30. DISORDERS OF SEX DEVELOPMENT (DSD)
Elizabeth T. Rosolowsky and Norman P. Spack
I. Definition and Nomenclature. The term “Disorders of Sex Development” (DSD) is
preferred over older terms such as “ambiguous genitalia,””pseudohermaphroditism,” and
“intersex” to connote atypical development of genetic, gonadal, and phenotypic sex. (Table
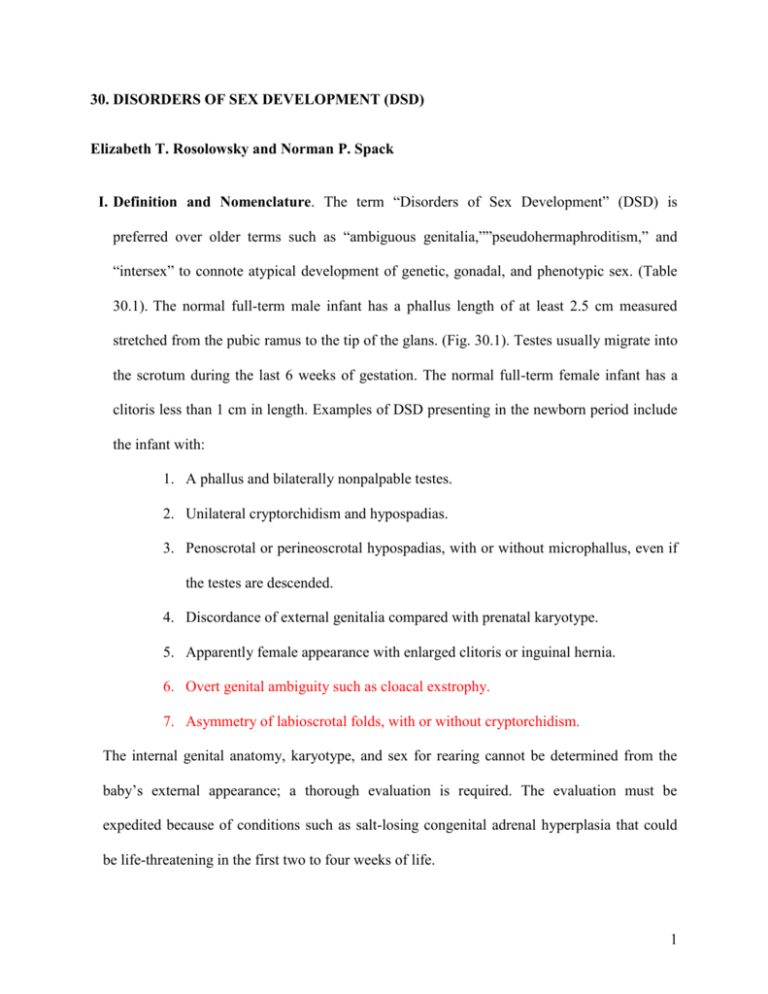
30.1). The normal full-term male infant has a phallus length of at least 2.5 cm measured
stretched from the pubic ramus to the tip of the glans. (Fig. 30.1). Testes usually migrate into
the scrotum during the last 6 weeks of gestation. The normal full-term female infant has a
clitoris less than 1 cm in length. Examples of DSD presenting in the newborn period include
the infant with:
1. A phallus and bilaterally nonpalpable testes.
2. Unilateral cryptorchidism and hypospadias.
3. Penoscrotal or perineoscrotal hypospadias, with or without microphallus, even if
the testes are descended.
4. Discordance of external genitalia compared with prenatal karyotype.
5. Apparently female appearance with enlarged clitoris or inguinal hernia.
6. Overt genital ambiguity such as cloacal exstrophy.
7. Asymmetry of labioscrotal folds, with or without cryptorchidism.
The internal genital anatomy, karyotype, and sex for rearing cannot be determined from the
baby’s external appearance; a thorough evaluation is required. The evaluation must be
expedited because of conditions such as salt-losing congenital adrenal hyperplasia that could
be life-threatening in the first two to four weeks of life.
1
II. Assignment of a sex for rearing. Rapidity in the determination of sex assignment is
essential for the parents’ peace of mind but must be balanced against prematurely drawing
conclusions about gender. Most causes can be clarified in two to four days, although some
cases may take one to two weeks or longer. Sex assignment depends on anatomy, functional
prenatal and postnatal endocrinology, and the potential for sexual functioning and fertility,
which may be independent of chromosomal sex. Until a gender assignment is made, genderspecific names or references should be withheld. Inappropriate statements may have
profound psychosocial consequences for families. After their infant’s genitalia are examined
in their presence, the parents should be told about the process of genital differentiation; that
their child’s genitalia are incompletely or variably formed; and that further tests will clarify
the problem and provide the necessary information to be able to assign the gender. If future
hormonal therapy is necessary, parents should be reassured that it will enable their child to
live a normal life. Options for surgery on the internal and/or external genitalia should be
discussed in the context of a team approach consisting of a pediatrician/neonatologist,
pediatric endocrinologist, pediatric surgeon, geneticist, and a counselor experienced in
dealing with these issues. No guarantees should be made about fertility.
III. Normal sexual development. The process of gonadal and genital differentiation is described
in Fig. 30.2. Sex determination progresses in stages. At fertilization, genetic sex is
determined. Under the influence of specific genes such as SRY (which encodes for testisdetermining factor) located on the short arm of the Y chromosome, gonadal sex is
determined by the seventh week of gestation. Specific ovarian-determining genes have also
been identified. 46,XX males and 46,XY females result from aberrant X-Y interchange
during paternal meiosis.
2
The testis secretes two hormones critical for genital formation: Anti-Müllerian hormone
(AMH) from the Sertoli cells, which causes regression of the Müllerian ducts (which would
otherwise become uterus, fallopian tubes, and upper vagina), and testosterone from the
Leydig cells, which promotes development of the Wolffian ducts (into the vas deferens,
seminal vesicles, and epididymis). Müllerian duct regression and Wolffian duct development
require high local concentrations of AMH and testosterone, respectively. Failure of a testis to
develop on one side may result in ipsilateral retention of Müllerian structures and regression
of Wolffian structures. The enzyme 5-reductase, in high concentration in genital skin,
converts testosterone to dihydrotestosterone, which is responsible for masculinizing of the
genital tubercle and labioscrotal folds to form the penis and scrotum, respectively. Formation
of normal male internal and external genitalia requires that the target tissues contain
functional androgen receptors.
The time course of fetal sexual differentiation is depicted in Fig. 30.3 and Table 30.2.
Phenotypic sex is established at the end of the first trimester. If a female infant is exposed to
excessive androgens during the first trimester, her clitoris and labioscrotal folds will virilize
and may appear indistinguishable from a normal male phallus and scrotum, although the
latter will be empty. Exposure to testosterone during the second and third trimesters lead to
clitoral enlargement and darkening and rugation of labioscrotal folds, but not labial fusion.
Testosterone synthesis during the first trimester in the male fetus is stimulated primarily by
placental human chorionic gonadotropin (hCG) due to its LH-like action. In the second and
third trimesters, male phallic growth and scrotal maturation are dependent on testicular
androgens stimulated by gonadotropins from the fetal pituitary. Endogenous growth hormone
3
also contributes to penile growth. High intrauterine concentrations of testosterone may
influence the brain in terms of later behavior and gender identity formation.
IV. Nursery evaluation of a newborn with suspected disorder of sex development.
A.History
1. Family history of hypospadias, congenital adrenal hyperplasia, cryptorchidism,
infertility, consanguinity, genetic syndromes.
2. Maternal drug exposure in pregnancy such as to synthetic androgens (e.g. Danazol),
anti-seizure
medication
(e.g.
Phenytoin,
Trimethadione),
anti-androgens
(e.g.
Finasteride, spironolactone), estrogens, or progestins.
3. Maternal virilization in pregnancy (maternal adrenal hyperplasia; virilizing adrenal or
ovarian tumor; fetal aromatase deficiency).
4. Neonatal deaths. Death from vomiting/dehydration of a male sibling in early infancy,
possibly
from
undiagnosed
congenital
adrenal
hyperplasia
(CAH).
Genital
manifestations of CAH from 21-hydroxylase deficiency in a male are subtle.
5. Placental insufficiency. Human chorionic gonadotropin (hCG) initiates first-trimester
synthesis of testosterone in the fetal testis.
B. Physical examination
1. The examiner should note stretched phallic length, width of the corpora (Table 30.3),
engorgement, presence of chordee, position of the urethral orifice, presence of a vaginal
opening, and pigmentation and symmetry of the scrotum or labioscrotal folds. Posterior
fusion of the labioscrotal folds is defined as an increased “anogenital ratio,” which is
determined by measuring the distance between the anus and posterior fourchette divided
4
by the distance between the anus and base of the clitoris. An anogenital ratio >0.5 is
indicative of early intrauterine androgen exposure.
2. Gonadal size, position, and descent should be carefully noted. A gonad below the
inguinal ligament is usually a testis, but an ovotestis and a uterus may present as a
hernia. Genital ambiguity with clitoromegaly or an apparently well-formed phallus and
an empty scrotum should raise immediate concern that the infant is a female virilized by
CAH.
3. Bimanual rectal examination may reveal Müllerian structures. e.g. a palpable cervix or
uterus in the midline.
4. Associated anomalies: Dysmorphic features suggest a more generalized disorder. DenysDrash syndrome (Wilms’ tumor and nephropathy) or WAGR syndrome (Wilms’ tumor,
Aniridia, Genitourinary anomalies, and mental Retardation) can affect both 46,XY and
46,XX infants and are due to mutations of the WT1 gene on 11p13. Other syndromes
associated with genital ambiguity include Smith-Lemli-Opitz, Robinow, Goldenhar
syndromes, and Trisomy 13.
5. Circumcision is contraindicated until a determination is made concerning the need for
surgical reconstruction.
C.Diagnostic tests
1. Laboratory tests are tailored to the differential diagnosis, though baseline serum
electrolytes, BUN, creatinine,17-hydroxyprogesterone, plasma renin activity, testosterone,
gonadotropins, and anti-Müllerian hormone are included or considered. Chromosome
analysis on peripheral blood can be performed using standard techniques within 72 hours
and more rapidly via fluorescent in situ hybridization (FISH). A standard karyotype may
5
reveal 46,XX, but portions of the Y chromosome containing the SRY gene may be
translocated to an X chromosome. FISH techniques may be required to locate or confirm
Y material.
2. Pelvic ultrasound, especially when the bladder is full, can determine whether a uterus
is present. Testes can often be visualized, ovaries less well. Magnetic resonance imaging
(MRI) may be needed to locate intra-abdominal testes.
3. Vesicourethrogram (VCUG) or genitogram. These studies may reveal a vagina with
cervix at its apex or a utricle (a Müllerian duct remnant).
V. 46,XX DSD (virilized 46,XX females). The infant has normally developed Müllerian
structures and no Wolffian structures but has evidence of external genital virilization.
A.The most common form of genital ambiguity is a female infant with congenital adrenal
hyperplasia from 21-hydroxylase (21-OH in Fig 30.4) due to mutations in the gene
CYP21. Virilization may occur in other adrenogenital syndromes: 11-hydroxylase (11OH or CYP11B1) deficiency or 3-hydroxysteroid dehydrogenase (3-HSD or HSD3B2)
deficiency. CYP11B1 deficiency also presents with hypertension, while CYP21 and
HSD3B2 deficiency may progress to hypovolemic shock if diagnosis is delayed.
1. State newborn screening programs may include screening for CYP21 deficiency. Blood
spot measurements on filter-paper of 17-hydroxyprogesterone (17-OHP) are ideally
performed between 48 and 72 hours post-natal age. An abnormal test is flagged when
17-OHP levels exceed 50 ng/mL (5000 ng/dL) 24-hours after birth in affected full-term
infants. Normal values must be determined for each individual program since they
depend on the filter-paper thickness and the radioimmunoassay used. In 90% of infants
with adrenogenital syndrome, the 17-OHP will be elevated. Worldwide newborn
6
screening programs for 17-OHP show an incidence of 1:15,000 births; the incidence
varies markedly by country. Salt-losers outnumber simple virilizers by 3:1. The
male:female sex ratio is 1:1. The diagnosis of CYP21 deficiency in boys is difficult to
make by phenotype alone, though hyperpigmentation of the scrotum can be a clue.
False-positive results occur in sick, premature, and low-birth-weight infants. Rapid
turnaround of results is critical to avert salt-wasting crises. Abnormal results should be
confirmed by serum measurements of 17-OHP on the 2nd or 3rd day of age.
Measurements of plasma renin activity and aldosterone may also help differentiate
between the salt-wasting and simple- virilizing forms. Serum electrolytes should be
monitored at least every other day until salt-wasting status is determined. Levels of 11deoxycorticosterone would be elevated and hypertension present in an infant with
CYP11B1 deficiency. A female infant virilized from HSD3B2 deficiency would not be
expected to have elevated 17-OHP on newborn screen.
2. Virilized females suspected of 21-hydroxylase deficiency should be started on
hydrocortisone 20 mg/m^2/day, divided into q8h dosing, after the above laboratory tests
have been obtained. Salt-wasting crises usually do not develop until the fifth to
fourteenth day of life (and as old as one month) and may occur in affected infants whose
virilization is not severe. Weight, fluid balance, and electrolytes must be monitored
closely with blood samples at least every two days to detect hyponatremia or
hyperkalemia during the first few weeks of life. If salt-wasting occurs, salt loss should
be replaced with intravenous normal saline with glucose added. Once the infant is
stabilized, NaCl 2 to 3 grams/day, divided into q6h dosing, should be added to the
7
formula. Fludrocortisone acetate (Florinef) 0.05 to 0.2 mg/day should be given for
mineralocorticoid replacement.
3. In a virilized 46,XX female suspected of having a form of CAH, who has normal
equivocal 17-OHP levels, an ACTH (Cortrosyn) stimulation test may be necessary to
demonstrate the adrenal enzyme defect (see Fig. 30.4).
B. Placental aromatase deficiency. The hallmark of this disorder is that both mother and baby
are virilized due to an inability to convert androgens to estrogens.
C.Maternal hyperandrogenic conditions: CAH or virilizing tumors of the adrenal or ovary.
VI. 46,XY DSD (undervirilized 46,XY males). Even if the chromosomes contain Y material,
the parents should not be hastily told that the child should be raised as a male. In addition,
only 50% of 46, XY children with DSD will receive a definitive diagnosis.
A.Environmental
disorders.
maternal
drug
ingestion
(finasteride,
phenytoin,
spironolactone).
B. Hereditary disorders. Usually at least one gonad is palpable and there are no Müllerian
structures because of anti-Müllerian hormone secreted from the testes.
1. Partial or complete end-organ resistance to testosterone leading to partial androgen
insensitivty syndrome (PAIS) or complete androgen insensitivity syndrome (CAIS) (Xlinked recessive mutations of the androgen receptor gene).
2. Enzyme defects in testosterone synthesis: deficiencies of 17-hydroxysteroid
dehydrogenase type 3 also known as 17-ketosteroid reductase (17-HSD in Fig. 30.4 or
HSD17B3),
3-hydroxysteroid
dehydrogenase
(3-HSD
or
HSD3B2),
17-
hydroxylase/17,20-lyase (17-OH or CYP17), and isolated 17,20-lyase (17,20 Des in Fig.
30.4).
8
3. Defects in testosterone metabolism (5-reductase type 2 or SRD5A2 deficiency).
Though generally uncommon, the Dominican Republic and Middle East, have a higher
prevalence.
C.Laboratory evaluation. Sampling of serum electrolytes may reveal hyperkalemia and
hyponatremia in HSD3B2 deficiency or hypokalemia in CYP17 deficiency. Additional
laboratory evaluation is focused on determining whether the cause of undervirilization is
due to a defect in testosterone synthesis, metabolism, or action.
1. Obtain blood samples for measurement of electrolytes, follicle-stimulating hormone
(FSH), luteinizing hormone (LH), testosterone, dihydrotestosterone (DHT), antiMüllerian
hormone,
dehydroepiandrosterone
17-hydroxyprogesterone,
(DHEA).
Measurement
of
androstenedione,
17-OH
pregnenolone,
and
11-
deoxycorticosterone, and plasma renin activity may help define the type of enzyme
deficiency. If the above results do not lead to a diagnosis, Human Chorionic
Gonadotropin (hCG), 500 IU, is given intramuscularly every other day for a total of
three doses. This stimulation test should preferably take place within the first two to
three months of life when the hypothalamic-pituitary-gonadal axis is active.
Measurements of DHEA, androstenedione, testosterone, and DHT concentrations are
repeated 24 hours after the final dose. Inability to increase the testosterone level in
response to hCG is characteristic of a biosynthetic defect in testosterone synthesis, LH
receptor insensitivity, or gestational loss of testicular tissue (“vanishing testes”). An
elevated testosterone:DHT ratio (>20:1) after hCG stimulation suggests 5-reductase
deficiency.
9
2. An ACTH stimulation test may be necessary to define earlier enzyme defects in
testosterone synthesis such as salt-losing (HSD3B2) or salt-retaining (CYP17)
deficiencies, which also produce cortisol insufficiency and congenital adrenal
hyperplasia (Fig. 30.4)
3. If the initial laboratory tests show high levels of testosterone that do not increase when
hCG
is
given
and
the
ratios
of
testosterone:androstenedione
and
testosterone:dihydrotestosterone are normal, the infant probably has PAIS. This can be
further evaluated by the monthly administration of 25 to 50 mg of intramuscular depot
testosterone for 3 months. Failure of the stretched phallus length to increase by 2.0 ± 0.6
cm supports the suspicion of PAIS. In the past, infants with PAIS were given a female
gender assignment and underwent gonadectomy and feminizing genitoplasty. This
practice has become controversial. When a testis is retained, these patients will virilize
to a variable degree during puberty but will develop gynecomastia and will not achieve
normal adult phallic size on their own. It is not possible, however, to predict the extent
to which an infant with PAIS will respond to exogenous testosterone.
Newborns with the complete form of androgen resistance have normal-appearing
female genitalia and absent Müllerian and Wolffian structures. They may be identified
by an antepartum 46,XY karyotype (amniocentesis) or the presence of an apparent
inguinal hernia that proves to be a testis. Infants with CAIS should be raised female.
Their gender identities are invariably female.
D.Other causes of microphallus (<2.5 cm in a full-term infant) with or without
cryptorchidism include: hypothalamo-pituitary disorders of fetal gonadotrophin production
such as septo-optic dysplasia or Kallman’s Syndrome. Infants with panhypopituitarism
10
often have neonatal hypoglycemia and direct hyperbilirubinemia. Among the many
syndromes associated with microphallus are: CHARGE association, Prader-Willi,
Robinow, Klinefelter, Carpenter, Meckel-Gruber, Noonan, de Lange, trisomy 21, Fanconi,
and fetal hydantoin. Treatment with testosterone enanthate 25 mg given intramuscularly
monthly for 3 months may produce substantial increase in penile length in these patients.
E. Bilateral cryptorchidism. Bilateral cryptorchidism at birth occurs in 3:1000 infants, most
of whom are premature. By one month of life, the testes are still undescended in 1:1000.
Either ultrasonography or MRI may reveal inguinal or abdominal testes, though MRI is more
sensitive for locating the latter. If testicular tissue cannot be found, serum FSH, LH, and
testosterone levels should be measured. These hormones rise shortly after birth, are elevated
until about 6 months of age in boys, and therefore should be measurable. If gonadotropins
and testosterone levels are low, then three doses of hCG 500 IU can be given intramuscularly
every other day and serum testosterone remeasured 24 hours after the final dose to determine
the presence and responsiveness of testicular tissue. Elevated serum gonadotropins and a low
basal testosterone concentration that fails to rise suggests absent or nonfunctioning testes.
Undetectable AMH is indicative of bilateral anorchia rather than undescended testes (see
below). A urologist should be consulted and, if surgery is indicated, orchidopexy should be
performed by one year of life. If abdominal testes cannot be brought into the scrotum, they
should be removed because of the three- to tenfold increased risk of germ cell cancer in
cryptorchid testes.
The presence of any of the following physical findings also merits evaluation for disorder of
sex development:
11
a. Unilateral cryptorchidism and hypospadias, especially proximal (e.g., perineal and
penile) hypospadias.
b. Unilateral cryptorchisim with microphallus.
Cryptorchidism occurs in congenital ichthyosis, anencephaly, neural tube defects, PraderWilli, Bardet-Biedl, Aarskog, Cockayne, Fanconi, Noonan’s, Trisomy 21, and Klinefelter’s
syndromes.
VII.
Gonadal Differentiation Disorders
A.Ovotesticular DSD (True hermaphroditism). Less than 10% are 46,XY; 50% are
46,XX; and the remainder show mosaicism (45,X/46,XY or 46,XY/47,XXY) or are
chimeric for 46,XX/46,XY. Laparotomy, gonadal biopsy, or both, may be required to
diagnose the rare ovotesticular DSD. Diagnosis is based on the histology of the gonads,
which, by definition, contain both testicular and follicle-containing ovarian tissue.
Whether or not the internal structures contain Wolffian or Müllerian elements depends on
the local presence of testosterone and AMH on that side of the abdomen. The external
genitalia may appear normal or may show incomplete labioscrotal fusion, asymmetric
labioscrotal folds, and hypospadias. Sex assignment should be based on the external and
internal genitalia and the degree of intrauterine androgen exposure. An hCG stimulation
test that produces a rise in serum testosterone concentration confirms the presence of
Leydig cells, while a measurable AMH level indicates the presence of Sertoli cells.
Dysgenetic Y chromosome-containing gonads should be removed. If a male sex
assignment is made, Müllerian structures should be removed.
12
B. Mixed gonadal dysgenesis (MGD). The hallmark of MGD is the presence of testis on one
side of the body and either a streak or dysgenetic testis on the other side. This disorder has
a 45,X/46,XY chromosomal complement. Often the Y chromosome is abnormal, or Ymaterial may have been translocated to an autosome. The combination of asymmetric
external genitals with one palpable testis in the labioscrotal fold is almost certainly MGD,
although the appearance can range from completely male to completely female. The gonad
governs the differentiation of the ipsilateral internal duct. A fallopian tube and uterus are
frequently present, and these structures can herniate into a labioscrotal fold. Gender
assignment is discretionary because of the marked phenotypic and hormonal variability.
About two-thirds are raised as girls. If AMH is measurable or an hCG stimulation test
causes a significant rise in serum testostosterone concentration indicative of testicular
tissue, the testis should be sought and either removed if female sex assignment is made, or
brought into the scrotum for close observation if a male sex assignment is made. Gonadal
neoplasia (gonadoblastoma) may arise in the first 20 years of life in up to 20% of these
children. Therefore, streak and dysgenetic gonads should be removed in infancy. MGD is
one type of gonadal dysgenesis disorder, with Turner’s syndrome (45,XO or 45,X/46,XX)
being the classic example of absent or lack of full gonadal differentiation. Children with
MGD may have features of Turner’s syndrome: webbed neck, lymphedema, short stature,
and occasional cardiac defects, specifically coarctation of the aorta. They should be
considered early candidates for growth hormone treatment.
C.46,XX or 46,XY “complete” gonadal dysgenesis (CGD). 46,XY CGD has also been
referred to as complete sex reversal. Most do not have genital ambiguity at birth; in fact,
these children appear female. Infants with 46,XY gonadal dysgenesis fail to masculinize,
13
owing to incomplete testicular differentiation as a result of abnormal functioning of the
SRY gene or of transcription factors that regulate the gene’s activity. Bilateral streak
gonads are present. The external genitalia usually appear female, but clitoromegaly may
occur if “gonadal” hilus cells secrete testosterone. Up to 30% of patients with 46,XY
gonadal dysgenesis may develop gonadoblastoma or germinoma. These gonads should be
removed in infancy. Internal structures are female due to inadequate production of antiMüllerian hormone and testosterone from the undifferentiated gonads. These patients are
usually raised female and may not be diagnosed until they fail to initiate puberty and
exhibit high gonadotrophins consistent with gonadal failure. With gonads retained, these
patients may virilize at puberty. Individuals with 46,XX sex reversal appear
phenotypically male. At puberty, they resemble patients with Klinefelter’s syndrome
(small testes, azoospermia, eunochoid body habitus, gynecomastia) due to testosterone
deficiency. A loss of Y chromosome during early embryogenesis, a cryptic mosaicism
with Y-bearing cell line, or translocation of Y chromosomal material to the X chromosome
may be responsible.
VIII. Table 30.4 summarizes causes and Figs. 30.5 and 30.6 describe an approach to
patients with ambiguous genitalia.
Use of Anti-Mullerian Hormone (AMH). The hCG stimulation test can be cumbersome and
expensive and occasionally requires protracted dosing to stimulate a refractory testis. AMH is
produced in a sexually dimorphic manner. Starting at birth, AMH from Sertoli cells rises to a
peak of 115 ng/mL at 6 months and declines during adolescence to an adult level of 4 ng/mL;
in contrast, granulosa cells of the ovary do not make any significant amounts of AMH until
puberty when levels also reach about 4 ng/mL.
14
Measuring AMH by ELISA can distinguish between absent and present testicular tissue. AMH
in the normal or detectable range has a 100% positive predictive value that testicular tissue is
present; the negative predictive value for anorchia is 94% if AMH is undetectable.
IX. Issues of Gender Assignment
In the past, a primary criterion for male gender assignment was phallic size adequate for
sexual function. This issue is currently being debated. 46,XY infants born with little or no
penile tissue have usually been given female sex assignment and surgically and hormonally
feminized by means of genitoplasty early in life and estrogen treatment at the age of puberty.
The decision to assign gender is, however, complicated by evidence that the prenatal
hormonal environment may influence gender identity formation and gender role behavior.
During the second trimester, the normal fetal testis produces levels of testosterone
comparable to an adult male. The 46,XY neonate born with minimal penile tissue, who is not
androgen resistant and who has been exposed to normal intrauterine testosterone
concentrations, may retain a male gender identity regardless of gender assignment. Fueling
the debate are the new techniques such as intracytoplasmic sperm injection (ICSI) which
makes fertilization possible without penetration or ejaculation.
Likewise, the issue of gender assignment in the case of the most severely virilized 46,XX
newborns with congenital adrenal hyperplasia who have completely fused labioscrotal folds
and a phallic urethra is also under debate. A minority opinion recommends male assignment
and gonadectomy, thereby eliminating the need for feminizing genitoplasty. Nevertheless,
most geneticists and endocrinologists continue to recommend female assignment to preserve
fertility.
15
Whether and when to perform genital surgery, particularly clitoral reduction in virilized
females, is also the subject of controversy. Whereas some intersexual adults view their
genital surgery as mutilation, most parents prefer surgery so that their child’s genitalia appear
more consistent with the gender of rearing. One-stage surgical procedures that preserve the
neurovascular bundle can be done in infancy and are much improved compared to the
clitorectomies routinely performed several decades ago.
Parents require a thorough explanation of their child’s condition while the laboratory and
imaging data become available so they can participate in the decision-making as the various
options for medical and surgical therapy and future prospects for sexual functioning, genital
appearance, fertility, and gender identity are evaluated. Long-term, unbiased studies of
gender identity and sexual functioning in individuals born with various forms of genital
ambiguity are needed to provide insight for everyone involved in the difficult task of
assigning an appropriate gender for a specific infant.
Suggested Readings
American Academy of Pediatrics. Committee on Genetics. Evaluation of the newborn with
developmental anomalies of the external genitalia. Pediatrics 2000; 106: 138.
Anhalt H., et al. Ambiguous genitalia. Pediatr Rev 1996; 17: 213.
Berenbaum S.A. Effects of early androgens on sex-typed activities and interests in adolescents
with congenital adrenal hyperplasia. Horm Behav 1999; 35: 102.
Creighton S.M., et al. Objective cosmetic and anatomical outcomes at adolescence of feminising
surgery for ambiguous genitalia done in childhood. Lancet 2001; 358: 124.
16
Diamond M., Sigmundson H.K. Management of intersexuality: Guidelines for dealing with
persons with ambiguous genitalia. Arch Pediatr Adolesc Med 1997; 151: 1046.
Drummon-Borg M., et al. Nonfluorescent dicentric Y in males with hypospadias. J Pediatr 1988;
113: 469.
Federman D.D., Donahoe P.K. Ambiguous genitalia—etiology, diagnosis and therapy. Adv
Endocrinol Metab 1995; 6: 91.
Hawkins J.R. The SRY gene. Trend Endocrinol Metab 1993; 4: 328.
Hawkins J.R., et al. Evidence for increased prevalence of SRY mutations in XY females with
complete rather than partial gonadal dysgenesis. Am J Hum Genet 1992; 51: 1979.
Hughes, I.A., Houk, C., Ahmed, S. F., Lee, P. A., LWPES Consensus Group, ESPE Consensus
Group. Consensus statement on management of intersex disorders. Archives of Disease in
Childhood 2006; 91: 554-563.
Lee MM. MIS/AMH in the assessment of cryptorchidism and intersex conditions. Mol Cell
Endocrinol 2003; 211: 91-98.
Lee P.A. Fertility in cryptorchidism: Does treatment make a difference? Endocrinol Metab Clin
North Am 1993; 22: 479.
New MI. Inborn errors of adrenal steroidogenesis. Mol Cell Endocrinol 2003; 211:75-83.
Neri G. Syndromal (and nonsyndromal) forms of male pseudohermaphrodism. Am J Med Genet
1999; 89: 201-9.
17
Page D.C., et al. Exchange of terminal portions of X- and Y- chromosomal short arms in human
XX males. Nature 1987; 328: 437.
Pang S., et al. Congenital adrenal hyperplasia due to 21 hydroxylase deficiency: Newborn
screening and its relationship to the diagnosis and treatment of the disorder. Screening 1993; 2:
105.
Papadimitriou DT. Puberty in subjects with complete androgen insensitivity syndrome.
Hormone Research 2006; 65(3): 126-31.
Pritchard-Jones K., et al. The candidate Wilms’ tumour gene is involved in genitourinary
development. Nature 1990; 346: 194.
Reiner W.G. Assignment of sex in neonates with ambiguous genitalia. Curr Opin Pediatr 1999;
11: 363.
Saenger P. Male pseudohermaphroditism. Pediatr Ann 1981;10:15.
Savage M.O., Lowe D.G. Gonadal neoplasia and abnormal sexual differentiation. Clin
Endocrinol 1990; 32: 519.
Schnitzer J.J., Donahoe P.K. Surgical treatment of congenital adrenal hyperplasia. Endocrinol
Metab Clin North Am 2001; 30: 137.
Styne D.M. The testes: Disorders of sexual differentiation and puberty. In: Sperling M.A. (Ed.),
Pediatric Endocrinology. Philadelphia: Saunders, 1996;424.
Therell B.L. Newborn screening for congenital adrenal hyperplasia. Endocrinol Metab Clin
North Am 2001;30:15.
18
Vainio S., et al. Female development in mammals is regulated by Wnt-4 signalling. Nature
1999;397:405.
Warne G.L., Zajac J.D. Disorders of sexual differentiation. Endocrinol Metab Clin North Am
1998;27:945.
Williams Textbook of Endocrinology. 10th Edition. Editors Larsen, Kronenberg, Melmed,
Polonsky. Chapter 22 “Disorders of Sex Differentiation” by Grumbach MM, Hughes IA, and
Conte FA. Copyright 2003 Elsevier Science, USA.
Witchel S.S., Lee P.A. Ambiguous genitalia. In: Sperling M.A. (Ed.), Pediatric Endocrinology.
Philadelphia: Saunders, 1996;32.
PREVIOUS
PROPOSED
Intersex
Disorders of Sex Development
Male pseudohermaphrodite
46, XY DSD
Undervirilization of an XY male
Undermasculinization of an XY male
Female pseudohermaphrodite
46, XX DSD
Overvirilization of an XX female
Masculinization of an XX female
True Hermaphrodite
Ovotesticular DSD
XX male or XX sex reversal
46, XX testicular DSD
19
XY sex reversal
46, XY complete gonadal dysgenesis
TABLE 30.1 Proposed revised nomenclature. (From Hughes, I. A., Houk, C., Ahmed, S. F., Lee,
P. A., LWPES Consensus Group, ESPE Consensus Group. (2006). Consensus statement on
management of intersex disorders. Archives of Disease in Childhood, 91(7), 554-563.)
FIG. 30.1. Stretched phallic length of normal premature and full-term babies (closed circles),
showing lines of mean 2 standard deviations. Correlation coefficient is 0.80. Superimposed are
data for two small-for-gestational-age infants (open triangles), seven large-for-gestational-age
infants (closed triangles), and four twins (closed boxes), all of whom are in the normal range.
(From Feldman K.W., Smith D.W. Fetal phallic growth and penile standards for newborn male
infants. J Pediatr 1975;86:395.)
FIG. 30.2. The process of gonadal, internal, and genital differentiation. (From Holm I.A.
Ambiguous genitalia in the newborn. In: Emans S.J. et al. (Eds.), Pediatric and Adolescent
Gynecology. Philadelphia: Lippincott-Raven, 1998:53.)
FIG. 30.3. Timelines for five aspects of sexual differentiation. (From White P.C., Speiser P.W.
Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Endocrine Rev. 21(3),
2000:245–291. Adapted from Barthold J.S., Gonzalez R. Intersex states. In: Gonzalez E.T.,
Bauer S.B. (Eds.), Pediatric Urology Practice. Philadelphia: Lippincott Williams & Wilkins,
1999;547–578.)
20
TABLE 30.2. TIMETABLE OF SEXUAL DEVELOPMENT
Days after Conception
Events of Sexual Development
19
Primordial germ cells migrate to the genital ridge
40
Genital ridge forms an undifferentiated gonad
44
Müllerian ducts appear; testes develop
62
Müllerian inhibitor (from testes) becomes active
71
Testosterone synthesis begins (induced by placental
chorionic gonadotropin)
72
Fusion of the labioscrotal swellings
73
Closure of the median raphe
74
Closure of the urethral groove
77
Müllerian regression is complete
FIG. 30.1. Stretched phallic length of normal premature and full-term babies (closed circles),
showing lines of mean 2 standard deviations. Correlation coefficient is 0.80. Superimposed are
data for two small-for-gestational-age infants (open triangles), seven large-for-gestational-age
infants (closed triangles), and four twins (closed boxes), all of whom are in the normal range.
(From Feldman K.W., Smith D.W. Fetal phallic growth and penile standards for newborn male
infants. J Pediatr 1975;86:395.)
SEX
POPULATION AGE
STRETCHED PENILE PENILE
21
LENGTH (CM)
WIDTH (CM)
M
USA
30 WKS GA
2.5
M
USA
TERM
3.5 (0.4)
M
JAPAN
TERM
2.9 (0.4)
M
AUSTRALIA
24-36 WEEKS GA
2.27 + (0.16 GA)
M
CHINA
3.1 (0.3)
1.07 (0.09)
M
INDIA
TERM
3.6 (0.4)
1.14 (0.07)
M
N. AMERICA
TERM
3.4 (0.3)
1.13 (0.08)
M
EUROPE
ADULT
13.3 (1.6)
CLITORAL
1.1 (0.1)
LENGTH CLITORAL
(MM)
WIDTH (MM)
3.32 (0.78)
F
USA
TERM
4.0 (1.24)
F
USA
ADULT
15.4 (4.3)
NULLIPAROUS
F
USA
ADULT
19.1 (8.7)
5.5 (1.7)
TABLE 30.3 Anthropometric measurements of the external genitalia. (Adapted from Hughes, I.
A., Houk, C., Ahmed, S. F., Lee, P. A., LWPES Consensus Group, ESPE Consensus Group.
(2006). Consensus statement on management of intersex disorders. Archives of Disease in
Childhood, 91(7), 554-563.)
FIG. 30.4. Pathways of steroid biosynthesis. (From Esoterix, 4301 Lost Hills Road, Calabasas
Hills, CA 91301.)
22
Disorders of testosterone synthesis
Ambiguous
Testes
46,XY
Side chain cleavage enzyme deficiency
17a-hydroxylase deficiency
3b-OH steroid dehydrogenase deficiency
17-lyase deficiency
17-ketosteroid reductase deficiency
End-organ resistance to testosterone
Complete testicular feminization
Female
Testes
46,XY
Incomplete testicular feminization
Ambiguous
Testes
46,XY
5a-reductase deficiency
Ambiguous
Testes
46,XY
Vanishing testes syndrome
Variable
Absent gonads
46,XY
Disorder of testosterone metabolism
Lack of Müllerian inhibiting substance Male
Testes, uterus, fallopian tubes 46,XY
TABLE 30.4 Causes of Ambiguous Genital Development (From Wolfsdorf J.I., Muglia L.,
Endocrine Disorders. In: Graef J.W. (Ed.), Manual of Pediatric Therapeutics. Philadelphia:
Lippincott-Raven, 1997:381–413.)
HCG = human chorionic gonadotropin; LH = luteinizing hormone.
FIG. 30.5. Algorithm for the evaluation of symmetrical genital ambiguity. A’dione =
androstenedione; AIS = androgen insensitivity syndrome; DHT = dihydrotestosterone; FSH =
follicle stimulating hormone; LH = luteinizing hormone; 17 Preg = 17-hydroxypregnenolone; 17
Prog = 17-hydroxyprogesterone; T = testosterone. (From Witchel S.S., Lee P.A., Ambiguous
23
genitalia. In: Sperling M.A. (Ed.), Pediatric Endocrinology. Philadelphia: Saunders, 1996:31–
49.)
FIG. 30.6. Algorithm for the evaluation of asymmetrical genital ambiguity. (From Witchel S.S.,
Lee P.A. Ambiguous genitalia. In: Sperling M.A. (Ed.), Pediatric Endocrinology. Philadelphia:
Saunders, 1996:31–49.)
24