Appendix 5 - QA Standards for Colonoscopy in England
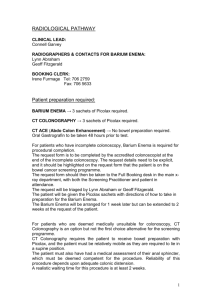
advertisement

Criteria for Screening Colonoscopy Centres Recommendations to the Bowel Cancer Screening Project Board 20th January 2009 1 Contents Purpose ............................................................................................................................................. 3 Background ....................................................................................................................................... 3 Summary of the Proposed Process for Northern Ireland............................................................... 4 Proposals for 3 Main Quality Areas ................................................................................................. 5 Introduction ..................................................................................................................................... 5 Endoscopy Unit Global Rating Scale (GRS) .................................................................................... 6 GRS Description and Associated Issues...................................................................................... 6 GRS Standard to be achieved ..................................................................................................... 6 Waiting Times ................................................................................................................................. 7 Waiting Times - Description and Associated Issues ..................................................................... 7 Waiting Times Standard to be achieved ....................................................................................... 8 Decontamination and Equipment..................................................................................................... 9 Decontamination & Equipment - Description and Associated Issues ........................................... 9 Decontamination & Equipment Standards to be achieved............................................................ 9 Proposed Criteria for Screening Colonoscopy Centres .............................................................. 10 Monitoring Progress Toward Meeting Criteria.............................................................................. 12 Appendix 1 - Selection Criteria for Screening Colonoscopy Centres in England ...................... 14 Appendix 2 - Selection Criteria for Bowel Cancer Screening Centres in Wales ......................... 15 Appendix 3 - GRS Measures .......................................................................................................... 17 Appendix 4 - Screening Colonoscopy Centre Tasks in England................................................. 18 Appendix 5 - QA Standards for Colonoscopy in England............................................................ 20 Appendix 6 - QA Standards for Colonoscopy in Scotland........................................................... 21 Appendix 7 - QA Standards for Colonoscopy in Wales ............................................................... 24 2 PURPOSE This paper has been prepared by the Modernising Endoscopy Services Project Team for the Bowel Cancer Screening Project Board. It makes recommendations about the criteria that endoscopy units should meet in order to perform screening colonoscopies. It is envisaged that ultimately all endoscopy units will meet these criteria. It is important to note the distinction between quality criteria that an endoscopy unit must meet before it can provide screening colonoscopies, and the quality standards that an endoscopy unit must meet after it has been selected to provide screening colonoscopies, as part of the wider quality assurance and performance management framework for the bowel cancer screening programme. This paper is concerned with the former. QA standards for screening colonoscopy in other parts of the UK are shown in appendices 5-7. Similar standards for Northern Ireland’s Bowel Cancer Screening Programme will be developed by the Bowel Cancer Screening Project Quality Assurance Group and the Modernising Endoscopy Services Project Team. These are not included in this document. B ACKGROUND Different approaches to the identification of screening colonoscopy centres have been taken in different parts of the UK. These are briefly outlined here to provide some background to this paper. The Bowel Cancer Screening Programme in England has set criteria that an endoscopy unit must meet before it can provide screening colonoscopies (included in Appendix 1). The criteria are measured by the Joint Advisory Group on Gastrointestinal Endoscopy (JAG) which then approves the unit as a screening colonoscopy centre. Approved units receive funds to support the provision of the screening colonoscopy service. In England, after an endoscopy unit has been selected to provide screening colonoscopies it must meet agreed quality standards in the provision of its screening colonoscopy services. These are shown in Appendix 5. Wales has developed criteria that endoscopy units must meet before providing screening colonoscopies; these are set out in Appendix 2. It has also defined QA standards for the programme which are shown in Appendix 7. The Scottish Bowel Screening Programme did not set criteria that had to be met before an endoscopy unit could provide screening colonoscopies. Scottish Health boards hold responsibility for the provision of screening colonoscopies and each Health Board was provided with a planning tool to help them predict the demand for screening colonoscopy arising from their screening programme each year. Scotland has developed quality standards as part of the wider QA framework for its screening programme; these include standards for pre-colonoscopy assessment, colonoscopy and histopathology. These are shown in Appendix 6. 3 SUMMARY OF THE PROPOSED PROCESS FOR NORTHERN IRELAND In line with practice in other areas of the UK, it is proposed that the Bowel Cancer Screening Project Board for Northern Ireland sets criteria that endoscopy units must meet before they can provide screening colonoscopies. This is the first step toward ensuring that this aspect of the screening programme is developed and managed to explicit quality standards, in line with best practice guidance on collaborative commissioning of screening programmes1. Proposed criteria for Northern Ireland are outlined later in this report, which pays special attention to three major areas, two of which (2&3 below) present a risk to achieving the target of having a Bowel Cancer Screening Programme in place by the end of December 2009: 1. GRS, 2. Waiting times, 3. Decontamination and equipment. Agreed criteria will be used to inform the commissioning of screening colonoscopy centres in Northern Ireland. It is anticipated that Trusts will be invited to indicate their intention to become a screening colonoscopy centre in late early February 2009, and submit associated documents / plans based on the agreed criteria by mid March 2009. The location of potential screening centres and associated secondary care services will be confirmed by commissioners late March / early April 2009. Progress of each potential screening colonoscopy centre and identified associated secondary care services toward meeting the agreed criteria and readiness for the introduction of screening will be monitored as follows: 1. Screening Colonoscopy Centres: The NICaN Modernising Endoscopy Services Project will facilitate a ‘Pre JAG Visit’ to each potential screening colonoscopy centre, focusing on how well it currently meets agreed criteria set out in this document and GRS quality standards, and what actions are required to meet them fully. This will take place in April / May 2009. It will be followed up by a ‘JAG Visit’ in September 2009, to check that the centre has met all the criteria and standards. If it does, it will be approved by commissioners to provide screening colonoscopies. 2. Associated secondary care services: The DHSSPS Service Delivery Unit, via the Modernising Endoscopy Services Project, will monitor progress of associated secondary care services (Pathology, Radiology, Surgery and Oncology) toward readiness for the implementation of bowel cancer screening. The Bowel Cancer Screening Project will develop additional quality standards against which screening colonoscopy and pathology services will be monitored when the screening programme begins. These will form just one part of the wider quality assurance and performance management framework for the bowel cancer screening programme. Department of Health, England ‘Collaborative Commissioning of National Screening Programmes; best practice guidance, Dec 2007 http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_081509 1 4 PROPOSALS FOR 3 M AIN QUALITY AREAS Introduction Ensuring that endoscopy units are providing a high quality, patient focused service before they can provide screening colonoscopies gives assurance that people who are referred for screening colonoscopy will receive a high quality, patient focused service. There are a range of quality measures and tools currently available to help decide whether an endoscopy unit is currently providing a high quality, patient focused service. This section of the report looks at three major quality measures and is therefore divided into three parts. 1. Endoscopy Unit Global Rating Scale (GRS) 2. Waiting Times 3. Decontamination and equipment (It should be noted that numbers 2 and 3 present a risk to achieving the target of having a Bowel Cancer Screening Programme in place by the end of December 2009.) Each of these parts describes the quality measure and associated issues, and outlines a standard to be achieved. In addition to the proposals on the three areas above, additional criteria based on those used in England, Scotland and Wales have been developed. These are shown on page 10 of this document. 5 Endoscopy Unit Global Rating Scale (GRS) GRS Description and Associated Issues All endoscopy units in Northern Ireland now use the Endoscopy Unit Global Rating Scale (GRS). This is a recognised self assessment audit tool developed through a partnership led by the National Endoscopy Team in England. It is now used in all NHS endoscopy units in the UK. GRS uses a number of quality measures to compare quality and performance between units. These measures fall into 4 Domains: 1. 2. 3. 4. Clinical Quality Patient Experience Training Workforce Within each domain there are a number of quality statements to which a yes/no answer is given. The quality statements dictate a score of A – D, with A being the highest quality and D indicating that improvements can be made to that aspect of the service. Appendix 3 shows all the broad quality measures that GRS includes. More detail can be seen on http://ni.globalratingscale.com/ A baseline for the GRS scores for all endoscopy units in Northern Ireland (NICaN August 2008) indicates that the majority of units are scoring level D in most items; however there are also a few C, B and A scores. It was anticipated that this would be the case, as was the experience in other parts of the UK, however it does not take long for units to improve their scores in most areas. The appointment of a Nurse Lead for Endoscopy will help units work together to raise the scores across the region. GRS Standard to be achieved In line with England, endoscopy units that wish to provide screening colonoscopy must achieve GRS level A in timeliness and B in all other GRS measures. 6 Waiting Times Waiting Times - Description and Associated Issues Fast access to screening colonoscopy for those who require it is a prerequisite of any screening programme. In England, endoscopy units must score GRS level A in timeliness; this means that routine patients are seen within six weeks and urgent patients within two weeks of referral. In Northern Ireland, the standard for diagnostic tests is 9 weeks for out patients and 13 weeks for day cases by March 20092. Bowel Cancer Screening Patients will be managed as day cases, of which colonoscopy pre-assessment is a part, so the generic standard of 13 weeks by March 2009 and in line with DHSSPS standards on waiting times thereafter applies. Waiting times are an important part of the criteria for the identification of units wishing to become bowel cancer screening centres; rapid access to screening colonoscopy is essential for those with a positive screening test. Other areas of the UK have prioritised this, for example Scotland’s Clinical Standards for Bowel Cancer Screening3 state that in Scotland: “The time between the receipt of a positive screening test result by the NHS Board and the offered appointment date for pre-colonoscopy assessment is within 14 days for at least 80% of individuals” And “In at least 95% of cases the interval between the notification of the positive screening test result to the NHS Board and the date offered for colonoscopy is no longer than 31 days” The Modernising Endoscopy Services Project Team believes in principal that it is desirable that Northern Ireland should not diverge significantly from the National standard of 6 weeks waiting time for routine symptomatic cases, and 2 weeks for urgent, as the criteria that screening colonoscopy centres should meet before providing screening colonoscopies. This is particularly important because the standards on waiting times for patients who are part of the Bowel Cancer Screening Programme (between receipt of a positive test and the date of colonoscopy) in England, Wales are 28 days and in Scotland 31 days. The risk attached to this strategy is that all endoscopy units in the region will fall short of meeting this target. The NICaN Modernising Endoscopy Services Leads have met with Trust endoscopy units to support them to increase their capacity as far as possible, however waiting times remain significantly longer than is desirable for the introduction of Bowel Cancer Screening. Waiting time reductions are currently being achieved through the provision of additional lists at weekends, with consultants working additional hours, or by sending patients to the Private Sector for their endoscopy. Feedback from the service indicates that these approaches to addressing waiting times are expensive, unsustainable, and focus energy and resource on ‘fire fighting’ rather than effective forward planning. It has been suggested by the Modernising Endoscopy Services Project Team that a period of consolidation is required to allow Trusts to forward-plan a more effective strategy to reduce colonoscopy waiting times over the longer term. While this may support long term planning and more effective service delivery in the symptomatic service, it would not address the matter of rapid access to screening colonoscopy for screening patients. Two possible strategies have been suggested to resolve the problem of waiting times in advance of the introduction of bowel cancer screening. The first is to put additional resource for staffing in to the larger endoscopy units (endoscopy nurses and medical and surgical endoscopists). The NICaN DHSSPS 2008 ‘Priorities for Action 2008/09 http://www.dhsspsni.gov.uk/prioritiesannualreport2008.pdf Clinical Standards Bowel Screening Programme, Quality Improvement Scotland, Feb 2007 http://www.bowelscreening.scot.nhs.uk/wpcontent/uploads/2007/06/bowelsc_stnf_feb07.pdf standard statement 5.a 2 3 7 Endoscopy Services Capacity Audit, carried out in 2007, highlighted the fact that Trusts are currently unable to accurately determine the demand for their service; this has made it difficult to provide an estimate of the numbers of additional staff required. The second is to provide the screening colonoscopy service in smaller endoscopy units, where demand is less. However, this is not a preferred option. Consultation with the Bowel Cancer Screening Project Team and Project Assurance Group has led to the proposal that a waiting time of 28 days for bowel cancer screening patients requiring colonoscopy should be implemented in Northern Ireland. The provision of dedicated funded lists to provide screening colonoscopy means that the introduction of bowel cancer screening should not adversely impact or jeopardise existing Trust plans to meet local waiting time standards of 13 weeks by March 2009 and DHSSPS standards on waiting times thereafter. The National Endoscopy Team have given their approval to this strategy and confirmed that it will not negatively influence the outcome of applications for JAG accreditation if endoscopy units have a clear timed plan in place to meet locally set standards on waiting times for colonoscopy4. Waiting Times Standard to be achieved The waiting time standard for the symptomatic service to meet in order to provide screening colonoscopies should be 13 weeks by March 2009 and in line with DHSSPS standards on waiting times therafter. Trusts must have a timed plan in place for their endoscopy units to meet these standards. The following waiting times should be adopted for bowel cancer screening patients in Northern Ireland: 14 days from confirmation of a positive FOBt result to colonoscopy pre-assessment; and 14 days from colonoscopy pre-assessment to colonoscopy. 4 Verbal confirmation obtained in a phone call to Ms Debbie Johnston, Operations Director, National Endoscopy Programme 8th January 2009. Ms Johnston coordinates the JAG visiting process for the JAG. 8 Decontamination and Equipment Decontamination & Equipment - Description and Associated Issues In England, many units that did not meet the JAG accreditation to become screening colonoscopy centres fell down in the area of decontamination5. High quality equipment is vital if stringent standards on decontamination are to be achieved. All endoscopy units should meet quality standards on decontamination and have equipment which is modern and fit for purpose, regardless of whether or not a screening service is provided. The DHSSPS Health Estates department is currently overseeing the improvement of Trust decontamination facilities. It anticipates that it is possible that not all endoscopy units will meet the standards it has set by the end of March 2009. Information about the equipment held by all 17 endoscopy units in the region has been collected by the NICaN Modernising Endoscopy Services Project as part of a regional audit of endoscopy services6. The audit found that 62% of the equipment in endoscopy units across the region is over 5 years old. The Belfast Trust held the greatest percentage of equipment over 5 years old, at 88%. The average life of an endoscope is between 7-8 years depending on use. All Trusts have received reports on this and have been made aware of the need to modernise their endoscopy equipment. Trusts are responsible for ensuring that their equipment meets standards. Decontamination & Equipment Standards to be achieved In line with work being undertaken by DHSSPS Health Estates, all endoscopy units (particularly those providing screening colonoscopy) must meet the standards on decontamination as outlined in the DHSSPS Health Estates guidance by the end of March 2009, and the JAG requirements on decontamination (2008) by September 2009. All endoscopy units should have a rolling equipment replacement programme in place. Those units that will provide screening colonoscopy should ensure that their endoscopes are less than 7 years old and still functioning effectively. 5 6 Roland Valori, National Clinical Lead for Endoscopy at national endoscopy event January 2008. NICaN, March 2008, Endoscopy Services Capacity Audit 9 PROPOSED CRITERIA FOR SCREENING COLONOSCOPY CENTRES This section of the report makes recommendations to the Bowel Cancer Screening Project Board on the criteria that screening colonoscopy centres in the region should meet. It is envisaged that in time all endoscopy units will meet these criteria, which have been developed based on those used in England and Wales (Appendices 1 and 2) and take into account the three issues discussed in the previous section. 1 Proposed Criteria Based on criteria from Global Rating Scale score of: Northern Ireland standards 2 A in Timeliness (that is, a symptomatic colonoscopy waiting time of 13 weeks by March 2009 and in line with DHSSPS standards on waiting times therafter) B in all other items. Be able to meet the screening programme IT requirements agreed by the Bowel Cancer Screening Project Board (to be specified early 2009) England 3 Ability to undertake and provide endoscopy unit audit data on Northern Ireland screening programme quality indicators for all colonoscopy performed in the unit, within which the screening patients will be identified, on a continuous basis to an identified QA office. England 4 Sufficient colonoscopists to provide timely colonoscopy for screen positive patients. The colonoscopists must meet agreed Northern Ireland approval criteria for colonoscopists, and plan to perform 120 colonoscopies per year per practitioner with at least one PA per week, rising to 150 per year within 2 years. England 5 Sufficient trained and competent: Specialist Screening Practitioners (staff to perform pre-assessment); England Adequate numbers of nursing staff (BSG guidelines i.e. 2 trained members of staff per room, one of whom is a qualified nurse) Wales Administrative staff to perform necessary administrative functions, reception and clerical duties England and Wales 6 Identification of a screening colonoscopy centre Lead, and professional leads for associated secondary care services as defined by the Bowel Cancer Screening Project Board. Each should have identified time within their job plans to perform this role. England 7 Ability to see all patients with a positive FOB test at an appointment with a specialist screening practitioner for colonoscopy pre-assessment within 14 days of receipt of notification to the screening colonoscopy centre that England / Wales / Scotland 10 the patient has had a positive FOB/screen result. 8 Ability to offer all patients with a positive FOB test an urgent colonoscopy appointment within 14 days of colonoscopy pre-assessment, since the suspicion of colorectal cancer is high. Wales / England 9 All patients should be seen on dedicated screening lists. - 10 Be able to begin providing screening colonoscopies from the end of December 2009. - 11 There should be a robust system in place for the referral of patients who are found to have cancer to the Trust Multi-disciplinary Team for Colorectal Cancer. Wales 12 Capacity within surgical, pathology, radiology and oncology services to absorb demand arising from bowel cancer screening. - 13 Complies with recommendations and standards for decontamination of equipment as outlined by DHSSPS Health Estates and meets JAG (2008) requirements on decontamination. - 14 Number of and type of scopes recommended by the BSG guidelines, and using endoscopes less than 7 years old which are still functioning effectively. Wales 15 Image capture facilities. Wales 16 Rolling equipment replacement plan. Wales 17 Be prepared to participate in a pre-JAG visit and JAG visit England 18 Be willing to release staff to attend meetings and training sessions as required by the needs of the screening programme Wales 11 MONITORING PROGRESS TOWARD MEETING CRITERIA Having established GRS in every endoscopy unit in Northern Ireland, the NICaN Modernising Endoscopy Services Project is using this as a basis to monitor progress in each unit toward GRS Scores of B in all items and A in timeliness. Each trust has been asked develop an initial Endoscopy Unit Modernising Endoscopy Services Action Plan for each of their endoscopy unit by the end of November 2008, based on GRS scores and including the actions needed to raise these scores to required standards. GRS ‘census’ will be undertaken as follows in Northern Ireland: Baseline – August 2008 (completed) End January 2009 End April 2009 End October 2009 End of April and October each year thereafter. In addition, the NICaN Modernising Endoscopy Services Project Leads have agreed a schedule of visits to each Trust to monitor progress and offer support where required as follows: November 2008 February 2009 May 2009 September 2009 November 2009 The Bowel Cancer Screening Project Board has recommended that progress toward current waiting time standards is discussed in these meetings, as well as being monitored via the regional SDU Cancer Services Steering Group Meeting. In addition, the Project Board has recommended that Trusts produce a rolling equipment replacement programme at these meetings, and discuss any associated actions. These recommendations have been formally communicated to Trusts by Mr. Hugh Mullen, Chair of the Bowel Cancer Screening Project Board in November 2008. When commissioners have decided on the location of screening colonoscopy centres, and in line with practice in England, it is proposed that the NICaN Modernising Endoscopy Services Project will arrange a ‘Pre JAG Visit’ to each potential screening colonoscopy centre. This will focus on how well the centre currently meets the proposed selection criteria, and what actions are required to ensure that they are met by the end of September 2009. This ‘Pre JAG visit’ will take place in April / May 2009. It will be followed up by a ‘JAG Visit’ in September 2009, to check that the centre has met all the required standards and is approved to provide screening colonoscopies. These Pre Jag and JAG visits will be conducted by a panel made up of an endoscopy Clinical, Training and Nurse Leads along with an external assessor from JAG as appropriate. The assessing panel will liaise with the Bowel Cancer Screening Project Board and Commissioners to feed back the outcomes of their visits. The DHSSPS Health Estates Department is currently responsible for monitoring Trust progress toward meeting its recommendations on decontamination by the end of March 2009. Compliance with the JAG standards on decontamination (2008) will be monitored through the Pre JAG and JAG visits. Trusts are responsible for ensuring that their equipment is modern and fit for purpose. 12 It is important that there is rapid access to treatment following diagnosis of colorectal cancers. Performance against the Northern Ireland Cancer Access Standards will provide an indication of whether units wishing to become screening centres are meeting the required access targets in advance of providing screening colonoscopies. Following England’s lead, it is proposed that screening patients are not included in cancer access standards at this point, but at a later date when the screening programme is well established. The introduction of bowel cancer screening will create additional demand not only on colonoscopy services, but on radiology, pathology, surgery and oncology services. The Modernising Endoscopy Services Project Team has been tasked with supporting capacity planning in identified screening colonoscopy centres for associated secondary care services. Ms Beth Malloy of the Service Delivery Unit at SDU will take forward this work, which will include monitoring Trust progress toward readiness to meet increased service demand arising from bowel cancer screening. 13 APPENDIX 1 - SELECTION CRITERIA FOR SCREENING COLONOSCOPY CENTRES IN ENGLAND This is taken from the document ‘NHS Bowel Cancer Screening Programme Wave 2: 2007/08 Advice to the NHS’ sourced from www.grs.nhs.uk Selection Criteria 1. Global rating scale score with particular emphasis on symptomatic waiting times and patient experience. 2. A satisfactory peer-review visit conducted under the auspices of the JAG. 3. Have an IT system able to meet national requirements and download data to national screening database OR ability to enter data directly and promptly onto national database via a web link. 4. Ability to undertake and provide endoscopy unit audit data on key quality indicators for all colonoscopy performed in the unit, within which the screening patients will be identified, on a continuous basis to the programme hub screening QA office. 5. Sufficient colonoscopists to provide timely colonoscopy for screen positive patients. The colonoscopists must be accredited and plan to perform 150 colonoscopies per year per practitioner with at least one PA per week*. 6. Sufficient trained and competent specialist screening practitioners and administrative staff to perform necessary functions. 7. Identification of a centre director and professional leads with identified time. 8. Ability to see all patients with a positive FOB test an appointment with a specialist screening practitioner within 10 days of the date of the result letter. 9. Ability to offer all patients with a positive FOB test an urgent appointment colonoscopy within two weeks of their appointment with the specialist screening practitioner since the suspicion of colorectal cancer is high. 10. At least 70% of patients should be seen on segmented lists. Segmentation in this context refers to patients on segmented lists having similar clinical characteristics and follow-up needs (in this case patients referred with a positive FOB test), i.e. at least 70% of patients will be seen on special lists for FOBt positive patients. 11. Estimated/preferred start date. 14 APPENDIX 2 - SELECTION CRITERIA FOR BOWEL CANCER SCREENING CENTRES IN W ALES Information courtesy of Dr Hilary Fielder, Bowel Screening Wales. Essential Desirable Service requirements Departmental multi disciplinary meetings as recommended by CSCG Complies with BSW assessment model for screening colonoscopists Adequate number of staff – (BSG guidelines i.e. 2 trained members of staff per room, one of whom is a qualified nurse) Appropriate grades of staff Relevant competencies achieved by nursing and HCA staff Dedicated reception and clerical staff Funding, IT support and routine replacement for local IT infrastructure including endoscopy system, network, hardware (PCs, printers, scanners, etc), and locally provided software (e.g. PAS, office software) Service and individual activity audit Able to provide specific audit data e.g. unplanned admissions, mortality and bleeding incidents Supportive radiology and pathology service Key performance indicators as prescribed by BSW Image capture System for monitoring and reviewing unpredicted incidents and near misses Environmental Based in an acute hospital with cardiac arrest team on site Complies with BSG Standard for decontamination of equipment and participates in all Wales audit Separate preparation area Sufficient room for increase in capacity Good decorative order Access to acute surgical opinion Adequate storage space Private rooms for discussion / admission/ SSP phone calls Separate waiting and recovery areas More than 1 colonoscopy room Facilities for trolley and seated recovery areas Equipment Number of scopes recommended by the BSG guidelines Modern video endoscopes <8 years old Image capture facilities Suitable networked IT infrastructure providing access to wide-area network (for links to Bowel Screening Video facilities 15 Information System, pathology system, etc), access to endoscopy system for direct data entry after examinations, with sufficient PCs, printers, scanners, etc, provided by and replaced by the local site Appropriate computerised endoscopy record system with interface and/or data exports for screening information (to be defined by Bowel Screening Wales) and funded software maintenance Dedicated resuscitation trolley and appropriately trained staff Piped oxygen to colonoscopy rooms and recovery rooms Equipment of monitoring blood pressure, ECG, pulse oximetry and ECG monitoring for high risk patients Equipment for cessation of bleeding and tattooing of polyps Capital asset replacement plan Training Offer access to and agree to attend BSW training programme Multidisciplinary training programme Trainees supervised for the required minimum number of cases All staff assessed as competent are able to practice Agree to attend a screening course relating to screening Identify medical and nursing leads and nominate facilitators/ mentors Willingness to release staff for meetings and training sessions Provision and updating of basic IT training (e.g. Windows, IT security, office software, etc), and endoscopy system use and data entry Sustainable delivery plan for training programme Work force development plans e.g. nurse colonoscopists Further Considerations: Geography Convenience for participants e.g. access, parking 16 APPENDIX 3 - GRS MEASURES Clinical Quality Consent process including patient information Safety Comfort Quality of procedure Appropriateness Communicating results to referrer Patient Experience Equality of access and equity of provision Timeliness Booking and choice Privacy and dignity Aftercare Ability to provide feedback to the service Workforce Skill mix review and recruitment Orientation and training Assessment and appraisal Staff are cared for Staff are listened to Training Environment and training opportunity Endoscopy trainers Assessment / Appraisal Equipment and educational materials 17 APPENDIX 4 - SCREENING COLONOSCOPY CENTRE TASKS IN ENGLAND Screening Colonoscopy Centres in England typically serve a population of between 500,000 and 2 million. They are the local face of the Bowel Cancer Screening Programme; they act as the local management point for the programme and provide nurse clinics and colonoscopy follow-up of FOBt positive individuals. They also act as the major source of information for the local health community. In England they are expected to take an active role in leading the promotion of the new services to the general public. Advice from NHS Cancer Screening to Strategic Health Authorities in England is that these services should be planned around a single clinical team. Screening Colonoscopy Centres in England provide: Specialist screening practitioner clinics offering colonoscopy pre-assessment (includes discussion about risks, fitness for colonoscopy, management of offer of colonoscopy and further investigations for cancers of the colon or rectum until discharge from programme); Colonoscopy clinics for screening participants with an abnormal FOBt result or who are scheduled for polyp surveillance; Referral for appropriate follow-up or treatment Information about the screening programme for the local health community; Information and support for local people in completing the FOBt (on referral from the programme hub); and Promotion of screening programme to the general public in their locality. Specific tasks for screening centres7 1. Set up clinics (both specialist screening practitioner and endoscopy). 2. Communication directly with patients regarding appointments and colonoscopy results. 3. Deal with telephone queries (bowel history and endoscopy). 4. Education of and liaison with local primary care and public health. 5. Coordination of/liaison with local health promotion activities to improve access to screening by all sections of society. 6. Liaison with programme hub including communication of results in a timely manner. 7. Monitor work flow and liaise with programme hub in order to adjust invitations, referrals where necessary. 8. Liaison with patients’ GPs. 9. Provide written confirmation of results of colonoscopy to the patient and their GP within one week of the examination. 10. Offer an appointment to discuss the results within two weeks for patients with high risk polyps or cancer. Continued… 7 NHS Screening programme wave 2 2007/08 advice to the NHS, Annex C, p15 https://www.bcsp.nhs.uk/DOCUMENTS/NHSBCSP-ADVICE-TO-NHS-JANUARY-07_1.pdf 18 11. Referral of individual patients for investigation and treatment according to local preagreed patterns (including barium enema and management of incidental findings). 12. Liaison with MDTs and treatment services including pathology to ensure appropriate follow up of results and facilitate audit. 13. Liaison with QA activity at programme hub. 14. Coordination of sites in which the team operate. 15. Monitoring and data collection including of treatment and histology outcomes and of adverse events. 16. Specialist screening practitioner clinic/endoscopy DNA follow up. 17. Transferring data/information to the programme hub. 19 APPENDIX 5 - QA STANDARDS FOR COLONOSCOPY IN ENGLAND Investigation after positive guaiac FOBt: Age 60 – 69 prevalent round Objective Measure Minimum Standard 1. Investigate individuals with positive FOB test results Acceptance rate of colonoscopy after positive FOBt > 85% undergo colonoscopy 2. Entire colon examined Completion rate with photographic evidence of Ileo-caecal valve/appendix orifice (unadjusted) > 90% completion 3. Identification of adenoma/cancer present in the population (i) Adenoma detection rate > 6 per 1000 screened Prevalent Screening Round (ii) Cancer detection rate Prevalent Screening Round >35 per 100 colonoscopies >2 per 1000 screened > 11 per 100 colonoscopies 4. Availability of polyps for pathological examination Polyp recovery >90% polyps excised 5. Planning of surgery (i) Identification of tumour position in correct segment of colon (ii) Tattooing of suspected malignant polyps (i) Minimum number of screening colonoscopies undertaken per year with full audit data of all standards listed >95% cancers (ii) Perforation rate <1:1000 colonoscopies (iii) Post polypectomy bleeding requiring transfusion <1:100 colonoscopies (iv) Post polypectomy perforation rate <1:500 colonoscopies 6. Minimising harms to the population (v) Rate of serious colonoscopic complications requiring unplanned admission 100% >150 <3 per 1000 colonoscopies 20 APPENDIX 6 - QA STANDARDS FOR COLONOSCOPY IN SCOTLAND Standard 5 Pre-colonoscopy assessment Standard Statement 5a The interval between receiving a positive screening test result and assessment for colonoscopy can result in significant anxiety. Essential Criteria Desirable Criteria 5a.1 The time between the receipt of a positive screening test result by the NHS board and the offered appointment date for pre-colonoscopy assessment is within 14 days for at least 80% of individuals. 5a.3 The time between the receipt of a positive screening test result by the NHS board and the offered appointment date for precolonoscopy assessment and offer them a further opportunity to do so. 5a.2 There are arrangements to identify all individuals who do not participate in precolonoscopy assessment and offer them a further opportunity to do so. Standard 5 Pre-colonoscopy assessment (continued) Standard Statement 5b Individuals with a positive screening test result are offered precolonoscopy assessment and are given an explanation of why, how and when colonoscopy is undertaken. Essential Criteria Desirable Criteria 5b.1 All individuals with a positive screening test result are offered a precolonoscopy assessment and a full explanation of the process of colonoscopy, the possible risks and the possible outcomes. The opportunity to discuss any concerns is provided at this stage and written information is also given. 5b.6 At least 95% of individuals who undergo pre-colonoscopy assessment and are deemed fit for 5b.2 Pre-colonoscopy assessment is carried out by a healthcare professional who has appropriate skills, knowledge and experience and follows national guidance in identifying those who would be at a higher risk than normal by undergoing colonoscopy. colonoscopy are offered a date at time of assessment. 5b.3 Clear and appropriate patient pathways are followed for individuals with a positive screening test result who do not proceed to colonoscopy. 5b.4 GPs are informed of all individuals with a positive screening test result who do not proceed to colonoscopy. 5b.5 At least 80% of individuals who undergo pre colonoscopy assessment and are deemed fit for colonoscopy are offered a date at the time of assessment. 21 Standard 6 Colonoscopy and histopathology Standard Statement 6a The time between notification of a positive screening test result and the performance of colonoscopy is minimized. Essential Criteria Desirable Criteria 6a.1 In at least 95% of cases, the interval between Type them here notification of the positive screening test result to the NHS board and the date offered for colonoscopy is within 31 days. 6a.2 In at least 95% of cases, GPs are notified of the results of colonoscopy within seven days. Standard 6 Colonoscopy and histhopathology (continued) Standard Statement 6b Colonoscopy is preformed to an appropriate standard. Essential Criteria Desirable Criteria 6b.1 Colonoscopy is carried out by a Colonoscopist who has demonstrated at least 90% colonoscopy completion in continuous audit and has undergone a Joint Advisory Group (JAG) approved course. 6b.4 Colonoscopy is carried out by a Colonoscopist who has undertaken screening colonoscopy accreditation. 6b.2 Screening colonoscopy is undertaken in a unit participating in the Global Rating Scale (GRS) 6b.3 There is a system to provide individuals undergoing colonoscopy with an indication of the findings, options and next steps (where appropriate) before being discharged. Continued… 22 Standard 6 Standard Statement 6c A completion of the entire large bowel is carried out after incomplete colonoscopy. Essential Criteria Desirable Criteria 6c.1 A date for a barium enema or a computed tomography (CT) colonography is offered within 31 days of an incomplete colonoscopy. 6c.5 The barium enema or CT colonography is offered on the same day as the incomplete colonoscopy, with the exception of when a polypectomy has been preformed. In this case, a barium enema or a CT colonography is not carried out within two weeks of the incomplete colonoscopy. 6c.2 The barium enema is preformed and reported by a suitably trained consultant radiologist and radiographer. 6c.3 CT colonography is preformed by a suitably trained radiologist or a radiographer and reported by a consultant radiologist. 6c.4 The reports for at least 80% of radiological examinations are authorized within seven days of the date of the examination. Standard 6 Standard Statement 6d Histopathology is carried out to an appropriate standard. Essential Criteria Desirable Criteria 6d.1 Histopathology reports include a clear indication of the main diagnosis, in accordance with the histhopathology information required by ISD. 6d.4 The histhopathology laboratory holds accreditation from the Clinical Pathology Accreditation (UK) Ltd to ISO 15189 standards. 6d.2 Histopathology reporting is in accordance with the guidelines of the Royal College of Pathologists (RCPath) and Scottish Intercollegiate Guidelines Network (SIGN) relating to colorectal pathology, if applicable to the specimen type being reported. 6d.3 The reports for at least 80% of the specimens submitted from the colonoscopy are authorized with in seven days of receipt of the specimen by the histhopathology laboratory. 23 APPENDIX 7 - QA STANDARDS FOR COLONOSCOPY IN W ALES 4.7 Specialist Screening Practitioner Assessment 4.7.1 Standard The interval between receiving a positive faecal occult blood test (FOBt) result and Specialist Screening Practitioner assessment is minimised. The time interval between a participant contacting the screening programme following a positive result and the first offered assessment appointment is within 14 calendar days for at least 95% of individuals. Rationale There is evidence that the time interval between receiving a positive result and assessment can result in significant anxiety. Essential Criteria 4.7.1a There are arrangements to identify all individuals who do not respond to positive letters and offer a further appointment. 4.7.1b Individuals with a positive result are asked to contact a central appointments telephone line. They are offered an appointment for Specialist Screening Practitioner telephone assessment at a time and location convenient to participants. 4.7.1c The first available appointment and chosen appointment must be documented for audit purposes. 4.7.1d If telephone assessment is not acceptable or appropriate to the participant a clinic appointment must be arranged to see the Specialist Screening Practitioner. 4.7.2 Standard Individuals with a positive result are offered assessment by a Specialist Screening Practitioner. They are given appropriate information, and an explanation of why, how and when colonoscopy or other investigations could be undertaken. Rationale There is evidence that providing information about tests, preparation and investigations reduces anxiety and encourages participation. Essential Criteria 4.7.2a All individuals with a positive FOBt result are offered an assessment, a full explanation of the process of colonoscopy, the possible risks and the possible outcomes are given. The opportunity to discuss any concerns is provided at this stage. 24 4.7.2b Assessment is carried out by a Specialist Screening Practitioner with appropriate skills and knowledge using an all Wales pro-forma. 4.7.2c The Specialist Screening Practitioner must have undertaken a training programme specified by Bowel Screening Wales. 4.7.2d Clear and appropriate pathways are followed for individuals with a positive FOBt result who do not proceed for colonoscopy. 4.7.2e 100% of participants deemed fit and who consent to colonoscopy are offered a date for the procedure at the assessment appointment. 4.7.2f Written information on colonoscopy and bowel preparation will be sent or given to participants who have been deemed fit and have accepted the offer of colonoscopy. 4.7.2g Bowel preparation medication will be prescribed and distributed according to local protocol. 4.7.2h Information on colonoscopy or other appropriate tests will be available in other formats. 4.7.3 Standard The time between notification of a positive faecal occult blood test (FOBt) and colonoscopy is minimised. In at least 95% of cases, the interval between the Specialist Screening Practitioner (SSP) assessment appointment and the first date offered for colonoscopy is within 14 calendar days. Rationale There is evidence that waiting for colonoscopy creates anxiety. Essential Criteria 4.7.3a The first available colonoscopy appointment will be offered to the participant. 4.7.3b A record of the first available appointment and the chosen appointment for colonoscopy must be captured on the Bowel Screening Information Management System. 4.7.3c Consent for colonoscopy must be captured using Bowel Screening Wales standardised postal consent form. continued 25 4.8 Colonoscopy 4.8.1 Standard The time between notification of a positive FOBt and colonoscopy is minimised. In at least 95% of cases, the interval between the notification of the positive screening result and the date offered for colonoscopy is within 28 days. Rationale There is evidence that waiting for colonoscopy creates anxiety. Essential Criteria 4.8.1a The first available colonoscopy appointment will be offered to the participant. 4.8.1b A record of the first available appointment and the chosen appointment for colonoscopy must be captured on the Bowel Screening Information Management System. 4.8.1c Consent for colonoscopy must be captured using BSW standardised postal consent form. 4.8.2 Standard Screening colonoscopy is only undertaken by senior colonoscopists who have been assessed and approved by Bowel Screening Wales. Rationale Colonoscopy can cause discomfort and complications and there is a small mortality associated with the procedure. Failure to complete colonoscopy, or incomplete visualization of the colonic mucosal surface may result in significant neoplasia being missed. Essential Criteria 4.8.2a Screening colonoscopists are expected to satisfy the following criteria prior to being accepted for assessment: • Minimum 120 colonoscopies performed or directly supervised per year; • Lifetime undertaking of more than 750 colonoscopies; • Lifetime perforation rate for diagnostic colonoscopy less than 1 in 1,000; • Pathology adjusted caecal intubation rate of at least 90% • Adenoma retrieval rate of at least 15% (as opposed to adenoma detection rate >20%). 4.8.2b Potential screening colonoscopists are assessed by BSW assessors using an approved model comprising of multiple choice questions, lesion recognition testing and a directly observed procedure skills assessment (DOPS). 26 4.8.2c Screening colonoscopists access annual update sessions provided by BSW. 4.8.2d Individual colonoscopists must submit colonoscopy reports and audit data as required by BSW. 4.8.2e Screening colonoscopists will be expected to undertake a minimum of 150 total colonoscopy procedures per annum, of which at least 50 should be screening colonoscopies. They must maintain experience undertaking screening colonoscopy as required by BSW and continue to satisfy all eligibility criteria for screening colonoscopists. 4.8.2f There is a system for collection of data on individual colonoscopists. 4.8.2g Screening colonoscopists participate in local and regional multidisciplinary education sessions and management meetings. 4.8.2h The Lead Screening Colonoscopist needs to be identified and is responsible for local Trust coordination of the screening programme. 4.8.3 Standard Colonoscopy is performed in an endoscopy unit that satisfies Bowel Screening Wales criteria for local assessment centres. Rationale Participants must receive an equitable high quality service across Wales. Essential Criteria 4.8.3a A local assessment centre screening plan is developed and maintained and a copy must be available in the screening unit. 4.8.3b All local assessment centres must comply with Bowel Screening Wales standards and protocols. 4.8.3c All local assessment centres must submit data requested by Bowel Screening Wales. 4.8.3d All local assessment centres must participate in Health Inspectorate Wales Audits if appropriate. 4.8.3e All local assessment centres are expected to participate in Joint Advisory Group (JAG) visits. 4.8.3f All local assessment centres will facilitate visits from Bowel Screening Wales when necessary and requested. 27 4.8.4 Standard If colonoscopy is incomplete further investigation is carried out to ensure the entire large bowel has been seen. Rationale Failure to complete colonoscopy may result in significant neoplasia being missed. Essential Criteria 4.8.4a Repeat colonoscopy should be considered if the initial procedure was limited by suboptimal bowel preparation. 4.8.4b Double contrast barium enema or CT colonography is offered depending on local protocol and participant suitability. 4.8.4c Whenever possible double contrast barium enema or CT colonography should be performed within 24 hours of the incomplete colonoscopy except when polypectomy has been undertaken. 4.8.4d A date for double contrast barium enema or CT colonography is given within 24 hours of the day of the incomplete colonoscopy. 4.8.4e Following incomplete colonoscopy further investigations will be undertaken within 31 days for 100% of participants. 4.8.4f Radiological investigations must be reported by named individuals who can demonstrate that they are appropriately trained. 4.8.4g Radiological reports will be sent to G.P s within 7 calendar days. 4.8.4h Participants will receive the results of all investigations within 7 calendar days of the final procedure. 4.8.4i A record of the first available appointment and the chosen appointment for further investigation must be captured on the Bowel Screening Information Management System. 28