NWAHS Education & Research Team, Learning Series
advertisement

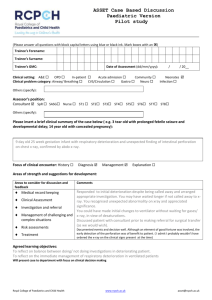
43 NWAHS Education & Research Team, Learning Series: Recognising and Responding to Clinical Deterioration Award category: Best team Contribution for Service Excellence and Leadership Award for Safety and Quality Contact: North West Nursing Midwifery Education Unit THO-NW 03 6430 6668 A pilot educational programme was rolled out across the then North West Area Health Service (NWAHS) from Oct 2011 – Oct 2012 to: • • • • Reduce the incidence of unrecognised clinical deterioration. Provide nurses with an educational program that supports the development of critical-thinking, problemsolving and decision-making skills Provide nurses with the knowledge and skills to develop confidence and competence in managing an acutely unwell/deteriorating patient Provide an educational program which meets the needs of adult learners The programme was designed to provide a comprehensive overview of the common acute clinical issues facing frontline nursing/midwifery, medical and allied health staff. It was intended to assist with the identification of patients who have (or area at risk) of clinical deterioration, and to provide a framework for clinical assessment, management and documentation of these events. The sessions were designed to utilise case-based learning, and intended to be interactive where possible. Nurses/midwives at all levels and from all clinical areas were eligible and encouraged to participate in the Program. Most of the patients who suffer significant adverse events in hospitals and other healthcare facilities (such as cardiac arrest, unplanned admission to ICU and unexpected death) have objective evidence of clinical deterioration within the hours preceding the event (Buist et al. 2004, Hillman et al. 2001). The programme was designed to ‘defrag the hard drive of the nurse/midwife/medico’ by understanding and educating on the importance of the ability of bedside clinicians to appropriately monitor, and assess patients using critical-thinking, problem-solving and decision-making skills. Ultimately, failure to recognise or respond appropriately to patients who deteriorate may result in increased morbidity and/or mortality This was based on a key recommendation of the Australian Commission of Safety and Quality in Health Care is that educational programs should include knowledge of clinical observations, identification of clinical deterioration, communication and clinical skills management (ACSQHC 2010). The programme has been instrumental in patient / client services by • • • • • Apply an analytical and reflective approach to patient assessment Integrate theoretical knowledge to ‘real-life’ clinical problems Communicate and document clinical concerns utilising a structured, systematic process Recognise the key markers of critical illness in patients in a variety of clinical settings Respond to common acute clinical emergencies utilising a priority management approach Clinically, detecting clinical deterioration, recognizing the key markers of clinical concern or critical illness: • • • • • • • • • • • • Using fluid balance charts to detect clinical deterioration Using ‘Early Warning Systems’ to detect ‘sick’ patients ‘Mandatory’ vs. ‘Worried’ MET call criteria Markers of clinical deterioration - looking beyond the obvious Identification of patients at high risk of clinical deterioration Systematic approach to clinical assessment and management —the ABCDE approach The role of the ICU Liaison nurse Post-anaesthetic patients who deteriorate—common causes and management priorities Surgical patients who deteriorate—common causes and management priorities Clinical deterioration in the paediatric patient Clinical deterioration in the obstetric patient The ‘DANGERS’ program—preventing the crash in Rural healthcare facilities. Responding to clinical deterioration – managing common acute conditions • • • • • • • • Communicating clinical concerns—using ISBAR communication tool Managing the patient with low urine output Managing the patient with hypoxia or other evidence of respiratory failure Managing the hypotensive patient Managing the patient with an acutely altered LOC Managing the patient with prolonged or refractory seizures Managing the patient with acute de-compensating arrhythmias Managing the patient on the ward having an AMI