total body hypothermia protocol for neonates with hypoxic
advertisement

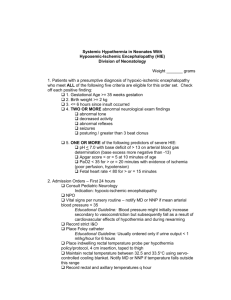
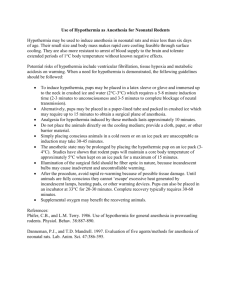
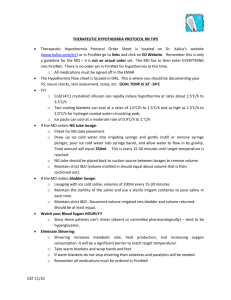
TOTAL BODY HYPOTHERMIA PROTOCOL FOR NEONATES WITH HYPOXIC ISCHEMIC ENCEPHALOPATHY (HIE) FOR USE DURING TRANSPORT The following guidelines are to assist with the assessment of neonates with HIE for total body hypothermia. If deemed eligible, all neonates who receive hypothermia should be transported to a tertiary NICU and ongoing management of these neonates should take place only in a tertiary NICU. Early referral is key to optimizing treatment. Evidence suggests that hypothermia in neonates with moderate to severe HIE reduces the severity of brain injury and leads to improved neurological outcome1-4. There is no evidence to support hypothermia in neonates with mild HIE. It is important for all neonates born with perinatal distress be assessed for risk factors and carefully monitored for signs of HIE immediately after, and for the first few hours after birth. If moderate or severe HIE is suspected, the tertiary centre should be contacted as early as possible in order to assess for eligibility for hypothermia. For eligible neonates, the earlier the initiation of hypothermia, the more likely it is to be effective, and hypothermia should be initiated within 6 hours of birth. 1.0 INCLUSION CRITERIA MUST HAVE ALL 3 INCLUSION CRITERIA 1.Evidence of intrapartum hypoxia ( 2 or more of the following criteria ) a. Apgar score 5 or less at 10 minutes b. Need for mechanical ventilation or resuscitation at 10 minutes c. Cord or blood gas within one hour of birth with pH less than 7.00, OR cord or arterial gas within one hour of birth with base deficit less than or equal to 12 2. Neonate = >35 weeks gestational age 3. Evidence of moderate or severe encephalopathy defined as clinical seizures OR Sarnat stage 2 or 3 TABLE Category 1. Level of consciousness 2. Spontaneous activity 3. Posture Moderate Encephalopathy Lethargic Decreased activity Distal flexion, truncal extension 4. Tone 5. Primitive reflexes Suck Moro 6. Autonomic system Pupils Gaze Heart rate Respirations Hypotonia (focal or general) Weak Incomplete Constricted Bradycardia Periodic breathing Severe Encephalopathy Stupor or coma No activity Decerebrate (arms extended and internally rotated, legs extended with feet in forced plantar flexion) Flaccid Absent Absent Dilated or non-reactive to light Skew deviation Variable HR Apnea *A neurological examination must be performed by skilled personnel to determine the degree of encephalopathy. 2.0 EXCLUSION CRITERIA • > 6 hours of birth (or later, at discretion of the attending neonatologist) • Birth weight less than 2.0 kg • Life threatening coagulopathy • Uncertainty about the diagnosis (Diagnosis to be confirmed by the Neonatal Fellow and/or Attending Neonatologist) • Infants who, in the opinion of the Attending Neonatologist, are unlikely to benefit from cooling Neonate with an imperforate anus if rectal probe to be used; not an exclusion if esophageal probe can be used 3.0 WHEN SHOULD COOLING BE COMMENCED? Earlier initiation of hypothermia may increase the degree of neuroprotection. For eligible neonates, hypothermia should be started within 6 hours of birth. The decision to start hypothermia after 6 hours of age will be at the discretion of the responsible neonatologist. There is currently no published evidence on the effects of starting hypothermia after 6 hours. Total body hypothermia to a target core body temperature of 33.0-34.0ºC can be achieved passively by turning all heat off or actively with cool packs. Most important is continuous temperature monitoring 4.0 HYPOTHERMIA FOR AN ELIGIBLE PATIENT IN THE REFERRING HOSPITAL IF TRANSPORT TEAM UNABLE TO ARRIVE WITHIN 6 HOURS AFTER BIRTH * MCH does not recommend cooling be commenced prior to arrival of the Transport team 1. Staffing and resources must be sufficient for constant monitoring and one to one nursing care until handover to the transport team 2. Ensure that the MCH neonatologist is in agreement with the decision to start hypothermia treatment before talking to parents. 3. Ensure that the parent(s) are aware that the results from studies have shown improved outcome for many of these babies, but that poor outcome is still possible and that this is a new therapy where long-term outcomes beyond 2 years of age are not known. (See Parent Information Sheet) 4. The referring hospital staff must be trained in the continuous monitoring of core (rectal/esophageal) temperature in advance. Specific equipment including a rectal/esophageal probe and a special module used to connect the probe to the monitor are required. Monitor rectal temperatures every 15 minutes and aim for a target temperature of 34ºC. 5. Ask MCH for the detailed hypothermia protocol to be faxed to you. Call the transport hotline at 905 521 2600 In the presence of severe encephalopathy where the risk of death or adverse neurodevelopmental outcome is assessed to be high, the responsible physician(s) may choose to not offer hypothermia treatment if the plan is to not pursue aggressive treatment. Note however, that initiation of hypothermia does not preclude a decision to withdraw life-sustaining therapy at a later time. REFERENCES 1. Gluckman PD, Wyatt JS, Azzopardi D, Ballard R, Edwards AD, Ferriero DM, Polin RA, Robertson CM, Thoresen M, Whitelaw A, Gunn AJ. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet 2005;365(9460):663-670 2. Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, Fanaroff AA, Poole WK, Wright LL, Higgins RD, Finer NN, Carlo WA, Duara S, Oh W, Cotten CM, Stevenson DK, Stoll BJ, Lemons AJ, Guillet R, Jobe AH. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med 2005;353:1574-1584 3. Jacobs S, Hunt R, Tarnow-Mordi W, Inder T, Davis P. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev 2007;(4):CD003311 4. Shah PS, Ohlsson A, Perlman M. Hypothermia to treat neonatal hypoxic ischemic encephalopathy: a systematic review. Arch Pediatr Adolesc Med 2007;161:951-958 5. Sahni R, Sanocka UM. Hypothermia for hypoxic-ischemic encephalopathy. Clin Perinatol 2008;35(4):71734 6. Thoresen M. Supportive care during neuroprotective hypothermia in the term newborn: adverse effects and their prevention. Clin Perinatol 2008;35(4):749-763 7. Barks JD. Technical aspects of starting a neonatal cooling program. Clin Perinatol 2008;35(4):765-775 8. Schulzke SM, Rao S, Patole SK. A systematic review of cooling for neuroprotection in neonates with hypoxic ischemic encephalopathy – are we there yet? BMC Pediatr 2007;7:30 9. Edwards AD, Azzopardi DV. Therapeutic hypothermia following perinatal asphyxia. Arch Dis Child Fetal Neonatal Ed 2006;91(2):F127-31 10. Hoehn T, Hansmann G, Buhrer C, Simbruner G, Gunn AJ, Yager J, Levene M, Hamrick SE, Shankaran S, Thoresen M. Therapeutic hypothermia in neonates. Review of current clinical data, ILCOR recommendations and suggestions for implementation in neonatal intensive care units. Resuscitation 2008;78(1):7-12