discussion 1267. Brown, A. S. (2006) Prenatal infection as a risk factor for schizophrenia. Schizophr Bull, 32, 200-202. Bunney, B. G., Bunney Jr, W. E. and A, C. (2000) Schizophrenia and glutamate: an update. In: American College of Neuropsychopharmacology Annual Meeting report. Cardone, M. H., Roy, N., Stennicke, H. R., Salvesen, G. S., Franke, T. F., Stanbridge, E., Frisch, S. and Reed, J. C. (1998) Regulation of cell death protease caspase-9 by phosphorylation. Science, 282, 1318-1321. Carlsson, A. (1988) The current status of the dopamine hypothesis of schizophrenia. Neuropsychopharmacology, 1, 179-186. Carlsson, M. and Carlsson, A. (1990) Interactions between glutamatergic and monoaminergic systems within the basal ganglia--implications for schizophrenia and Parkinson's disease. Trends Neurosci, 13, 272-276. Castellani, S. and Adams, P. M. (1981) Acute and chronic phencyclidine effects on locomotor activity, stereotypy and ataxia in rats. Eur J Pharmacol, 73, 143-154. Castle, D., Wessely, S., Der, G. and Murray, R. M. (1991) The incidence of operationally defined schizophrenia in Camberwell, 1965-84. Br J Psychiatry, 159, 790-794. Chaperon, F., Muller, W., Auberson, Y. P., Tricklebank, M. D. and Neijt, H. C. (2003) Substitution for PCP, disruption of prepulse inhibition and hyperactivity induced by N-methyl-D-aspartate receptor antagonists: 147 preferential involvement of the NR2B rather than NR2A subunit. Behav Pharmacol, 14, 477-487. Chen, Q. and Reiner, A. (1996) Cellular distribution of the NMDA receptor NR2A/2B subunits in the rat striatum. Brain Res, 743, 346-352. Cheng, N., Maeda, T., Kume, T., Kaneko, S., Kochiyama, H., Akaike, A., Goshima, Y. and Misu, Y. (1996) Differential neurotoxicity induced by LDOPA and dopamine in cultured striatal neurons. Brain Res, 743, 278283. Chong, V. Z., Thompson, M., Beltaifa, S., Webster, M. J., Law, A. J. and Weickert, C. S. (2008) Elevated neuregulin-1 and ErbB4 protein in the prefrontal cortex of schizophrenic patients. Schizophr Res, 100, 270-280. Choquet, D. and Triller, A. (2003) The role of receptor diffusion in the organization of the postsynaptic membrane. Nat Rev Neurosci, 4, 251265. Chowdari, K. V., Bamne, M., Wood, J., Talkowski, M. E., Mirnics, K., Levitt, P., Lewis, D. A. and Nimgaonkar, V. L. (2008) Linkage disequilibrium patterns and functional analysis of RGS4 polymorphisms in relation to schizophrenia. Schizophr Bull, 34, 118-126. Chowdari, K. V., Mirnics, K., Semwal, P. et al. (2002) Association and linkage analyses of RGS4 polymorphisms in schizophrenia. Hum Mol Genet, 11, 1373-1380. Clements, R. L. and Greenshaw, A. J. (2005) Differential effects of 7-OH-DPAT and apomorphine on hyperactivity induced by MK-801 (dizocilpine) in rats. Neuropharmacology, 49, 1007-1016. Conn, P. J. and Pin, J. P. (1997) Pharmacology and functions of metabotropic glutamate receptors. Annu Rev Pharmacol Toxicol, 37, 205-237. Cousins, S. L., Papadakis, M., Rutter, A. R. and Stephenson, F. A. (2008) Differential interaction of NMDA receptor subtypes with the post-synaptic density-95 family of membrane associated guanylate kinase proteins. Journal of Neurochemistry, 104, 903-913. Coyle, J. T. and Tsai, G. (2004) The NMDA receptor glycine modulatory site: a therapeutic target for improving cognition and reducing negative symptoms in schizophrenia. Psychopharmacology (Berl), 174, 32-38. 148 Craddock, N., O'Donovan, M. C. and Owen, M. J. (2005) The genetics of schizophrenia and bipolar disorder: dissecting psychosis. J Med Genet, 42, 193-204. Crocker, S. J., Smith, P. D., Jackson-Lewis, V. et al. (2003) Inhibition of calpains prevents neuronal and behavioral deficits in an MPTP mouse model of Parkinson's disease. J Neurosci, 23, 4081-4091. Cross, D. A., Alessi, D. R., Cohen, P., Andjelkovich, M. and Hemmings, B. A. (1995) Inhibition of glycogen synthase kinase-3 by insulin mediated by protein kinase B. Nature, 378, 785-789. Cull-Candy, S., Brickley, S. and Farrant, M. (2001) NMDA receptor subunits: diversity, development and disease. Curr Opin Neurobiol, 11, 327-335. Danos, P., Baumann, B., Bernstein, H. G., Franz, M., Stauch, R., Northoff, G., Krell, D., Falkai, P. and Bogerts, B. (1998) Schizophrenia and anteroventral thalamic nucleus: selective decrease of parvalbuminimmunoreactive thalamocortical projection neurons. Psychiatry Res, 82, 110. Davies, G., Welham, J., Chant, D., Torrey, E. F. and McGrath, J. (2003) A systematic review and meta-analysis of Northern Hemisphere season of birth studies in schizophrenia. Schizophr Bull, 29, 587-593. Depoortere, R., Dargazanli, G., Estenne-Bouhtou, G. et al. (2005) Neurochemical, electrophysiological and pharmacological profiles of the selective inhibitor of the glycine transporter-1 SSR504734, a potential new type of antipsychotic. Neuropsychopharmacology, 30, 1963-1985. Depoortere, R., Perrault, G. and Sanger, D. J. (1999) Prepulse inhibition of the startle reflex in rats: effects of compounds acting at various sites on the NMDA receptor complex. Behav Pharmacol, 10, 51-62. Dong, Y. N., Waxman, E. A. and Lynch, D. R. (2004) Interactions of postsynaptic density-95 and the NMDA receptor 2 subunit control calpain-mediated cleavage of the NMDA receptor. J Neurosci, 24, 11035-11045. Dong, Y. N., Wu, H. Y., Hsu, F. C., Coulter, D. A. and Lynch, D. R. (2006) Developmental and cell-selective variations in N-methyl-D-aspartate receptor degradation by calpain. J Neurochem, 99, 206-217. du Bois, T. M., Deng, C., Han, M., Newell, K. A. and Huang, X. F. (2009) Excitatory and inhibitory neurotransmission is chronically altered following 149 perinatal NMDA receptor blockade. Eur Neuropsychopharmacol, epub ahead of print. du Bois, T. M. and Huang, X. F. (2007) Early brain development disruption from NMDA receptor hypofunction: relevance to schizophrenia. Brain Res Rev, 53, 260-270. du Bois, T. M., Huang, X. F. and Deng, C. (2008) Perinatal administration of PCP alters adult behaviour in female Sprague-Dawley rats. Behav Brain Res, 188, 416-419. Duan, J., Martinez, M., Sanders, A. R., Hou, C., Burrell, G. J., Krasner, A. J., Schwartz, D. B. and Gejman, P. V. (2007) DTNBP1 (Dystrobrevin binding protein 1) and schizophrenia: association evidence in the 3' end of the gene. Hum Hered, 64, 97-106. Duncan, G. E., Moy, S. S., Lieberman, J. A. and Koller, B. H. (2006) Typical and atypical antipsychotic drug effects on locomotor hyperactivity and deficits in sensorimotor gating in a genetic model of NMDA receptor hypofunction. Pharmacol Biochem Behav, 85, 481-491. Egan, M. F., Straub, R. E., Goldberg, T. E. et al. (2004) Variation in GRM3 affects cognition, prefrontal glutamate, and risk for schizophrenia. Proc Natl Acad Sci U S A, 101, 12604-12609. Ellenbroek, B. A., Budde, S. and Cools, A. R. (1996) Prepulse inhibition and latent inhibition: the role of dopamine in the medial prefrontal cortex. Neuroscience, 75, 535-542. Ellenbroek, B. A. and Cools, A. R. (2000) Animal models for the negative symptoms of schizophrenia. Behav Pharmacol, 11, 223-233. Engelmann, M., Wotjak, C. T. and Landgraf, R. (1995) Social discrimination procedure: an alternative method to investigate juvenile recognition abilities in rats. Physiol Behav, 58, 315-321. Etienne, P. and Baudry, M. (1987) Calcium dependent aspects of synaptic plasticity, excitatory amino acid neurotransmission, brain aging and schizophrenia: a unifying hypothesis. Neurobiol Aging, 8, 362-366. Feng, B., Tse, H. W., Skifter, D. A., Morley, R., Jane, D. E. and Monaghan, D. T. (2004) Structure-activity analysis of a novel NR2C/NR2D-preferring NMDA receptor antagonist: 1-(phenanthrene-2-carbonyl) piperazine-2,3dicarboxylic acid. Br J Pharmacol, 141, 508-516. 150 Fenton, W. S. and McGlashan, T. H. (1991) Natural history of schizophrenia subtypes. II. Positive and negative symptoms and long-term course. Arch Gen Psychiatry, 48, 978-986. Figueredo-Cardenas, G., Anderson, K. D., Chen, Q., Veenman, C. L. and Reiner, A. (1994) Relative survival of striatal projection neurons and interneurons after intrastriatal injection of quinolinic acid in rats. Exp Neurol, 129, 37-56. File, S. E. and Seth, P. (2003) A review of 25 years of the social interaction test. Eur J Pharmacol, 463, 35-53. Finnegan, K. T., Kanner, M. I. and Meltzer, H. Y. (1976) Phencyclidine-induced rotational behavior in rats with nigrostriatal lesions and its modulation by dopaminergic and cholinergic agents. Pharmacol Biochem Behav, 5, 651660. Floresco, S. B., Todd, C. L. and Grace, A. A. (2001) Glutamatergic afferents from the hippocampus to the nucleus accumbens regulate activity of ventral tegmental area dopamine neurons. J Neurosci, 21, 4915-4922. Ford, L. M., Norman, A. B. and Sanberg, P. R. (1989) The topography of MK801-induced locomotor patterns in rats. Physiol Behav, 46, 755-758. Fredriksson, A. and Archer, T. (2003) Hyperactivity following postnatal NMDA antagonist treatment: reversal by D-amphetamine. Neurotox Res, 5, 549564. Fredriksson, A. and Archer, T. (2004) Neurobehavioural deficits associated with apoptotic neurodegeneration and vulnerability for ADHD. Neurotox Res, 6, 435-456. Fredriksson, A., Archer, T., Alm, H., Gordh, T. and Eriksson, P. (2004) Neurofunctional deficits and potentiated apoptosis by neonatal NMDA antagonist administration. Behav Brain Res, 153, 367-376. French-Mullen, J. M. and Rogawski, M. A. (1992) Phencyclidine block of calcium current in isolated guinea-pig hippocampal neurones. J Physiol, 456, 85105. French, E. D. and Ceci, A. (1990) Non-competitive N-methyl-D-aspartate antagonists are potent activators of ventral tegmental A10 dopamine neurons. Neurosci Lett, 119, 159-162. Friston, K. J. (1992) The dorsolateral prefrontal cortex, schizophrenia and PET. J Neural Transm Suppl, 37, 79-93. 151 Friston, K. J., Liddle, P. F., Frith, C. D., Hirsch, S. R. and Frackowiak, R. S. (1992) The left medial temporal region and schizophrenia. A PET study. Brain, 115 ( Pt 2), 367-382. Frizelle, P. A., Chen, P. E. and Wyllie, D. J. (2006) Equilibrium constants for (R)[(S)-1-(4-bromo-phenyl)-ethylamino]-(2,3-dioxo-1,2,3,4-tetrahydroquino xalin-5-yl)-methyl]-phosphonic acid (NVP-AAM077) acting at recombinant NR1/NR2A and NR1/NR2B N-methyl-D-aspartate receptors: Implications for studies of synaptic transmission. Mol Pharmacol, 70, 1022-1032. Gao, X. M. and Tamminga, C. A. (1994) An increase in NMDA-sensitive [3H]glutamate and [3H]kainate binding in hippocampus 24 hours after PCP. Neurosci Lett, 174, 149-153. Garey, R. E. and Heath, R. G. (1976) The effects of phencyclidine on the uptake of 3H-catecholamines by rat striatal and hypothalamic synaptosomes. Life Sci, 18, 1105-1110. Garthwaite, G. and Garthwaite, J. (1986) Neurotoxicity of excitatory amino acid receptor agonists in rat cerebellar slices: dependence on calcium concentration. Neurosci Lett, 66, 193-198. Geddes, J. R. and Lawrie, S. M. (1995) Obstetric complications and schizophrenia: a meta-analysis. Br J Psychiatry, 167, 786-793. Geyer, M. A. and Ellenbroek, B. (2003) Animal behavior models of the mechanisms underlying antipsychotic atypicality. Prog Neuropsychopharmacol Biol Psychiatry, 27, 1071-1079. Geyer, M. A., Krebs-Thomson, K., Braff, D. L. and Swerdlow, N. R. (2001) Pharmacological studies of prepulse inhibition models of sensorimotor gating deficits in schizophrenia: a decade in review. Psychopharmacology (Berl), 156, 117-154. Goff, D. C. and Evins, A. E. (1998) Negative symptoms in schizophrenia: neurobiological models and treatment response. Harv Rev Psychiatry, 6, 59-77. Goldberg, T. and Gold, J. (1995) Neurocognitive deficits in schizophrenia. In: Schizophrenia, (W. D. Hirsch SR ed.), pp. 146–162. Blackwell Science. Grace, A. A. (1991) Phasic versus tonic dopamine release and the modulation of dopamine system responsivity: a hypothesis for the etiology of schizophrenia. Neuroscience, 41, 1-24. 152 Guttmann, R. P., Baker, D. L., Seifert, K. M., Cohen, A. S., Coulter, D. A. and Lynch, D. R. (2001) Specific proteolysis of the NR2 subunit at multiple sites by calpain. J Neurochem, 78, 1083-1093. Guttmann, R. P., Sokol, S., Baker, D. L., Simpkins, K. L., Dong, Y. and Lynch, D. R. (2002) Proteolysis of the N-methyl-d-aspartate receptor by calpain in situ. J Pharmacol Exp Ther, 302, 1023-1030. Hanania, T., Hillman, G. R. and Johnson, K. M. (1999) Augmentation of locomotor activity by chronic phencyclidine is associated with an increase in striatal NMDA receptor function and an upregulation of the NR1 receptor subunit. Synapse, 31, 229-239. Hanania, T. and Johnson, K. M. (1999) Regulation of NMDA-stimulated [14C]GABA and [3H]acetylcholine release by striatal glutamate and dopamine receptors. Brain Res, 844, 106-117. Hardingham, G. E. and Bading, H. (2002) Coupling of extrasynaptic NMDA receptors to a CREB shut-off pathway is developmentally regulated. Biochem Biophys Acta, 1600, 148-153. Hardingham, G. E. and Bading, H. (2003) The Yin and Yang of NMDA receptor signalling. Trends Neurosci, 26, 81-89. Hardingham, G. E., Fukunaga, Y. and Bading, H. (2002) Extrasynaptic NMDARs oppose synaptic NMDARs by triggering CREB shut-off and cell death pathways. Nat Neurosci, 5, 405-414. Hargreaves, E. L. and Cain, D. P. (1995) MK801-induced hyperactivity: duration of effects in rats. Pharmacol Biochem Behav, 51, 13-19. Hargreaves, R. J., Rigby, M., Smith, D., Hill, R. G. and Iversen, L. L. (1993) Competitive as well as uncompetitive N-methyl-D-aspartate receptor antagonists affect cortical neuronal morphology and cerebral glucose metabolism. Neurochem Res, 18, 1263-1269. Harich, S., Gross, G. and Bespalov, A. (2007a) Stimulation of the metabotropic glutamate 2/3 receptor attenuates social novelty discrimination deficits induced by neonatal phencyclidine treatment. Psychopharmacology (Berl), 192, 511-519. Harich, S., Koch, M. and Schwabe, K. (2007b) Effects of repeated dizocilpine treatment on adult rat behavior after neonatal lesions of the entorhinal cortex. Prog Neuropsychopharmacol Biol Psychiatry. 153 Harris, L. W., Sharp, T., Gartlon, J., Jones, D. N. and Harrison, P. J. (2003) Long-term behavioural, molecular and morphological effects of neonatal NMDA receptor antagonism. Eur J Neurosci, 18, 1706-1710. Harrison, P. J. and Owen, M. J. (2003) Genes for schizophrenia? Recent findings and their pathophysiological implications. Lancet, 361, 417-419. Harrison, P. J. and Weinberger, D. R. (2005) Schizophrenia genes, gene expression, and neuropathology: on the matter of their convergence. Mol Psychiatry, 10, 40-68; image 45. Harvey, J. and Collingridge, G. L. (1993) Signal transduction pathways involved in the acute potentiation of NMDA responses by 1S,3R-ACPD in rat hippocampal slices. Br J Pharmacol, 109, 1085-1090. Hatton, C. J. and Paoletti, P. (2005) Modulation of triheteromeric NMDA receptors by N-terminal domain ligands. Neuron, 46, 261-274. Higgins, G. A., Ballard, T. M., Huwyler, J., Kemp, J. A. and Gill, R. (2003) Evaluation of the NR2B-selective NMDA receptor antagonist Ro 63-1908 on rodent behaviour: evidence for an involvement of NR2B NMDA receptors in response inhibition. Neuropharmacology, 44, 324-341. Hirsch, S. R., Das, I., Garey, L. J. and de Belleroche, J. (1997) A pivotal role for glutamate in the pathogenesis of schizophrenia, and its cognitive dysfunction. Pharmacol Biochem Behav, 56, 797-802. Honey, C. R., Miljkovic, Z. and MacDonald, J. F. (1985) Ketamine and phencyclidine cause a voltage-dependent block of responses to L-aspartic acid. Neurosci Lett, 61, 135-139. Ikonomidou, C., Bosch, F., Miksa, M. et al. (1999) Blockade of NMDA receptors and apoptotic neurodegeneration in the developing brain. Science, 283, 70-74. Ivanov, A., Pellegrino, C., Rama, S., Dumalska, I., Salyha, Y., Ben-Ari, Y. and Medina, I. (2006) Opposing role of synaptic and extrasynaptic NMDA receptors in regulation of the extracellular signal-regulated kinases (ERK) activity in cultured rat hippocampal neurons. J Physiol, 572, 789-798. Jackson, M. E., Homayoun, H. and Moghaddam, B. (2004) NMDA receptor hypofunction produces concomitant firing rate potentiation and burst activity reduction in the prefrontal cortex. Proc Natl Acad Sci U S A, 101, 8467-8472. 154 Jardemark, K. E., Liang, X., Arvanov, V. and Wang, R. Y. (2000) Subchronic treatment with either clozapine, olanzapine or haloperidol produces a hyposensitive response of the rat cortical cells to N-methyl-D-aspartate. Neuroscience, 100, 1-9. Javitt, D. C., Steinschneider, M., Schroeder, C. E. and Arezzo, J. C. (1996) Role of cortical N-methyl-D-aspartate receptors in auditory sensory memory and mismatch negativity generation: implications for schizophrenia. Proc Natl Acad Sci U S A, 93, 11962-11967. Javitt, D. C. and Zukin, S. R. (1991) Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry, 148, 1301-1308. Jentsch, J. D., Redmond, D. E., Jr., Elsworth, J. D., Taylor, J. R., Youngren, K. D. and Roth, R. H. (1997) Enduring cognitive deficits and cortical dopamine dysfunction in monkeys after long-term administration of phencyclidine. Science, 277, 953-955. Jentsch, J. D., Tran, A., Taylor, J. R. and Roth, R. H. (1998) Prefrontal cortical involvement in phencyclidine-induced activation of the mesolimbic dopamine system: behavioral and neurochemical evidence. Psychopharmacology (Berl), 138, 89-95. Johansson, C., Jackson, D. M. and Svensson, L. (1994) The atypical antipsychotic, remoxipride, blocks phencyclidine-induced disruption of prepulse inhibition in the rat. Psychopharmacology (Berl), 116, 437-442. Johansson, C., Jackson, D. M., Zhang, J. and Svensson, L. (1995) Prepulse inhibition of acoustic startle, a measure of sensorimotor gating: effects of antipsychotics and other agents in rats. Pharmacol Biochem Behav, 52, 649-654. Johnson, K. M. (1982) Phencyclidine: behavioral and biochemical evidence against the anticholinergic hypothesis. Pharmacol Biochem Behav, 17, 5357. Johnson, K. M. and Jones, S. M. (1990) Neuropharmacology of phencyclidine: basic mechanisms and therapeutic potential. Annu Rev Pharmacol Toxicol, 30, 707-750. Johnson, K. M., Phillips, M., Wang, C. and Kevetter, G. A. (1998) Chronic phencyclidine induces behavioral sensitization and apoptotic cell death in the olfactory and piriform cortex. J Neurosci Res, 52, 709-722. 155 Johnson, K. M., Snell, L. D., Sacaan, A. I. and Jones, S. M. (1989) Pharmacological Regulation of the Phencyclidine-Binding Site Associated with the N-Methyl-D-Aspartate Receptor-Operated Ion Channel. Drug Development Research, 17, 281-297. Johnson, K. M., Snell, L. D., Sacaan, A. I. and Jones, S. M. (1993) Pharmacologic regulation of the NMDA receptor-ionophore complex. NIDA Res Monogr, 133, 13-39. Jones, S. M., Snell, L. D. and Johnson, K. M. (1989) Characterization of the binding of radioligands to the N-methyl-D-aspartate, phencyclidine, and glycine receptors in buffy coat membranes. J Pharmacol Methods, 21, 161-168. Kelley, A. E., Cador, M. and Stinus, L. (1989) Exploration and its measurement: a psychopharmacological perspective: Neuromethods (13) Psychopharmacology. Humana Press, Totowa, NJ. Keppel, G. (1982) Design and analysis : a researcher's handbook. Prentice-Hall, Englewood Cliffs, NJ. Kim, E. and Sheng, M. (2004) PDZ domain proteins of synapses. Nat Rev Neurosci, 5, 771-781. Kim, M. J., Dunah, A. W., Wang, Y. T. and Sheng, M. (2005) Differential roles of NR2A- and NR2B-containing NMDA receptors in Ras-ERK signaling and AMPA receptor trafficking. Neuron, 46, 745-760. Kitaichi, K., Yamada, K., Yoneda, Y., Ogita, K., Hasegawa, T., Furukawa, H. and Nabeshima, T. (1995) Risperidone prevents the development of supersensitivity, but not tolerance, to phencyclidine in rats treated with subacute phencyclidine. Life Sci, 56, 531-543. Koch, M. and Bubser, M. (1994) Deficient sensorimotor gating after 6hydroxydopamine lesion of the rat medial prefrontal cortex is reversed by haloperidol. Eur J Neurosci, 6, 1837-1845. Kochhar, A., Zivin, J. A. and Mazzarella, V. (1991) Pharmacologic studies of the neuroprotective actions of a glutamate antagonist in ischemia. J Neurotrauma, 8, 175-186. Kohr, G. (2006) NMDA receptor function: subunit composition versus spatial distribution. Cell Tissue Res, 326, 439-446. 156 Komuro, H. and Rakic, P. (1993) Modulation of neuronal migration by NMDA receptors. Science, 260, 95-97. Koros, E., Rosenbrock, H., Birk, G., Weiss, C. and Sams-Dodd, F. (2007) The selective mGlu5 receptor antagonist MTEP, similar to NMDA receptor antagonists, induces social isolation in rats. Neuropsychopharmacology, 32, 562-576. Korostishevsky, M., Kaganovich, M., Cholostoy, A. et al. (2004) Is the G72/G30 locus associated with schizophrenia? single nucleotide polymorphisms, haplotypes, and gene expression analysis. Biol Psychiatry, 56, 169-176. Kovelman, J. A. and Scheibel, A. B. (1984) A neurohistological correlate of schizophrenia. Biol Psychiatry, 19, 1601-1621. Krystal, J. H., Karper, L. P., Seibyl, J. P., Freeman, G. K., Delaney, R., Bremner, J. D., Heninger, G. R., Bowers, M. B., Jr. and Charney, D. S. (1994) Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry, 51, 199-214. Kutsuwada, T., Kashiwabuchi, N., Mori, H. et al. (1992) Molecular diversity of the NMDA receptor channel. Nature, 358, 36-41. Lahti, A. C., Holcomb, H. H., Medoff, D. R. and Tamminga, C. A. (1995) Ketamine activates psychosis and alters limbic blood flow in schizophrenia. Neuroreport, 6, 869-872. Lahti, A. C., Weiler, M. A., Tamara Michaelidis, B. A., Parwani, A. and Tamminga, C. A. (2001) Effects of ketamine in normal and schizophrenic volunteers. Neuropsychopharmacology, 25, 455-467. Lan, J. Y., Skeberdis, V. A., Jover, T., Grooms, S. Y., Lin, Y., Araneda, R. C., Zheng, X., Bennett, M. V. and Zukin, R. S. (2001) Protein kinase C modulates NMDA receptor trafficking and gating. Nat Neurosci, 4, 382390. Lane, H. Y., Huang, C. L., Wu, P. L., Liu, Y. C., Chang, Y. C., Lin, P. Y., Chen, P. W. and Tsai, G. (2006) Glycine transporter I inhibitor, N-methylglycine (sarcosine), added to clozapine for the treatment of schizophrenia. Biol Psychiatry, 60, 645-649. Large, C. H. (2007) Do NMDA receptor antagonist models of schizophrenia predict the clinical efficacy of antipsychotic drugs? J Psychopharmacol, 21, 283-301. 157 Largent, B. L., Gundlach, A. L. and Snyder, S. H. (1984) Psychotomimetic opiate receptors labeled and visualized with (+)-[3H]3-(3-hydroxyphenyl)-N-(1propyl)piperidine. Proc Natl Acad Sci U S A, 81, 4983-4987. Lau, G. C., Saha, S., Faris, R. and Russek, S. J. (2004) Up-regulation of NMDAR1 subunit gene expression in cortical neurons via a PKAdependent pathway. J Neurochem, 88, 564-575. Laurie, D. J. and Seeburg, P. H. (1994) Ligand affinities at recombinant Nmethyl-D-aspartate receptors depend on subunit composition. Eur J Pharmacol, 268, 335-345. Lee, J. M., Zipfel, G. J. and Choi, D. W. (1999) The changing landscape of ischaemic brain injury mechanisms. Nature, 399, A7-14. Legault, M., Rompre, P. P. and Wise, R. A. (2000) Chemical stimulation of the ventral hippocampus elevates nucleus accumbens dopamine by activating dopaminergic neurons of the ventral tegmental area. J Neurosci, 20, 16351642. Lei, G., Anastasio, N., Fu, Y., Neugebauer, V. and Johnson, K. M. (2009) Activation of Dopamine D1 Receptors Prevents Phencyclidine-Induced Neurotoxicity by Enhancing Synaptic NMDA Receptor Strength. Journal of Neurochemistry, under review. Lei, G., Xia, Y. and Johnson, K. M. (2008) The role of Akt-GSK-3beta signaling and synaptic strength in phencyclidine-induced neurodegeneration. Neuropsychopharmacology, 33, 1343-1353. Lei, S. Z., Zhang, D., Abele, A. E. and Lipton, S. A. (1992) Blockade of NMDA receptor-mediated mobilization of intracellular Ca2+ prevents neurotoxicity. Brain Res, 598, 196-202. Lewis, D. A. (1997) Schizophrenia and disordered neural circuitry. Schizophr Bull, 23, 529-531. Lewis, D. A. and Lieberman, J. A. (2000) Catching up on schizophrenia: natural history and neurobiology. Neuron, 28, 325-334. Li, P. A., Howlett, W., He, Q. P., Miyashita, H., Siddiqui, M. and Shuaib, A. (1998) Postischemic treatment with calpain inhibitor MDL 28170 ameliorates brain damage in a gerbil model of global ischemia. Neurosci Lett, 247, 1720. 158 Liao, G. Y., Wagner, D. A., Hsu, M. H. and Leonard, J. P. (2001) Evidence for direct protein kinase-C mediated modulation of N-methyl-D-aspartate receptor current. Mol Pharmacol, 59, 960-964. Lieberman, J. A. (1993) Understanding the mechanism of action of atypical antipsychotic drugs. A review of compounds in use and development. Br J Psychiatry Suppl, 7-18. Lisman, J. E., Coyle, J. T., Green, R. W., Javitt, D. C., Benes, F. M., Heckers, S. and Grace, A. A. (2008) Circuit-based framework for understanding neurotransmitter and risk gene interactions in schizophrenia. Trends Neurosci, 31, 234-242. Liu, A., Hoffman, P. W., Lu, W. and Bai, G. (2004a) NF-kappaB site interacts with Sp factors and up-regulates the NR1 promoter during neuronal differentiation. J Biol Chem, 279, 17449-17458. Liu, L., Wong, T. P., Pozza, M. F., Lingenhoehl, K., Wang, Y., Sheng, M., Auberson, Y. P. and Wang, Y. T. (2004b) Role of NMDA receptor subtypes in governing the direction of hippocampal synaptic plasticity. Science, 304, 1021-1024. Liu, X. Z., Xu, X. M., Hu, R. et al. (1997) Neuronal and glial apoptosis after traumatic spinal cord injury. J Neurosci, 17, 5395-5406. Liu, Y., Wong, T. P., Aarts, M. et al. (2007) NMDA receptor subunits have differential roles in mediating excitotoxic neuronal death both in vitro and in vivo. J Neurosci, 27, 2846-2857. Lodge, D. and Johnson, K. M. (1990) Noncompetitive excitatory amino acid receptor antagonists. Trends Pharmacol Sci, 11, 81-86. Lu, X., Rong, Y. and Baudry, M. (2000) Calpain-mediated degradation of PSD-95 in developing and adult rat brain. Neurosci Lett, 286, 149-153. Luby, E. D., Gottlieb, J. S., Cohen, B. D., Rosenbaum, G. and Domino, E. F. (1962) Model psychoses and schizophrenia. Am J Psychiatry, 119, 61-67. Lynch, D. R. and Guttmann, R. P. (2001) NMDA receptor pharmacology: perspectives from molecular biology. Curr Drug Targets, 2, 215-231. Lynch, D. R. and Guttmann, R. P. (2002) Excitotoxicity: perspectives based on N-methyl-D-aspartate receptor subtypes. J Pharmacol Exp Ther, 300, 717-723. 159 Maayani, S., Weinstein, H., Ben-Zvi, N., Cohen, S. and Sokolovsky, M. (1974) Psychotomimetics as anticholinergic agents. I. 1-Cyclohexylpiperidine derivatives: anticholinesterase activity and antagonistic activity to acetylcholine. Biochem Pharmacol, 23, 1263-1281. MacDonald, J. F., Miljkovic, Z. and Pennefather, P. (1987) Use-dependent block of excitatory amino acid currents in cultured neurons by ketamine. J Neurophysiol, 58, 251-266. Mansbach, R. S. and Geyer, M. A. (1989) Effects of phencyclidine and phencyclidine biologs on sensorimotor gating in the rat. Neuropsychopharmacology, 2, 299-308. Marenco, S. and Weinberger, D. R. (2000) The neurodevelopmental hypothesis of schizophrenia: following a trail of evidence from cradle to grave. Dev Psychopathol, 12, 501-527. Martel, M. A., Wyllie, D. J. and Hardingham, G. E. (2009) In developing hippocampal neurons, NR2B-containing N-methyl-d-aspartate receptors (NMDARs) can mediate signaling to neuronal survival and synaptic potentiation, as well as neuronal death. Neuroscience, 158, 334-343. Martin, P., Carlsson, M. L. and Hjorth, S. (1998) Systemic PCP treatment elevates brain extracellular 5-HT: a microdialysis study in awake rats. Neuroreport, 9, 2985-2988. Martinez, Z. A., Halim, N. D., Oostwegel, J. L., Geyer, M. A. and Swerdlow, N. R. (2000a) Ontogeny of phencyclidine and apomorphine-induced startle gating deficits in rats. Pharmacol Biochem Behav, 65, 449-457. Martinez, Z. A., Oostwegel, J., Geyer, M. A., Ellison, G. D. and Swerdlow, N. R. (2000b) "Early" and "late" effects of sustained haloperidol on apomorphine- and phencyclidine-induced sensorimotor gating deficits. Neuropsychopharmacology, 23, 517-527. Martinez, Z. A., Platten, A., Pollack, E., Shoemaker, J., Ro, H., Pitcher, L., Geyer, M. A. and Swerdlow, N. R. (2002) "Typical" but not "atypical" antipsychotic effects on startle gating deficits in prepubertal rats. Psychopharmacology (Berl), 161, 38-46. Mauceri, D., Gardoni, F., Marcello, E. and Di Luca, M. (2007) Dual role of CaMKII-dependent SAP97 phosphorylation in mediating trafficking and insertion of NMDA receptor subunit NR2A. J Neurochem, 100, 1032-1046. 160 McBain, C. J. and Mayer, M. L. (1994) N-methyl-D-aspartic acid receptor structure and function. Physiol Rev, 74, 723-760. McDonald, J. W., Silverstein, F. S., Cardona, D., Hudson, C., Chen, R. and Johnston, M. V. (1990a) Systemic administration of MK-801 protects against N-methyl-D-aspartate- and quisqualate-mediated neurotoxicity in perinatal rats. Neuroscience, 36, 589-599. McDonald, J. W., Silverstein, F. S. and Johnston, M. V. (1990b) MK-801 pretreatment enhances N-methyl-D-aspartate-mediated brain injury and increases brain N-methyl-D-aspartate recognition site binding in rats. Neuroscience, 38, 103-113. McGlashan, T. H. (1996a) Early detection and intervention in schizophrenia: editor's introduction. Schizophr Bull, 22, 197-199. McGlashan, T. H. (1996b) Early detection and intervention in schizophrenia: research. Schizophr Bull, 22, 327-345. McInnis, J., Wang, C., Anastasio, N., Hultman, M., Ye, Y., Salvemini, D. and Johnson, K. M. (2002) The role of superoxide and nuclear factor-kappaB signaling in N-methyl-D-aspartate-induced necrosis and apoptosis. J Pharmacol Exp Ther, 301, 478-487. Mechri, A., Saoud, M., Khiari, G., d'Amato, T., Dalery, J. and Gaha, L. (2001) [Glutaminergic hypothesis of schizophrenia: clinical research studies with ketamine]. Encephale, 27, 53-59. Moghaddam, B. (1994) Recent basic findings in support of excitatory amino acid hypotheses of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry, 18, 859-870. Moghaddam, B., Adams, B., Verma, A. and Daly, D. (1997) Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci, 17, 2921-2927. Monyer, H., Burnashev, N., Laurie, D. J., Sakmann, B. and Seeburg, P. H. (1994) Developmental and regional expression in the rat brain and functional properties of four NMDA receptors. Neuron, 12, 529-540. Morris, B. J., Cochran, S. M. and Pratt, J. A. (2005) PCP: from pharmacology to modelling schizophrenia. Curr Opin Pharmacol, 5, 101-106. 161 Mouri, A., Noda, Y., Enomoto, T. and Nabeshima, T. (2007) Phencyclidine animal models of schizophrenia: approaches from abnormality of glutamatergic neurotransmission and neurodevelopment. Neurochem Int, 51, 173-184. Murray, R. M., O'Callaghan, E., Castle, D. J. and Lewis, S. W. (1992) A neurodevelopmental approach to the classification of schizophrenia. Schizophr Bull, 18, 319-332. Murray, T. F. and Horita, A. (1979) Phencyclidine-induced stereotyped behavior in rats: dose response effects and antagonism by neuroleptics. Life Sci, 24, 2217-2225. Nath, R., Raser, K. J., McGinnis, K., Nadimpalli, R., Stafford, D. and Wang, K. K. (1996) Effects of ICE-like protease and calpain inhibitors on neuronal apoptosis. Neuroreport, 8, 249-255. Neyton, J. and Paoletti, P. (2006) Relating NMDA receptor function to receptor subunit composition: limitations of the pharmacological approach. J Neurosci, 26, 1331-1333. Nicolson, R., Lenane, M., Hamburger, S. D., Fernandez, T., Bedwell, J. and Rapoport, J. L. (2000) Lessons from childhood-onset schizophrenia. Brain Res Brain Res Rev, 31, 147-156. Niethammer, M., Kim, E. and Sheng, M. (1996) Interaction between the C terminus of NMDA receptor subunits and multiple members of the PSD-95 family of membrane-associated guanylate kinases. J Neurosci, 16, 21572163. Numakawa, T., Yagasaki, Y., Ishimoto, T. et al. (2004) Evidence of novel neuronal functions of dysbindin, a susceptibility gene for schizophrenia. Hum Mol Genet, 13, 2699-2708. Ogren, S. O. and Goldstein, M. (1994) Phencyclidine- and dizocilpine-induced hyperlocomotion are differentially mediated. Neuropsychopharmacology, 11, 167-177. Olney, J. W. and Farber, N. B. (1995a) Glutamate receptor dysfunction and schizophrenia. Arch Gen Psychiatry, 52, 998-1007. Olney, J. W. and Farber, N. B. (1995b) NMDA antagonists as neurotherapeutic drugs, psychotogens, neurotoxins, and research tools for studying schizophrenia. Neuropsychopharmacology, 13, 335-345. 162 Olney, J. W., Ikonomidou, C., Mosinger, J. L. and Frierdich, G. (1989a) MK-801 prevents hypobaric-ischemic neuronal degeneration in infant rat brain. J Neurosci, 9, 1701-1704. Olney, J. W., Labruyere, J. and Price, M. T. (1989b) Pathological changes induced in cerebrocortical neurons by phencyclidine and related drugs. Science, 244, 1360-1362. Olney, J. W., Wozniak, D. F., Jevtovic-Todorovic, V., Farber, N. B., Bittigau, P. and Ikonomidou, C. (2002) Drug-induced apoptotic neurodegeneration in the developing brain. Brain Pathol, 12, 488-498. Paoletti, P. and Neyton, J. (2007) NMDA receptor subunits: function and pharmacology. Curr Opin Pharmacol, 7, 39-47. Pavlik, A. and Teisinger, J. (1980) Effect of cycloheximide administered to rats in early postnatal life: prolonged inhibition of DNA synthesis in the developing brain. Brain Res, 192, 531-541. Pawlowski, L., Mathe, J. M. and Svensson, T. H. (1990) Phencyclidine activates rat A10 dopamine neurons but reduces burst activity and causes regularization of firing. Acta Physiol Scand, 139, 529-530. Paxinos, G. and Watson, C. (1986) The rat brain in stereotaxic coordinates. Academic Press, Sydney ; New York. Pechnick, R. N. and Hiramatsu, M. (1994) The effects of MK-801 on body temperature and behavior in the rat: cross-sensitization and crosstolerance with phencyclidine. Eur J Pharmacol, 252, 35-42. Phillips, M., Wang, C. and Johnson, K. M. (2001) Pharmacological characterization of locomotor sensitization induced by chronic phencyclidine administration. J Pharmacol Exp Ther, 296, 905-913. Pierce, R. C. and Kalivas, P. W. (1997) A circuitry model of the expression of behavioral sensitization to amphetamine-like psychostimulants. Brain Res Brain Res Rev, 25, 192-216. Pilowsky, L. S., Kerwin, R. W. and Murray, R. M. (1993) Schizophrenia: a neurodevelopmental perspective. Neuropsychopharmacology, 9, 83-91. Pisani, A., Gubellini, P., Bonsi, P., Conquet, F., Picconi, B., Centonze, D., Bernardi, G. and Calabresi, P. (2001) Metabotropic glutamate receptor 5 mediates the potentiation of N-methyl-D-aspartate responses in medium spiny striatal neurons. Neuroscience, 106, 579-587. 163 Pradet-Balade, B., Boulme, F., Beug, H., Mullner, E. W. and Garcia-Sanz, J. A. (2001) Translation control: bridging the gap between genomics and proteomics? Trends Biochem Sci, 26, 225-229. Prybylowski, K., Chang, K., Sans, N., Kan, L., Vicini, S. and Wenthold, R. J. (2005) The synaptic localization of NR2B-containing NMDA receptors is controlled by interactions with PDZ proteins and AP-2. Neuron, 47, 845857. Qiao, H., Noda, Y., Kamei, H., Nagai, T., Furukawa, H., Miura, H., Kayukawa, Y., Ohta, T. and Nabeshima, T. (2001) Clozapine, but not haloperidol, reverses social behavior deficit in mice during withdrawal from chronic phencyclidine treatment. Neuroreport, 12, 11-15. Qin, Z., Wang, Y. and Chasea, T. N. (2000) A caspase-3-like protease is involved in NF-kappaB activation induced by stimulation of N-methyl-Daspartate receptors in rat striatum. Brain Res Mol Brain Res, 80, 111-122. Raggi, M. A., Mandrioli, R., Sabbioni, C. and Pucci, V. (2004) Atypical antipsychotics: pharmacokinetics, therapeutic drug monitoring and pharmacological interactions. Curr Med Chem, 11, 279-296. Rasmussen, B. A., O'Neil, J., Manaye, K. F., Perry, D. C. and Tizabi, Y. (2007) Long-term effects of developmental PCP administration on sensorimotor gating in male and female rats. Psychopharmacology (Berl), 190, 43-49. Reynolds, G. P. and Beasley, C. L. (2001) GABAergic neuronal subtypes in the human frontal cortex--development and deficits in schizophrenia. J Chem Neuroanat, 22, 95-100. Reynolds, I. J. and Miller, R. J. (1989) Ifenprodil is a novel type of N-methyl-Daspartate receptor antagonist: interaction with polyamines. Mol Pharmacol, 36, 758-765. Robbins, T. W. (1990) The case of frontostriatal dysfunction in schizophrenia. Schizophr Bull, 16, 391-402. Robinson, T. E. and Berridge, K. C. (1993) The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Brain Res Rev, 18, 247-291. Ross, C. A., Margolis, R. L., Reading, S. A., Pletnikov, M. and Coyle, J. T. (2006a) Neurobiology of schizophrenia. Neuron, 52, 139-153. 164 Ross, R. G., Heinlein, S. and Tregellas, H. (2006b) High rates of comorbidity are found in childhood-onset schizophrenia. Schizophr Res, 88, 90-95. Rothman, S. M. and Olney, J. W. (1995) Excitotoxicity and the NMDA receptor-still lethal after eight years. Trends Neurosci, 18, 57-58. Rubinfeld, B., Albert, I., Porfiri, E., Fiol, C., Munemitsu, S. and Polakis, P. (1996) Binding of GSK3beta to the APC-beta-catenin complex and regulation of complex assembly. Science, 272, 1023-1026. Saido, T. C., Sorimachi, H. and Suzuki, K. (1994) Calpain: new perspectives in molecular diversity and physiological-pathological involvement. FASEB J, 8, 814-822. Sams-Dodd, F. (1995) Automation of the social interaction test by a videotracking system: behavioural effects of repeated phencyclidine treatment. J Neurosci Methods, 59, 157-167. Sams-Dodd, F. (1996) Phencyclidine-induced stereotyped behaviour and social isolation in rats: a possible animal model of schizophrenia. Behav Pharmacol, 7, 3-23. Sams-Dodd, F. (1998) A test of the predictive validity of animal models of schizophrenia based on phencyclidine and D-amphetamine. Neuropsychopharmacology, 18, 293-304. Sams-Dodd, F. (1999) Phencyclidine in the social interaction test: an animal model of schizophrenia with face and predictive validity. Rev Neurosci, 10, 59-90. Sans, N., Petralia, R. S., Wang, Y. X., Blahos, J., 2nd, Hell, J. W. and Wenthold, R. J. (2000) A developmental change in NMDA receptor-associated proteins at hippocampal synapses. J Neurosci, 20, 1260-1271. Sans, N., Prybylowski, K., Petralia, R. S., Chang, K., Wang, Y. X., Racca, C., Vicini, S. and Wenthold, R. J. (2003) NMDA receptor trafficking through an interaction between PDZ proteins and the exocyst complex. Nat Cell Biol, 5, 520-530. Scallet, A. C., Schmued, L. C., Slikker, W., Jr. et al. (2004) Developmental neurotoxicity of ketamine: morphometric confirmation, exposure parameters, and multiple fluorescent labeling of apoptotic neurons. Toxicol Sci, 81, 364-370. 165 Scott, D. B., Blanpied, T. A. and Ehlers, M. D. (2003) Coordinated PKA and PKC phosphorylation suppresses RXR-mediated ER retention and regulates the surface delivery of NMDA receptors. Neuropharmacology, 45, 755767. Sharp, F. R., Tomitaka, M., Bernaudin, M. and Tomitaka, S. (2001) Psychosis: pathological activation of limbic thalamocortical circuits by psychomimetics and schizophrenia? Trends Neurosci, 24, 330-334. Shelley, A. M., Ward, P. B., Catts, S. V., Michie, P. T., Andrews, S. and McConaghy, N. (1991) Mismatch negativity: an index of a preattentive processing deficit in schizophrenia. Biol Psychiatry, 30, 1059-1062. Sherwood, N. M. and Timiras, P. S. (1970) A stereotaxic atlas of the developing rat brain. University of California Press, Berkeley, CA. Simpkins, K. L., Guttmann, R. P., Dong, Y., Chen, Z., Sokol, S., Neumar, R. W. and Lynch, D. R. (2003) Selective activation induced cleavage of the NR2B subunit by calpain. J Neurosci, 23, 11322-11331. Sircar, R. (2003) Postnatal phencyclidine-induced deficit in adult water maze performance is associated with N-methyl-D-aspartate receptor upregulation. Int J Dev Neurosci, 21, 159-167. Sircar, R., Follesa, P. and Ticku, M. K. (1996) Postnatal phencyclidine treatment differentially regulates N-methyl-D-aspartate receptor subunit mRNA expression in developing rat cerebral cortex. Brain Res Mol Brain Res, 40, 214-220. Sircar, R. and Sircar, D. (2006) Repeated ethanol treatment in adolescent rats alters cortical NMDA receptor. Alcohol, 39, 51-58. Smith, R. C., Meltzer, H. Y., Arora, R. C. and Davis, J. M. (1977) Effects of phencyclidine on [3H]catecholamine and [3H]serotonin uptake in synaptosomal preparations from rat brain. Biochem Pharmacol, 26, 14351439. Snell, L. D., Yi, S. J. and Johnson, K. M. (1988) Comparison of the effects of MK801 and phencyclidine on catecholamine uptake and NMDA-induced norepinephrine release. Eur J Pharmacol, 145, 223-226. Snigdha, S. and Neill, J. C. (2008) Efficacy of antipsychotics to reverse phencyclidine-induced social interaction deficits in female rats-A preliminary investigation. Behav Brain Res, 187, 489-494. 166 Soriano, F. X. and Hardingham, G. E. (2007) Compartmentalized NMDA receptor signalling to survival and death. J Physiol, 584, 381-387. Soriano, F. X., Papadia, S., Hofmann, F., Hardingham, N. R., Bading, H. and Hardingham, G. E. (2006) Preconditioning doses of NMDA promote neuroprotection by enhancing neuronal excitability. J Neurosci, 26, 45094518. Spooren, W., Mombereau, C., Maco, M., Gill, R., Kemp, J. A., Ozmen, L., Nakanishi, S. and Higgins, G. A. (2004) Pharmacological and genetic evidence indicates that combined inhibition of NR2A and NR2B subunit containing NMDA receptors is required to disrupt prepulse inhibition. Psychopharmacology (Berl), 175, 99-105. Standley, S., Roche, K. W., McCallum, J., Sans, N. and Wenthold, R. J. (2000) PDZ domain suppression of an ER retention signal in NMDA receptor NR1 splice variants. Neuron, 28, 887-898. Steinpreis, R. E. (1996) The behavioral and neurochemical effects of phenyclidine in humans and animals: some implications for modeling psychosis. Behav Brain Res, 74, 45-55. Steinpreis, R. E. and Salamone, J. D. (1993) The role of nucleus accumbens dopamine in the neurochemical and behavioral effects of phencyclidine: a microdialysis and behavioral study. Brain Res, 612, 263-270. Strous, R. D. and Javitt, D. C. (1996) The N-methyl-D-aspartate receptor and schizophrenia. Isr J Med Sci, 32, 275-281. Suvarna, N., Borgland, S. L., Wang, J., Phamluong, K., Auberson, Y. P., Bonci, A. and Ron, D. (2005) Ethanol alters trafficking and functional N-methyl-Daspartate receptor NR2 subunit ratio via H-Ras. J Biol Chem, 280, 3145031459. Swerdlow, N. R., Braff, D. L., Taaid, N. and Geyer, M. A. (1994) Assessing the validity of an animal model of deficient sensorimotor gating in schizophrenic patients. Arch Gen Psychiatry, 51, 139-154. Swerdlow, N. R., Lipska, B. K., Weinberger, D. R., Braff, D. L., Jaskiw, G. E. and Geyer, M. A. (1995) Increased sensitivity to the sensorimotor gatingdisruptive effects of apomorphine after lesions of medial prefrontal cortex or ventral hippocampus in adult rats. Psychopharmacology (Berl), 122, 2734. 167 Takadera, T., Matsuda, I. and Ohyashiki, T. (1999) Apoptotic cell death and caspase-3 activation induced by N-methyl-D-aspartate receptor antagonists and their prevention by insulin-like growth factor I. J Neurochem, 73, 548-556. Taube, H. D., Montel, H., Hau, G. and Starke, K. (1975) Phencyclidine and ketamine: comparison with the effect of cocaine on the noradrenergic neurones of the rat brain cortex. Naunyn Schmiedebergs Arch Pharmacol, 291, 47-54. Terranova, J. P., Chabot, C., Barnouin, M. C., Perrault, G., Depoortere, R., Griebel, G. and Scatton, B. (2005) SSR181507, a dopamine D(2) receptor antagonist and 5-HT(1A) receptor agonist, alleviates disturbances of novelty discrimination in a social context in rats, a putative model of selective attention deficit. Psychopharmacology (Berl), 181, 134-144. Thomas, C. G., Miller, A. J. and Westbrook, G. L. (2006) Synaptic and extrasynaptic NMDA receptor NR2 subunits in cultured hippocampal neurons. J Neurophysiol, 95, 1727-1734. Tovar, K. R. and Westbrook, G. L. (1999) The incorporation of NMDA receptors with a distinct subunit composition at nascent hippocampal synapses in vitro. J Neurosci, 19, 4180-4188. Tovar, K. R. and Westbrook, G. L. (2002) Mobile NMDA receptors at hippocampal synapses. Neuron, 34, 255-264. Tran, D. H., Gong, R. and Tang, S.-J. (2007) Differential roles of NR2A and NR2B subtypes in NMDA receptor-dependent protein synthesis in dendrites. Neuropharmacology, 53, 252-256. Tsutsumi, T., Hirano, M., Matsumoto, T. et al. (1995) Involvement of dopamine D1 receptors in phencyclidine-induced behavioral stimulation in rats. Clin Neuropharmacol, 18, 64-71. Umbricht, D., Schmid, L., Koller, R., Vollenweider, F. X., Hell, D. and Javitt, D. C. (2000) Ketamine-induced deficits in auditory and visual context-dependent processing in healthy volunteers: implications for models of cognitive deficits in schizophrenia. Arch Gen Psychiatry, 57, 1139-1147. Vaisanen, J., Ihalainen, J., Tanila, H. and Castren, E. (2004) Effects of NMDAreceptor antagonist treatment on c-fos expression in rat brain areas implicated in schizophrenia. Cell Mol Neurobiol, 24, 769-780. 168 van Zundert, B., Yoshii, A. and Constantine-Paton, M. (2004) Receptor compartmentalization and trafficking at glutamate synapses: a developmental proposal. Trends Neurosci, 27, 428-437. Vanderklish, P. W. and Bahr, B. A. (2000) The pathogenic activation of calpain: a marker and mediator of cellular toxicity and disease states. Int J Exp Pathol, 81, 323-339. Vanderschuren, L. J., Schoffelmeer, A. N., Mulder, A. H. and De Vries, T. J. (1998) Dizocilpine (MK801): use or abuse? Trends Pharmacol Sci, 19, 7981. Vanhoutte, P. and Bading, H. (2003) Opposing roles of synaptic and extrasynaptic NMDA receptors in neuronal calcium signalling and BDNF gene regulation. Curr Opin Neurobiol, 13, 366-371. Verebey, K., Kogan, M. J. and Mule, S. J. (1981) Phencyclidine-induced stereotype in rats: effects of methadone, apomorphine, and naloxone. Psychopharmacology (Berl), 75, 44-47. Verma, A. and Moghaddam, B. (1996) NMDA receptor antagonists impair prefrontal cortex function as assessed via spatial delayed alternation performance in rats: modulation by dopamine. J Neurosci, 16, 373-379. Vickers, A. E. M. and Fisher, R. L. (2004) Organ slices for the evaluation of human drug toxicity. Chemico-Biological Interactions, 150, 87-96. Vincent, J. P., Bidard, J. N., Lazdunski, M., Romey, G., Tourneur, Y. and Vignon, J. (1983) Identification and properties of phencyclidine-binding sites in nervous tissues. Fed Proc, 42, 2570-2573. Wang, C., Fridley, J. and Johnson, K. M. (2005) The role of NMDA receptor upregulation in phencyclidine-induced cortical apoptosis in organotypic culture. Biochem Pharmacol, 69, 1373-1383. Wang, C., McInnis, J., Ross-Sanchez, M., Shinnick-Gallagher, P., Wiley, J. L. and Johnson, K. M. (2001) Long-term behavioral and neurodegenerative effects of perinatal phencyclidine administration: implications for schizophrenia. Neuroscience, 107, 535-550. Wang, C., McInnis, J., West, J. B., Bao, J., Anastasio, N., Guidry, J. A., Ye, Y., Salvemini, D. and Johnson, K. M. (2003) Blockade of phencyclidineinduced cortical apoptosis and deficits in prepulse inhibition by M40403, a superoxide dismutase mimetic. J Pharmacol Exp Ther, 304, 266-271. 169 Wang, C., Showalter, V. M., Hillman, G. R. and Johnson, K. M. (1999) Chronic phencyclidine increases NMDA receptor NR1 subunit mRNA in rat forebrain. J Neurosci Res, 55, 762-769. Wang, C. Z. and Johnson, K. M. (2005) Differential effects of acute and subchronic administration on phencyclidine-induced neurodegeneration in the perinatal rat. J Neurosci Res, 81, 284-292. Wang, C. Z. and Johnson, K. M. (2007) The role of caspase-3 activation in phencyclidine-induced neuronal death in postnatal rats. Neuropsychopharmacology, 32, 1178-1194. Wang, C. Z., Yang, S. F., Xia, Y. and Johnson, K. M. (2008) Postnatal Phencyclidine Administration Selectively Reduces Adult Cortical Parvalbumin-Containing Interneurons. Neuropsychopharmacology, 33, 2442-2455. Wang, R. Y. and Liang, X. (1998) M100907 and clozapine, but not haloperidol or raclopride, prevent phencyclidine-induced blockade of NMDA responses in pyramidal neurons of the rat medial prefrontal cortical slice. Neuropsychopharmacology, 19, 74-85. Waxman, E. A. and Lynch, D. R. (2005) N-methyl-D-aspartate receptor subtypes: multiple roles in excitotoxicity and neurological disease. Neuroscientist, 11, 37-49. Wechsler, A. and Teichberg, V. I. (1998) Brain spectrin binding to the NMDA receptor is regulated by phosphorylation, calcium and calmodulin. EMBO J, 17, 3931-3939. Weinberger, D. R. (1987) Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry, 44, 660-669. Weinberger, D. R. (1996) On the plausibility of "the neurodevelopmental hypothesis" of schizophrenia. Neuropsychopharmacology, 14, 1S-11S. Weinberger, D. R. (2000) Neurodevelopmental Perspectives on Schizophrenia. In: American College of Neuropsychopharmacology Annual Meeting report. Weissman, A. D., Marquis, K. L., Moreton, J. E. and London, E. D. (1989) Effects of self-administered phencyclidine on regional uptake of 2-deoxy-D-[114C]glucose in brain. Neuropharmacology, 28, 575-583. 170 Wenthold, R. J., Prybylowski, K., Standley, S., Sans, N. and Petralia, R. S. (2003) Trafficking of NMDA receptors. Annu Rev Pharmacol Toxicol, 43, 335-358. Westbrook, G. L., Krupp, J. J. and Vissel, B. (1997) Cytoskeletal interactions with glutamate receptors at central synapses. Soc Gen Physiol Ser, 52, 163175. Wiley, J. L. (1998) Nitric oxide synthase inhibitors attenuate phencyclidineinduced disruption of prepulse inhibition. Neuropsychopharmacology, 19, 86-94. Wiley, J. L., Buhler, K. G., Lavecchia, K. L. and Johnson, K. M. (2003a) Pharmacological challenge reveals long-term effects of perinatal phencyclidine on delayed spatial alternation in rats. Prog Neuropsychopharmacol Biol Psychiatry, 27, 867-873. Wiley, J. L., Harvey, S. A., Balster, R. L. and Nicholson, K. L. (2003b) Affinity and specificity of N-methyl- D-aspartate channel blockers affect their ability to disrupt prepulse inhibition of acoustic startle in rats. Psychopharmacology (Berl), 165, 378-385. Williams, K. (2001) Ifenprodil, a novel NMDA receptor antagonist: site and mechanism of action. Curr Drug Targets, 2, 285-298. Wilson, M. A., Kinsman, S. L. and Johnston, M. V. (1998) Expression of NMDA receptor subunit mRNA after MK-801 treatment in neonatal rats. Brain Res Dev Brain Res, 109, 211-220. Wozniak, D. F., Hartman, R. E., Boyle, M. P., Vogt, S. K., Brooks, A. R., Tenkova, T., Young, C., Olney, J. W. and Muglia, L. J. (2004) Apoptotic neurodegeneration induced by ethanol in neonatal mice is associated with profound learning/memory deficits in juveniles followed by progressive functional recovery in adults. Neurobiol Dis, 17, 403-414. Wu, H. Y., Hsu, F. C., Gleichman, A. J., Baconguis, I., Coulter, D. A. and Lynch, D. R. (2007) Fyn-mediated Phosphorylation of NR2B Tyr-1336 Controls Calpain-mediated NR2B Cleavage in Neurons and Heterologous Systems. J Biol Chem, 282, 20075-20087. Wu, H. Y. and Lynch, D. R. (2006) Calpain and synaptic function. Mol Neurobiol, 33, 215-236. 171 Wu, H. Y., Yuen, E. Y., Lu, Y. F., Matsushita, M., Matsui, H., Yan, Z. and Tomizawa, K. (2005) Regulation of N-methyl-D-aspartate receptors by calpain in cortical neurons. J Biol Chem, 280, 21588-21593. Xia, Y., Wang, C. Z., Liu, J., Anastasio, N. C. and Johnson, K. M. (2008) Lithium protection of phencyclidine-induced neurotoxicity in developing brain: the role of phosphatidylinositol-3 kinase/Akt and mitogen-activated protein kinase kinase/extracellular signal-regulated kinase signaling pathways. J Pharmacol Exp Ther, 326, 838-848. Xu, X. and Domino, E. F. (1994) Asymmetric cross-sensitization to the locomotor stimulant effects of phencyclidine and MK-801. Neurochem Int, 25, 155159. Yamada, Y., Chochi, Y., Ko, J. A., Sobue, K. and Inui, M. (1999a) Activation of channel activity of the NMDA receptor-PSD-95 complex by guanylate kinase-associated protein (GKAP). FEBS Lett, 458, 295-298. Yamada, Y., Chochi, Y., Takamiya, K., Sobue, K. and Inui, M. (1999b) Modulation of the channel activity of the epsilon2/zeta1-subtype N-methyl D-aspartate receptor by PSD-95. J Biol Chem, 274, 6647-6652. Yamashima, T. (2004) Ca2+-dependent proteases in ischemic neuronal death: a conserved 'calpain-cathepsin cascade' from nematodes to primates. Cell Calcium, 36, 285-293. Young, C., Jevtovic-Todorovic, V., Qin, Y. Q., Tenkova, T., Wang, H., Labruyere, J. and Olney, J. W. (2005) Potential of ketamine and midazolam, individually or in combination, to induce apoptotic neurodegeneration in the infant mouse brain. Br J Pharmacol, 146, 189-197. Zhang, S. J., Steijaert, M. N., Lau, D., Schutz, G., Delucinge-Vivier, C., Descombes, P. and Bading, H. (2007) Decoding NMDA Receptor Signaling: Identification of Genomic Programs Specifying Neuronal Survival and Death. Neuron, 53, 549-562. Zheng, X., Zhang, L., Wang, A. P., Araneda, R. C., Lin, Y., Zukin, R. S. and Bennett, M. V. (1999) Mutation of structural determinants lining the Nmethyl-D-aspartate receptor channel differentially affects phencyclidine block and spermine potentiation and block. Neuroscience, 93, 125-134. Zhou, M. and Baudry, M. (2006) Developmental changes in NMDA neurotoxicity reflect developmental changes in subunit composition of NMDA receptors. J Neurosci, 26, 2956-2963. 172 Vita Noelle Anastasio was born on December 16, 1978 to Philip and Barbra Anastasio in Metairie, Louisiana. After college, she worked as a research assistant for Dr. Kenneth M. Johnson in the Pharmacology and Toxicology department at University of Texas Medical Branch in Galveston, Texas. In August, 2003, she enrolled in the M.S. program in the department of Pharmacology and Toxicology at UTMB and completed her degree in August, 2005. In 2006, she was awarded a Ruth L. Kirschstein NRSA F31 Fellowship from the National Institute on Drug Abuse to pursue her doctoral studies. During the 2007-2008 academic year, she was chosen as a Bromberg Scholar which entailed serving as a scientific research mentor to a local high school student, Zoe O’Connor. In 2008, she was awarded the James E. Beall II Memorial Award in Anatomy and Neurosciences. Education B.A. 2001, University of Texas at Austin, Austin TX M.S. 2005, University of Texas Medical Branch, Galveston TX Publications in Peer-Reviewed Journals Anastasio NC, Xia Y, O’Connor ZR, and Johnson KM (2009) NR2A-containing Synaptic NMDA Receptors Mediate Phencyclidine-Induced Neurotoxicity and the Subsequent Development of Schizophrenia-Like Behaviors in the Rat Neuroscience in revision Lei G, Anastasio NC, Fu Y, Neugebauer V, and Johnson KM (2008) Activation of Dopamine D1 Receptors Prevents Phencyclidine-Induced Neurotoxicity by Enhancing Synaptic NMDA Receptor Strength. Journal of Neurochemistry accepted 2009 Feb 26 Xia Y, Wang CZ, Liu Jie, Anastasio NC, and Johnson KM (2008) Lithium Protection of Phencyclidine-Induced Neurotoxicity in Developing Brain: The Role of PI-3 Kinase and MEK/ERK Signaling Pathways. Journal of Pharmacology and Experimental Therapeutics 326(3):838-48 Anastasio NC and Johnson KM (2008b) Atypical Antischizophrenic Drugs Prevent Changes in Cortical N-methyl-D-Aspartate Receptors and Behavior Following Sub-Chronic Phencyclidine Administration in Developing Rats. Pharmacology, Biochemistry and Behavior 90(4):569-77 Anastasio NC and Johnson KM (2008a) Differential Regulation of the N-methylD-Aspartate Receptor by Acute and Sub-chronic Phencyclidine Administration in the Developing Rat. Journal of Neurochemistry 104(5):1210-8 Wang C, Anastasio NC, Popov V, LeDay A, and Johnson KM (2004) Blockade of N-Methyl-D-Aspartate by Phencyclidine Causes the Loss of Corticostriatal Neurons. Neuroscience 125:473-483 Wang C, McInnis J, West J, Bao J, Anastasio NC, Guidry J, Ye Y, Salvemini D, and Johnson KM (2003) Blockade of Phencyclidine-Induced Cortical Apoptosis and Deficits in Prepulse Inhibition by M40403, a Superoxide Dismutase Mimetic. Journal of Pharmacology and Experimental Therapeutics 304(1):266-271 McInnis J, Wang C, Anastasio NC, Hultman M, Ye Y, Salvemini D, and Johnson KM (2002) The Role of Superoxide and Nuclear Factor-B Signaling in NMethyl-D-Aspartate Induced Necrosis and Apoptosis. Journal of Pharmacology and Experimental Therapeutics 301(2):478-487 Abstracts Anastasio NC, Xia Y, Wang CZ and Johnson KM (2008) The role of NMDAR 2A and 2B in PCP-induced neurotoxicity and development of locomotor sensitization. College on Problems of Drug Dependence. San Juan, Puerto Rico Anastasio NC, Xia Y, Wang CZ and Johnson KM (2008) Synaptic versus extrasynaptic NMDA receptors: Role in PCP-induced neurotoxicity and development of locomotor sensitization. Experimental Biology/ASPET. San Diego, CA Xia Y, Wang CZ, Anastasio NC and Johnson KM (2008) BDNF protects against phencyclidine neurotoxicity in neonatal brain via activation of the PI-3K/Akt/GSK3β and MEK/ERK pathways. Experimental Biology/ASPET. San Diego, CA Anastasio NC, Xia Y, and Johnson KM (2007) PCP-treatment dependent differential regulation of the NMDAR is dependent on PSD-95 expression and mediated by calpain. Canada College on Problems of Drug Dependence. Quebec City, Xia Y, Wang CZ, Anastasio NC and Johnson KM (2007) Lithium protection of phencyclidine neurotoxicity in neonatal brain is mediated by brain-derived neurotrophic factor activation of MEK/ERK signaling. Experimental Biology/ASPET. Washington, D.C. Xia Y, Wang CZ, Anastasio NC and Johnson KM (2006) Lithium chloride protection of phencyclidine-induced neurotoxicity in corticostriatal slices. The NIMH, Division of Intramural Research Programs, the first Pre-doctoral Research Festival. Washington, D.C. Anastasio NC and Johnson KM (2006) PCP-induced regulation of the NMDAR and development of locomotor sensitization. College on Problems of Drug Dependence. Scottsdale, AZ Anastasio NC and Johnson KM (2006) Effects of typical and atypical antipsychotics in a PCP-induced behavioral model of schizophrenia. Experimental Biology/ASPET. San Francisco, CA Anastasio NC and Johnson KM (2005) Pharmacological analysis of phencyclidine-induced regulation of the NMDA receptor. American Society for Neurochemistry. Madison, WI Anastasio NC and Johnson KM (2005) Pharmacological analysis of PCPinduced regulation of the NMDA receptor. National Student Research Forum. Galveston, TX Anastasio NC and Johnson KM (2004) Effect of olanzapine on PCP-induced changes in the N-Methyl-D-Aspartate receptor (NMDAR). Society for Neuroscience. San Diego, CA Anastasio NC and Johnson KM (2004) Role of NF-B in NMDA-induced cell death in cultured neurons. International Society of Neurochemistry: Advanced School of Neurochemistry. Avignon, France Wang C, Anastasio NC, Geng T, LeDay A, and Johnson KM (2003) Phencyclidine-induced cortical apoptosis is associated with reduced PSA-NCAM and synaptophysin in the striatum. Society for Neuroscience. New Orleans, LA Johnson KM, McInnis J, Wang CZ, Anastasio NC, Bao J, Ye Y, and Wang C (2003) Regional specificity and time course of phencyclidine-induced apoptosis in rat brain. Experimental Biology/ASPET. San Diego, CA Wang C, Bao J, Guidry J, West J, Anastasio NC, Ye Y, Robeson N, McInnis J, and Johnson KM (2002) Association of phencyclidine-induced cortical apoptosis with reduced PSA-NCAM expression in the nucleus accumbens. Society for Neuroscience. Orlando, FL Guidry J, Bao J, Wang C, Anastasio NC, Ye Y, Robeson N, and Johnson KM (2002) NMDA-induced neuronal apoptosis is mediated by an early increase in nuclear NF-B p50 and p65 proteins. Society for Neuroscience. Orlando, FL Permanent address: 1750 League City Pkwy Apt 223 League City, Texas 77573 This dissertation was typed by Noelle C. Anastasio.