ACLS Drug
advertisement

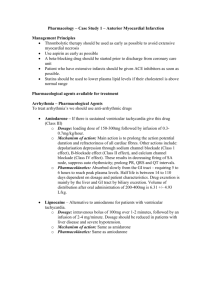
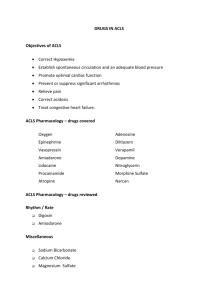
Adenosine (Adenocard) First Line ACLS Drug YES! Indications and uses Adenosine slows tachycardias associated with the AV node via modulation of the autonomic nervous system without causing negative inotropic effects. It acts directly on sinus pacemaker cells and vagal nerve terminals to decrease chronotropic and dromotropic activity. Adenosine is the drug of choice for paroxysmal supraventricular tachvcardia (PSVT) and can be used diagnostically for stable, wide complex tachyardias of unknown type after two doses of lidocaine. Dosage and Administration Give 6mg IV push rapidly over 1-3 seconds as close to vein as possible. If no response is observed after 1-2 min, administer 12 mg over 1-3 sec. The second 12 mg dose may be repeated once if needed (maximum 30 mg dose). Adverse Reactions The following Side Effects have been documented: Facial flushing, lightheadedness, paresthesia, headache, diaphoresis, palpitations, chest pain, hypotension, nausea, metallic taste, and shortness of breath. Special Considerations Contraindicated in the following rhythms: Second- or third-degree AV block, or sick-sinus syndrome. Atrial flutter, Atrial fibrillation, and Ventricular tachycardia. Adenocard will cause a 6-10 arrest, this is expected. Methylxanthines (for example, caffeine and theophylline) antagonize the action of adenosine. Dipyridamole potentiates the effect of adenosine; reduction of adenosine dose may be required. Carbamazepine may potentiate the AV-nodal blocking effect of adenosine. Atropine First Line ACLS Drug YES! Indications and uses Indications: Increases the Heart Rate. Uses: Used in bradycardia rhythms to increase the heart rate. (see special considerations) Also used in Asystole. Dosage and Administration Give 0.5-1mg I.V. push every 3-5 minutes to a maximum dose of 3 mgs. May be given down the endotracheal tube. Mix with 10cc normal saline when giving the E.T. route. Adverse Reactions May cause worsening of myocardia ischemia, worsening of AV Blocks, and may cause PVC's or Ventricular Tachycardia. May result in undesired tachycardia. Special Considerations Doses smaller than 0.5mg may enhance bradycardia and should not be used. Atropine is no longer indicated in Second Degree Type II or Third Degree AV Blocks! Dobutamine First Line ACLS Drug NO! Indications and uses Indications: Dobutamine is a positive inotrophic drug, resulting in increased myocardial contracture, thus improving cardiac output. Uses: Dobutamine is used primarily in congestive heart failure associated with poor cardiac output. Dosage and Administration The usual dose is 1 gram mixed in 250cc Normal Saline. The starting dose is 2.mcg/kg/min I.V. then titrated up to 20mcg/kg/min. Adverse Reactions Dobutamine may cause hypotension secondary to it's beta-2 properties. Tachycardia may result from Dobutamine's beat-1 properties, do not permit the heart rate to increase by 10% of it's original rate. Dobutamine may cause an increase in ventricular ectopy. Special Considerations It is recommended that Dobutamine be titrated and controlled by a volumetric infusion pump. Continuous cardiac monitoring is a necessity, and frequent blood pressure measurement is recommended. Dopamine First Line ACLS Drug YES! Indications and uses Indications: Dopamine is used primarily for the treatment of hypotension that is not secondary to hypovolemia. Dopamine has different effects at precise dosage levels. Greater than 10mcg/kg/min it has Alpha properties used to treat hypotension. At low dosage, 1-3mcg/kg/min it has dopaminergic properties that result in vasodilitation of renal, messenteric, and cerebral arteries. At dosages between 310mcg/kg/min it has beta-1 properties, similar to dobutamine. Uses: For treatment of hypotension that is not volume related. First line drug for hypotension starting at 10mcg/kg/min. If the systolic blood pressure is less than 70mmhg, use norepinephrine. Dosage and Administration Mix 800mgs of Dopamine in 250cc of Normal Saline. Titrate as follows. Renal Perfusion: 1-3mcg/kg/min Beta Range: 3-10mcg/kg/min Alpha Range:10-20mcg/kg/min, greater than 20mcg/kg/min switch to Norepinephrine. Adverse Reactions Profound tachycardia may result in the presence of hypovolemia. Always treat the underlying hypovolemia before using Dopamine. May increase both suprventricular and ventricular ectopy. At higher doses myocardial blood flow may be reduced. Special Considerations Use with a volumetric infusion device. Epinephrine First Line ACLS Drug YES! Indications and uses Indications: Improved coronary and cerebral profusion is the primary beneficial effect of epinephrine during cardiac arrest. May also increase automaticity and make VF more susceptible to DC countershock. Uses: Epinephrine is the first drug of choice of all ACLS situations where the patient is pulseless, dead! Dosage and Administration Intermediate dose: Give 1mg IV push every 3-5 minutes, there is no maximum dose. May be given down the endotracheal tube. Mix with 10cc normal saline when giving the E.T. route. Escalating dose: Give 2-5 mg IV every 3-5 min. High dose: Give 0.1 mg/kg IV every 3-5 min. Adverse Reactions May cause worsening of myocardial ischemia and may cause PVC's or Ventricular Tachycardia. May result in undesired tachycardia. Special Considerations ACLS Epinephrine strength is 1:10000 solution for IV. If 1:1000 is all that is available, it must be mixed with 10cc Normal Saline for a final product of 1:10000 solution! Isoproterenol First Line ACLS Drug NO! Indications and uses Indications: Isoproterenol has lost favor with ACLS because of it's potential to worsen myocardial ischemia. In situations where Isoproterenol was used in the past, TCP is the treatment of choice. Uses: Increases pacemaker SA automaticity and AV conduction. Dosage and Administration IV infusion: Titrate 0.5mcg to 5mcg minutes. Adverse Reactions May cause worsening of myocardial ischemia and may cause PVC's or Ventricular Tachycardia. May result in undesired tachycardia. Hypotension from vasodilitation. Special Considerations Transcutanous pacing is now the treatment of choice in place of Isoproterenol. There has been supportive evidence that Isoproterenol may be helpful in Torsades de Point. Lidocaine First Line ACLS Drug YES! Indications and uses Indications: Suppression of Ventricular ectopy, Ventricular Tachycardia, and Ventricular Fibrillation. Uses: Lidocaine is the first line anti-arrhythmic drug of choice. Lidocaine is used to treat PVC's, Ventricular Tachycardia, and Ventricular Fibrillation. Dosage and Administration Give 1-1.5mg/kg IV every 3-5 min. up to a maximum dose of 3mg/kg. In ACLS situations if Lidocaine was used to suppress ventricular arrythmias, always follow with an infusion. Lidocaine can be given down the endotracheal tube. For an infusion mix 2 grams in 500cc Normal Saline Soultion. Infusion rate is 1-4mg/min. Adverse Reactions Lidocaine Toxcity may cause CNS depression, convulsions, coma, hypotension and death. Special Considerations In patients with impaired liver function or patients over 70, give the recommended bolus, but decrease the normal infusion rate by 50% Magnesium Sulfate First Line ACLS Drug YES! Indications and uses Indications: Magnesium sulfate is gaining popularity as an initial treatment in the management of various dysrhythmias, particularly torsades de pointes, and dysrhythmias secondary to a tricyclic antidepressant overdose or digitalis toxicity. The drug is also considered as a class Ila agent (probably helpful) for refractory ventricular fibrillation and ventricular tachycardia after administration of lidocaine or bretylium doses. Uses: Used primarily for the treatment of Torsades de points. Dosage and Administration 1-2 grams IV diluted in 100cc of Normal Saline. Adverse Reactions The following adverse reations have been documented: Diaphoresis, facial flushing, hypotension, depressed reflexes, hypothermia, reduced heart rate, circulatory collapse, and respiratory depression. Special Considerations CNS depressant effects may be enhanced if the patient is taking other CNS depressants. Serious changes in cardiac function may occur with cardiac glycosides. Norepinephrine First Line ACLS Drug YES! Indications and uses Indications: Norepinephrine stimulates alpha-, beta1-, and beta2-adrenergic receptors in dose-related fashion. It is indicated for non volume related hypotension. It is the first pressor of choice if the systolic BP is less than 70mmhg. Dopamine is the first pressor of choice if the systolic BP is between 70 and 90mmhg. Uses: Systolic blood pressure less than 70mmhg, in a non-volume depleted patient. Also used for the treatment of cardiogenic shock. Dosage and Administration Mix 4mg of Norepinephrine in 250cc of Normal Saline. Start at 2mcg/min and titrate up for desired effect. Adverse Reactions May cause worsening of myocardial ischemia and may cause PVC's or Ventricular Tachycardia. May result in undesired tachycardia. Special Considerations Do not use Norepinephrine without correcting the underlying hypovolemia. Norepinephrine should always be used with a volumetric pump. Oxygen First Line ACLS Drug YES! Indications and uses Indications: Oxygen is used in hypoxemia or suspected hypoxemia. Supplemental oxygen raises the blood oxygen saturation, providing better tissue oxygenation. Has been proven to decrease the workload on the myocardium. Uses: Used as one of the first line treatments in all ACLS Situations. Dosage and Administration Stable Patients: Start with Nasal Prongs at 2-4lpm. May increase as needed or change device as needed to meet patient's requirements. Unstable Patients: Start with Simple Mask at 6-8lpm, or situation warrants use nonrebreather mask at 12-15lpm. Dead Patients: Use Bag-valve-mask device with reservoir at 12-15lpm. Use airway adjunct to support ventilation. Intubation is the airway of choice in all dead patients. Adverse Reactions Any time oxygen is initiated be aware of patient's condition. If patient's condition worsens, change to higher delivery device. If at any time the patient's airway or ventilatory status worsens, support with the appropriate airway and Bag-valvemask device with reservoir. Special Considerations Always evaluate your patient's ventilatory status on an on-going basis. Procainamide First Line ACLS Drug NO! Indications and uses Indications: Procainamide suppresses phase-4 depolarization in normal ventricular muscle and Purkinje fibers, reducing the automaticity of ectopic pacemakers. It also suppresses reentry dyrhythmias by slowing intraventricular conduction. Procainamide may be effective in treating PVCs and recurrent ventricular tachycardia that cannot be controlled with lidocaine. Uses: Procainamide is indicated for ventricular dysrhythmias not controlled by Lidocaine. Procainamide is not a first drug of choice for treatment of ventricular dysrhythmias. Dosage and Administration 20 mg/min (30 mg/min for refractory VF): maximum dose is 17 mg/kg Maintenance infusion (after resuscitation from cardiac arrest) is 1-4 mg/min. For infusion, mix 2 grams of Procainamide in 500cc Normal Saline. Adverse Reactions Contraindicated in the following, Second- and third-degree AV block, digitalis toxicity, and Torsades de pointes. Special Considerations End Points to Procainamide administration are, suppression of arrhythmia, hypotension, widening of the QRS greater than 50% of original width, and maximum dose reached. Sodium Bicarbonate First Line ACLS Drug NO! Indications and uses Indications: Routine administration of Sodium Bicarbonate is longer recommended. Hyperventilation is the treatment of choice to correct both metabolic and respiratory acidosis. Uses: Known preexisting bicarbonate-responsive acidosis Intubated patient with continued long arrest interval Upon return of spontaneous circulation after long arrest interval Tricyclic antidepressant overdose Alkalinization for treatment of specific intoxications. Dosage and Administration Give 1 mEq/kg IV, you may repeat with 0.5 mEq/kg q 10 min. Adverse Reactions Metabolic alkalosis, hypoxia, rise in intracellular Pco2 and increased tissue acidosis, electrolyte imbalance (tetany), seizures and tissue sloughing at injection site. Special Considerations Hyperventilation is the treatment of choice to correct both metabolic and respiratory acidosis in a Code Blue situation. Verapamil First Line ACLS Drug YES! Indications and uses Indications: Verapamil is used as an antidysrhythmic and antianginal agent. It works by inhibiting the movement of calcium ions across cell membranes. The slow calcium ion current blocked by verapamil is more important for the activity of the SA and AV nodes than for many other tissues in the heart. By interfering with this current, calcium channel blockers achieve some selectivitv of action. Verapamil decreases atrial automaticity, reduces AV conduction velocity, and prolongs the AV nodal refractory period. In addition, verapamil depresses mvocardial contractility, reduces vascular smooth muscle tone, and dilates coronary arteries in normal and ischemic tissues. Uses: Primarily used in PSVT, Atrial flutter with a rapid ventricular response and Atrial fibrillation with a rapid ventricular response. Dosage and Administration Give 2.5-5.0 mg IV bolus over 2 min; repeat doses of 5-10 mg may be given every 1530 min. Adverse Reactions Hypotension, espcially in hypovolemic patients. Other reactions are, dizziness, headache, nausea and vomiting, bradycardia, complete AV block, and peripheral edema. Special Considerations Give Calcium Chloride as reversal agent for Verapamil.