case discussion
advertisement

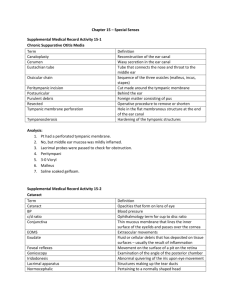
Chapter 5 Inflammation AIMS 1. To grasp basic pathological changes of inflammation and characteristics of acute and chronic inflammation. 2. To be familiar with the sequence of events in inflammation as well as the structural and molecular mechanisms underlying them, and to be familiar with systemic effects of inflammation combining with case discussion. CONTENTS Gross specimen Tissue section Acute severe hepatitis Acute severe hepatitis Amoebic abscess of the liver Epidemic encephalitis B Serous inflammation Skin blister Skin blister Fibrinous inflammation Diphtheria Diphtheria Bacillary desentery Bacillary desentery Fibrinous pericarditis Fibrinous pericarditis Alterative inflammation Exudative inflammation Lobar pneumonia Purulent inflammation Suppurative appendicitis Phlegmonous appendicitis Suppurative meningitis Suppurative meningitis Abscess of the liver Abscess of the liver Abscess of the lung Abscess of the lung Abscess of the kidney Abscess of the kidney Abscess of the brain Abscess of the myocardium Abscess of the cerebellum Organization of abscess Phlegmonous inflammation of the skin Proliferative inflammation Non-specific inflammation Chronic cholecystitis Chronic cholecystitis Granulomatous inflammation Tuberculosis of the lung Tuberculosis of the lung Foreign body granuloma 78 Inflammatory polyp Inflammatory polyp of the intestine Inflammatory polyp of the intestine KEY POINTS OF SPECIMEN OBSERVATION 1. Alterative inflammation Basic pathologic changes (1) Gross morphology ◆ Organ presents swollen caused by cell degeneration; or a reduction in volume owing to massive cellular necrosis. ◆ The specimen presents necrosis, such as coagulative necrosis, liquefactive necrosis or gangrene. (2) Histopathology ◆ Parenchyma cell presents degeneration and/or necrosis, such as hydropic degeneration, fatty degeneration, coagulative necrosis, and liquefactive necrosis ◆ Mesenchyma cell appears mucoid degeneration or fibrinoid necrosis. ◆ Vessel dilate and inflammatory cell infiltrate. Specimen observation (ⅰ) Acute severe viral hepatitis Case abstract: Male, 45 years old, he suffered fatigue, severe vomit and abdominal turgor 3 days before, 1 day later he rapidly progressed into anuresis, delirium, marked confusion and stupor to deep coma. Laboratory examination: electrolyte and acid-base disturbances, apparently elevated blood ammaonia levels, raising blood urea nitrogen and creatinine concentration. He died of haematemesis and coma. Gross specimen: (Fig.5-01) The liver shrinks and is transformed into a limp, red organ covered by a wrinkled, too-large capsule. On cut surface, necrotic areas have a muddy red, mushy appearance with blotchy bile staining. Tissue section: (Fig.5-02a, b)Complete destruction of hepatocytes in contiguous lobules leaves only a collapsed reticulin framework and preserved portal tracts. Question: Which basic pathologic changes of inflammation are reflected in this 79 lesion? (ⅱ) Amoebic abscess of the liver Gross specimen: (Fig.5-03) On the cut surface of the liver, there is a solitary discrete abscess, 6 cm in diameter. The cavity is filled with some pasty material likened to anchovy paste, and has a shaggy fibrin lining. Question: Why does amebic abscess of liver belong to alterative inflammation not purulent inflammation? (ⅲ) Epidemic encephalitis B Case abstract: Female, 4 years old. She suffered from outburst of hyperpyrexia, twitch, and coma and was dead. Tissue section: (Fig.5-04a,b,c) What pathologic changes happen in brain tissue? Which one is dominant? Question: Why does it belong to alterative inflammation? 2. Exudative inflammation Basic pathologic changes (1) Gross morphology ◆ Serous inflammation: Focally inflammatory edema, or hydrops in body cavity. ◆ Fibrinous inflammation: Grayish-white membranous material, pseudomembrane, appears on the surface of inflamed tissues of the organ (e.g. fibrinous pleurisy); and Cor Villosum (e.g. fibrinous pericarditis) appears in inflamed pericardium. It also leads to consolidation in lung. ◆ Purulent inflammation: It shows the production of green-yellow, turbid pus, consisting of neutrophils, infecting organisms and liquefactive necrosis. Abscess or empyema or phlegmonous inflammation could be seen.. (2) Histopathology ◆ Blood vessels dilate. ◆ Serous inflammation: Abundant pink protein-rich fluid exudates with relatively 80 low cellular content and inflammatory cells. ◆ Fibrinous inflammation: Plentiful fibrinogen containing inflammatory exudates precipitate to form a tangled threadlike network or sometimes to form as an amorphous coagulum. ◆ Purulent inflammation: The exudates are composed of large amounts of neutrophils and pus cells, necrotic tissues, and edema fluid. Specimen observation (ⅰ) Skin blister Gross specimen: (Fig.5-05) Blisters are filled with serous effusion and scattered over skin surface. Tissue section: (Fig.5-06) Cross-section of a skin blister shows the epidermis separated from the dermis by a focal collection of serous effusion, few cells and fibrin. Question: In which diseases could this pathological change be presented? (ⅱ) Diphtheria Gross specimen: (Fig.5-07a, b)Dissections performed on larynx, bronchus and trachea all reveal a rough congested mucosa covered by a layer of grayish-white pseudomembrane. Such membrane adheres tightly on epiglottic and laryngeal regions; while, it is loosely connected with the sub-mucosa of trachea and bronchus. Tissue section: (Fig.5-08a,b)Mucosal pseudomembrane is composed of fibrin, damaged mucosa and neutrophils. Question: What is pseudomembranous inflammation? What is the difference between the sequel of laryngeal and tracheal diphtheria lesions? (ⅲ) Bacillary dysentery Case abstract: Male, 12 years old. 1 day ago, he ate raw seafood, today complained of abdominal pain and cramping, diarrhea and tenesmus. Stool examination: loose stools contain blood, pus and mucus. Gross specimen: (Fig.5-09a, b) (a)This is a pseudomembranous enterocolitis that 81 takes place on the mucosa. The mucosal surface of the colon seen is hyperemic and is partially covered by whitish-yellow exudates. (b) Bran-like substances surface the colon mucosal folds, and some fuse into pieces to form grayish-white pseudomembrane. Mucosa appears thickened due to edema. Tissue section: (Fig.5-10a, b) Necrosis of colon’s mucosal superficial layer directed the development of pseudomembrane, a product that constitutes the mixture of abundant fibrin, mucus, injured tissue, neutrophils, RBC and bacilli. Furthermore, surrounding mucosa and submucosa become congested and edematous due to neutrophile and macrophage infiltration. (ⅳ) Fibrinous pericarditis Gross specimen: (Fig.5-11a, b, c) (a) Fibrinous exudates are found on the heart surface. Fine villose form a heavy shaggy coat on the pericardium, results in the “cor villosum.” The heart is characterized by a rough, ragged appearance and is also known as the “shaggy heart”. (b) The pericardial cavity has been opened to reveal a fibrinous pericarditis with strands of stringy pale fibrin between visceral and parietal pericardium. (c) The epicardial surface of the heart shows a shaggy fibrinous exudate. This appearance has often been called a "bread and butter" pericarditis. Tissue section: (Fig.5-12a, b, c) Microscopically, the fibrinous exudates are seen to consist of pink strands of fibrin jutting from the pericardial surface at the upper right. Below this, there are a few scattered inflammatory cells. (d) High-power of a fibrinous pericarditis with a pink meshwork of fibrin exudates, and the fibrinous exudates are organized by granulation tissue. Question: How does the cor villosum formed?Which diseases can contribute to cor villosum?What manifestations could be caused clinically? What are the sequels? (ⅴ) Lobar pneumonia(see also respiratory system diseases) (ⅵ) Suppurative appendicitis Case abstract: Male, 35 years old, he complained of mild fever, nause, and vomit, and pain, at first periumbilical but then localizing to the right lower quandrant. 82 Physical examination: abdomianl tenderness, particularly in the region of the appendix. WBC: 20×109/L. Gross specimen: (Fig.5-13a, b, c) (a) Seen here is acute appendicitis with yellow-white to tan exudates and hyperemia, including the periappendiceal fat superiorly, rather than a smooth, glistening pale tan serosa surface. The appendix is swollen. (b) The appendix has been sectioned in half. The serosa surface at the left shows yellow exudates. The cut surface at the right demonstrates yellowish-tan mucosal exudation with a hyperemic border. (c) Note the perforation of the appendix. (ⅶ) Phlegmonous appendicitis Tissue section: (Fig.5-14a, b, c) (a) Microscopically, the mucosa shows ulceration and undermining by an extensive neutrophilic exudate. (b)The appendiceal lumen is filled with pink-stained pus, consisting of living and degenerated neutrophil polymorphs with liquefied tissue debris. The appendiceal wall is thickened due to a large number of neutrophils and is noticeably congested, edematous. (c) Neutrophils extend into and through the wall of the appendix. Question: What are the clinical manifestations and complications caused by this lesion? (ⅷ) Suppurative meningitis Case abstract: Female, 6 years old. 2 days ago she suffered from headache and vomiting, suffered coma and was dead. Physical examination: T 40 ℃ , unconsciousness and neck stiffness. WBC: 22.5×109/L, N: 0.80. CSF: cloudy, increased pressure with as many as 3.5×109/L WBC, a raised protein level, and a markedly reduced glucose content. Gross specimen: (Fig.5-15a, b) A deposition of viscid, cream-colored suppurative exudates sits in sub-arachnoid space, especially of the frontal, parietal and occipital lobes. In severe parts, the exudate obscures the sulci and gyri. Blood vessels on the cerebral surface are dilated. Tissue section: (Fig.5-16a, b) Low power view showing inflammatory exudates 83 in the widen subarachnoid space at the depth of a sulcus. The exudates are composed of plenty of neutrophils, pus cells, a few monocytes and fibrin. The meningeal blood vessels are engorged extensively. (b) High magnification shows neutrophils and fibrin. Question:Which type of purulent inflammation does this specimen belong to?What are the clinical manifestations and symptoms caused by this lesion? (ⅸ) Abscess of the liver Gross specimen: (Fig.5-17) On cut surface of the liver, there is a abscess 6cm in diameter, the center has whitish-yellow pus formation accompanied by local liver necrosis, and is walled off by proliferated grayish-white fibrous tissue. Tissue section: (Fig.5-18) The left part is the abscess infiltrated by large amounts of neutrophils, some of them undergo degeneration and necrosis. The right part portal cord could be seen. (ⅹ) Abscess of the lung Gross specimen: (Fig.5-19a, b) The abscess is round shaped and about 3 cm in diameter. The cavity of the abscess in the lower lobe of left lung is filled with pus; it has a coarse inner surface and is surrounded by fibrous tissues, which formed a thin suppurative wall. Some suppurative exudates attach to the pleura on the surface of the abscess. (b) There are rounded abscess cavities formations in the upper and lower lobes; the purulent material inside has drained out. Tissue section: (Fig.5-20) This more focal abscess contains a neutrophilic exudate as well as dark blue bacterial colonies, losing the normal alveolar structure. Question:What is the difference between early and late stage of abscess wall? (ⅹⅰ) Abscess of the kidney Gross specimen: (Fig.5-21) In the lower pole of the kidney is a 1 cm pale yellow abscess. Infections can reach the kidney either by ascending up the urinary tract (from a bladder infection, for example) or by hematogenous spread with sepsis. This lone 84 abscess was probably hematogenous in origin. Tissue section: (Fig.5-22a, b) Focal renal tissues are necrotic, and a large quantity of necrotic neutrophils accumulates. Renal mesenchyma engorgement and edema take place peripherally to the abscess. (ⅹⅱ) Abscess of the brain Gross specimen: (Fig.5-23) On the cut surface of the brain, there is a round abscess 2.5cm in diameter situated in the occipital lobe, and it is filled with some yellowish-white pus. The abscess is demarcated by thick fibrous wall. (ⅹⅲ) Abscess of the cerebellum Gross specimen: (Fig.5-24) Please describe by yourself. (ⅹⅳ)Abscess of myocardium Tissue section: (Fig.5-25) Seen here is a micro-abscess in the myocardium. There are localized collections of neutrophils in alveolar cavity. The irregular dark purple center is a collection of bacteria that are the cause for this abscess. (ⅹⅴ)Organization of abscess Tissue section: (Fig.5-26a, b) (a) The wall of an abscess that is organizing has granulation tissue, seen here at the left. The purulent exudate with some hemorrhage is seen at the right in the abscess center. (b) The abscess has a mixture of inflammatory cells, but the wall of the abscess is "organizing" with ingrowth of capillaries and fibroblasts (granulation tissue). (ⅹⅴⅰ) Phlegmonous inflammation of the skin Gross specimen: (Fig.5-27) Epidermis exfoliated with whitish-yellow purulent exudates is present in the subcutaneous tissue. The lesion appears diffused with unclear boundary and the dermis is clearly thickened. 85 Question:Which tissue or organ does this lesion usually happen?What is the difference between phlegmonous inflammation and abscess? 3. Proliferative inflammation Basic pathologic changes (1) Gross morphology ◆ The commonest appearance of non-specific proliferative inflammation are thickening of the wall of a hollow viscus and fibrosis. Inflammatory polyp or inflammatory pseudotumor sometimes could be seen. ◆ Granulomatous inflammation appears well-circumscribed tuberculous focus formation. (2) Histopathology ◆ The commonest features of non-specific proliferative inflammation are : ① Infiltration of lymphocytes, mononuclear and plasma cells; ② Proliferation of vascular endothelial cells, fibroblasts and parenchyma cells; ③ Connective tissue replacement of damaged tissue, accomplished by proliferation of small blood vessels and fibrosis. ◆ The commonest feature of granulomatous inflammation is granuloma formation, it consists of a microscopic aggregation of macrophages that are transformed into epithelium-like cells surrounded by a collar of mononuclear leukocytes, principally lymphocytes and occasionally plasma cells. The foreign material or necrosis can be identified in the center of the granuloma. Specimen observation (ⅰ) Chronic cholecystitis Gross specimen: (Fig.5-28) The gallbladder mucosa is coarse and the wall is thickened by fibrous tissue. Tissue section: (Fig.5-29) Please describe by yourself. (ⅱ) Pulmonary miliary tuberculosis (see also chapter 15) Gross specimen: (Fig.5-30) There are a multitude of small, round, slightly protruded, 86 tan granulomas, about 2 to 4 mm in size, scattered throughout the lung parenchyma. Tissue section: (Fig.5-31a, b, c) The tuberculous granuloma (tubercle) shows an area of central caseous necrosis, plenty of epithelioid cells, Langhans-type giant cells and lymphocytes. The caseous necrotic focus appears as pink, amorphous granular debris, loss of all cellular detail. (d) The epithelioid cells have a pale pink granular cytoplasm with indistinct cell boundaries; nuclei tend to be long and stringy. Epithelioid cells fuse to form Langhans giant cells containing 20 or more small nuclei arranged either peripherally (Langhans-type giant cell) or haphazardly (foreign body type giant cell). (ⅲ) Foreign body granuloma Tissue section: (Fig.5-32) Two foreign body giant cells are seen just to the right of center where there is a bluish strand of suture material from a previous operation, and there are also macrophages, fibroblasts. Question: Morphologically what is the difference of foreign body giant cell and Langhans-type giant cell? (ⅳ) Inflammatory polyp of intestine Gross specimen: (Fig.5-33) Smooth mass of tissue (polyp) with stalks protrudes outwards from the surface of intestinal mucosa. Tissue section: (Fig.5-34) Mucosal epithelium, gland and granulation proliferate, and there are lymphocyte and plasma cell infiltration. Question:Please describe the process of polyp formation. What kind of inflammation does it belong to? CASE DISCUSSION 87 Clinical case Case abstract. A forty-year old male suffered from furuncle of the neck,the patient experienced localized redness, swelling, pain and heat. Ten days later, local redness and swelling expanded to the size of a palm and body temperature measured to be 38℃. Surgical procedures (dissection and drainage) were performed on the swelling furuncle, later that night the patient felt shivery, fever and headache. On the following day, physical examination showed mild jaundice, swelling of the liver and the spleen, WBC 21×109/L and body temperature was 39℃. Discussion To make a pathologic diagnosis of the case and to explain the above clinical manifestations using learned knowledge on acute inflammation. Autopsy case Case abstract. Female, 62 year-old, was admitted to the hospital for emergency care of fever and upper abdominal pain that lasted for 3 days. Current Case abstract. Two days ago, the patient experienced upper abdominal pain and a fever of 38.8℃. Anti-inflammation treatment received at a local hospital turned out to be inadequate. On the third day, the patient was inhospitalized due to the deterioration of above mentioned symptoms, multiple vomits, and listlessness. Past Case abstract. Diabetes for 7 years, gallstones for 2 years. Physical examination. The patient behaved apathetically,body temperature was 38.2℃ and BP12.0/8.0kpa. Mild jaundice of the sclera and peripheral regions of the skin, swollen lymph nodes of the neck, clear auscultation of the lung bilaterally, heart rate 120/min,weak heart sound,sub-xiphoid and upper right abdominal pain(+),and unsatisfactory palpation of the liver and spleen. Laboratory diagnosis. WBC 28.4×109/L,bacillary nucleus 9%,polymorphic nucleus80%. Hepatic-splenic ultrasound:enlarged liver and spleen, dilation of intra-hepatic bile ducts, gallstone formed. Clinical diagnosis. ① Acute cholecystitis, 88 cholethiasis ? ② Suppurative cholangitis?③Septicemia,inflammatory shock?④TypeⅡdiabetes. Treatment. Alimentary decompression, anti-inflammation and anti-shock were performed. Treatments were ineffective and the patient died 2 days later. Autopsy records Skin:Mild jaundice. Lymph node:Lymph nodes of the neck and groin are swollen. Heart:270g.Tissue slice:Myocardial cells are degenerated and necrosis. Liver: 1800g. Increased in size,the edges are obtunded, cut edge turned inside out, its color became pale and cloudy. Bile duct dilated, whitish-yellow pus accumulated in the cavity. Spleen: 220g. Capsule ruffled with soft sensation. Under light microscope: macrophage proliferated, sinal endothelial cells are swollen and exfoliated, and macrophages and a few neutrophils are present inside the splenic sinus. Kidney: 185g. Increased in size, cut face protruded, cut edge turned inside out, the color became pale and cloudy (Fig.5-35). Light microscope: (Fig.5-36) what pathological changes can be seen microscopically? Please describe by yourself. Discussion 1. What lesions are there in this case according to autopsy specimens and tissue slides? What correlation is there among these lesions? 2. To analyze the correlation of lesions and clinical manifestations. 3. To analyze the cause of death in the patient. PRACTICE REPORT 1. Illustrate the histological morphology of ① Fibrinous pericarditis; ② Myocardium abscess. 2. Describe the pathologic characteristics of phlegmonous inflammation. 3. Write out the outline of case discussions. 89 QUESTIONS FOR REVIEW 1. How to diagnose inflammation pathologic morphologically? 2. What characteristics posed by all exudative inflammations have in common under light microscope? What are the differences in clinical symptoms among different types of exudative inflammations? 3. Compare the following pairs based on the morphology and sequel of lesions (1) Fibrinous inflammation in mucosa versus in serosa. (2) Abscess versus phlegmonous inflammation. (3) Acute inflammation versus chronic inflammation. (China Medical University Han Yuchen, Qiu Xueshan) 90