THE ROLE OF TWO TUMOUR MARKERS – SQUAMOUR CELL
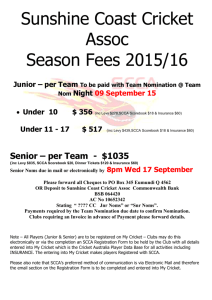
advertisement

THE ROLE OF TWO TUMOUR MARKERS – SQUAMOUR CELL CARCINOMA ANTIGEN AND CARCINOEMBRYONIC ANTIGEN IN THE MONITORING OF PATIENTS WITH CARCINOMA OF THE CERVIX UTERI MANAGED AT KENYATTA NATIONAL HOSPITAL DR. WARAMBO B.A (MBCHB) Supervisors: 1. PROF. ORINDA D.A.O (B Pharm, PhD) DEPARTMENT OF CLINICAL CHEMISTRY 2. PROF.KIGONDU C.S (BSc, PhD) DEPARTMENT OF CLINICAL CHEMISTRY 3. DR. MUTUNGI A. (MBChB, MMed Obs/Gyn) DEPARTMENT OF OBSTETRICS AND GYNAECOLOGY 4. DR. RANA F.S. (MBChB, MMed Path) DEPARTMENT OF PATHOLGY Degree: MMed Pathology 1998 SUMMARY The serum levels of two tumour markers, squamous cell carcinoma antigen (SCCA) and carcinoembryonic antigen (CEA) were measured in 75 patients with primary cervical cancer to determine the correlation with the clinical presence of tumour and response to radiation therapy and also in 75 control subjects. The results showed that 76% (57/75) of the patients with malignant disease had elevated (greater than 2.5ng/ml) pre-therapeutic levels of SCCA and 100% (75/75) of the control subjects had titres of this marker below the cut off of 2.5ng/ml. the mean titres of SCCA for the cases of malignant disease was 20.9 ± 30.9ng/ml, significantly higher (p<0.001) than that recorded for the control group of 0.3 ± 0.4ng/ml. The positive predictive value of a single serum SCCA titre greater than 2.5ng/ml was 76% while a value less than 2.5ng/ml was 77.4% specific for absence of disease. The mean titres for stage I through IV were 0.8, 16.9, 25.7 and 14.2ng/ml respectively with an overall higher mean for late disease than for early disease. Within the squamous cell variant the expression of this antigen was related to degree of differentiation of the tumour cells with the titres falling with loss of differentiation. None of the adenocarcinomas encountered were seropositive for this marker. Thirty three of the patients completed a course of radiotherapy during the study. They attained a post treatment mean for SCCA of 2.6ng/ml which was significantly lower (p less than 0.001) than their pre-therapeutic mean of 19.7ng/ml. Normalization of serum marker levels was achieved in 73.9% (17/23). On the other hand, 66.2% (49/74) of the patients with malignant disease had elevated (> 3.0ng/ml) titres of CEA while 86.6% of the control subjects had titres below the cut-off of 3.0gn/ml. The group mean titres of this marker for the cases was 26.2 ± 62.1ng/ml as against 2.1 ± 1.6ng/ml for the controls. The positive predictive values of a single titre above 3.0ng/ml was 68.6% while a value less than 3.0ng/ml was 68% specific for absence of disease. The association of this marker with disease stage was shown with mean levels for stage I, II, III, IV recoded as 35.1, 15.2, 34.8 and 43.6ng/ml respectively. The overall mean post-treatment titre of 10.6ng/ml, though above the cut-off value was significantly lower (p=0.005) than the pretherapeutic mean of 21.5 ± ng/ml. Only 20% (4/20) achieved normalization of marker levels following radiation therapy. While there was no relationship noted between the serum levels of this marker and tumour differentiation in squamous malignancies, both adenocarcinomas encountered were seropositive with a group mean of 10.6ng/ml. It is concluded that of the two tumour markers studies, SCCA correlated well with disease status in squamous cell carcimona of the uterine cervix and that its determination would be useful in monitoring progression of disease and in evaluating response to radiation therapy. It would provide a useful adjunct in the management of patients with this variant of cervical malignancy. CEA was also seen to correlate with disease process in carcinoma of the cervix. However, this correlation was weaker than that observed with SCCA. The small number of adenomatous tumours encountered did not allow the behavior of either marker to be conclusively studied.