(PRN) Medication
advertisement

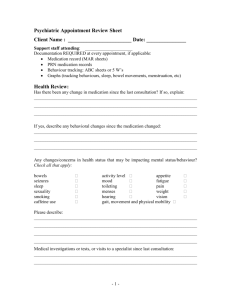
Medicines Policy for Care Staff trained and competent to administer medicines Title: Procedure for administration of PRN or ‘as required ’medication Date Review date Purpose of this document This procedure for the administration of when required (PRN) medication is to provide consistency of treatment for the service user. Competencies required To successfully complete the medicines training and update sessions To complete the competencies and to be able to demonstrate the required skills and knowledge to ensure safe practice. To adhere to the standards specified in this Policy People covered All service users. Procedure: Administration of When Required (PRN) Medication Medication with a ‘when required’ dose (PRN) is usually prescribed to treat short term or intermittent medical conditions i.e. it is not to be taken regularly. Medicines used to treat nausea or vomiting following a specific treatment regime as an example, are often taken by people who are experiencing symptoms irregularly. In such circumstances the person may not need the tablets every day. To ensure the medication is given as intended a specific plan for administration must be recorded in the care plan and ideally kept with the MAR charts. Information on why the medication has been prescribed and Page 1 of 7 how to give it should be sought from the prescriber, the supplying pharmacist or other healthcare professionals involved in the treatment of the person. Consideration should be given to the person’s capacity to refuse the medication. When providing staff with information the needs of the person must be identified e.g. if signs of pain are expressed in a non-verbal way. A record does not have to be made at each medicine round to show the person has been offered the medication. However the care plan should demonstrate that staff know what the medication is for and have made an assessment on whether the person requires the medication. PRN medication should not be offered or given only at the times listed on the MAR chart or at specific medication rounds. As it is for occasional use the person should be offered the medication at the times they are experiencing the symptoms either by telling a member of staff or by staff identifying the person’s need as outlined in the care plan. The exact time the medication was given and the amount given should be recorded on the MAR. If PRN medication is given regularly then a referral to the prescriber should be considered for a review of the person’s medication, as their medical condition may have changed and the treatment required may need altering. Similarly if the medication is not having the expected effects the prescriber should be contacted. In both cases the response to the medication should be clearly recorded. PRN medication that is still in use and in date should be carried over from one month to the next and not disposed of. A record of the quantity carried over should be recorded on the new MAR so there is an accurate record of the quantity in stock and to help when performing audits. PRN medication is best supplied in an original box rather than a monitored dosage system (MDS). This allows for a check on the expiry date and reduces waste. PRN or ‘when required’ medicines must be given in accordance with the prescribers instructions, details of which should be recorded on the Care Plan and on the MAR chart. If the instructions are not clear, clarification Page 2 of 7 needs to be sought from the prescriber and a PRN Medication Instructions Form completed. This form will detail the maximum dosage in 24 hours, how often the dose can be repeated and details of how and when the medication should be given.The form should be signed by the prescriber and by the person requesting the clarification or receiving the information. This procedure should be adopted for any service users prescribed “when required” (PRN) medication which does not contain clear directions. The Care Manager should ensure completion of form Information from the Prescriber – PRN Instructions by the prescriber whenever clarification is needed. If the form Information from the Prescriber – PRN Instructions has not been completed, the care worker will be unable to administer the drug. The Care Manager must obtain full information. If necessary, further information and advice should be sought from the prescriber. This includes medication prescribed by a hospital prescriber. The form Information from the Prescriber – PRN Instructions must be made available to the care worker and placed in the Residents Records next to the MAR. The care worker must consult the form Information from the Prescriber – PRN Instructions before administration of the medication. Immediately after witnessing the administration of medication, the care worker must document the dose, time and reason for administration e.g. pain or constipation on the MAR. Page 3 of 7 Standards: Written Information is available for staff to know how to administer the medication Staff know what the medication has been prescribed for Staff know when to give the medication or ask the person if they need it. Staff know what symptoms to look out for A written record makes clear the maximum amount to be given in a day or the time to leave between doses Staff offer the medication at times other than the usual medication rounds Relevant records are clearly made on the MAR chart The medication policy and procedure cover the administration of PRN medication Care plans provide detailed information on medication prescribed as ‘when required’ Staff understand what the medication is for If PRN medication is given regularly there are regular reviews taking place PRN medication is offered at times to meet the needs of the person There are accurate records of administration made PRN medications are held in suitable quantities and are in date Page 4 of 7 Information from the Prescriber – PRN Instructions PRN (WHEN REQUIRED) MEDICATION INSTRUCTIONS Name of Service User: DOB: Address: Medication Dose Reason for Medication Dosage Criteria E.g. Give 1 if……………. Give 2 if……………. How often dose can be repeated Page 5 of 7 Max in 24 hours Further info. e.g. after food Review Date Circumstances for reporting to GP Tick as appropriate Persistent need for upper level of dosage Never requesting dosage Requesting too often Side effects experienced Other (please state) Prescribers Signature: ………………………………….Date…………….. Person seeking clarification/receiving information Signature…………………………………… Date……………………….. Page 6 of 7 Page 7 of 7