Section 6 – Blood Component Transfusions
Chapter 464 – Red Blood Cell Transfusions and Erythropoietin Therapy
Ronald G. Strauss
Red blood cells (RBCs) are transfused to increase the oxygen-carrying capacity of the blood and, in
turn, to maintain satisfactory tissue oxygenation. Guidelines for RBC transfusions in children and
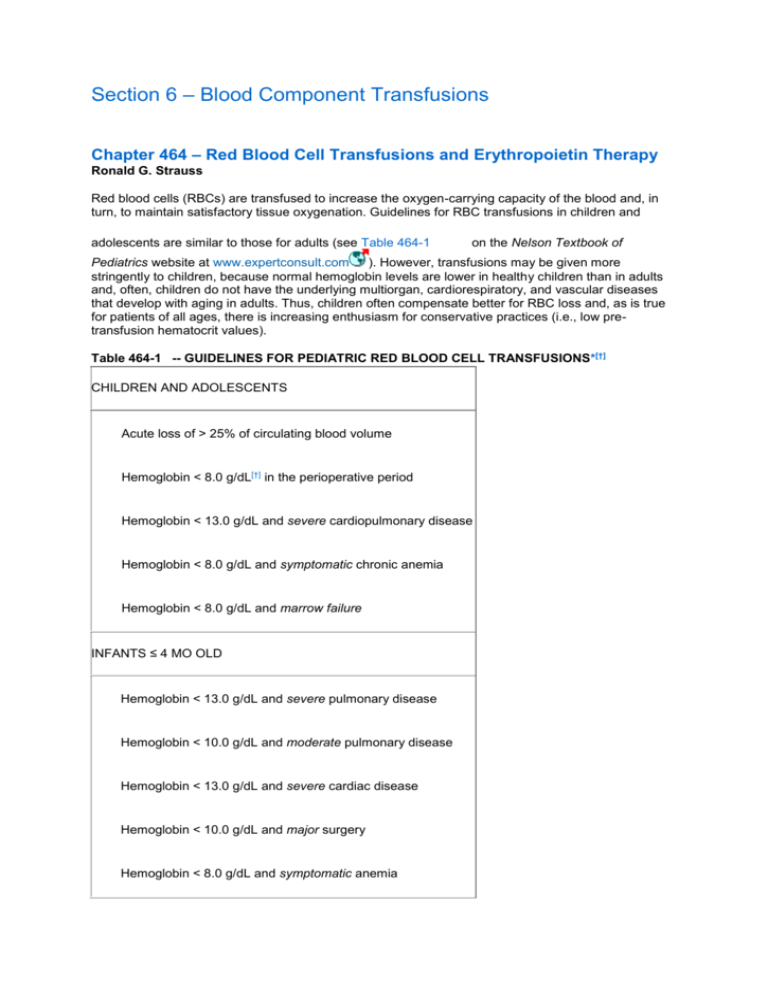
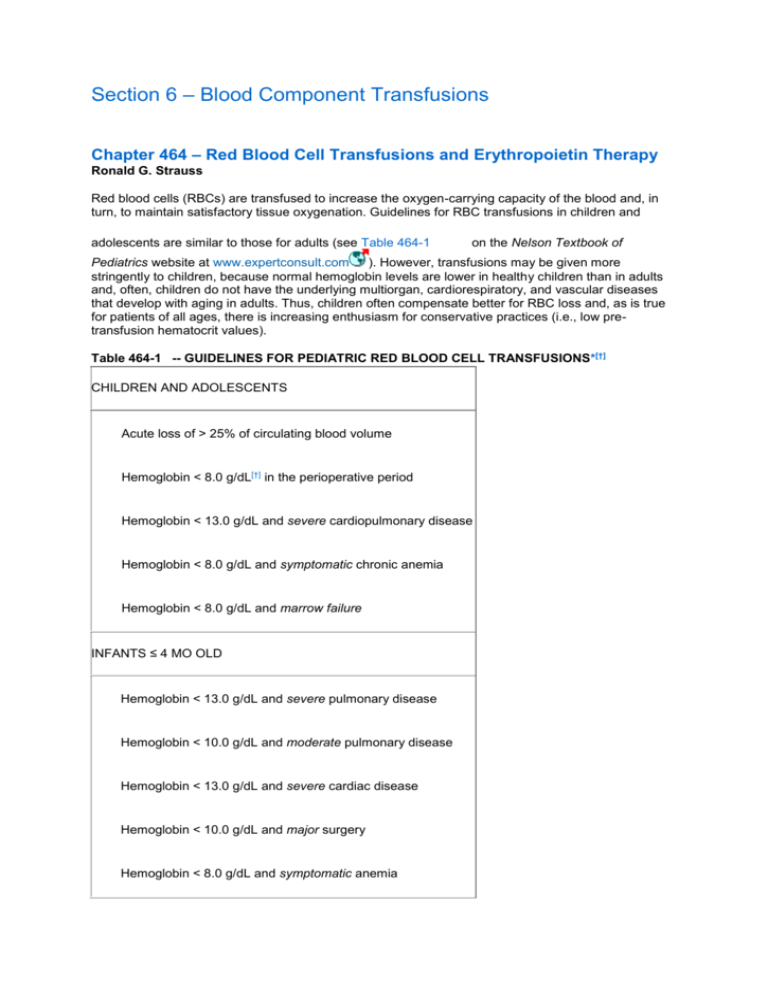
adolescents are similar to those for adults (see Table 464-1
on the Nelson Textbook of
Pediatrics website at www.expertconsult.com
). However, transfusions may be given more
stringently to children, because normal hemoglobin levels are lower in healthy children than in adults
and, often, children do not have the underlying multiorgan, cardiorespiratory, and vascular diseases
that develop with aging in adults. Thus, children often compensate better for RBC loss and, as is true
for patients of all ages, there is increasing enthusiasm for conservative practices (i.e., low pretransfusion hematocrit values).
Table 464-1 -- GUIDELINES FOR PEDIATRIC RED BLOOD CELL TRANSFUSIONS*[†]
CHILDREN AND ADOLESCENTS
Acute loss of > 25% of circulating blood volume
Hemoglobin < 8.0 g/dL[†] in the perioperative period
Hemoglobin < 13.0 g/dL and severe cardiopulmonary disease
Hemoglobin < 8.0 g/dL and symptomatic chronic anemia
Hemoglobin < 8.0 g/dL and marrow failure
INFANTS ≤ 4 MO OLD
Hemoglobin < 13.0 g/dL and severe pulmonary disease
Hemoglobin < 10.0 g/dL and moderate pulmonary disease
Hemoglobin < 13.0 g/dL and severe cardiac disease
Hemoglobin < 10.0 g/dL and major surgery
Hemoglobin < 8.0 g/dL and symptomatic anemia
* Words
in italics must be defined for local transfusion guidelines.
† Pre-transfusion
blood hemoglobin level (or hematocrit estimated by hemoglobin g/dL × 3) prompting a red blood cell
transfusion. Values vary among published reports and should be determined locally to fit best with practices judged to be
optimal by local MDs.
In the perioperative period, it is unnecessary for most children to maintain hemoglobin levels of 8 g/dL
or greater, a level frequently desired for adults. There should be a compelling reason to prescribe any
postoperative RBC transfusion, such as continued bleeding with hemodynamic instability, because
most children (without continued bleeding) can, over time, restore their RBC mass with iron therapy.
The most important measures in the treatments of acute hemorrhage are to control the hemorrhage
and to restore the circulating blood volume and tissue perfusion with crystalloid and/or colloid
solutions. If the estimated blood loss is > 25% of the circulating blood volume (>17 mL/kg) and the
patient's condition remains unstable, RBC transfusions may be indicated along with plasma
transfusions at a 1 : 1 ratio of RBC : plasma volumes. In acutely ill children with severe pulmonary
disease requiring assisted ventilation, it is common practice to maintain the hemoglobin level close to
the normal range, although the efficacy of this practice has not been documented by controlled
scientific studies.
The pre-transfusion blood hemoglobin level or hematocrit that should prompt a RBC transfusion is
controversial (i.e., restricted or a low pre-transfusion level vs liberal or a high pre-transfusion level)
despite a substantial amount of published information, including randomized clinical trials. Some
physicians in critical care settings prefer to transfuse RBCs quite conservatively (i.e., restricted
guidelines) and to permit modest anemia, because patients with levels close to the normal range (i.e.,
liberal guidelines) have poorer outcomes. Studies in critically ill adults demonstrated better outcomes
when the hemoglobin level was maintained at 7-9 g/dL than at 10-12 g/dL. However, anemic adults
with significant cardiac disease did better with hemoglobin levels maintained at 13 g/dL than at
10 g/dL. Similar studies in children admitted to intensive care units found no inferiority when RBC
transfusions were given by restricted guidelines (transfusion threshold of 7 g/dL), although the patients
were in stable clinical status and needed few transfusions. In contrast, unstable critically ill children
may need more liberal RBC transfusions.
With chronic anemia, the decision to transfuse RBCs should not be based solely on blood hemoglobin
levels, because children compensate well and may be asymptomatic despite low hemoglobin levels.
Patients with iron deficiency anemia are often treated successfully with oral iron alone, even at
hemoglobin levels < 5 g/dL. Factors other than hemoglobin concentration to be considered in the
decision to transfuse RBCs include: (1) the patient's symptoms, signs, and compensatory capacities;
(2) the presence of cardiorespiratory, vascular, and central nervous system disease; (3) the cause and
anticipated course of the anemia; and (4) alternative therapies, such as recombinant human
erythropoietin (EPO) therapy, which is known to reduce the need for RBC transfusions and to improve
the overall condition of children with chronic renal insufficiency (Chapter 529.2). In anemias that are
likely to be permanent, it is also important to balance the detrimental effects of anemia on growth and
development against the potential toxicity associated with repeated transfusions. RBC transfusions for
disorders such as sickle cell anemia and thalassemia are discussed in Chapters 456.1 and 456.9.
For neonates, nearly all aspects of RBC transfusions remain controversial (i.e., the accepted
indications for RBC transfusions, restricted vs liberal pre-transfusion hemoglobin/hematocrit levels,
optimal RBC product to be transfused) despite data from several controlled scientific studies.
Generally, RBCs are given to maintain a hemoglobin value believed to be the most desirable for each
neonate's clinical status (see Table 464-1). More restricted guidelines (i.e., lower pre-transfusion
hemoglobin/hematocrit levels) have been studied, but results are controversial, and conventional
guidelines are recommended until more definitive data are published (see Table 464-1). This clinical
approach is imprecise, but more physiologic indications, such as measurement of RBC mass,
available calculations of oxygen delivery and tissue extraction, and imaging of tissue perfusion, are too
cumbersome for clinical practice. Because definitive data are limited, it is important for pediatricians to
critically evaluate the need for neonatal RBC transfusions in light of the pathophysiologic need, as
discussed later.
During the first few weeks of life, all neonates experience a decline in circulating RBC mass caused
both by physiologic factors and, in sick premature infants, by phlebotomy blood losses. In healthy term
infants, the nadir hemoglobin value rarely falls to < 11 g/dL at an age of 10-12 wk. This “physiologic”
drop in RBCs does not require transfusions. In contrast, the decline occurs earlier and is more
pronounced in premature infants, even in those without complicating illnesses, in whom the mean
hemoglobin concentration falls to approximately 8 g/dL in infants of 1.0-1.5 kg birthweight and to
7 g/dL in infants weighing < 1.0 kg at birth. Most infants with birthweight <1.0 kg experience significant
“anemia of prematurity” and need RBC transfusions. A key reason that the nadir hemoglobin values of
premature infants are lower than those of term infants is the former group's relatively diminished
plasma EPO level in response to anemia (Chapters 97.1 and 440). The mechanisms responsible for
low plasma EPO levels are only partially defined. One factor is the reliance of preterm infants on the
liver as the primary site of EPO production during the first few weeks of life. The liver is less
responsive than the kidneys to anemia and tissue hypoxia. Thus, preterm infants exhibit a sluggish
EPO response to falling hematocrit values. The second factor is that EPO disappears more rapidly
from the plasma in infants than in adults (i.e., rapid clearance or metabolism).
Low plasma EPO levels provide a rationale for the use of recombinant EPO in the treatment of anemia
of prematurity. Proper doses of EPO and iron effectively stimulate neonatal erythropoiesis. However,
the efficacy of EPO therapy to substantially diminish the need for RBC transfusions has not been
convincingly demonstrated, particularly for sick, extremely premature neonates, and recombinant EPO
has not been widely accepted as a treatment for anemia of prematurity (Chapter 97.1). In rare cases,
some preparations of EPO have been associated with the development of anti-EPO antibodies in
adults that have produced severe anemia.
Because of the controversies over recombinant EPO therapy, many low birthweight preterm infants
need RBC transfusions (see Table 464-1). In neonatal patients with severe respiratory disease,
defined as requiring relatively large quantities of oxygen and ventilator support, it has been customary
to maintain blood hemoglobin at > 13 g/dL (hematocrit > 40%). Proponents believe that transfused
RBCs containing adult hemoglobin, with their superior interaction with 2,3-diphosphoglycerate and
leading to better oxygen offloading than that of fetal hemoglobin, are likely to provide optimal oxygen
delivery throughout the period of diminished pulmonary function. Although this practice is widely
recommended, little evidence is available to firmly establish its efficacy or to define its optimal use (the
best hemoglobin level for each degree of pulmonary dysfunction), and as mentioned earlier, more
restricted guidelines have been suggested. Infants with less severe cardiopulmonary disease may
require less vigorous support; hence, a lower hemoglobin level is suggested for those with only
moderate disease. Consistent with the rationale for oxygen delivery in neonates with severe
respiratory disease, it seems appropriate to keep the hemoglobin value > 13 g/dL (hematocrit > 40%)
in neonates with severe cardiac disease leading to either cyanosis or congestive heart failure.
The optimal hemoglobin level for neonates facing major surgery has not been established by definitive
studies. However, it seems reasonable to maintain the hemoglobin level at > 10 g/dL (hematocrit >
30%) because of the limited ability of a neonate's heart, lungs, and vasculature to compensate for
anemia; the inferior off-loading of oxygen because of the diminished interaction between fetal
hemoglobin and 2,3-diphosphoglycerate; and the developmental impairment of neonatal renal,
hepatic, and neurologic function. This transfusion guideline must be applied with flexibility to individual
infants facing different kinds of surgery.
Stable neonates do not require RBC transfusion, regardless of their blood hemoglobin levels, unless
they exhibit clinical problems attributable to anemia. Proponents of RBC transfusions for symptomatic
anemia believe that the low RBC mass contributes to tachypnea, dyspnea, tachycardia, apnea and
bradycardia, feeding difficulties, and lethargy, which can be alleviated by transfusion of RBCs.
However, anemia is only one of several possible causes of these problems, and RBC transfusions
should only be given when clinical problems are attributable to the anemia.
The RBC product of choice for children and adolescents is the standard suspension of RBCs
separated from whole blood by centrifugation and resuspended in an anticoagulant/preservative
storage solution at a hematocrit value of approximately 60% for storage up to 42 days, per U.S. Food
and Drug Administration (FDA) approval. The usual dose is 10-15 mL/kg, but transfusion volumes vary
greatly, depending on clinical circumstances (continued vs arrested bleeding, hemolysis). For
neonates, many centers transfuse the same RBC product as selected for older children, whereas
others prefer a packed RBC concentrate (hematocrit 70-90%). Either is infused slowly (over 2-4 hr) at
a dose of approximately 15 mL/kg. Because of the small quantity of extracellular fluid given at these
relatively high hematocrit values and the slow rate of transfusion, the type of RBC
anticoagulant/preservative solution used does not pose risks for premature infants. Packing RBCs by
centrifugation at the time the aliquot is issued for transfusion ensures that a consistent RBC dose is
infused with each transfusion but is not mandatory and is impractical for some blood banks.
The traditional use of relatively fresh RBCs (<7 days of storage) has been halted in many centers in
favor of diminishing donor exposure by using a single unit of RBCs to obtain aliquots for transfusing
each infant throughout its permitted duration of storage (currently 42 days). Neonatologists who insist
on transfusing only fresh RBCs generally are fearful of the rise in the plasma potassium (K +) level that
occurs in RBC units during extended storage. After 42 days of storage, plasma K+ levels are
approximately 50 mEq/L (0.05 mEq/mL), a value that, at 1st glance, seems alarmingly high. However,
the actual dose of K+ transfused in the extracellular fluid is tiny. An infant weighing 1.0 kg, given a
15 mL/kg transfusion of packed RBCs (hematocrit 80%), receives 3 mL of extracellular fluid that
contains only 0.15 mEq of K+, and it will be transfused slowly. However, the safety of stored RBCs
may not apply to large-volume (>25 mL/kg) transfusions infused rapidly, in which greater doses of K+
may be harmful.
For children weighing >30-40 kg who are to undergo surgery, autologous RBC transfusions may be
another alternative to donor allogeneic RBCs. Preoperative autologous blood collections from the
patient occur up to 6 wk before the surgery and require careful considerations for the volume to be
drawn, vascular access, use of EPO and iron to help restore the donated RBCs, and so on. Acute
normovolemic hemodilution occurs in the preoperative period, in which blood is withdrawn from the
patient and replaced with saline, a task often difficult in centers without experience in the process.
Salvaged autologous blood is collected from blood loss during the operation but is impractical
unless the volume of blood salvaged is fairly large to permit washing and transfusion of a significant
number of RBCs.
Bibliography
Bell EF, Strauss RG, Widness JA, et al: Randomized trial of liberal versus restrictive guidelines for red
blood cell transfusion in preterm infants. Pediatrics 2005; 115:1685-1691.
Centers for Disease Control and Prevention : HIV transmission through transfusion—Missouri and
Colorado, 2008. MMWR 2010; 59(41):1335-1338.
Eder AF, Hillyer CD, Dy BA, et al: Adverse reactions to allogeneic whole blood donation by 16- and
17-year olds. JAMA 2008; 299:2279-2286.
Guay J, de Moerloose P, Lasne D: Minimizing perioperative blood loss and transfusions in
children. Can J Anaesth 2006; 53:559-567.
Hebert PC, McDonald BJ, Tinmouth A: Clinical consequences of anemia and red cell transfusion in the
critically ill. Crit Care Clin 2004; 20:225-235.
Kirpalani H, Whyte RK, Andersen C, et al: The premature infants in need of transfusion (PINT) study:
a randomized, controlled trial of a restrictive (low) versus liberal (high) transfusion threshold for
extremely low birth weight infants. J Pediatr 2006; 149:301-307.
Kuehn BM: CDC launches surveillance system to improve blood transfusion
safety. JAMA 2010; 303:1467.
Lacroix J, Hébert PC, Hutchison JS, et al: Transfusion strategies for patients in pediatric intensive care
units. N Engl J Med 2007; 356:1609-1619.
The Lancet: Improving blood safety worldwide : Lancet 2007; 370:361.
Lee JS, Gladwin MT: The risks of red cell storage. Nat Med 2010; 16:381-382.
Morley SL: Red blood cell transfusions in acute paediatrics. Arch Dis Child Educ Pract
Ed 2009; 94:65-73.
Ross SD, Allen IE, Henry DH, et al: Clinical benefits and risks associated with epoetin and darbepoetin
in patients with chemotherapy-induced anemia: a systematic review of the literature. Clin
Ther 2006; 28:801-831.
Stramer SL, Wend U, Candotti D, et al: Nucleic acid testing to detect HBV infection in blood donors. N
Engl J Med 2011; 364(3):234-247.
Strauss RG: Commentary: is it safe to limit allogeneic red blood cell transfusions to
neonates?. Neonatology 2008; 93:217-222.
Strauss RG: Controversies in the management of the anemia of prematurity using single-donor red
blood cell transfusion and/or recombinant human erythropoietin. Transfus Med Rev 2006; 20:34-44.
Strauss RG: How I transfuse red blood cells and platelets to infants. Transfusion 2008; 48:209-217.
Vamvakas EC, Strauss RG: Meta-analysis of controlled clinical trials studying the efficacy of
recombinant human erythropoietin in reducing blood transfusions in the anemia of
prematurity. Transfusion 2001; 41:406.
Copyright © 2011 Elsevier Inc. All rights reserved. Read our Terms and Conditions of Use and our Privacy Policy.
For problems or suggestions concerning this service, please contact: online.help@elsevier.com
Chapter 465 – Platelet Transfusions
Ronald G. Strauss
Guidelines for platelet (PLT) support of children and adolescents with quantitative and qualitative PLT
disorders are similar to those for adults (see
Table 465-1 on the Nelson Textbook of Pediatrics
website at www.expertconsult.com
), in whom the risk of life-threatening bleeding after injury or
occurring spontaneously can be related to the severity of thrombocytopenia. PLT transfusions should
be given to patients with PLT counts < 50 × 109/L when they are bleeding or are scheduled for an
invasive procedure, and the PLT count should be maintained > 50 × 109/L until bleeding ceases or the
patient is stable after the procedure.
Table 465-1 -- GUIDELINES FOR PEDIATRIC PLATELET (PLT) TRANSFUSION*
CHILDREN AND ADOLESCENTS
PLT count < 50 × 109/L and bleeding
PLT count < 50 × 109/L and an invasive procedure
PLT count < 20 × 109/L and marrow failure with hemorrhagic risk factors
PLT count < 10 × 109/L and marrow failure without hemorrhagic risk factors
PLT count at any level, but with PLT dysfunction plus bleeding or an invasive procedure
INFANTS ≤ 4 MO OLD
PLT count < 100 × 109/L and bleeding or during extracorporeal membrane oxygenation
PLT count < 50 × 109/L and an invasive procedure
PLT count < 20 × 109/L and clinically stable
PLT count < 50 × 109/L and clinically unstable
PLT count at any level, but with PLT dysfunction plus bleeding or an invasive procedure
* Words
in italics must be defined for local transfusion guidelines.
Studies of patients with thrombocytopenia resulting from bone marrow failure indicate that the risk of
spontaneous bleeding increases markedly when PLT levels fall to < 20 × 10 9/L, and hemorrhagic risk
factors (infection, organ failure, clotting abnormalities, mucosal lesions, severe graft versus host
disease, or anemia) are present. In this high-risk setting, prophylactic PLT transfusions are given to
maintain a PLT count > 20 × 109/L. This threshold has been challenged by studies of adult patients,
who in many instances were selected to be in relatively good clinical condition without hemorrhagic
risk factors. Consequently, a lower PLT transfusion trigger of 5-10 × 109/L is recommended for stable
(i.e., low-risk) patients. In practice, however, severe thrombocytopenia is commonly associated with
the development/occurrence of risk factors, including fever, antimicrobial therapy, active bleeding,
need for an invasive procedure, disseminated intravascular coagulation, and liver or kidney
dysfunction with clotting abnormalities. In these situations, PLT transfusions are given to maintain
relatively high PLT counts. Despite the desire by some physicians to elevate the blood PLT count to
80 × 109/L or 100 × 109/L or even higher, there are no definitive data to justify a true benefit of PLT
transfusions given at a PLT count > 50 × 109/L, unless bleeding is active with a PLT count between 50
and 100 × 109/L and thrombocytopenia seems to be the only cause.
Qualitative PLT disorders may be inherited or acquired (in advanced hepatic or renal insufficiency or
when blood flows through an extracorporeal circuit, such as during extracorporeal membrane
oxygenation [ECMO] or cardiopulmonary bypass). In patients with such disorders, PLT transfusions
are justified only if the risk of significant bleeding is quite high or actually occurs. Because inherited
PLT dysfunction often is lifelong and repeated transfusions may lead to alloimmunization and
refractoriness (i.e., poor response to PLT transfusions), prophylactic PLT transfusions are rarely
justified, unless an invasive procedure is planned. In these cases, an abnormal result with the use of a
modern PLT function device or, historically, a bleeding time more than twice the upper limit of
laboratory normal may be taken as diagnostic evidence of PLT dysfunction. However, an abnormal
bleeding time or any other abnormal laboratory test result is poorly predictive of hemorrhagic risk or
the need to transfuse PLTs. Alternative therapies, particularly desmopressin acetate, should be
considered to avoid PLT transfusions. Antiplatelet medications (nonsteroidal anti-inflammatory drugs)
should be avoided in these patients.
In neonates, hemostasis is quantitatively and qualitatively different from that in older children, and the
potential exists for either serious hemorrhage or thrombosis. Blood PLT counts ≥150 × 10 9/L are
present after 17 wk gestational age. Approximately 1% of term infants demonstrate PLT counts <150 ×
109/L, but bleeding in such infants is rare. In contrast, 25% preterm of neonates treated in intensive
care units exhibit blood PLT counts < 150 × 109/L at some time during admission, with about 4%
overall and 50% of those < 1.0 kg birth weight receiving PLT transfusions. Multiple pathogenetic
mechanisms underlying thrombocytopenia are involved in these sick neonates, predominantly
accelerated PLT destruction plus diminished PLT production, as evidenced by decreased numbers of
megakaryocyte progenitors and relatively low upregulation of thrombopoietin levels during
thrombocytopenia, compared with thrombocytopenic children and adults.
Blood PLT counts < 100 × 109/L pose significant clinical risks for premature neonates. Bleeding time
may be prolonged at PLT counts < 100 × 109/L in infants with birth weight < 1.5 kg; PLT dysfunction is
suggested by bleeding times that are disproportionately long for the degree of thrombocytopenia. The
risk of hemorrhage may be increased in thrombocytopenic infants. However, in a randomized trial,
transfusing PLTs prophylactically whenever the PLT count fell to < 150 × 109/L (i.e., below the lower
limit of normal) to maintain the average PLT count at > 200 × 109/L, in comparison with transfusing
PLTs only when the PLT count fell to < 50 × 109/L to maintain the average PLT count at approximately
100 × 109/L, did not result in a lower incidence of intracranial hemorrhage (28% vs. 26%, respectively).
Thus, there is no documented benefit to prophylactic transfusion of PLTs for modest thrombocytopenia
(PLT count > 50 × 109/L) to sustain a blood PLT count in the normal range. As an exception, infants
with inherited PLT dysfunction disorders and bleeding, and those at high risk of bleeding owing to
acquired PLT dysfunction, such as during ECMO, commonly receive transfusions to keep their PLT
counts > 100 × 109/L. Although basic questions about the relative risks of different degrees of
thrombocytopenia in various clinical settings are only partially answered, guidelines acceptable to
many neonatologists are listed in Table 465-1. For optimal PLT transfusion practices, each hospital
should develop guidelines that satisfy local practices and should attempt to avoid violations of the
practices.
The goal of most PLT transfusions is to raise the PLT count above 50 × 109/L and to increase that for
neonates to ≥ 100 × 109/L. These increases can be achieved consistently in children weighing up to
30 kg by infusion of 5 to 10 mL/kg of standard (unmodified) PLT concentrates, obtained either from
processing whole blood units or by plateletpheresis. For larger children, the appropriate dose is 3-4
pooled whole blood–derived PLT units or 1 apheresis unit. Because PLT concentration varies in
different PLT products made available for transfusion, each hospital should monitor post-transfusion
PLT counts and determine the dose that works best locally. PLT concentrates should be transfused as
rapidly as the patient's overall condition permits, certainly within 2 hr. Patients requiring repeated PLT
transfusions should receive leukocyte-reduced blood products, including PLT concentrates, to diminish
alloimmunization and PLT refractoriness and to reduce the risk of transfusion-transmitted
cytomegalovirus infection.
Routinely reducing the volume of PLT concentrates for infants and small children by additional
centrifugation steps is both unnecessary and unwise. Transfusion of 10 mL/kg of an unmodified PLT
concentrate is adequate because it adds 10 × 109 PLTs to 70 mL of blood (the blood volume of a 1-kg
neonate), a number calculated (taking the usual hematocrit and post-transfusion PLT recovery values
into account) to increase the PLT count by 100 × 109/L. This calculated increment has been validated
because it is consistent with the actual increment reported. Moreover, 10 mL/kg is not an excessive
transfusion volume, provided that the intake of other IV fluids, medications, and nutrients is monitored
and adjusted. It is important to select PLT units for transfusion with the ABO group identical to that of
the recipient and to avoid repeated transfusion of group O PLTs to group A or B recipients, because
passive anti-A or anti-B in group O plasma can lead to hemolysis. Although proven methods exist to
reduce the volume of PLT concentrates when truly warranted (e.g., many transfusions are anticipated,
in which the quantity of passive anti-A or anti-B might lead to hemolysis, or failure of 10 mL/kg of
unmodified PLT concentrate to increase the PLT count), additional processing should be performed
with great care because of probable PLT loss, clumping, and dysfunction caused by the additional
handling, all of which could diminish the efficacy and increase the toxicity of PLT transfusions.
Bibliography
Chakravorty S, Murray N, Roberts I: Neonatal thrombocytopenia. Early Hum Dev 2005; 81:35-41.
Christensen RD, Paul DA, Sola-Visner MC, et al: Improving platelet transfusion practices in the
neonatal intensive care unit. Transfusion 2008; 48:2281-2284.
Josephson CD, Su LL, Christensen RD, et al: Platelet transfusion practices among neonatologists in
the United States and Canada: results of a survey. Pediatrics 2009; 123:278-285.
Murray NA: Evaluation and treatment of thrombocytopenia in the neonatal intensive care unit. Acta
Paediatr Suppl 2002; 91:74-81.
Strauss RG: Low-dose prophylactic platelet transfusions: time for further study, but too early for
routine clinical practice. Transfusion 2004; 44:1680-1682.
Copyright © 2011 Elsevier Inc. All rights reserved. Read our Terms and Conditions of Use and our Privacy Policy.
For problems or suggestions concerning this service, please contact: online.help@elsevier.com
Chapter 466 – Neutrophil (Granulocyte) Transfusions
Ronald G. Strauss
Guidelines for granulocyte transfusion (GTX) are listed in Table 466-1
on the Nelson Textbook
of Pediatrics website at www.expertconsult.com
. Although GTX has been used sparingly in the
past, the ability to collect markedly higher numbers of neutrophils from donors stimulated with
recombinant granulocyte colony-stimulating factor (G-CSF) plus dexamethasone has led to renewed
interest, particularly for recipients of hematopoietic progenitor cell transplantation. GTX should be
reconsidered at institutions where neutropenic patients continue to die of progressive bacterial and
fungal infections or to suffer substantial morbidity despite the optimal use of antimicrobial agents (i.e.,
“antibiotics”) and recombinant myeloid growth factors.
Table 466-1 -- GUIDELINES FOR PEDIATRIC GRANULOCYTE TRANSFUSIONS*
CHILDREN AND ADOLESCENTS
Severe neutropenia (blood neutrophil count <0.5 × 109/L) and infection (bacterial, yeast, or
fungal) unresponsive or progressive despite appropriate antimicrobial therapy.
Qualitative neutrophil defect and infection (bacterial or fungal) unresponsive to appropriate
antimicrobial therapy
INFANTS ≤4 MO OLD
Blood neutrophil count <3.0 × 109/L in 1st wk of life or <1.0 × 109/L thereafter and fulminant bacterial
infection
* Words
in italics must be defined for local transfusion guidelines.
The role of GTX added to antibiotics for patients with severe neutropenia (blood neutrophil count <0.5
× 109/L) due to bone marrow failure is similar for adults and children. Infected neutropenic patients
usually show response to antibiotics alone, provided that bone marrow function recovers early during
the infection. Because children with newly diagnosed leukemia show rapid response to induction
chemotherapy, they are rarely candidates for GTX. In contrast, infected children with sustained bone
marrow failure (malignant neoplasms resistant to treatment, aplastic anemia, and hematopoietic
progenitor cell transplant recipients) may benefit when GTX is added to antibiotics. The efficacy of
GTX for bacterial sepsis unresponsive to antibiotics in patients with severe neutropenia (blood
neutrophil count <0.5 × 109/L) is supported by many controlled studies, whereas GTX's efficacy for
yeast and fungal infections remains unproven despite some encouraging reports.
Children with qualitative neutrophil defects (neutrophil dysfunction) usually have adequate numbers of
blood neutrophils but are susceptible to serious infections, because their cells kill pathogenic
microorganisms inefficiently. Neutrophil dysfunction syndromes are rare, and no definitive studies
have established the efficacy of GTX. However, several patients with progressive life-threatening
infections have shown striking improvement with the addition of GTX to antimicrobial therapy. These
disorders are chronic, and because of the risk of inducing alloimmunization, GTX is recommended
only when serious infections are clearly unresponsive to antimicrobial drugs.
Neonates are unusually susceptible to severe bacterial infections, and a number of defects of neonatal
body defenses may be contributing factors. These abnormalities are accentuated in sick premature
neonates, and it is logical to consider GTX. Neonates exhibiting fulminant sepsis, relative neutropenia
(blood neutrophil count < 3.0 × 109/L during the 1st wk of life and < 1.0 × 109/L thereafter), and a
severely diminished neutrophil marrow storage pool (with < 10% of nucleated marrow cells postmitotic
neutrophils) are at particularly great risk of dying if treated only with antibiotics. Although some studies
have shown a significant benefit from GTX, it is rarely used today because it is difficult to obtain in a
timely fashion. Instead, some neonatologists consider alternative therapies, including IV
immunoglobulin and recombinant myeloid growth factors (G-CSF or granulocyte-macrophage colonystimulating factor [GM-CSF]). Results of studies evaluating IV immunoglobulin have been mixed, but a
meta-analysis found significant benefit for neonates with proven sepsis. Current data are insufficient to
determine whether recombinant myeloid growth factors have a role in treating these neonates, despite
the fact that both G-CSF and GM-CSF have been demonstrated to enhance myelopoiesis and raise
neutrophil counts in infants. Importantly, G-CSF is efficacious for the long-term treatment of several
types of severe congenital neutropenia.
Once the decision to provide GTX has been made, an adequate dose of fresh leukapheresis cells
must be transfused. Neonates and infants weighing < 10 kg should receive 1-2 × 109/kg neutrophils
per GTX. Larger infants and children should receive a total dose of at least 1 × 1010 neutrophils per
GTX; the preferred dose for adolescents is 5-8 × 1010 per GTX, a dose requiring donors to be
stimulated with G-CSF plus dexamethasone. GTX should be given daily until either the infection
resolves or the blood neutrophil count is sustained above 1.0 × 109/L for a few days.
Bibliography
Price TH: Granulocyte transfusion therapy. J Clin Apheresis 2006; 21:65-71.
Strauss RG: Neutrophil collection and transfusion. In: Simon TL, Snyder EL, Solheim BG, et
al ed. Rossi's principles of transfusion medicine, ed 4. Bethesda, MD: AABB & Blackwell Publishing
Ltd; 2009:219-227.
Copyright © 2011 Elsevier Inc. All rights reserved. Read our Terms and Conditions of Use and our Privacy Policy.
For problems or suggestions concerning this service, please contact: online.help@elsevier.com
Chapter 467 – Plasma Transfusions
Ronald G. Strauss
Guidelines for plasma transfusion in children (see Table 467-1
on the Nelson Textbook of
Pediatrics website at www.expertconsult.com
) are similar to those for adults. Plasma is transfused
to replace clinically significant deficiencies of plasma proteins (nearly always clotting proteins) for
which more highly purified concentrates are not available. Two interchangeable plasma products are
available for transfusion, plasma frozen within 8 hr of collection (fresh frozen plasma) and plasma
frozen within 24 hr of collection. Although levels of factors V and VIII are lower in the latter plasma
product, they are equally efficacious for literally all indications for plasma transfusions (see Table 4671). Requirements for plasma vary with the specific protein being replaced, but a starting dose of
15 mL/kg is usually satisfactory.
Table 467-1 -- GUIDELINES FOR PEDIATRIC PLASMA TRANSFUSIONS*
INFANTS, CHILDREN, AND ADOLESCENTS
Severe clotting factor deficiency AND bleeding
Severe clotting factor deficiency and an invasive procedure
Emergency reversal of warfarin effects
Dilutional coagulopathy and bleeding (e.g., massive transfusion)
Anticoagulant protein (antithrombin III, proteins C and S) replacement
Plasma exchange replacement fluid for thrombotic thrombocytopenic purpura or for disorders in
which there is risk of bleeding due to clotting protein abnormalities (e.g., liver failure)
* Words
in italics must be defined for local transfusion guidelines.
Transfusion of plasma is efficacious for the treatment of deficiencies of clotting factors II, V, X, and XI.
Deficiencies of factor XIII and fibrinogen are treated with cryoprecipitate. Transfusion of plasma is not
recommended for the treatment of patients with severe hemophilia A or B, von Willebrand disease, or
factor VII deficiency, because safer factor VII, VIII, and IX concentrates are available. Moreover, mild
to moderate hemophilia A and certain types of von Willebrand disease can be treated with
desmopressin (Chapter 471). An important use of plasma is for rapid reversal of the effects of warfarin
in patients who are actively bleeding or who require emergency surgery (in whom functional
deficiencies of factors II, VII, IX, and X cannot be rapidly reversed by vitamin K). Results of screening
coagulation tests (prothrombin, activated partial thromboplastin, and thrombin times) should not be
assumed by themselves to reflect the integrity of the coagulation system or regarded as indications for
plasma transfusions. To justify plasma transfusion, coagulation test results must be related to the
patient's clinical condition. Transfusion of plasma in patients with chronic liver disease and prolonged
clotting times is not recommended unless bleeding is present or an invasive procedure is planned,
because correction of the clotting factor deficiencies is brief.
Plasma also contains several anticoagulant proteins (antithrombin III, protein C, and protein S) whose
deficiencies have been associated with thrombosis. In selected situations, plasma may be appropriate
as replacement therapy, along with anticoagulant treatment, in patients with these disorders. However,
when available, purified concentrates are preferred. Other indications for plasma include replacement
fluid during plasma exchange in patients with thrombotic thrombocytopenic purpura (i.e., thrombotic
microangiopathies) or other disorders for which plasma is likely to be beneficial (plasma exchange in a
patient with bleeding and severe coagulopathy). Plasma is not indicated for correction of hypovolemia
or as immunoglobulin replacement therapy, because safer alternatives exist (albumin or crystalloid
solutions and IV immunoglobulin, respectively).
In neonates, plasma transfusion merits special consideration. Clotting times are “physiologically”
prolonged owing to developmental deficiency of clotting proteins, and plasma should be transfused
only after reference to normal values adjusted for the birthweight and age of the infant (i.e., not to
normal ranges for older children and adults). The indications for plasma in neonates include: (1)
reconstitution of red blood cell (RBC) concentrates to simulate whole blood for use in massive
transfusions (exchange transfusion or cardiovascular surgery); (2) hemorrhage secondary to vitamin K
deficiency; (3) disseminated intravascular coagulation with bleeding; and (4) bleeding in congenital
coagulation factor deficiency when more specific treatment is either unavailable or inappropriate. The
use of prophylactic plasma transfusion to prevent intraventricular hemorrhage in premature infants is
not recommended, as efficacy has not been proven. Plasma should not be used as a suspending
agent to adjust the hematocrit values of RBC concentrates before small-volume RBC transfusions to
neonates because it offers no apparent medical benefit over the use of sterile solutions such as
crystalloid and albumin. Similarly, the use of plasma in partial exchange transfusion for the treatment
of neonatal hyperviscosity syndrome is unnecessary, because safer crystalloid or colloid solutions
(e.g., albumin) are available.
In the treatment of bleeding infants, cryoprecipitate is often considered because of its small infusion
volume. However, cryoprecipitate contains significant quantities of only fibrinogen, von Willebrand
factor, and factors VIII and XIII. Thus, it is not effective for treating the usual clinical situation in
bleeding infants with multiple clotting factor deficiencies, despite the appeal and convenience of a
small infusion volume. In preliminary studies, infusions of very small volumes of recombinant activated
factor VII have been lifesaving in patients with hemorrhage due to several mechanisms. Because the
efficacy and toxicity of factor VIIa have not been fully defined in these “off-label” (not approved by the
U.S. Food and Drug Administration) uses, it must be considered experimental therapy at this time.
Bibliography
Felderhoff-Mueser U, Buhrer C: Clinical measures to preserve cerebral integrity in preterm
infants. Early Hum Dev 2005; 81:237-244.
Goldenberg NA, Manco-Johnson MJ: Pediatric hemostasis and use of plasma components. Best Pract
Res Clin Haematol 2006; 19:143-155.
O'Shaughnessy DF, Atterbury C, Bolton Maggs P, et al: Guidelines for the use of fresh-frozen plasma,
cryoprecipitate and cryosupernatant. Br J Haematol 2004; 126:11-28.
Stanworth SJ, Brunskill SJ, Hyde CJ, et al: Is fresh frozen plasma clinically effective? A systematic
review of randomized controlled trials. Br J Haematol 2004; 126:139-152.
Copyright © 2011 Elsevier Inc. All rights reserved. Read our Terms and Conditions of Use and our Privacy Policy.
For problems or suggestions concerning this service, please contact: online.help@elsevier.com
Chapter 468 – Risks of Blood Transfusions
Ronald G. Strauss
The greatest risk of a blood transfusion is receiving a transfusion intended for another patient. This risk
is particularly high for infants, because identification bands may not be attached to their bodies,
difficulties in drawing pretransfusion compatibility testing blood sample may lead to deviations in usual
policies, and infants cannot speak to identify themselves. Thus, particular care must be taken to
ensure accurate patient and blood sample identification.
Although the risks of allogeneic blood transfusions are low, transfusions must be given judiciously.
Taking nucleic acid amplification testing (NAT) and all other donor-screening activities (antibody and
epidemiology screening) into account, a current estimate of the risk of transfusion-associated HIV is
approximately one per every 2,000,000 donor exposures. Similarly, with NAT, the risk of viral hepatitis
C is one per every 1,500,000 to 2,000,000 donor exposures (Table 468-1). NAT identifies circulating
viral material in the window period before antibodies develop and is used to detect HIV, hepatitis C,
and West Nile virus. NAT is also available for hepatitis B, but its use for this purpose is variable and
controversial.
Table 468-1 -- ESTIMATED RISKS IN TRANSFUSION PER UNIT TRANSFUSED IN THE USA
ESTIMATED RISK
Febrile reaction
1/300
Urticaria or other cutaneous reaction
1/50-100
Red blood cell alloimmunization
1/100
Mistranfusion
1/14,000-19,000
Hemolytic reaction
1/6,000
Fatal hemolysis
1/1,000,000
Transfusion-associated lung injury
1/5,000
HIV1 and HIV2
1/2,000,000-3,000,000
Hepatitis B
1/100,000-200,000
Hepatitis C
1/1,000,000-2,000,000
Human T-cell lymphotrophic virus (HTLV) I and II 1/641,000
Bacterial contamination
1/5,000,000
Malaria
1/4,000,000
Anaphylaxis
1/20,000-50,000
Graft versus host disease
Uncommon
Immunomodulation
Unknown
From Klein HG, Spahn DR, Carson JL: Red blood cell transfusion in clinical practice, Lancet 370:415–
426, 2007.
Transfusion-associated cytomegalovirus (CMV) can be nearly eliminated by transfusion of leukocyte
reduced cellular blood products or by selection of blood from donors who are seronegative for
antibody to cytomegalovirus. Although it is logical to hypothesize that first collecting blood components
from CMV-seronegative donors and then removing the white blood cells (WBCs) might improve safety,
no data are available to document the efficacy of this combined approach. Moreover, findings from
one study suggest that this combined approach, surprisingly, may be incorrect. Large quantities of
CMV are present “free” in the plasma of healthy-appearing donors during primary infection (while CMV
antibodies are either still absent or are newly emerging), rather than being leukocyte associated as
they are during latent infection, when substantial quantities of antibodies are present. Thus, virus will
not be removed by leukocyte reduction, and donors will be misclassified as CMV seronegative
because antibody is below the limits of detection in window-phase or early infection. Because nearly
all plasma CMV disappears after donors are seropositive for CMV antibody for several months and the
virus is almost exclusively leukocyte associated at this time, the best method to reduce CMV risk may
be to effectively perform leukocyte reduction of blood from donors known to be CMV seropositive for at
least 1 year.
Additional infectious risks include other types of hepatitis (A, B, E) and retroviruses
(human T-cell lymphotropic virus types I and II and HIV-2), syphilis, parvovirus B19,
Epstein-Barr virus, human herpesvirus 8, West Nile virus, yellow fever vaccine virus,
malaria, babesiosis, Anaplasma phagocytophilum, and Chagas disease. Variant
Creutzfeldt-Jacob disease has also been transmitted by blood transfusions in humans.
Transfusion-associated risks of a noninfectious nature that may occur include hemolytic and
nonhemolytic transfusion reactions, fluid overload, graft versus host disease, electrolyte and acid-base
imbalances, iron overload if repeated transfusions are needed long term, increased susceptibility to
oxidant damage, exposure to plasticizers, hemolysis with T-antigen activation of red blood cells, posttransfusion purpura, acute lung injury, immunosuppression, and alloimmunization (see Table 468-1).
Immunomodulation may be reduced by leukocyte reduction. Transfusion reactions and
alloimmunization to red blood cell and leukocyte antigens seem to be uncommon in infants. Adverse
effects are seen primarily in massive transfusion settings, such as exchange transfusions and trauma
or surgery, in which relatively large quantities of blood are needed, but are rare with the small-volume
transfusions usually given.
Premature infants are known to have immune dysfunction, but their relative risk of post-transfusion
graft versus host disease is controversial. The postnatal age of the infant, the number of
immunocompetent lymphocytes in the transfusion product, the degree of human leukocyte antigen
compatibility between donor and recipient, and other poorly described phenomena determine which
infants are truly at risk for graft versus host disease. Regardless, many centers caring for preterm
infants transfuse exclusively γ-irradiated cellular products. Directed donations with blood drawn from
blood relatives must always be irradiated because of the risk of engraftment with transfused HLAhomozygous, haploidentical lymphocytes. Cellular blood products given as intrauterine and exchange
transfusions should be γ-irradiated, as are transfusions for patients with severe congenital
immunodeficiency disorders (severe combined immunodeficiency syndrome and DiGeorge syndrome
requiring heart surgery) and transfusions for recipients of hematopoietic progenitor cell transplants.
Other groups who are potentially at risk but for whom no conclusive data are available include patients
given T-cell antibody therapy (antithymocyte globulin or OKT3), those with organ allografts, those
receiving immunosuppressive drug regimens, and those infected with HIV.
Current practice uses γ-irradiation from a cesium, cobalt, or linear acceleration source at doses
ranging from 2,500 to 5,000 cGy; a minimum dose of 2,500 cGy is required. All cellular blood
components should be irradiated, but frozen “acellular” products, such as plasma and cryoprecipitate,
do not require it. Leukocyte reduction cannot be substituted for γ-irradiation to prevent graft versus
host disease.
Bibliography
Alter HJ, Kein HG: The hazards of blood transfusion in historical perspective. Blood 2008; 112:26172626.
Centers for Disease Control and Prevention : Anaplasma phagocytophilum transmitted through blood
transfusion—Minnesota, 2007. MMWR Morbid Mortal Wkly Rep 2008; 57:1145-1148.
Centers for Disease Control and Prevention : Transfusion-related transmission of yellow fever vaccine
virus—California, 2009. MMWR Morbid Mortal Wkly Rep 2010; 59:34-36.
Centers for Disease Control and Prevention : West Nile virus transmission via organ transplantation
and blood transfusion—Louisiana, 2008. MMWR Morbid Mortal Wkly Rep 2009; 58:1263-1266.
Centers for Disease Control and Prevention : Blood donor screening for Chagas disease—United
States, 2006–2007. MMWR Morbid Mortal Wkly Rep 2007; 56:141-143.
Hladik W, Dollard SC, Mermin J, et al: Transmission of human herpesvirus 8 by blood transfusion. N
Engl J Med 2006; 355:1331-1338.
Klein HG, Spahn DR, Carson JL: Red blood cell transfusion in clinical practice. Lancet 2007; 370:415426.
Strauss RG: Data-driven blood banking practices for neonatal RBC
transfusions. Transfusion 2000; 40:1528-1540.
Zieman M, Krueger S, Maier AB, et al: High prevalence of cytomegalovirus DNA in plasma samples of
blood donors in connection with seroconversion. Transfusion 2007; 47:1972-1983.(plus Editorial,
pages 1955–1958)
Copyright © 2011 Elsevier Inc. All rights reserved. Read our Terms and Conditions of Use and our Privacy Policy.
For problems or suggestions concerning this service, please contact: online.help@elsevier.com