Donor Medical History
advertisement
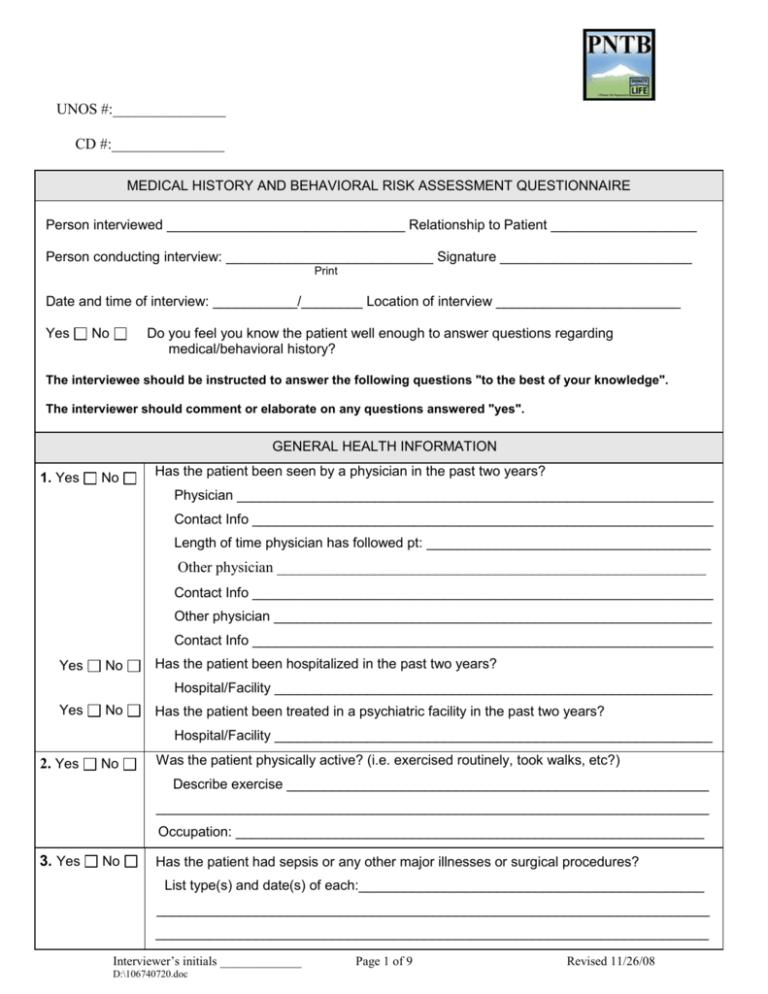
UNOS #:_______________ CD #:_______________ MEDICAL HISTORY AND BEHAVIORAL RISK ASSESSMENT QUESTIONNAIRE Person interviewed _______________________________ Relationship to Patient ___________________ Person conducting interview: ___________________________ Signature _________________________ Print Date and time of interview: ___________/________ Location of interview ________________________ Yes No Do you feel you know the patient well enough to answer questions regarding medical/behavioral history? The interviewee should be instructed to answer the following questions "to the best of your knowledge". The interviewer should comment or elaborate on any questions answered "yes". GENERAL HEALTH INFORMATION 1. Yes No Has the patient been seen by a physician in the past two years? Physician ______________________________________________________________ Contact Info ____________________________________________________________ Length of time physician has followed pt: _____________________________________ Other physician _________________________________________________________ Contact Info ____________________________________________________________ Other physician _________________________________________________________ Contact Info ____________________________________________________________ Yes No Has the patient been hospitalized in the past two years? Hospital/Facility _________________________________________________________ Yes No Has the patient been treated in a psychiatric facility in the past two years? Hospital/Facility _________________________________________________________ 2. Yes No Was the patient physically active? (i.e. exercised routinely, took walks, etc?) Describe exercise _______________________________________________________ ________________________________________________________________________ Occupation: _____________________________________________________________ 3. Yes No Has the patient had sepsis or any other major illnesses or surgical procedures? List type(s) and date(s) of each:_____________________________________________ ________________________________________________________________________ ________________________________________________________________________ Interviewer’s initials _____________ D:\106740720.doc Page 1 of 9 Revised 11/26/08 UNOS #:_______________ CD #:_______________ Has the patient taken any medications on a regular basis (include over-the-counter, and herbals)? Specify medications ______________________________________________________ 4. Yes No Yes No Was the patient compliant with medications? Yes No Was the patient allergic to any medications? _____________________________________ Yes No Did the patient have any other allergies (food, latex)? ______________________________ 5. Yes No Did the patient use tobacco products? _____________________________________________________________________ Type of tobacco products __________________________________________________ Packs per day __________________________________________________________ For how long ___________________________________________________________ If the patient stopped using tobacco products, approximate date ___________________ 6. Yes No Did the patient drink alcohol? Type _________________________________________________________________ Quantity ______________________________________________________________ How long _____________________________________________________________ If the patient stopped drinking alcohol, approximate date ________________________ 7. Yes No Did the patient ever use non-prescribed drugs or other substances? (e.g. cocaine, marijuana, methamphetamines, steroids, inhalants) Type ________________________________________________________________ How much ___________________________________________________________ How long ____________________________________________________________ Route of administration? ______________________________________ Last time used? ____________________________________________ 8. Yes No Was the patient ever exposed to toxic substances (e.g. lead, pesticides, or other)? List substances the patient was exposed to ___________________________________ If exposed, did this result in symptoms; if yes explain ____________________________ ____________________________________________________________________ Year and duration of exposure? ____________________________________________ Interviewer’s initials _____________ D:\106740720.doc Page 2 of 9 Revised 11/26/08 UNOS #:_______________ CD #:_______________ 9. Yes No In the past three years has the patient traveled outside of the United States (Including Canada)? Country – Name and Location (City/Region) _________________________________ Month and year of stay __________________ Length of stay ___________________ Purpose of trip ________________________________________________________ Yes No Was the patient born, lived in, or stayed in any other country (including military bases) other than United States for a cumulative period of time greater than 3 months? Explain _______________________________________________________________ Yes No Has the patient ever been diagnosed with Chagas disease? Explain _______________________________________________________________ Yes No Has the patient taken anti-malarial drugs, had malaria, or been in malarial endemic area within the last year? Explain: ______________________________________________________________ 10. Yes No Has the patient ever been diagnosed with, or treated for West Nile Virus? Explain ________________________________________________________________ Yes No Did the patient have a history of a fever with headache within the last 10 days? Explain: _______________________________________________________________ 11. Yes No Has the patient ever received blood transfusions or blood products prior to this admission? What type, where, and when ______________________________________________ Yes No Ever been a blood donor? Yes No Been refused as a blood donor or told not to donate? Reason _______________________________________________________________ 12. Yes No Did the patient ever receive a human or animal organ, tissue, or live cell transplant (i.e. bone, cornea, skin, heart, kidney, dura mater, etc.)? Type of transplant ___________________________________ Date ______________ Hospital/Facility ________________________________________________________ Yes No Did the patient ever have intimate contact * with a person or persons who received an organ or tissue transplant from a source of animal origin? Explain: _____________________________________________________________ *Intimate contact defined as sexual partner, shared razors/toothbrush, or laboratory/health care personnel with repeated mucosal/percutaneous exposure. 13. Yes No In the past 12 months did the patient have any of the following: tattoos, ear or body piercing, acupuncture, Botox injections or accidental needle stick? Explain: _________________________________________________________________ If yes, answer the following: Were the instruments used in the procedures listed above shared? ______________ Was it performed professionally? _________________________________________ Explain accidental needle stick injury: _____________________________________ Interviewer’s initials _____________ D:\106740720.doc Page 3 of 9 Revised 11/26/08 UNOS #:_______________ CD #:_______________ 14. Yes No In the past 12 months, was the patient bitten by any animal? Explain (evaluate for suspected rabies): _____________________________________ ________________________________________________________________________ 15. Yes No In the past 12 months, was the patient vaccinated (including flu shots, tetanus) or immunized for any reason? Explain: ______________________________________________________________ Date and reason _______________________________________________________ Yes No Was the patient vaccinated for Hepatitis? Reason: _______________________________ 16. Yes No In the past months has the patient received the smallpox vaccination, or had close contact with the vaccination site of anyone else? Explain: Yes No _____________________________________________________________ Did the patient have any illnesses or complications due to the vaccine? Explain _____________________________________________________________ 17. Yes No Was the patient ever given human derived pituitary growth hormone? Explain: __________________________________________________________ Date of treatment:______________________ 18. Yes No Did the patient have any history of heart disease, chest pain, poor circulation (especially in the legs), or leg ulcers? Explain: ______________________________________________________________ Yes No High blood pressure? Duration ___________________________________________________________ Specify medications __________________________________________________ Yes No Yes NA No Was the patient compliant with medications? Family history of CAD? Explain: ______________________________________________________________ 19. Yes No Did the patient have any type of liver disease? _________________________________ Yes No Been told of having any type of hepatitis? Explain: ______________________________ Yes No Had a positive test for hepatitis? Explain:______________________________________ Yes No Have any history of yellow jaundice? Explain: __________________________________ Yes No Did the patient have any close contact with persons diagnosed with viral hepatitis in the past 12 months? Explain the nature of the contact (i.e. shared razor, toothbrush, sexual contact) : _____________________________________________________________________ Interviewer’s initials _____________ D:\106740720.doc Page 4 of 9 Revised 11/26/08 UNOS #:_______________ CD #:_______________ 20. Yes No Yes No Did the patient have a history of kidney related diseases, kidney stones, frequent urine infections or kidney infections? Explain: ____________________________________________________________ Ever been treated with kidney dialysis? Date ____________ Type ___________________ How long __________________ Hospital/Facility ______________________________________________________ 21. Yes No Yes No Did the patient have a history of digestive or intestinal problems, bloody stools, persistent diarrhea, intestinal surgery, or intestinal cancer? Explain: ____________________________________________________________ Recent weight loss? Explain how much? and reason? ________________________________________ Current height _____________________ Current weight __________________________ 22. Yes No Did the patient have a history of diabetes? If yes, please answer the following: Age at diagnosis ____________________________________________________ Did the patient require medication? ______________________________________ Specify __________________________________________________________ Duration of treatment _______________________________________________ Was the patient compliant with medication? _______________________________ Yes No NA Was the patient diagnosed with gestational diabetes? Explain: ________________________________________________________ 23. Yes No Did the patient have any history of lung disease, asthma, emphysema? Explain: ________________________________________________________________ Yes No Treatment required? Specify ______________________________________________________________ Yes No Yes No Did the patient ever receive a TB test? Was the TB test positive for tuberculosis? If yes, describe follow-up/treatment:_______________________________________ ____________________________________________________________________ 24. Yes No Has the patient ever had cancer (including lymphoma, leukemia, melanoma, tumor) or positive biopsies? Specify medications and other treatments:__________________________________ ____________________________________________________________________ If yes, specify number of years cancer-free _________________________________ Interviewer’s initials _____________ D:\106740720.doc Page 5 of 9 Revised 11/26/08 UNOS #:_______________ CD #:_______________ 25. Yes No Does the patient have any history of autoimmune or chronic degenerative disease, such as: Multiple sclerosis, scleroderma, amyotrophic lateral sclerosis (ALS), rheumatoid arthritis, polyarteritis nodosa, systemic lupus erythematosis, sarcoidosis, or metabolic bone disease? Approximate onset and treatment of any above disease/diagnosis: ________________ _____________________________________________________________________ 26. Yes No Did the patient suffer from any type of neurologic or brain disease such as: Alzheimer's, Parkinson’s, seizures, gait changes, sudden unexplained anxiety or personality changes, visual changes, hallucinations, periods of confusion or recent memory loss, dementia, history of brain tumor, polio or degenerative neurological disease, encephalitis, or meningitis? Explain: __________________________________________________________ Yes No Does the patient or family member have a history of Creutzfeldt-Jakob Disease (CJD) or a risk of developing CJD? Explain ___________________________________________________________ 27. Yes No Did the patient have any history of: Bone or joint disease, arthritis, history of broken bones, bone tumor, complaints of stiff or sore joints? Explain: ____________________________________________________________ 28. Yes No Did the potential donor have a history of skin infections such as leprosy, eczema, dermatitis, inflammatory skin diseases, or abrasions? Explain ______________________________________________________________ Yes No Does the patient have a current skin problem? Explain: _____________________________________________________________ HIGH RISK BEHAVIOR QUESTIONS 29. Yes No Has the patient received human derived clotting factor concentrates for hemophilia or related clotting disorders? Explain ______________________________________________________________ Interviewer’s initials _____________ D:\106740720.doc Page 6 of 9 Revised 11/26/08 UNOS #:_______________ CD #:_______________ 30. Has the patient recently exhibited or experienced any: Yes No Unexplained weakness? Yes No Fatigue or flu-like symptoms such as night sweats, persistent cough, shortness of breath, colds, or swollen lymph nodes for greater than one month? Yes No Nausea, vomiting, persistent diarrhea? Yes No Fever > 100.5 F for greater than 10 days? Yes No White spots in mouth? Yes No Blue or purple spots on the skin or mucus membranes? Explain: ___________________________________________________________ Yes No Has the patient experienced any periods of explained or unexplained weight loss? Explain _____________________________________________________________ 31. Yes No In the past 12 months has the patient had or been treated for any sexually transmitted disease (i.e. gonorrhea, syphilis, genital herpes, chlamydia)? Explain: ______________________________________________________________ Medications __________________________________________________________ 32. Yes No Has the patient ever been tested for HIV? Result and reason for the test: ____________________________________________ 33. Yes No In the past five years has the patient used a needle to inject drugs into his/her veins, muscle, or under his/her skin for non-medical use? Explain: ________________________________________________________________ 34. Yes No NA Male Donors: Has the patient had sex with another male in the past 5 years? Yes No NA Female Donors: Has the patient had sex within the last year with a male who has had sex with another male in the past 5 years? 35. Yes No Explain ________________________________________________________________ Has the patient engaged in sex in exchange for money or drugs in the past 5 years? Explain ______________________________________________________________ 36. Yes No Was the patient exposed to, known or suspected, viral hepatitis or HIV infected blood through accidental needle stick or through contact with an open wound, non-intact skin, or mucous membrane in the past 12 months? Explain ______________________________________________________________ 37. Yes No Was the patient an inmate of a correctional system or jail, or released from a correctional system or jail, in the past 12 months? Date _________________________ Duration ______________________________ Name of facility _______________________________________________________ Reason for incarceration ________________________________________________ Interviewer’s initials _____________ D:\106740720.doc Page 7 of 9 Revised 11/26/08 UNOS #:_______________ CD #:_______________ 38. Yes No Has the patient had sex in the past 12 months with any person known, or suspected to have viral hepatitis or HIV infection? Explain _____________________________________________________________ 39. Yes No Has the patient ever had sex with any person described in the above questions # 29-39 in the past twelve months? Explain _____________________________________________________________ NA Only complete if patient has a history of Intravenous Drug Use 40. Frequency of injection of IV drugs? Explain: ____________________________________________________________ Duration of time that the patient used IV drugs? Explain: ____________________________________________________________ Last time the patient used IV drugs? Explain: ____________________________________________________________ Yes No Did the patient share needles? Explain: ____________________________________________________________ Please provide information to verify clean needle use. Explain: ____________________________________________________________ Yes No History of skin abscess, cellulitis, or general sepsis? Explain: ____________________________________________________________ Yes No Did the patient participate in a Methadone or detox program? When and for how long? ________________________________________________ PEDIATRIC DONORS 41. Yes No Is the child 18 months of age or less? 42. Yes No NA If under 5 years of age, breast fed within the past 12 months? If “yes” for question #41 or 42 a Medical History and Behavioral Risk Assessment questionnaire must be completed by the mother to determine if the child is at risk for transmission of HIV or viral hepatitis infection. Interviewer’s initials _____________ D:\106740720.doc Page 8 of 9 Revised 11/26/08 UNOS #:_______________ CD #:_______________ NA 43. Yes EYE DONORS No Did the patient have a history of any diseases, infections, or surgeries involving the eyes? Please list ____________________________________________________________ Yes No Did the patient have a history of: Glaucoma, cataracts, corneal disease, laser surgery, retinoblastoma, lens implant Explain: _______________________________________________________________ If yes to above, please obtain Eye physician and contact information: ________________ _______________________________________________________________________ 44. Yes No ALL DONORS Having answered questions about medical conditions and behavioral risk factors, do you now have any questions or concerns that would make you think organ or tissue donation should not proceed? Please explain your concerns: _______________________________________________________________________ _______________________________________________________________________ Yes No Are there other individuals that may give additional information regarding medical/behavioral questions? Name __________________________________________________________________ Contact Info _____________________________________________________________ COMMENTS Interviewer’s initials _____________ D:\106740720.doc Page 9 of 9 Revised 11/26/08