Systemic sclerosis (SSc) can be categorized into two different
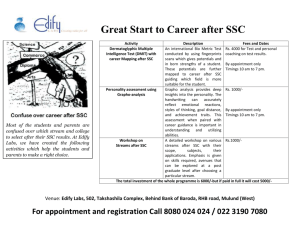
advertisement

Brian Kim Rheumatology Clerkship Systemic Sclerosis Systemic sclerosis (SSc) can be categorized into five different subsets depending on the extent of skin involvement (1). Limited cutaneous systemic sclerosis (lcSSc) is defined as skin thickening limited to the distal extremities with or without facial involvement. Most of these patients develop features of the CREST syndrome and generally carry a good prognosis (70% survival at 10 years). However, a subset of these patients can develop pulmonary hypertension independent of any changes in terms of pulmonary fibrosis. In contrast to lcSSc, diffuse cutaneous SSc (dcSSc) has a generally worse, albeit variable, prognosis (40-60% survival at 10 years) due to the involvement of visceral organs including the lungs, heart, kidney, and GI tract. In contrast to the pulmonary hypertension seen in lcSSc, dcSSc is associated with pulmonary fibrosis. Cardiopulmonary complications remain the leading cause of mortality in this disease. Overlap syndrome is another subset in which patients exhibit features of SSc in addition to features of other connective tissue diseases such as SLE, dermatomyositis, or rheumatoid arthritis. Some patients can exhibit features of SSc without any definite clinical or laboratory findings to make a diagnosis and are classified as having undefined connective-tissue disease. Finally, localized scleroderma is another subset in which patients can have linear scleroderma or morphea without any systemic involvement. Successful treatments for SSc have been difficult to identify and develop because of the variable course of the disease (spontaneous improvement frequently occurs), the inherent unresponsiveness of the disease to many interventions, and poorly designed studies in the past to evaluate possible therapies (1,2). Randomized controlled trials have not supported the efficacy of penicillamine, chlorambucil, ketanserin, interferon-, or or photopheresis (1). Currently there is no widely effective therapy reported for the treatment of SSc in terms of disease-modification. In this paper, potential new treatments will be discussed within the context of the current understanding of the pathogenesis of SSc, focusing on dcSSc. The pathogenesis of SSc is thought involve three different features: excessive collagen deposition, vascular damage, and uncontrolled inflammation (2). Although it remains unclear how these different pathways come together, each feature presents itself as a potential point of intervention. The presence of autoantibodies and inflammatory lesions in the skin and lung highly suggest that control of the inflammatory cascade can attenuate the progression of SSc. A recent randomized, controlled trial using oral cyclophosphamide demonstrated a modest benefit in terms of lung function, skin thickening, and quality of life (3). Recent randomized controlled trials using methotrexate are demonstrating some benefit in terms of skin score and overall well-being (3). One trial using cyclosporine demonstrated some benefit in SSc patients but also with significant adverse effects on blood pressure and renal function (4). A recent case study using mycophenolate mofetil as a first-line agent reported significant improvement in five patients (5). However, such studies would have to be expanded to larger controlled trials to establish efficacy. Overall, general immunosuppressive therapies are showing very modest success. TGF-, a cytokine involved in modulating proliferation and inflammation, has emerged as a potential key player in the induction of fibrosis. Its effects are thought to be mediated primarily through fibroblasts and their production of extracellular matrix proteins. Currently, monoclonal antibody antagonists are in development to target this pathway. Interestingly, losartan, an angiotensin II type 1 receptor antagonist has demonstrated antagonism of TGF- in animal models, most strikingly in a mouse model of Marfan Syndrome (5). Given the desirable effect of lowering blood pressure and the well-established benefit of using ACE inhibitors for renal crisis associated with SSc, a clinical trial using losartan would be interesting to see if it clinically attenuates the fibrosis associated with SSc. Treatments targeting fibrosis using Bosentan and interferon- have proven equivocal with regard to disease modification. Bosentan is used for idiopathic pulmonary hypertension to block pulmonary vasoconstriction. The lack of interferon- in mice has been shown to contribute to fibrosis (1). Another potential target to reduce excessive collagen deposition is the platelet-derived growth factor receptor (PDGFR). A recent study demonstrated that patients with SSc harbor serum autoantibodies that can stimulate PDGFR. They demonstrated that this stimulatory activity can induce the production of type I collagen and -smooth-muscle actin, thereby recapitulating the phenotype seen in scleroderma fibroblasts (6). PDGFR has already been implicated as a mediator of converting smooth muscle cells to myofibroblasts resulting in endothelial damage. Thus, developing antagonistic antibodies to block the activity of PDGFR shows great promise as a potential therapeutic in limiting both vascular damage and fibrosis. Treatments that target the vascular pathology of SSc include epoprostenol, treprostinil, and iloprost which can supply prostacyclin to the pulmonary vascular endothelium (1). In addition to bosentan, sildenafil has also been used for vascular dilatation. These agents have shown to improve functionality and quality of life but a clear improvement in terms of mortality has yet to be demonstrated. Bosentan has been shown to decrease the occurrence of new digital ulcers and calcium-channel blockers, iloprost, epoprostenol, and nitroglycerin paste have shown to lessen Raynaud’s disease attacks and lessen digital ulceration modestly (1). The therapies targeting vascular damage remain limited. Whether SSc is primarily due to excessive inflammation, vascular damage, or fibrosis, there is a significant amount of evidence that implicates pathologic bone marrow-derived immune cells as key players in all of these processes. As such stem cell transplantation remains a promising avenue by which to dramatically alter the immune status of patients with severe SSc. Small, uncontrolled studies suggest that both allogeneic and autologous stem cell transplantation can result in significant resolution of the disease (1,7). There are two large multicenter studies currently underway including the European ASTIS trial and the US SCOT trial (1). The main barriers to stem cell treatment will be the risks associated with the procedure as well as being able to identify patients whose prognosis is grave enough to require a transplant. Given the variability in terms of disease progression, until the factors mediating a more severe course of disease are clearly delineated, this will remain a challenge. Whether such an intervention will require implementation early in the course of the disease to have maximal impact or can reverse disease that has already progressed significantly remains to be seen from the trials. Through both previous and ongoing studies, sets of validated response measures are being developed to better standardize and report responses to treatment for SSc (1). This will likely improve the quality and reliability of research articles reported and enable clinicians to assess whether a given patient is likely to respond to a specific treatment. Overall, SSc is an incredibly difficult disease to treat and prevent from progression. However, new mechanistic insights into the disease along with ambitious trials using stem cell transplantation hold great promise for both better understanding and treating SSc. 1. Klippel JH, Crofford, LJ, Stone JH, Weyand CM (eds). Atlanta: Arthritis Foundation, 2001. 2. Charles C, Clements P, Furst DE. Systemic sclerosis: hypothesis-driven treatment strategies. The Lancet 2006;367:1683. 3. Tashkin DP, Elashoff R, Clements PJ et al. Cyclophosphamide versus placebo in scleroderma lung disease. N Engl J Med 2006 2006;354:2655. 4. Clements PJ, Furst DE, Silver RM, et al. Cyclosporin (CsA) in systemic sclerosis (SSc): Results of a 48-week open safety study in 10 SSc patients. Arthritis Rheum 1993; 36:75. 5. Liossis SN, Bounas A, Andonopoulos AP. Mycophenolate mofetil as first-line treatment improves clinically evident early scleroderma lung disease. Rheumatology (Oxford). 2006;45:1005. 6. Baroni SS, Santillo M, Bevilacqua F et al. Stimulatory autoantibodies to the PDGF receptor in systemic sclerosis. N Engl J Med 2006;354:2667. 7. Nash RA, Nelson JL, George GE et al. Allogeneic marrow transplantation in patients with severe systemic sclerosis. Arthritis & Rheumatism 2006;54;1982.