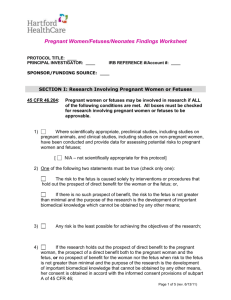
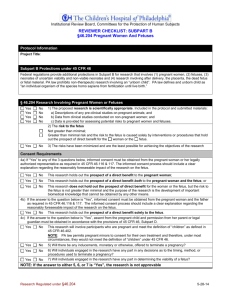
Pregnant Women, Human Fetuses, and Neonates
advertisement

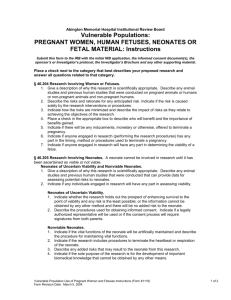
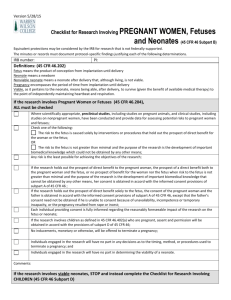
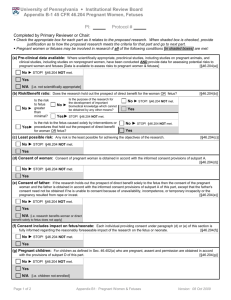
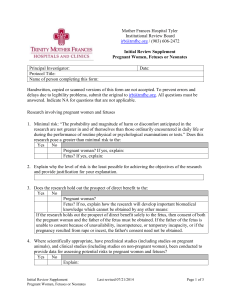
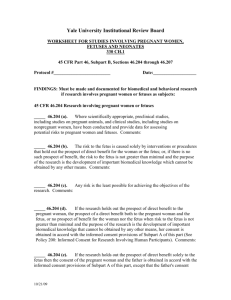
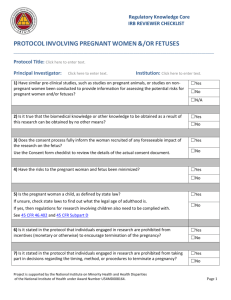
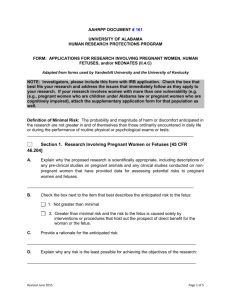
Last Revised: 8/2009 Page 1 of 4 Pregnant Women, Human Fetuses, and Neonates Introduction: The IRB recognizes the additional protections required under Federal law for pregnant women, human fetuses and neonates who participate in research (45 CFR 46, Subpart B). Definitions: Pregnancy encompasses the period of time from implantation until delivery. A woman shall be assumed to be pregnant if she exhibits any of the pertinent presumptive signs of pregnancy, such as missed menses, until the results of a pregnancy test are negative or until delivery (45 CFR 46.202, Subpart B). Fetus means the product of conception from implantation until delivery. (45 CFR 46.202, Subpart B). Neonate means a newborn. (45 CFR 46.202, Subpart B). Policy: A research protocol is considered to include pregnant women, human fetuses, and/or neonates when: any of the above are the target population that will be recruited; or pregnancy occurs during the course of a research study and information about the pregnancy, fetus and/or neonate will be obtained as part of the research study. A) Pregnant women and fetuses In order to approve the inclusion of pregnant women in a research protocol, the following conditions listed in 45 CFR 46.204, Subpart B must be met: Where scientifically appropriate, preclinical studies, including studies on pregnant animals and clinical studies on non-pregnant women, have been conducted and provide data for assessing potential risks to pregnant women and fetuses. The risk to the fetus: o is caused solely by interventions or procedures that hold out the prospect of direct benefit for the woman or the fetus; or, o if there is no prospect of benefit, the risk to the fetus is not greater than minimal and the purpose of the research is the development of important biomedical knowledge which cannot be obtained by any other means. Any risk is the least possible for achieving the objectives of the research. The research must either: o holds out the prospect of direct benefit to the pregnant woman, the prospect of direct benefit for the woman or the fetus; or o no prospect of benefit for the woman nor fetus when risk to the fetus is not greater than minimal and the purpose of the research is the UHCMC IRB Policies and Procedures Last Revised: 8/2009 Page 2 of 4 development of important biomedical knowledge that cannot be obtained by any other means And her consent is obtained in accord with the informed consent provisions of 45 CFR 46 Subpart A. If the research holds out the prospect of direct benefit solely to the fetus, then the consent of the pregnant woman and the father must be obtained in accord with the informed provisions of 45 CFR 46 Subpart A, except that the father’s consent need not be obtained if he is unable to consent because of unavailability, incompetence, or temporary incapacity or the pregnancy resulted in rape or incest. Each individual providing consent is fully informed regarding the reasonably foreseeable impact of the research on the fetus or neonate. For children who are pregnant, assent must be obtained from the pregnant child and consent from her parent or legal guardian. No inducement, monetary or otherwise will be offered to terminate a pregnancy. Individuals engaged in the research will have no part in determining the viability of a neonate. The research protocol must address how these conditions are met and provide sufficient justification for inclusion of pregnant women. If a research protocol proposes to collect information from the pregnant partner of a research subject, the pregnant partner becomes a “research subject” and the provisions under OHRP and FDA regulations, including 45 CFR 46 Subpart B, are applicable. This includes obtaining informed consent from the pregnant partner for participation. B) Neonates The IRB may approve research that involves the following categories of neonates: neonates of uncertain viability, non-viable neonates, viable neonates if all of the following are met (45 CFR 46.205, Subpart B), as well as additional criteria listed for each special population below: Where scientifically appropriate, preclinical and clinical studies have been conducted and provide data for assessing potential risk to neonates. Each individual providing consent is fully informed regarding the reasonably foreseeable impact of the research on the neonate. Individuals engaged in the research will have no part in determining the viability of a neonate. 1) Neonates of uncertain viability A neonate whose viability has not yet been ascertained may only be involved in research if all of the following additional conditions are met: The research holds out the prospect of enhancing the probability of survival of the neonate to the point of viability, and any risk is the least possible for achieving that objective, or UHCMC IRB Policies and Procedures Last Revised: 8/2009 Page 3 of 4 The purpose of the research is the development of important biomedical knowledge which cannot be obtained by other means and there will be no added risk to the neonate resulting from the research; and The legally effective informed consent of either parent of the neonate or, if neither parent is able to consent because of the unavailability, incompetence, or temporary incapacity, the legally effective informed consent of either parent’s legally authorized representative is obtained, except that the consent of the father or his legally authorized representative need not be obtained if the pregnancy resulted from rape or incest. 2) Nonviable neonate After delivery, a neonate that is living but is not considered viable may be involved in research if all of the following additional conditions are met: Vital functions of the neonate will not be artificially maintained. The research will not terminate the heartbeat or respiration of the neonate. There will be no added risk to the neonate resulting from the research. The purpose of the research is the development of important biomedical knowledge that cannot be obtained by other means. The legally effective informed consent of both parents of the neonate must be obtained. If either parent is unable to consent because of unavailability, incompetence, or temporary incapacity, the informed consent of one parent of a nonviable neonate will suffice to meet the requirements except that the consent of the father need not be obtained if the pregnancy resulted from rape or incest. The consent of a legally authorized representative of either or both of the parents of a nonviable neonate will not suffice to meet the requirements. 3) Viable neonates A neonate determined to be able to survive to the point of independently maintaining heartbeat and respiration (“viable”) upon delivery may be included in research to the extent permitted by and in accordance with OHRP (including Subpart D) and FDA requirements C) Additional considerations when the pregnant subject is a minor In addition to the regulations under 45 CFR 46 Subpart B, if the pregnant subject is also a minor, there are additional considerations that must be accounted for under 45 CFR 46 Subpart D, Additional Protections for Children Involved as Research Subjects. Please see IRB policy “Protocol Submission Requirements” and “Assent from Children in Research Studies” for more information. Prior to inclusion of pregnant minors in research, parental permission must be obtained or the IRB must approve a waiver of the requirement for parental permission in accordance with 45 CFR 46.116 or 45 CFR 46.117. UHCMC IRB Policies and Procedures Last Revised: 8/2009 Page 4 of 4 In research protocols that involve pregnancy testing of subjects who are minors, the following is required: If the female age 13 years or younger, positive results of the pregnancy test must be shared with both the child and the parent or legal guardian. In addition, the pregnancy must be reported to the local public children’s service agency (PCSA) per UHCMC reporting requirements (see UHCMC Clinical Policy 1.2 “Child Abuse and Neglect”. This must be documented in the research record. If the female is age 14 years or older, the results of the pregnancy test must be shared with the minor. The results do not automatically have to be shared with the parent or legal guardian unless the parent or legal guardian asks for the results. This must be documented in the research record. If the research study is a clinical trial and wishes to obtain information and/or enroll the minor pregnant partner of a currently enrolled male research subject, the following additional protections are required: o If there is no known risk to the pregnancy as a result the male partner’s participation in the research study, the study staff may ask the male partner to talk to the minor female partner to see if she wishes to participate in the research study with her parents consent. If the female pregnant partner wishes to participate, she and her parent or legal guardian can contact the study staff to discuss participation in more detail. o If there is a known or theoretical risk to the pregnancy as a result of the male partner’s participation in the research study, the male subject should instruct his pregnant partner to contact study staff. The study staff should disclose relevant information about the study, including possible risks to pregnancy and potential follow-up. The pregnant partner should discuss this with her parent or legal guardian, who should then contact the study staff for follow-up. References and/or Regulatory Citations: 45 CFR 46, Subpart B 45 CFR 46.204 45 CFR 46.205 Related Policies: IRB Policy, Assent from Children for Research Studies IRB Policy, Protocol Submission Requirements IRB Policy, Department Review of Protocols IRB Policy, Additional Required Reviews UHCMC Clinical Policies, Administrative Policy and Procedure Manual II, “1.2: Child Abuse and Neglect” UHCMC IRB Policies and Procedures