2-4 Mass Fatality Considerations[1]
advertisement
![2-4 Mass Fatality Considerations[1]](http://s3.studylib.net/store/data/007888423_2-b4989f39f57cf82749182a6de8d0f1d9-768x994.png)
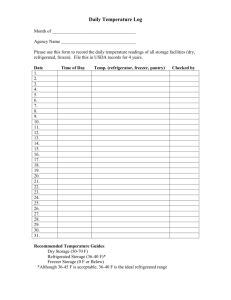
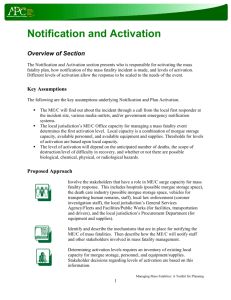
Chapter 2 – Patient Management Hospital Surge Capacity Toolkit CHAPTER 2 – PATIENT MANAGEMENT 2-4 MASS FATALITY CONSIDERATIONS1 Decomposition/Refrigerated Storage Until the spread of disease and the associated mortality rate slows, the hospital must focus on the collection of minimal but specific victim identification materials and the placement of the deceased in temporary storage. Those who die during a surge event may need to be stored for an extended period until the Medical Examiner/Coroner is able to identify remains, determine cause and manner of death, and issue a death certificate. Hospitals should plan to: Augment existing refrigerated morgue spaces to manage an increased number of human remains. Bring refrigerated trailers or conex boxes with diesel or electrical power to the medical facility to increase human remains storage. Identify secure spaces on medical facility property, which have the capability to decrease room temperatures. These areas may be required to store human remains for medical facilities without the ability to locate or obtain refrigerated trailers. Body decomposition slows once remains are placed in cold storage (between 37–42 degrees Fahrenheit). Bodies can be stored for up to 6 months in refrigerated storage, which may provide Medical Examiner/Coroner and funeral directors enough time to process all bodies in accordance with jurisdictional standards and traditional public expectations. Placing all remains in refrigerated storage may not be an option due to several factors, including limited gasoline to supply generators, limited maintenance personnel to repair broken units, limited refrigeration units. Thus, a nontraditional method of temporary storage, such as temporary interment, may be necessary. The healthcare facility must be prepared to make public statements regarding storage solutions, particularly the employment of long-term temporary interment. Personal Effects Management Maintain separate personal effects (PE) storage area for items belonging to the deceased. Establish policy for documenting and recording all PE on a chain of evidence document. Have all chain of evidence documents signed by the retrieving funeral homes (contracted by the families) when they pick up the remains and PE. Family Bereavement Provide mental health and counseling services. Provide an environment in which the families may grieve in private. 1 Adapted from: Capstone Document: Mass Fatality Management for Incidents Involving Weapons of Mass Destruction, Prepared By: U.S. Army Research Development and Engineering Command, August 2005. May 2008 2-4 Mass Fatality Considerations Page 1 of 2 Hospital Surge Capacity Toolkit Chapter 2 – Patient Management Death Certificates Before a body can be released to the family or transition to permanent final disposition, a death certificate is required. When a death is attended and the identity is known, it may be difficult to obtain a signed death certificate during a healthcare surge because hospital staff physicians will be overwhelmed caring for the living. Licensed physicians who are not hospital staff could/can augment the medical treatment facilities by reviewing medical records to complete and certify death certificates. Depending upon the capabilities of the jurisdiction, Medical Examiner/Coroner and their trained staff could also assist in the certification of death for medical treatment facilities. Planning Recommendation The following references may be helpful to you as you develop your Mass Fatality Plan: A-3, pages 9-16 – Stanford University Medical Center – Mass Fatality Plan APC Toolkit, Managing Mass Fatalities: A Toolkit for Planning available online at www.sccphd.org May 2008 2-4 Mass Fatality Considerations Page 2 of 2