FUNDAMENTALS INDEX
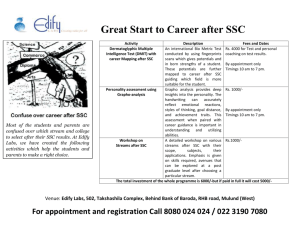
advertisement

The Financial Advisor Guide to Employee Benefits Self-Study Course # 3 EMPLOYEE BENEFIT PLANS AN OVERVIEW OF HOW EMPLOYEE BENEFITS ARE CHANGING In 2011, more than $200 billion was spent for health care in Canada with approximately 70 per cent of the costs paid for by the federal and provincial governments’ publicly funded system. Canadian employers pay for most of the remaining 30 per cent of non-essential medical and dental expenses, according to the Canadian Institute for Health Information and Statistics Canada. While employer medical and dental plans were originally designed to be supplementary to the publicly funded government plan, as a result of the federal and provincial cut backs in healthcare services employers and private insurers across this country have had to alter and redesign their medical and dental plans to keep up with emerging trends of higher claims and new cost realities. In an age where publicly covered services continue to be reduced, we are likely to see corporations in Canada share continue to increase in the coming years. In the midst of these economic pressures on the current healthcare system, employees are demanding better company medical and dental benefit plans. While the traditional corporate employee medical and dental benefit plans in Canada provide coverage for semi-private hospital rooms, prescription drugs, dental, chiropractors, physiotherapists, vision care, extended health coverage and travel medical insurance, employees are asking for more options than ever before. Opinions on what to add are largely influenced by age and experience - items like teeth whitening can compete with orthotics. Older employees want expanded drug coverage, while younger workers are concerned about their deductibles. The end result is employees want choice and employers want/need to contain their costs. 2 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 The vast majority of Canadian small and mid-sized businesses offer medical and dental benefits to their workforces by utilizing insurance carriers. With the consolidation frenzy of the last decade, the number of insurance carriers has dwindled in an effort to make the Canadian players more globally competitive. This new, streamlined landscape has been good for the carriers, but not for the small and medium sized Canadian business, which have been underserved by the carriers focused on delivering shareholder value with big premium clients which are $500,000 or more in annual premiums. The increasing pressures on the current healthcare system, the consolidation of the insurance industry and the growing employee demand for more flexible and expanded coverage is having the greatest impact on the small and medium-sized Canadian business. With health and dental care costs escalating by approximately 15% for health and 7% for dental. Small and medium sized employers are facing uncontrollable and unpredictable costs to their businesses to provide these benefits. Employers have tried to curtail these costs by introducing annual limits, co-insurance, deductibles and exclusions to their medical and dental plans. Throughout this course, we will take a look at the flexibility of different Employee Benefit Plans, as well as how the Government Plans complement or sometimes integrate into Corporate Employee Benefit Programs to provide a comprehensive and wide ranging support system for employers and employees in Canada. We will study such Employee Benefits as Life & Accidental Death & Dismemberment, Health, Dental, Short Term Disability (Weekly Indemnity), Long Term Disability (LTD), Employee Assistance, Group Critical Illness and Best Doctors. We will also cover Health Spending Accounts, Health & Welfare Trusts, Cost Plus, Administrative Services Only (ASO), and Individual Health & Dental plans. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 3 On the Government side of benefits, we will look at the various programs that are available. AN INTRODUCTION TO EMPLOYEE BENEFITS Canadians and Health Insurance The vast majority of Canadians and their dependents are protected by one or more of the health and life insurance industry’s products and services. In 2010, 23.1 million Canadians had extended health care coverage, 12.9 million had dental coverage, and 10.5 were covered by disability insurance. In 2010 Canadians paid 28.5 billion in premiums on new and existing health insurance policies and received 22.4 billion in payments from health benefit programs. Insured health benefit plans played an essential role in providing protection against financial loss for millions of Canadians The Aging and Health Insurance The senior population (adults 65 and up) is the fastest growing population group in Canada. In 2011, 4,981.200 Canadians were 65 years old or older. This is more than double the Canadian senior population in 1981 (2,361,000). The senior population in Canada is expected to reach 5.9 million in 2016, 6.7 million in 2021 and 9.2 million in 2041. As Canadians are living longer, we will have long-term health care needs Health insurance responds to these needs, without threatening personal savings, assets and financial security Health insurance provides the flexibility to deal with individual needs as they arise 4 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Even though Group Insurance benefits (also known as Employee Benefits) have been in existence since 1920, there have been substantial gains, to the point where today they are more significant than individual insurance. Employee Benefits do however, have limitations that make it clear that it is to be regarded as an add on and not to be relied on as the main foundation of any individual’s financial security. Many businesses, industries and associations are concerned with holding on to their employees. Although Employee Benefits can be considered an expense to many companies, the employees look at it as a fringe benefit. In this day and age where job vacancies are very competitive, many applicants want to find out more about benefits before they accept a position with the company. Although a Company does not have to be incorporated to have Employee Benefits, there are many benefits of incorporating a business for the opportunity to obtain tax advantaged employee benefits. The benefits provided could cover the many formats of Employee Benefits to plans that provide individual retirement accounts or traditional Registered Pension Plans and a host of other plans. Corporate and Government Benefits can cover the following areas: Health Benefits Disability Benefits Retirement Benefits For the purpose of this course, we will only deal with the first two. Description of Employee Benefit Plans Employee Benefits are plans whereby the employees of a firm may be insured as a group under one contract, with the insurance being payable for the benefit of persons other than the employer. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 5 By issuing insurance in this way, it is possible to insure employees at a low net cost and also extend the benefit of insurance to many employees who, because of age, physical condition, occupation or cost, would not be able to secure individual policies. Approximately 50% of all Canadian workers are covered by Employee Benefit programs. THE TRADITIONAL SOURCES OF BENEFIT GROUPS ARE: Employer Groups The Employer groups are the main source of groups and the Employer/Employee Group Benefits are the most stable in the industry. There could be one company or family of companies with the Master Contract being issued to the Employer or Head Office that would cover all the employees in the firm. Trade Associations Group Benefits provided for Trade Associations are based on the fact that while they may have many different employers, all the employees are engaged in similar occupations such as building supply companies or automobile dealerships. Professional Associations Groups of Professionals like Doctors, Dentists, Lawyers etc. who are often too small to purchase Employee Benefits individually by office, but when banded together with other professional offices constitute a very large group. Unions (Health and Welfare Benefits) Unions often provide Group Benefits for their “actively at work” members who may work for many different employers or group of employers. As long as the member is working, the Union Benefits are funded by a system known as “Bank Hours” meaning a contribution (pennies per hour) paid for by the employer. When the employee is laid off, the surplus in their “Bank” will carry their health benefits for an indeterminate length of time. 6 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Many Insurance carriers break these groups down into size bands: Large Group - 200 to 20,000 lives plus. Standard Group - 25 to 200 lives plus, Small Groups - 3 – 25 lives. Medical evidence is usually required for any group of 10 lives or under. WHAT ARE THE ADVANTAGES OF EMPLOYEE BENEFIT PLANS? Employer Employers can pay a substantial amount of the cost. Employer premiums are tax deductible. Attracts and helps to maintain valuable employees, therefore reduces the high cost of turnover. Can be used to meet the competition when looking at employees who already have Employee Benefits. Provides the employer with a sense of moral obligation when dealing with families of deceased or disabled employees. Provides employees with a sense of security, therefore loyalty and productivity are increased. Employee Benefits plans are flexible when it comes to implementing, administration and changes in personnel. An unincorporated owner of a business can be included for coverage, even though these premiums would not be deductible. Employee No evidence of health is required, depending on the size of the company insured. Employers paid premiums are not a taxable benefit. There is an added amount of financial security in the event of death, disability, and out of country expenses for the employees and their dependents. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 7 Employees have the right to convert the Life Benefit to a private insurance plan. On termination, the Group Life remains in force for 31 days without charge. Group Contracts do not contain a suicide clause. FUNDAMENTAL PRINCIPLES OF EMPLOYEE BENEFITS Employee Benefits exist for the benefit of the complete group and therefore the individual member is not required to submit medical information, depending on size of the insured company. There are five fundamental principles of Employee Benefits, which are required: 1. The employee must be actively at work If the employee is on disability leave, their coverage will not be effective until they return to work. This guarantees the principles that all employees can be insured. 2. Non-discriminatory Insurance Schedule No one employee can pick or choose the type or size of their individual coverage. The Master Contract exists between the employer and the Insurance Company and details with the type and amount of coverage. The only choice that the employee has, if membership is not a condition of employment, is whether to join or not. There generally is a waiting period of between 30 and 90 days. 3. Deductions at source Employee’s contributions are source deducted and then combined with the employer’s share so that one cheque is remitted. 8 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 4. Mandatory Employer Contribution Usually the employer will pay one half of the premium billed each month, but sometimes they may pay a larger percentage. If they pay 100%, this is known as a Non-contributor Plan. 5. Spreading the Risk To ensure that the risk is spread over the entire employee group, each group size has a minimum enrolment. Small plans with 10 lives or less may demand 100% participation and may request a health statement. A medium size plan of 50 employees or more might require 85% and a large plan would require 75% participation. WHAT ARE THE FACTORS THAT DRIVE THE PREMIUM FOR AN EMPLOYEE BENEFIT PLAN? 1. Premium Rates Premium Rates are set based on number of employees, age, sex and amount of insurance. The price is charged at a monthly rate per thousand of coverage (i.e. .18 per $1000 of coverage). All members therefore will pay the same amount per month regardless of age or sex. The premium required may also have been adjusted in part to claim experience or occupations that are more hazardous as well as gender bias. The premiums are generally adjusted each year according to experience. If the policy is participating, the adjustment may be in the form of a dividend and in a non-participating policy will take the form of an increase or decrease in rate. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 9 2. Experience Basis At the Anniversary of the plan, the past years claims are compared to the amount of premium charged. This is known as “the experience” and the plan is experience rated. The Insurer will wish to retain a small percentage of the premium charged i.e. 26%, and therefore if claims were higher that 74%, the premiums will be increased so as to guarantee next year’s percentage. At the same time, anticipated increased costs from health care providers are factored into the renewal premium. This anticipated cost is known as “Trend or Inflation”. 3. Pooled Basis It is common practice for a carrier to place all their small group cases in a common “pool”. Premiums and claims are accounted on a pooled basis and the rates rise or fall based on the claims vs. the premiums paid. It is not unusual for larger groups to have the Life Insurance, AD & D and LTD benefits also pooled. In this way, one large claim will not adversely affect next year’s rates. 4. Retention Basis The insurer may on the other hand indicate how much they wish to retain at the start of the year. This is used for administrative costs, commissions, taxes and reserves. The claims will be the unknown factor. The refund or reduction of rate will depend on the claims and retention costs. In effect, this transfers the risk element to the employer. Retention Basis is generally used for larger groups. 5. Target-loss Ratio The ratio of the expected amount of claims divided by the anticipated premiums for the next year gives the Insurance Company their profit margins. It is even more of a concern to the employer, as this figure drives their premium. 10 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 6. Inflation The increase in the cost of the expenses the Insurance Company covers on a group plan, such as the rising cost of prescriptions. 7. Utilization This represents how often an insured certificate holder has used any benefit of the plan. The number of claims per year per certificate usually measures utilization. Inflation and utilization are blended to provide an average figure. 8. Natural Aging This is the portion of a rate increase that results simply because each certificate holder has aged by one year since the last renewal. 9. Composition Change The change in rates caused by actually insuring different employees. The variables, which affect the change, are age, sex, dependent status and earnings of the employee. For example, a single male age 22 and earning $28,000 replacing a married female, aged 53 and earning $48,000 will have a downward effect on the group rates. BENEFITS THAT THE INSURED EMPLOYEE OR THEIR DEPENDANTS CAN USE AT SOME POINT IN THEIR LIVES Life insurance Benefit schedules must not discriminate between employees but a different schedule can apply to any different class of employees. The three main factors that affect the amount of insurance are: Earnings Level Position, or Flat Amount Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 11 Often the life insurance can be 1, 2 or 3 times earnings. The contract will usually contain a non-evidence limit and a maximum amount that the Insurance Company will issue as well as a minimum amount e.g. 10,000 minimum – 250,000 maximum. A description of the terms from this section of the Master Contract: Annual Salary Refers to the Schedule of Benefits with respect to each Insured Employee, the regular annual fixed gross remuneration or its annual equivalent they receive from the Policyowner, but will not include, overtime pay, commissions, overrides, bonuses, allowances, dividends or any form of remuneration which is not predetermined. Basic Benefit This is the amount of Basic Life as indicated on the Schedule of Benefits for the Employee Life Insurance Benefit. Death Benefit The Employee Life Insurance Benefit will be the Basic Benefit. Upon suitable proof of death of the Insured Employee, the Company will pay the amount of Employee Life Insurance to the named beneficiary. If no beneficiary is designated, or if the beneficiary predeceased the Insured Employee the death benefit will be payable to the estate of the Insured Employee. Conversion The employee, by law, has the right to convert without evidence of insurability, their Group Life Benefit within the following parameters: Application must be made and premium paid within 31 days of termination of contract or employment. 12 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Conversion may be to any plan offered by the Carrier including Term Insurance, Whole Life or other regular plan or it may be a special “conversion” contract. The employee cannot convert an amount in excess of the level of coverage they enjoyed under the plan. Premium is based on their attained age. Conversion Notes Full Life coverage is continued for 31 days, without charge after termination of employment or at termination of the entire contract. The Converted Policy will be dated 31 days from termination. If the Contract is terminated or replaced, it usually stipulates: All employees who have been insured five years or more may convert up to a predetermined amount, minus and amount for which the employee will become eligible under any group policy being issued or reinstated within 31 days after the date of termination. Beneficiary Designation The same beneficiary designations apply to Group Life Benefits as to individual contracts. An irrevocable beneficiary can be designated on the Group Life Benefit. Survivor Benefits The Contract may contain a benefit that is equal to 25% of the deceased employee’s salary plus an extra percentage for each dependent child. Remarriage generally will eliminate the benefit. Taxation The employer’s contributions are an expense deduction and the employee receives them as a taxable benefit. The employee cannot deduct this contribution. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 13 Waiver of Premium and Disability In the event of a total disability, before retirement, the group life premiums will be waived. They will Re-commence upon recovery. Some contracts include a benefit whereby the premiums are waived and the face amount is paid out in equal annual installments over a period i.e. five years. In the event of recovery, the installments paid will reduce the amount of the Group Life Benefit. Extension of Life Benefits in Retirement The cost of the full life benefit would be prohibitive if carried from date of retirement until death, so, if offered, the coverage may be modified in any of a couple of ways: 1. Benefit continued at a reduced 50% level with a maximum amount e.g. 10,000. Premium maybe required from the retired employee. The employer may pay the premium or a single premium. 2. Continue the coverage with an annually reducing benefit for the first five years of retirement. Variation of this method would leave a residual benefit of $2000 for life. GROUP INSURANCE PRODUCTS Creditor Group Many feel that, even at a low price, loan repayment insurance is an unnecessary addition to their monthly loan payment. The "it could never happen to me" attitude is understandable when your health is good and you're in the prime of your life, but the statistics on death and disability add a different perspective. Some Interesting Creditor Insurance Statistics: Over 6,000,000 Canadians a year will suffer an accidental injury Accidents are the leading cause of death for Canadians 45 years of age and under 14 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 One in four Canadians between 25 and 45 years will be disabled for at least 90 days Canadian insurers pay disability benefits under loan insurance plans in excess of $230 million per year Often overlooked, creditor insurance is one of your most convenient and sensible insurance options. It can allow you to protect your family and dependents from the worry of handling debt, if your income were not available to make the payments. For example, mortgage life insurance offers a very straightforward but valuable benefit. If you are insured, your mortgage will be paid off for you (up to a set amount) when you pass away. This means that you never have to worry that your family will be burdened with your mortgage in the event of such a tragedy. Insurance is provided for each borrower of funds on a group basis, up to a certain maximum. The premium charged is a flat rate per $100 borrowed on outstanding indebtedness. Creditor Insurance Limitations In addition to the other hazards involved with replacing of life insurance contracts, the following hazards, risks and uncertainties are added when individual life insurance is replaced with group creditor insurance: Group creditor insurance coverage normally decreases as you pay off the loan or mortgage but the premiums you have to pay often remain the same or even increase over time. Normally you cannot continue with the same group creditor insurance coverage if you decide to re-finance the mortgage or the loan with another lender. If your health or insurability deteriorates it may not be as easy to shop the market for the best loan rate and to keep the insurance, you run the risk of your lender getting this information and this, in turn, may affect your ability to renew or continue with the loan itself. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 15 If the policy expires before you do...they profit. If you expire while the policy is still in force, the institution is usually the beneficiary. You will rarely, if ever, get a fair opportunity to fully examine the policy contract. (Normally all you receive is a single certificate, which is subject to the Master Policy, which, of course, you do not normally get). You have less regulatory protection since the regulators rarely, if ever, require that the creditor complete a comparison disclosure form when they replace individual insurance with their group creditor insurance. The fact of the matter is, the group creditor life insurance may be cancelled with little or no notice to you. Many financial banking institutions now offer Credit Balance Insurance that is intended for all eligible credit card holders. This covers the balance of any current transactions and usually covers an individual’s credit card payment in the case of: Death; Loss of use or dismemberment; Disability; Loss of employment; First diagnosis of a critical illness. Or any combination of the above. Savings Group Insurance Insurance is provided for depositors and/or investors, as a plan becomes selfcompleting if they die. It generally would cover the contractual payment period only, but not equal to the total goal to be saved. Association Group Insurance Very simply, Association Group Insurance means, a group formed from members of a trade or a professional association for group insurance under one master health insurance contract. 16 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 All other Employee Benefits Plans have two parties contributing or “employer pay all” plans. The hybrid of Employee Benefits is a cross between true group and grouped individual coverage, known as Association Group Insurance. Associations are groups of individuals or companies with similar occupations. Lawyers, Doctors and some hardware chains all belong to Associations. The main difference is that the Association arranges for Group Coverage for its members and the individual member pays all the premiums. The master contract exists between the Association and the Insurer. The individual member receives a certificate that details coverage. Participation is up to the individual member and so participation may be somewhat lower than true group. Due to the nature of Associations, the individual member has less control and input into what the coverage will be and the changes that can be made to the plan without their input. Individual insurance is a superior product in most ways except for cost. Advantages of Association Plans: Provides for more economical coverage that would otherwise be available. Allow for mass purchase and group discounting. Arranged by the Association and only requires payment to activate. Provides for larger amounts of Life Insurance on younger lives, when more coverage is necessary. Certificate issued, showing coverage. Right to convert Life Insurance within 60 days of termination. Disadvantages of Association Plans: Coverage reduces in later years and the premiums can be increased without notice, plan amendments, restrictions or termination without input of member. Restrictive clauses, lower maximums and can contain a two-year suicide clause. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 17 The Association holds the Master policy. There is lack of control by the member, subject to adverse experience due to other association members. ACCIDENTAL DEATH AND DISMEMBERMENT (AD &D) An AD & D benefit is usually included as part of the life benefit. The principle sum, payable in the event of an accidental death, quite often matches the amount of Life Insurance. Most AD&D benefits cover for Loss of Use, and not just death. Usually there is a period before a loss of speech or hearing will be paid to the Insured. This time is 12 months with many Insurance Companies. The coverage detail lists numerous dismemberment’s each with its own percentage loss of the principle sum. An example of some AD&D that could be payable: Loss of life, or Loss of both hands, or Loss of both feet, or Loss of sight of both eyes, or Loss of one hand or one foot and sight of one eye, or Loss of speech and hearing in both ears, or Loss of Use of upper and lower limbs (Quadriplegia) A benefit equal to three quarters the Amount Insured for the: Loss of one arm or one leg, or Loss of Use of both arms, or Loss of Use of both legs (Paraplegia) 18 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 A benefit equal to one half the Amount Insured for the: Loss of one hand only, or Loss on one foot only, or Loss of sight in one eye only, or Loss of speech or hearing in both ears, or Loss of Use of upper and lower limbs of one side of body (Hemiplegia) A benefit equal to one quarter the Amount Insured for the: Loss of thumb and index finger on the same hand, or Loss of hearing in one ear. Loss This term refers to hands or feet that have been severed at or above the wrist or ankle joint; with respect to eyes, entire and irrecoverable loss of the sight beyond remedy by surgical or other means; with respect to arms and legs, complete severance at or above the elbow or knee joints etc. Loss of Use With respect to arms, hands, legs and feet, total loss of the ability to perform each action and service that the arm, hand, leg or foot was able to perform before the accident occurred. It must be entire and irrecoverable. Exclusions of AD&D The benefits of this feature will not apply if the Insured Employee’s death, Loss of Use or Loss results from one of the following: Suicide or intentionally self-inflicted injury. While in the process of committing a criminal offence. Service in the military OR driving while intoxicated. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 19 DEPENDANT LIFE Most group policies offer a Dependent Life option to the employees. As an example, it could be $10,000 of the spouse and $5,000 for children who are dependent of the Insured Employee. This benefit is a small extra to help take care of some of the final expenses of the dependent at death. The cost for this benefit is usually very low. GROUP DISABILITY PLANS Disability is insured against, with two compatible benefits, either of which can stand-alone. There are of course the Canada Pension Plan and Employment Insurance (formerly Unemployment Insurance Commission Sick Benefit) that will help cover the uninsured individual of a group plan. These will be discussed later in the course. WEEKLY INDEMNITY (REFERRED TO AS WI OR SHORT TERM DISABILITY) STD has become the standard alternative to the Unemployment Insurance Commission’s (EI) short-term disability benefit, which commenced July 1, 1971. Short-term disability plans can be set up in many different formats. It is important during a fact find to find out what the Employer has in mind, and how their disability goals can be complimented with this product. The STD Plan, to replace Employment Insurance (EI) must provide benefits that are the equivalent to the minimum EI benefits or better in order to qualify for an Employer discount on their EI premiums. The typical Weekly Indemnity Plan therefore has the following benefits: Waiting Period 0 days Accident 7 days Sickness 20 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Benefit Maximum of 70% of pre-disability income (66.7% standard) to a dollar maximum per week, if the benefit is taxable, a lesser amount if the benefit is non-taxable. This benefit would match the EI benefit of 17 weeks. Both the waiting period and benefit period can be adjusted depending on the plan. Weekly indemnity can be written on a non-occupational basis, if Workers Compensation Benefits are provided, thereby reducing the premium required. It is also beneficial for an Agent / Broker to know how the government Employment Insurance (EI) Benefit works in co-ordination with Employee Benefit Plans. Premium Payment and Income Tax for Group Disability plans The basic rules for Group Disability Plans are: If the employee pays the premiums, the benefit received is tax-free. If the employer contributes any amount towards the premium, the benefit is taxable. LONG TERM DISABILITY (LTD) Long Term Disability is a plan designed to replace the income of the most serious and prolonged disabilities of the employee. It is designed to complement and enhance the disability income when weekly indemnity ceases, or the EI Disability stops. Waiting Period: 120 days Benefit: 66.7% (although 50 – 75% is common in some instances). Benefit Period: to age 65 In order to be familiar with Long Term Disability terminology, you should know the meaning of the following, so that you can explain LTD properly. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 21 Injury Accidental bodily injury sustained by the Insured Employee. Sickness This term refers to any sickness or disease of the Insured Employee, providing that it is not excluded elsewhere in the Provisions of the contract. Indexed Pre-Disability Earnings This income is taken from the average of: Earnings, if the Long Term Disability is taxable or, Take home Pay if the Long Term Disability benefit is non-taxable. Elimination Period The initial period of continuous Total Disability of an Insured Employee during which no Long Term Disability Benefit is payable. Elimination periods can fluctuate, and are referred to in the Schedule of Benefits that are found at the beginning of a contract. Many long-term Disability provisions will include reference to the payment of Long Term Disability Benefits, Recurrent Disability, Rehabilitation, Exclusions and Reduction of Coverage’s. It is also interesting to note that definitions will differ within the Insurance industry. Another compliment to Disability plans within an Employee Benefit Program is the Canada Pension Disability plan. We have included some useful updated information for you later in the course. HEALTH CARE (EXTENDED HEALTH CARE) Extended Health Care Benefit is a benefit that picks up where Provincial Hospital Plans leave off. It provides an extension for some benefits and provides other benefits not available through the Government Plans. The benefits vary from Province to Province, but the core benefits are consistent. 22 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Health Care (EHC) provides a host of benefits that supplement the Government Benefits (they cannot replace them) until the Government maximum have been reached. The Health Care Benefits usually provide for: Semi-private or private room accommodation in a hospital Prescription drugs Private duty nursing Ambulance services and Appliance and prosthesis Paramedical services Eye and hearing care Before we look at the different coverage’s under this part of an Employee Benefits plan, we have included some definitions of terms that play a major role when referring to this section of the plan. Medical Care Means the necessary services; supplies or treatment provided or ordered in the treatment of Sickness or injury and, with the exception of Dental Benefits for Accidents and Vision Care, Medical Care must be ordered by a Physician in the treatment of the Sickness or injury. Eligible Expense Refers to any charge for Medical Care actually incurred by a Person who is insured while the coverage is in effect. This care must be a covered benefit, and has to be of a reasonable and customary charge not in excess of the maximum amount that is shown for such benefit. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 23 Emergency This sudden, unexpected occurrence requires immediate medical attention. This also refers to non-elective relief of severe pain, suffering or disease, which cannot be delayed until the Insured Person returns to their home province. Participating Pharmacy (Preferred Provider) This Pharmacy has a valid agreement in force to be able to accept pay-direct drug claims. Generic Drugs and Medicine This may or may not be referred to under the drug portion of the plan. Generic Drugs refer to the lowest cost drugs and medicines that contain the same amount of the same active ingredients in the same dosage form as directed by the Physician’s prescription. Dispensing Fee The profession has for a long time abused this area. Dispensing fees vary from location to location. Fees are charged by a pharmacist for the preparation and dispensing of drugs that are covered under the plan. Many Insurance Companies will offer many options when it comes to this area. The thing to remember here is that the sooner the Insurance Company has to pay for the drugs, the higher the premiums to the Employer will be for the drug coverage benefit. Drug Card Much like a credit card, it is an identification card issued by a third party company that is used to participate in a pay-direct drug reimbursement program. Deductible Amount This amount must be paid before the Insurance Company will pay any Health Benefit. There may also be a family deductible amount that has to be satisfied during a specific period. 24 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Coinsurance Amount This is the amount or percentage of any eligible expense which are payable by the Company in excess of any deductible amount. All Insurance Companies will offer other benefits when looking at the Health Benefit component of an Employee Benefit package. There may be reference to Extension of Benefits, Survivor Benefits, Limitations and Exclusions. What are the insured components of the Health Care Benefits? Semi-private or private hospital component This refers to the Insurance Company reimbursing the difference between the Hospital’s ward and semi-private rates. Insurance Companies usually has no limitations on the number of days of confinement. The insured’s Physician in consultation with the Hospital dictates this Drug component Again, this is one of the most widely used areas on any group plan. The drugs covered can be Generic, or Name Brand, as specified by the Physician. Any drugs prescribed have to be recognized as being effective in the treatment of the sickness or injury being treated and cannot be excessive. These drugs and medicines can also include: Insulin supplies (i.e. Needles, syringes and diagnostic tests), but will not include any swabs and rubbing alcohol, All injectibles including serums, vaccines and injectibles vitamins, and Extemporaneous Compounds prepared by a pharmacist. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 25 Exclusions Any drug medication that may be purchased without a prescription (i.e. over the counter products, whether they have a prescription or not). Fertility Drugs (unless specifically spelled out in the Master Policy). Anabolic steroids. Items deemed cosmetic. Vitamins (except injectibles). Patent medicines First aid and surgical supplies. Atomizers and vaporizers. Salt and sugar substitutes. Infant formula, dietary foods and aids. Contact lens care products. Diagnostic aids and laboratory tests. Contraceptives other than oral. Lozenges, mouthwash, toothpaste and cosmetics. Non-medicated shampoos, skin cleaners, skin protectors, emollients and soaps. Anti –smoking agents, unless specified otherwise. Any benefit covered by any government plan. MAJOR MEDICAL COMPONENT Usually there is a stipulation stating that any of the following will be covered in the Insured’s province of residence. Medical Supplies and Appliances The Insurance Company may, at its option provide for the rental or purchase of some or all of the following durable equipment. Many of the coverage’s below will have either a lifetime or one time ceiling on dollar amount of reimbursement from the Insurance Company. This depends on each individual corporate Employee Benefit plan. 26 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Some benefits with limitations are: Aerosol equipment, mist tents and nebulizers for cystic fibrosis, acute emphysema, chronic obstructive bronchitis or chronic asthma. Artificial eyes including the repair and replacement of. Bed rails braces with rigid supports. Diabetic monitoring and administration equipment. Breast prosthesis. Wheelchairs. Insurance Companies will not usually cover the maintenance of any durable equipment. Depending on the type of coverage’s offered by the Employee Benefit plan, the following supplies and devices may also be covered: Casts, canes, crutches and walkers. Cervical collars, Burn garments orthopedic shoes. Oxygen and oxygen supplies but not usually containers. Splints, excluding any dental splints. Support hose, stump socks. Urethral catheters. Ambulance Services This is standard coverage with all carriers. The Insurance Company will pay for local transportation by a licensed ambulance to and from a Hospital that is qualified to render the necessary Emergency Medical Care. The benefit would also cover any air ambulance or commercial airfare if it were deemed necessary to provide transportation to the nearest Hospital if the Insured person cannot be transported otherwise. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 27 Private Duty Nursing When an Insured person requires the services of a private duty nurse in their home, and if the home is not an institution, payment will be made. Usually a maximum amount is eligible to be paid out. The person providing the services must be one of the following: Registered Graduate Nurse (R.N.) Registered Nursing Assistant (RNA) Certified Nursing Assistant (C.N.A.) Licensed Practical Nurse (L.P.N.) The above individuals must be registered with the appropriate provincial registry or the out of province equivalent, but cannot be related to the Insured person. There must be a recommendation of a Physician that pertains to the nature of the sickness or injury being treated. Homemaking or companion duties will not be covered. Paramedical Services This section of an Employee Benefit Plan covers the following professionals when they provide service while not confined to a Hospital. Usually there are maximums, while any payment will not begin until any Government Health Insurance Plan has paid their portion. The following are standard professionals covered under most plans: Speech Therapist Clinical Psychologist Masseur Chiropractor Osteopath Podiatrist / Chiropodist / Naturopath Physiotherapist 28 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Other benefits covered under this section of the contract: Dental benefits for accidents. Hearing Aids Eye Exams Medic Alert Convalescent Hospital Out of Province of Residence coverage Accidental Dental coverage DENTAL CARE Dental Care is statistically the most used benefit and can be remembered by the following acrostic: P Preventative Care E Endodontist M Major Restoration O Orthodontics There are some definitions that you should be familiar with. They are very general in nature, but you should be able to explain them to the Employer or their Employee’s when called upon to do so. You should know the differences of each. Terms to remember: Dentist or Oral Surgeon Dental Assistant Fee Guide Periodontal Services Endodontist Services Orthodontic Services Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 29 Both Health and Dental care may have a deductible such as $25/$50 and/or a CoInsurance factor (20/80%). Deductibles are applied against the first claims of the calendar year until satisfied. Co-insurance is applied against each claim. They both result in lower premiums being charged for the benefit. The Dental Benefit could have a maximum amount that can be charged for each calendar year by each insured member and their dependent’s (e.g. $1,500) and sometimes a different maximum for different levels of care. Survivor Benefits Many plans provide for continuing survivor benefits for the dependents in the event of the death of the Insured person. It is not uncommon for the length of time to differ among Insurance Companies. Who Pays the Premiums? Non Contributory Plans that are employer “pay all” are said to have the following advantages: Employees enjoy the fact that they do not contribute to the plan cost and lower paid employees can participate in the same level of care as the more highly paid employees. The plan has lower administration costs, is easy to install and maintain. All employees are automatically covered, thereby eliminating missed coverage or uninsured employee death or disability. Premiums are tax deductible for the employer, but are a taxable benefit to the employee. If the employee reimburses the employer for their portion of the premiums, the premium ceases to be a taxable gain. 30 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Disadvantages The employer bears the maximum cost, which may limit how comprehensive the plan may be. The employee must take into income the premium paid on their behalf (Taxable Benefit). Benefits received as payments under Weekly Indemnity or LTD is taxable to the employee. Contributory Plans When an employee contributes a portion of the premium it allows for more overall premium that should result in a more overall comprehensive plan. Employees have a greater degree of “ownership” when they pay part of the cost. Helps to eliminate excessive claims (creating high experience ratios), thereby resulting in lower renewal increases. Notes to Contributions: Since employer payment of disability premium (all or part) results in a taxable benefit when received, it is advisable to designate the employee’s contribution to pay disability premiums. If the contribution will not cover the entire disability premium, the LTD portion should be paid before the Weekly Indemnity portion. Effective with the February 24, 1998 Federal Budget, Health and Dental premiums became deductible for the self-employed. GROUP CRITICAL ILLNESS INSURANCE It's a fact that one out of every three Canadians will contract a life-altering illness during his or her lifetime. And with today's advances in medical science, the chances of survival are greater than ever. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 31 But will your finances survive? Few of us are prepared for the financial burdens that can threaten both our lifestyle and our security. Convalescence, private nursing costs, reduction or permanent loss of income, a change of profession, child care, medical income, medical equipment or home refitting, mortgage and other debt payments. In addition, even relocation of your home to a new locale or climate may be in order as a result of any illness. Some real statistics Heart disease: 1 in 4 Canadians will contract some form of heart disease. 75,000 Canadians suffer heart attacks each year. However, there has been a 50% decrease in the heart and stroke rate since 1950. Life threatening cancer: 1 in 3 Canadians will develop a life threatening cancer. 125,000 new cancer cases are diagnosed each year. Stroke: 50,000 Canadians suffer a stroke each year. 75% survive the initial event. Multiple Sclerosis: More than 50,000 Canadians have Multiple Sclerosis MS is the most common neurological disease among young Canadians. 32 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 The Cost of Living with a Critical Illness The impact of surviving a critical illness goes beyond the physical and emotional consequences. Consider some of the new expenses you might face if you were to survive a debilitating stroke. LIFESTYLE ADAPTATION EXPENSES TRANSPORTATION EXPENSES HOME CONVERSION EXPENSES Home Care Companion: $100 per 8 hour shift Nurse: $240 per 8 hour shift Wheelchair Non-Motorized: $275 - $775 Motorized: $3,500 - $5,600 Walker No-Wheels: $120 - 200 Wheels: $220 - $600 Motorized Scooter $1,400 - $6,000 Chauffeur $50 per hour Van Conversion (assumes already own a minivan) Electric lift: $2,690 Automatic door opener: $900 Hand controls: $600 Remote for hand controls: $625 Power seat base: $2,000 Raised roof: $3,500 Van doors raised: $2,000 Wheelchair tie down: $50 Total: $12,365 Exterior Access Ramp leading to house: $50 per square foot Landing at end of ramp: $15 per square foot Porch lift: $4,500 Bathroom Toilet, shower, sink: $8,000 $15,000 Grab bars: $100 per bar Doors All doorways: $800 per unit Patio doors: $2,000 Automatic front door: $2,200 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 33 Stairs Lift for straight stairway: $3,500 Lift for circular stairway: $13,000 Elevator: $15,000 - $25,000 Additions Wheelchair needs 5 foot turning radius (most homes are not built to provide this): $100 - $150 per foot Many people who survive critical illnesses face serious financial constraints as they attempt to recover. Now there is a solution that takes away the financial strain of surviving a critical illness. Fundamentally, critical illness coverage is about helping to ensure you have the financial resources to sustain you during a critical illness. By obtaining such coverage on a group basis, however, you can enjoy additional benefits. Foremost is the ability to receive coverage without medical underwriting. The average age of the employees may present barriers to their obtaining coverage on an individual basis. For an individual, a medical assessment may preclude or restrict coverage, or incur a higher premium. On a group basis, however, coverage is guaranteed and provided at a premium at least 20 per cent below that of an individual policy. As a bonus, group coverage is portable. Employees who leave your firm may continue their coverage - and retain the group-discounted premium - up to age 75. Critical illness is a valuable complement to a company's existing disability insurance coverage. Critical illness policies provide a lump-sum, non-taxable benefit 30 days after diagnosis of one of 16 major illnesses covered under the plan. Disability insurance only pays a percentage of your current income and requires proof of inability to work. 34 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 A lump-sum payment can help a person cope - physically, financially and emotionally - with a major illness. Beyond reducing stress and anxiety, critical illness coverage can help to pay for treatments not covered by or readily available through the public health-care system. Group CI Insurance like individual CI can: Pay for out-of-country or experimental treatments, Cover mortgage or loan payments, address workspace and/or living modifications, Cover a recovery vacation, What Illnesses Will Critical Illness Insurance cover? CI insurance will provide a lump sum benefit just 30 days after the diagnosis of one of the following critical illnesses: The following list is by no means complete, as Insurance companies are constantly adding new illnesses to their CI portfolio Alzheimer’s Loss of Speech Blindness Major Organ Transplant Coma Motor Neuron Disease (ALS or Lou Gehrig's Disease) Coronary Artery Bypass Surgery Multiple Sclerosis Deafness Paralysis Diabetes (insulin-dependent) Parkinson’s Heart Attack Severe burns Kidney Failure Stroke Loss of Limbs Occupational HIV Life Threatening Cancer Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 35 You choose the level of coverage that meets your needs. Should you contract a critical illness; the lump sum payment will help you maintain your lifestyle and your financial health. Critical Illness benefits for your corporate clients: Provide financial assistance to a valued workforce at a reasonable cost. Foster good employer-employee relations. Contributions are treated as a low-cost, tax-deductible business expense. Benefits for your corporate clients’ employees: Reassurance of a capital lump sum payment if serious illness should strike. Protection against the most commonly suffered critical illnesses (cancer, stroke, heart attack and kidney failure etc.). Help and support during rehabilitation. Cash to help clear debts or cover household bills. GROUP LONG-TERM CARE PLANS (Becoming more prevalent) The Health Care Crisis and Your Future Canadians like to assume most of their health care needs will be looked after with little direct financial strain. But times are changing. With government cutbacks, insured health services are diminishing and there may be some nasty shocks in the years to come. Even under optimistic scenarios, provincial health plans won't cover all the options you need to consider if you develop a long-term illness or suffer a disability. 36 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Long-Term Care insurance allows you to take control of your future needs, with the freedom to receive personal attention from care-givers in the comfort of your own home or to select a private care facility. A Long-Term Care plan can protect you against a drain on your financial resources and a strain on your family. Potential Consequences of Not Planning Ahead It's not easy to pay the difference between what provincial health plans cover and what people requiring long-term attention truly deserve. Think for a moment about how you would finance care in a private facility, with costs that can easily climb beyond $3,000 a month per person. Try to imagine how you would pay for home care services, which could end up costing even more. This is something to consider in your long-range financial planning to avoid facing unpleasant alternatives. Without proper long-term care planning your group clients employees may be forced to: Deplete their savings. Sell their house. Rely on their children to support them. Severely lower their standard of living. Let the government make their care decisions. EMPLOYEE ASSISTANCE PLANS Employee Assistance and Wellness Program There has been a tremendous increase in demand for services provided by Employee Assistance Programs (EAPs). In fact, this field has grown so rapidly that today most firms are looking at providing Employee and Family Assistance and Wellness Programs. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 37 There are a number of companies offering EAPs. Traditionally it has been insurance carriers that came up with plan designs to provide different services. However, a number of companies are currently directly specializing in providing services in this field. EAPs will usually provide services in dealing with: critical illnesses and disability counseling retirement planning alcohol and drug abuse and psychological disorders financial or legal problems relocation sexual harassment divorce and more Perhaps the most important feature of an EAP is confidentiality. Under the new Privacy Information Act this program provides an ideal solution for any employer who wants to keep employees productive and satisfied in the workplace. Many insurers will provide assistance in getting professional advice to select the right Employee and Family Assistance Program for employees. GOVERNMENT BENEFITS Employment Insurance (EI) Benefits – Formerly UIC The Employment Insurance Act is a total restructuring of the old Unemployment Insurance program and was implemented in January 1997. The Act was designed to help today's labour force, providing assistance where it is most needed and offering incentives for claimants to return to work. 38 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Employment Insurance (EI) provides temporary financial assistance for unemployed Canadians while they look for work or upgrade their skills. Canadians who are sick, pregnant or caring for a newborn or adopted child, as well as those who must care for a family member who is seriously ill with a significant risk of death, may also be assisted by Employment Insurance. The Employment Insurance system is based on hours of paid work and adheres to fluctuations in work situations such as part-time, extended hours and compressed weeks. The principle of the hour’s system is simple, regardless of whether you work fulltime, part-time, as a seasonal worker or on and off throughout the year, the hours that you work and for which you are paid are accumulated toward eligibility for EI benefits. Using hours instead of weeks to calculate eligibility ensures that you are credited for all your paid work time. This approach applies to overtime, which is calculated hour for hour no matter what the rate of pay. As well, paid leave of any type is insured for the number of hours that normally would be worked in that period, regardless of rate of pay. Employment Insurance Premiums As of January 1, 2012, the employee rate per $100 of insurable earnings is $1.83. The corresponding employer rate is $2.56 per $100. Maximum insurable earnings for 2012 are $45,900. The new legislative authority requires the EI Commission to set the rate by November 14th every year so that employers can plan for the following year. The 2012 maximum employee contribution amount will be $839.97. The 2012 EI premium rate for Quebec will be $1.47 per $100 for employees and $2.06 for employers. Quebec offers its own parental benefits, resulting in a saving for EI and explaining the difference with the rate for the rest of Canada. The maximum annual EI employee premium in Quebec is $674.73 for 2012. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 39 What is covered? For those who lose a job through no fault of their own, are able to work and are available for work. You must have worked a certain number of insurable hours, normally from 420 to 700, over a qualifying period, usually the previous 52 weeks. The number of insurable hours required depends on where you live in Canada and the unemployment rate for that region. Who is eligible? To be eligible for regular benefits you must show that: you have been without work and without pay for at least 7 consecutive days; and In the last 52 weeks or since your last claim, this period is called the qualifying period, you have worked for the required number of insurable hours. The hours are based on where you live and the unemployment rate in your economic region at the time of filing your claim for benefits. Qualifying period The qualifying period is the shorter of: The 52-week period immediately before the start date of a claim, or The period since the start of a previous EI claim if that claim had started during the 52 week-period. Only the insurable hours that fall within the qualifying period are used to start a benefit period. However, the qualifying period may be extended up to 104 weeks under certain conditions. How much does the individual receive? The basic benefit rate is 55% of your average insured earnings up to a maximum amount of $485 per week in 2012. Your EI payment is a taxable income, meaning federal and provincial or territorial - if it applies - taxes will be deducted. 40 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 You could receive a higher benefit rate if you are in a low-income family — net income up to a maximum of $25,921 per year (2011) — with children and you or your spouse receive the Canada Child Tax Benefit (CCTB). You are then entitled to the Family Supplement. EI MATERNITY, PARENTAL AND SICKNESS BENEFITS This government is available for those who are pregnant, caring for a newborn or adopted child or sick. Who is eligible? To be entitled to maternity, parental or sickness benefits you must show that: Your regular weekly earnings have been decreased by more than 40%; and You have accumulated 600 insured hours in the last 52 weeks or since your last claim. This period is called the qualifying period. If you have been paid EI benefits in the past and you received a written notice, for example, a warning letter or a penalty letter, for making a false statement, the required number of hours worked to claim maternity, parental and sickness benefits will be higher. Working while on maternity, parental and sickness benefits If you work while on maternity or sickness benefits, your earnings will be deducted dollar for dollar from your benefits. On the other hand, if you work while on parental benefits you can earn $50 per week or 25% of your weekly benefits, whichever is higher. Any monies earned above that amount will be deducted dollar for dollar from your benefits. You must, of course, report any earnings you make while collecting maternity, sickness or parental benefits. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 41 Various types of earnings Earnings paid or payable by your employer at the end of your employment or while you are receiving benefits, generally affect payment of your benefits. Maternity benefits Maternity benefits are payable to the birth mother or surrogate mother for a maximum of 15 weeks. To receive maternity benefits you are required to have worked for 600 hours in the last 52 weeks or since your last claim. You need to prove your pregnancy by signing a statement declaring the expected due or actual date of birth. The mother can start collecting maternity benefits either up to 8 weeks before she is expected to give birth or at the week she gives birth. Maternity benefits can be collected within 17 weeks of the actual or expected week of birth, whichever is later. Please note that the date you file your claim is very important in order for you to receive the maximum maternity benefits you are entitled to. If the actual date of birth is different from the expected date of birth, it is very important that you provide this date as soon as possible after the birth of your child. If your baby is hospitalized, then the 17 week limit can be extended for every week your child is in the hospital up to 52 weeks — following the week of the child's birth. You will still receive benefits for a maximum of 15 weeks, but payments can be delayed until your child comes home. The weekly EI payment and the number of weeks to be paid remain the same even if you give birth to more than one child at the same time. At the same time you present a claim for maternity benefits, yourself or/and partner can ask for parental benefits. 42 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Termination of a pregnancy When a pregnancy terminates within the first 19 weeks of pregnancy, it is considered an illness under EI. If that is the case, sickness benefits may be paid as long as the qualifying conditions for sickness benefits are met. On the other hand, if the pregnancy terminates in the 20th week or later, the claim for benefits can be considered for maternity benefits if the qualifying conditions for maternity benefits are met. The eligibility period for EI parental benefits can be extended for members of military families Note: The Government of Canada introduced a new measure in July 2010 to extend the eligibility period for EI parental benefits, up to a maximum of 104 weeks. This extension is available to Canadian Forces members who are prevented from collecting all their parental benefits during the regular 52-week eligibility period because their parental leave has been deferred or interrupted by an imperative military requirement. The regular eligibility period starts during the week of birth for a newborn or the week a child is placed with you for adoption and continues for the following 52 weeks. Parental benefits Parental benefits are payable either to the biological or adoptive parents while they are caring for a new-born or an adopted child, up to a maximum of 35 weeks. To receive parental benefits you are required to have worked for 600 hours in the last 52 weeks or since your last claim. You must sign a statement declaring the newborn's date of birth, or, when there is an adoption, the child's date of placement for the purpose of the adoption, and the name and address of the adoption authority. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 43 Parental benefits can be claimed by one parent or shared between the two partners but will not exceed a combined maximum of 35 weeks. Claimants making application for parental benefits must provide the name and Social Insurance Number (SIN) of the other parent for cross-reference purposes. Parental benefits for biological parents and their partners are payable from the child's birth date and for adoptive parents and their partners from the date the child is placed with you. Parental benefits are only available within the 52 weeks following the child's birth, or for adoptive parents, within the 52 weeks from the date the child is placed with you, unless your child is hospitalized. The weekly EI payment and the number of weeks to be paid remain the same even if you give birth to more than one child or if you adopt at the same time. Compassionate Care Benefits Employment Insurance Covers Care of Dying Relatives Since January 4, 2004, eligible Canadian workers who take time off work to care for a gravely ill family member can receive up to six weeks of employment insurance benefits over a period of six months. Their jobs will also be protected. Before the introduction of the compassionate care benefits, Canadians who took time off to help a dying relative usually had to depend on their employer's goodwill to be allowed unpaid leave and may have had to put their jobs at risk. To qualify for the compassionate care employment insurance benefits, an applicant must have worked 600 hours in the previous 52 weeks, and also must show that regular weekly earnings have decreased by 40 percent. A medical certificate must be provided to show that the family member has a high risk of death within 26 weeks. 44 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Compassionate care includes providing emotional support, arranging for third-party support or directly providing the care. The benefits apply to care for a gravely ill child, spouse or common-law partner, and parent, and include spouses and common-law partners of parents. The compassionate care benefits can be shared between eligible family members and the dying family member can be in another country. The federal government estimates that about 270,000 Canadians will be eligible for the compassionate care benefits every year. Quitting your job for compassionate care reasons It is hoped that compassionate care benefits will help you provide care or support to a gravely ill family member at risk of dying without having to quit your job. If you do quit, you may still be paid compassionate care benefits, but there is a possibility that you will not be paid regular benefits. You may be able to receive regular benefits if voluntarily leaving your employment was the only reasonable alternative in your case, considering all the circumstances. In other words, you took all the necessary steps to avoid quitting your employment. Labour disputes If your absence from work to claim compassionate care benefits was already approved by your employer before the work stoppage for strike, lockout or other form of labour dispute, you may be eligible for EI benefits. Compassionate care benefits outside Canada Compassionate care benefits to care for or support a family member who is gravely ill and at risk of dying can be paid regardless of where that family member — patient — lives. You have to apply for benefits and submit the same information/documents as required for a person taking care of a gravely ill family member residing in Canada. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 45 If you go outside Canada, you must advise Human Resources and Skills Development Canada. Employment Insurance (EI) Fishing benefits A fisher is a self-employed person engaged in fishing. The following outlines how the fishing benefits may apply to you. If you are not self-employed in fishing, but you still work in the fishing industry for someone else, regular benefits, maternity, parental and sickness or compassionate care benefits may be the solution. To qualify for fishing benefits, fishers need sufficient earnings from selfemployment in fishing in a maximum 31 week period before their claim starts —this period is called the qualifying period. You will need to earn at least between $2,500 and $4,200 to qualify for fishing benefits. This amount varies based on the unemployment rate in your region. If you have been paid EI benefits in the past and you received a written notice, for example, a warning letter or a penalty letter, for making a false statement, the amount of fishing earnings required to claim fishing benefits will be higher. If during the 52-week period that precedes the beginning of the qualifying period, you have $3,000 or more of fishing earnings or 490 hours or more of: Self-employment in fishing, Fishing benefits, Training relating to fishing which has been authorized by an Human Resources and Skills Development Canada (HRSDC) officer, Workers compensation, Employment measures related to fishing or A combination of the above, 46 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 However, if you have just started working as a self-employed fisher, or have returned to fishing after an absence of a year or more preceding your qualifying period, you may need to earn a minimum of $5,500 of fishing earnings to qualify. Also, if you have received one week or more of maternity or parental benefits in the 208 weeks preceding the 52-week period prior the qualifying period you will need to earn between $2,500 and $4,200 to qualify for benefits. Qualifying period The qualifying period during which earnings may be accumulated will vary according to the fishing seasons. It can start: during the week of March 1st or during the week of September 1st The maximum length of the qualifying period is 31 weeks counting back from the week prior to the beginning of your claim. It is important to realize that the EI Commission is considered “second payer” in many instances. This means that the benefits could be cut back or eliminated unless or until the other benefits run out. EI benefits are paid secondary to and reduced or eliminated by: Any income including wages or commissions from employment. Any payments in compensation for an accident or work-related illness, such as workers' compensation for lost wages. Income from Employee Benefits for sickness or loss of income. Some accident compensation for loss of wages. Retirement income from an employment pension, military or police pension, Canada or Quebec Pension Plan or provincial plan based on employment. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 47 Money received from the following sources, will not affect EI benefits: Disability pensions. Workers' compensation payments from a permanent settlement. Supplemental insurance benefits under a private plan approved by Human Resources Development Canada for sickness benefits. Supplemental payments to maternity or parental benefits provided by employers (as long as the combined income of the benefit and supplement do not exceed 100% of your normal weekly salary. Your private sickness or disability wage-loss insurance. Retroactive rises in your wages or salary. Because EI is considered the second payor in the above situations, many employers have opted out of the EI Sickness Benefit program by providing their employees with plans, which are at least equal to or better than the EI Commission. For employers who exercise this option, the Employment Insurance Act allows for a premium reduction to employers who have an employee income protection plan meeting certain standards. These types of plans must be in the form of a formal commitment from the employer. The formal commitment could be: A union or association agreement. An industry-wide welfare trusts contract or a private carrier’s insurance policy An employee’s handbook or a personnel policy bulletin. A board of director’s minute stating employees’ entitlement to disability income benefits. 48 Any commitment in writing by the employer to the employees. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 The employer must reapply each year for the premium reduction by certifying that the plan continues to meet all the above criteria. As a rule of thumb, the premium reduction to the employer is approximately $75.00 - $100.00 per year per employee. This may not seem like much, but consider the company with many employees. This would translate into large savings, and at the same time provide a superior plan. EI DISABILITY BENEFIT Provide a limited short-term benefit that is provided to all insured workers. Waiting Period: 14 days Benefit: 60% for low-income workers 55% for high-income workers, based on insurable earnings. Benefit Period: 15 weeks CANADA PENSION PLAN DISABILITY BENEFITS The Canada Pension Plan (CPP) disability benefit is available to people who have made enough contributions to the CPP, and whose disability prevents them from working at any job on a regular basis. The disability must be long lasting or likely to result in death. People who qualify for disability benefits from other programs may not qualify for the CPP disability benefit. You must apply for a disability benefit in writing. There are also benefits available to the children of a person who receives a CPP disability benefit. The CPP disability benefit is administered by Social Development Canada (SDC), a federal government department. It may take as long as three months for you to find out if your application for a disability benefit has been accepted. This time frame is much shorter for terminally ill applicants. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 49 If an application for a CPP disability benefit is not granted, there are three opportunities to have the application reviewed or reconsidered. Once a person qualifies for and begin receiving a CPP disability benefit, they must contact SDC to keep them informed of certain specific events in your life. Some examples include: if the person changes their name or their address, or if they earn over a certain amount each year. SDC will occasionally review the health and work status of people receiving a CPP disability benefit, to ensure that they continue to be eligible. Definition of CPP / QPP Disability The disability pension is payable to a contributor who satisfies the definition of “disabled.” Generally, it means physical or mental impairment that is both severe and prolonged. Severe means the inability to pursue any substantially gainful employment, while prolonged means that the disability is likely to be of indefinite duration or is likely to result in death. Under the QPP, the definition is modified in the case of a contributor age 60 or older. He or she will be deemed to be disabled if unable to pursue, on a permanent basis, his or her current occupation. Definition of 'Severe and Prolonged' Severe" means that a person is incapable of regularly pursuing any substantially gainful occupation. Within this definition, the words mean: Incapable - Not able or fit to pursue any substantially gainful occupation as a result of the disability. Regularly - The capacity to work is sustainable. 50 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Pursuing - To actually engage in an occupation, and does not mean being able to look for work. Work that a person might reasonably be expected to do regardless of whether it is his/her previous job by virtue of: Having the necessary skills, education or training; Having the capacity to acquire those necessary skills, education or training in the short term; and, Having reasonable access to suitable employment, given the individual's limitations but does not mean a job has to be available. Substantially gainful occupation: Work that is productive and profitable. This is measured in part by a dollar amount that is set annually and against which a person's earnings are compared. However, earnings alone do not determine whether the regular capacity to pursue work exists. CPP also assesses elements of functional capacity, productivity and performance. "Prolonged" means that the disability will prevent the individual from going back to work in the next 12 months, or is likely to result in death. To qualify, the applicant must meet both the "severe" and "prolonged" criteria. HRDC medical adjudicators assess the severity of the disability first. If the applicant does not meet the "severe" criteria, HRDC does not consider the question of whether the disability is prolonged. Many people mistakenly believe that CPP eligibility decisions are granted on the basis of a specific disease or condition alone. This is not the case. Rather, the decision is based on the limitations that a disease or condition imposes on a person's ability to work and earn an income on a regular basis. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 51 Remarriage does not revoke a surviving spouse’s pension. If the second spouse dies, the calculation of the pension may be based on the higher of the pensions that would have been payable to the now-deceased contributors. This definition is so restrictive, that usually CPP / QPP benefits will not be taken into account in planning for an unforeseen disability. If you do however, are qualified to receive CPP /QPP disability benefits, the chances are that you won’t be receiving them for long… they will eventually become survivor’s benefits. Who is eligible to receive CPP/QPP Disability? For the payment of a disability pension to a survivor or for payment of benefits for a child of a disabled pensioner, a contributor must have contributed for: 2 out of the last 3 years of the contributory period or 5 out of the last 10 years of the contributory period Have not received a CPP / QPP retirement pension benefit for longer than 12 months For those individuals who have contributed 10 years or more and are under Age 65 they must not have received the retirement benefit of longer than 12 months. A disabled survivor who is eligible for both a survivor’s pension and a disability pension can receive an amount equal to the maximum retirement pension plus the higher of the two flat-rate components of the survivor’s and disability pensions. The disability for a child of a contributor who becomes disabled will be the same as or orphans, but the qualifying period is the same as for the disability pension itself and the benefit commences with the disability pension and ceases with the disability pension or when a child is no longer a dependent. Orphan’s benefits are payable to the surviving spouse or guardian if the orphan is under age 18 and are payable directly to the orphan from age 18. 52 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 In cases where both parents are contributors and they die or become disabled, a dependent child can receive two benefits. How CPP disability benefits are calculated: Benefits are based on earnings and contributions credited to an applicant's CPP or QPP account and on how long he or she contributed (this is known as the contributory period). A portion of the monthly disability benefit is based on a flat rate. Contributions on pensionable earnings: Contributions to CPP are made on annual earnings above a minimum amount called the "yearly basic exemption" (YBE). Since 1998, this amount has been frozen at $3,500. No contributions are made on earnings above a limit called the "year's maximum pensionable earnings". This amount is linked with the average Canadian wage. It changes each year. CPP contributions are made on earnings between the basic exemption and the maximum pensionable earnings for the year. They are based on: Employment earnings from salary or wages; and Self-employment earnings. The employer matches each employee's contribution. Those who are selfemployed pay both shares. Earnings and contributions can also be gained or reduced by splitting CPP credits between two people who separate or divorce (see Splitting CPP Credits). A person cannot make voluntary contributions to the CPP. The Canada Revenue Agency is responsible for collecting and recording contributions. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 53 Anyone can ask for a record of the earnings recorded in his or her account. This is called a Statement of Contributions and can be requested once a year. It includes estimates of disability, retirement, death and survivor benefits. When a benefit becomes payable, earnings in a contributory period are adjusted to reflect current dollar values. All CPP benefits are based on the earnings, contributions and number of years in a person's contributory period. Contributory period: Each person has his or her own contributory period, which is based on the span of time it is hypothetically possible for a person to contribute to the CPP. To determine a person's lifetime average pensionable earnings, his or her earnings are divided by the months in his or her contributory period. The contributory period is calculated from January 1, 1966, or the month following the applicant's 18th birthday, whichever is later, and ends the earliest of the following: The month in which the contributor is deemed to have a disability; The month before the retirement pension starts; The month of the contributor's 70th birthday; or The month the contributor dies. Months when a person received a disability benefit from the CPP or QPP are not included in the contributory period. Years of zero or low income: Most people do not work from the age of 18 to retirement without some interruption in their employment history. For example, they can be: Unemployed. In school or university. Receiving disability benefits; or Raising children. 54 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Although CPP calculations include both how much and how long a person has contributed, some periods of low income can be dropped out of the calculation. Dropping out periods of low income can increase the amount of a person's benefit. Here are some ways the calculation can be adjusted: Child rearing drop-out provision means months of little or no earnings because of caring for children less than seven years of age who were born after December 31, 1958, can be excluded from the contributory period when benefits are calculated. Unlike the other three drop-out periods listed below, this benefit must be applied for by the client. The+ 65 drop-out If a contributor works between the ages of 65 and 70, higher earnings from those years can be used to replace months of little or no earnings earlier in the contributory period. The 15 percent drop-out The 15 percent drop-out applies to everyone who has contributed to the CPP for at least 10 years. After the number of months in a person's contributory period is determined, the 15 percent of that period when his or her earnings were lowest are dropped out of the benefit calculation. The benefit amount he or she receives is calculated on the earnings and contributions recorded in the remaining 85 percent of the contributory period. The Disability drop-out The months in which a person receives CPP disability benefits are excluded from his or her contributory period when benefits are calculated. Other considerations in calculating benefits Other circumstances must be considered in the calculation of a person's contributions to the CPP. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 55 Quebec Pension Plan credits: If a person has contributed to the QPP and the CPP, his or her contributions to both plans will be combined. Both plans will be used to determine whether the person meets the contributory requirements and to calculate the benefit he or she will receive. If the person contributed only to the QPP, or contributed to both plans but resided in Quebec at the time he or she applied for the disability benefit, the QPP would pay the disability benefit. Social security agreements with other countries Anyone who has contributed to a social security program in a country with which Canada has a social security agreement may use those credits to help meet the contributory requirements of the CPP. Once eligibility is established, however, the amount payable is based only on actual contributions to the CPP and/or QPP. CPP credits might also help an individual qualify for a foreign pension. This is done by adding periods of contributions to the CPP and/or QPP to periods of coverage under the social security program(s) of the other country. A person must meet that country's contributory requirements to be entitled to a benefit from that country. Splitting CPP credits In a legal marriage or a common-law relationship (whether opposite-sex or same sex), both spouses share in the building of their assets and entitlements, including CPP credits. When a relationship ends, the CPP credits built up by the couple during the time they lived together can be divided equally between them. This is called "credit splitting". Splitting CPP credits protects the spouse who was the lower wage earner or had no wages during a couple's years together by increasing his or her CPP credits. This means that he or she would be eligible for a larger benefit once the application is approved. 56 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 In the case of a legal divorce or annulment that took place on or after January 1, 1987, no application is needed. Simply notify the government that the divorce occurred and they will ask for certain information. In all other cases (e.g., legal or common-law separation), an application requesting credit splitting is required. There is a time limit for applying if a person is in one of the following two situations: A legally separated person whose spouse has died must apply within three years of the spouse's date of death. A person separated from a common-law union (which has lasted one or more years) must apply for credit splitting within four years of the separation. STEPS IN THE CALCULATION OF A DISABILITY BENEFIT To determine the amount of a CPP disability benefit, the basic retirement amount must first be calculated. The disability benefit is equal to 75 percent of a person's calculated retirement pension, plus the flat rate. 1. Pensionable earnings for every year of a person's contributory period are adjusted to their current value. 2. All drop-outs are applied to the record of earnings. However, no drop-outs can be applied if the number of months remaining in the contributory period is less than 48. 3. After all the earnings have been adjusted to reflect their current value, and the periods of little or no earnings have been removed, the earnings for the remaining months are added together and divided by the number of months remaining in the contributory period. This provides the contributor's average monthly pensionable earnings. 4. The retirement pension is calculated at 25 percent of the average monthly pensionable earnings. 5. The disability pension is calculated at 75 percent of the retirement pension, plus a flat rate. The flat rate used in the formula is the flat rate for the year in which the benefit is effective. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 57 Combined benefits People who are receiving a survivor's pension may also have contributed to the CPP on the basis of their own earnings and may also be entitled to a disability benefit. A CPP recipient can get both a survivor and a disability benefit at the same time. CPP combines the two benefits into one monthly payment. There are, however, limits to what a person can receive, which will not equal the total of both benefits. In such cases, the survivor receives a combined pension which is calculated as follows: If the survivor also receives a disability benefit, the larger of the two flat-rate amounts is paid. Any earnings-related benefits or benefit components may be added together, but their total may not exceed 75 percent of the maximum retirement pension payable for the year in which the contributor becomes eligible for the second benefit. Benefits The monthly disability pension is a flat-rate component (subject to review) plus an earnings-related component equal to 75% of the calculated retirement pension. It will be payable to age 65 (unless the disability pensioner dies or recovers) when it will be replaced by the retirement pension. A spouse already disabled at the contributor’s death is entitled to the full survivor’s pension at any age under age 65. If the disabled spouse recovers before attaining age 45, the pension will be reduced by 1/120th for each month he or she is under age 45. 58 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 For contributor: Waiting period: 3 months Amount: Flat rate (indexed) plus 75% of what remaining benefit would have been at age 65 (in 2012, $445.50 plus 75% of age 65 retirement benefit) For qualifying child: Amount: Flat rate (indexed) - 224.62 in 2012 TAXATION OF CPP / QPP BENEFITS Contributions are tax deductible and benefits taxable when received. Individuals who receive income from more than one source may find that they have taxes to pay when they file their income tax return. This can happen if they receive income that has no tax withheld or not enough tax withheld at source. This is often the case for individuals who receive Canada Pension Plan (CPP), Quebec Pension Plan (QPP), or Old Age Security (OAS) benefits in addition to other pension, interest, employment, or self-employment income. For anyone applying for CPP, QPP or OAS benefits, it is important to understand that the addition of this income could mean they will owe taxes when they file their next income tax return. To determine this, they should calculate what their tax liability will be for the year. If they expect to have to pay tax, they may find it convenient to arrange to have tax withheld from their CPP benefits, or they can increase the amount that is already withheld on another source of income. Clients who need help calculating their tax liability should contact their tax services office. For identification purposes, they may be asked to provide their social insurance number, date of birth, and the total income amount they reported on line 150 of their last tax return. This information is also necessary if the enquiries agent needs to access their personal tax information. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 59 SELECTED MONTHLY MAXIMUM SURVIVOR and DISABILITY BENEFITS Canada Pension Plan rates are adjusted every January if there are increases in the cost of living as measured by the Consumer Price Index. The table below lists the maximum and average monthly rates for Canada Pension Plan benefits in 2011/2012. Canada Pension Plan Payment Rates Type of benefit Average monthly benefit (October 2011) Maximum monthly benefit (2012) Disability benefit $820.96 $1185.50 $512.64 $986.67 $383.56 $543.82 $301.15 $592.00 Children of disabled contributors benefit $218.50 $224.62 Children of deceased contributors benefit $218.50 $224.62 $701.46 $986.67 $949.22 $1185.50 $2,276.62 $2,500.00 Retirement pension (at age 65) Survivors benefit (under age 65) Survivors benefit (age 65 and over) Combined survivors & retirement benefit (pension at age 65) Combined survivors & disability benefit Death benefit (max lump sum) 60 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 How Does Long Term Disability compare to the Canada Pension Plan The Canada Pension Plan disability benefit commenced May 1970. It is paid only in the event of a severe and prolonged disability of a taxpayer. The CPP disability benefit is a primary payer and since the LTD integration clause may limit the total benefit that can be received, the CPP and LTD benefits may be either “offset or stacked”. Offsetting the CPP Benefit will reduce the LTD premium, while stacking will not affect the rates. The CPP Benefit can be offset totally or just the contributors portion. Primary offset will result in some premium relief. LTD and CPP Benefits may be the deciding factor of whether a family survives economically or not. Certainly anything less is sure economic disaster. In 2012 close to 400,000 Canadians will receive either CPP or QPP disability benefits. More than $300 million in benefits will be paid. WHAT ABOUT THE CANADA PENSION PLAN (CPP) RESERVE FUND? The reserve fund stood at $152.3 billion at September 30, 2011 – down slightly from June 2011, but up almost 10% compared to one year earlier. Between 2005 and 2010 CPP assets grew at an annual rate of 3.8% - substantially better than the performance of most other country’s pension programs. The fund now has about 55 % invested in stocks, 30% in bonds, 4% in cash and money market securities, 5% in real estate and 4% in private equity. WORKMENS COMPENSATION BOARD (WCB) We all are aware that the Government provides for on the job coverage for any accident, injury or work related sickness. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 61 History of the WCB Workers' compensation (or employees' compensation as it is called in the federal public service), was one of the first additional employment benefits established for federal public employees. This was in 1918, the same year that the charter for civil service employment, the Civil Service Act, was passed. This major advance was designed; it was said at the time, to place government employees on the same footing as employees in private industry. The original arrangement, whereby provincial workers' compensation boards look after the treatment of injured employees and adjudicate and pay compensation claims on behalf of the Government of Canada, continues to this day. The provinces are reimbursed for these and other services by Human Resources and Skills Development Canada. Human Resources and Skills Development Canada receives and processes claims from employees of federal departments and agencies. Claims are forwarded to the appropriate provincial authority, and Human Resources and Skills Development Canada is concerned with the provision of workers' compensation benefits for each claimant until a case has been settled. A file is maintained on each claim and other records are kept for accounting and statistical purposes. A general advisory service is provided to employees and their unions, as well as to employers, on the interpretation and application of the legislation. Since each claim for workers' compensation is highly personal, it should be dealt with promptly and with every consideration for the person involved. Each claim also being unique must be handled with attention to detail and be as accurate as possible. This can only be achieved if accident reports and other forms or material are carefully completed and submitted promptly. 62 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 What do the different Provinces call Workmen’s Compensation? Alberta Workers' Compensation Board British Columbia Workers' Compensation Board Manitoba Workers' Compensation Board New Brunswick Workplace Health, Safety, and Compensation Commission (WHSCC) Newfoundland Workers' Compensation Commission of Newfoundland and Labrador Northwest Territories and Nunavut Workers' Compensation Board of the Northwest Territories and Nunavut Nova Scotia Workers' Compensation Board Ontario Workplace Safety and Insurance Board Prince Edward Island Workers' Compensation Board Quebec Commission de la santé et de la sécurité du travail (CSST) Saskatchewan Workers' Compensation Board Yukon Workers' Compensation, Health and Safety Board Association of Workers' Compensation Boards of Canada Even though each Province has its own form of Workmen’s Compensation, they are all members of this Association. The Association of Workers’ Compensation Boards of Canada (AWCBC) was founded in 1919 as a non-profit organization. It was established to facilitate the exchange of information between Workers’ Compensation Boards and Commissions at a time when workers’ compensation law, policy and administration were in their infancy. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 63 There were six founding members: Ontario, Nova Scotia, British Columbia, Manitoba, Alberta, and New Brunswick. Saskatchewan joined in 1929, Quebec 1931, Prince Edward Island 1949, and Newfoundland 1950. Lastly, the Northwest Territories and Nunavut and Yukon Territory joined in 1974. Membership has expanded to include two honorary members, and a number of associate members who are interested and focus on activities consistent with the AWCBC's vision which supports the common goal of safe workplaces and healthy workers. ONTARIO For illustration purposes, we will highlight Ontario’s WSIB Over the past few years, there have been significant changes at the old Workers Compensation Board. They have a new name WSIB with a new focus on: Worker and employer self-reliance. Adjustments to the workplace accident plan. A goal to have a fully funded system by 2014. Under the Workplace Health and Safety Insurance Board, there will be a greater emphasis on accident-employer involvement in rehabilitation and return to work planning. They would like to have more worker co-operation in return to work planning, where the employee takes an active part in the process. There are new monetary changes to the benefits received. The compensation level will reduce to 85% of pre-injury average net earnings. There will also be an inflation-indexing factor: 1%, to a maximum of 4%. There will however be full indexing for 100% disabled workers and survivors. An important benefit change undertaken is to eliminate chronic occupational stress. There are new guidelines for chronic pain healing time as well as Benefit payment time. 64 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 2012 Premium Rates The 2012 average premium rate for Schedule 1 employers is $2.40 for every $100 of insurable earnings, an increase from $2.35 in 2011. This increase does not mean rates will increase for all employers. Premium rates for individual rate groups have been recalculated based primarily on injury frequency and claims costs for individual rate groups. Annual Maximum Earnings Ceiling The annual maximum earnings ceiling for 2012 is $81,700. Earnings over the annual maximum are not insured. GENERAL WORKMEN’S COMPENSATION GUIDELINES AND RULES Employees hired abroad Employees engaged locally in another country are divided into two groups for workers' compensation purposes: 1. Employees and their dependents, in a country that has a workers' compensation law, who are entitled to benefits because the employing department contributes to the country's compensation fund; 2. Employees and their dependents who are not entitled to workers' compensation under any local (national) law. To report accidents in the second group, refer to "Persons locally engaged outside Canada" under "Responsibilities of the employer". Employees on travel status As a general rule, employees are covered by the Act whenever they are traveling on duty, in Canada or abroad, as long as they are engaged in work for their department or agency at the time of injury. However, coverage is not provided during any departure from the itinerary that is for personal reasons. A compensation claim is handled by the province in which the worker is usually employed. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 65 Death occurring away from home When an employee dies as the result of an occupational injury or disease while serving at a location other than his or her usual place of employment, and the resultant charges exceed the amount of compensation payable, a supplementary payment may be made with the approval of Treasury Board. The additional expenses are usually for the preparation and transportation of the body. Particulars of any such claims should be sent by the employer to the appropriate Regional Injury Compensation Unit of Human Resources and Skills Development Canada, as soon as possible after the accident. Flying accidents compensation regulations When injured or killed while travelling on a non-scheduled flight (a flight in an aircraft that is not a private one and that is not operated on a scheduled flight), an employee or his or her dependent’s may make a claim either under the Government Employees' Compensation Act or under the provisions of the Flying Accidents Compensation Regulations. Any claims made under the regulations should be forwarded to the nearest office of the Canadian Pension Commission. The appropriate Regional Injury Compensation Unit of Human Resources and Skills Development Canada should also be notified of the accident. Right to choose your own doctor An injured person has the right to choose a doctor for the required treatment, but once the choice is made it must be adhered to. Permission to change doctors must be obtained in writing from the provincial workers' compensation authority except in Quebec where there is no such restriction. 66 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Benefits provided The nature and extent of medical treatment, the type of hospital accommodation, the scale of compensation for loss of earnings in cases of disability, and the rates of benefits for the dependents of deceased employees are the same as those provided in the Provincial Workers' Compensation Acts. For example, a federal worker employed in Ontario and injured while at work qualifies for benefits available in that province. Occupational diseases In each province, occupational diseases are recognized for workers' compensation purposes. In addition, regulations authorized by Section 8 of the Act provide a broader coverage in some instances for public service employees. Under these regulations, any disease, other than the occupational ones cited in provincial acts, that is due to the nature of the employment and peculiar to or characteristic of a particular process, trade or occupation in which the person was employed at the time the disease was contracted, may be compensated. In addition, the regulations provide for coverage of employees working abroad (other than locally-engaged employees) for diseases that result from the environmental conditions of the place outside Canada to which the employee was assigned. Disallowance of claims The most common reasons for disallowing a claim are the following: It is not shown clearly that the disability is the result of an accident, or occupational disease. The injury or occupational disease reported did not arise out of and in the course of employment. A description of an accident is given, but the disability is not the result of it. The injury reported is not substantiated by medical evidence. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 67 The employer will be informed by Human Resources and Skills Development Canada or a provincial workers' compensation board of the decision. The question of eligibility for compensation can be determined only by the workers' compensation authorities. Departmental officials do not have any adjudication authority but must report all work place injuries and occupational diseases, other than first-aid only incidents, to the appropriate Regional Injury Compensation Unit of Human Resources and Skills Development Canada. Rehabilitation services Federal government employees are eligible for rehabilitation services provided under the Provincial Acts. These include physical medical treatment and, in some provinces, vocational rehabilitation, with retraining for other work, in cases where the injury leaves the employee with a permanent disability that makes it impossible for him or her to resume his or her former occupation. Where desirable and feasible, there is specialized training in academic and commercial fields. Occasionally an injured employee is physically incapable of resuming usual duties because of injuries resulting from the accident. If the disability is temporary, every effort should be made, as soon as he or she is well enough, to assign the employee to work that is within his or her capabilities until such time as he or she is able to resume pre-accident duties. If the employee is permanently incapacitated to an extent that will not permit resumption of former duties, he or she should be assisted in every way to obtain work appropriate to his or her remaining capabilities. Review and appeals All jurisdictions allow an opportunity for reconsideration of unfavourable decisions. An employee, the employer or their representatives may ask for a review of a decision by directing such a request to the appropriate provincial authority. This request should contain sufficient new or additional evidence, usually medical, to warrant a review of the claim. 68 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Responsibilities of the employer Workers' compensation for occupational injuries and diseases is an employee's right, not a privilege, and it is the responsibility of the employer and Human Resources and Skills Development Canada to see that this right is protected. To enable Human Resources and Skills Development Canada to do its job effectively, the employer must report within three days all injuries involving medical attention or lost time. HRSDC determines whether the employer is covered under the Government Employees' Compensation Act and obtains required information on employee status. Claims are checked immediately for accuracy and completeness, countersigned, and then forwarded to the appropriate provincial workers' compensation authority. The compensation authority decides whether the disablement is the result of an occupational injury or disease, and determines the benefits to be provided. Immediate attention Employees who are injured should be given immediate attention. In order to minimize the severity of the injury the first priority is first aid and/or medical care. Should the employee need to be transported to a medical facility, transportation will be provided by the employer. Reporting injuries Each employer is responsible for establishing and disseminating appropriate departmental directives and instructions concerning the procedures for notification of occupational injuries or diseases. It is the responsibility of the injured employee to notify his or her immediate supervisor of the injury as soon as possible. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 69 In cases where, as a result of a work injury, an employee has had to obtain medical treatment outside of working hours, he or she should personally notify the employer immediately upon return to work, or by some other appropriate means if he or she is unable to return to work. Every employer is required to establish procedures and monitoring systems to ensure that all employee occupational injuries or illnesses that require professional medical care (beyond first aid) are reported to the appropriate Regional Injury Compensation Unit of Human Resources and Skills Development Canada within three days of their occurrence. Such injuries must be reported on the compensation form prescribed by the workers' compensation board of the province where the injured employee is usually employed. Compensation forms must not be sent directly to a provincial workers' compensation authority. The employer is required to maintain an accurate record of the date, type of injury, etc., for all minor injuries that involve first aid only, that is, those which do not require the services of a medical doctor. These records are to be retained in the work place for two years. Employers are reminded that in the case of first aid, injuries should not be reported to Human Resources and Skills Development Canada. If the employer does not agree with the details of the accident as stated by the employee, the employee's version must appear in the compensation form, but should be accompanied by appropriate comments regarding the employer's view of the circumstances. In addition, the employer may request an impartial investigation by the provincial compensation board. All compensation forms must be signed by the foreperson, supervisor, or other responsible person in charge who has first-hand knowledge of the occurrence. 70 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 The original signed compensation form and subsequent employer's reports are to be submitted by the employer in duplicate to the appropriate Regional Injury Compensation Unit of Human Resources and Skills Development Canada. Statistical information Records of accidents are essential to successful occupational safety programs just as records of production costs, sales, profits and losses are essential to the successful operation of business. To improve occupational health and safety, it is necessary to have accurate records of the incidence of work injuries and illnesses. This in turn allows occupational groups, departments or agencies to identify those problem areas that require immediate attention. Therefore, the compensation form should be filled out as completely and accurately as possible. Details such as an employee's age, the date current employment started, and the employee's wage or salary level (in cases where the injured person is or will be disabled beyond the day of the injury) should also be entered on the accident report. Employers are required to ensure that all compensation forms furnish complete and related details of the accident and the nature of the injury. For example, it is not sufficient to indicate in a general way that an employee injured him or herself or suffered pain. It should be stated whether the injury was a contusion, bruise, laceration, strain, etc. The specific part of the body which was injured and the cause of the injury should also be identified. Recurrent disability An employee may be absent because of the recurrence of a disability sometime after the return to work. Subsequent absences should be reported to the appropriate Regional Injury Compensation Unit of Human Resources and Skills Development Canada by means of an explanatory letter or an amended compensation form. The original claim and/or file number should be quoted if available. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 71 The claim is then referred to the appropriate provincial authority. When the employee again returns to work, an Employer's Subsequent Statement must be submitted. If the employee’s income continues When completing a compensation form involving time off from work, particular attention should be given to the item regarding amounts that have been paid or will be paid to the injured employee for the period of disability. If the employing department or agency intends to grant salary in the form of injury-on-duty leave, this should be indicated by stating either "Will be paid salary for period of disability" or "Will be paid salary if claim accepted by the compensation board". The Employer's Subsequent Statement, completed when the employee returns to work, and should also state the amount paid and the period for which the employee was paid salary. Injury-on-duty leave Public service employees are generally entitled to this type of leave through the employment regulations or through their collective agreement provided the claim is approved by the appropriate workers' compensation authority. Human Resources and Skills Development Canada is prepared to inform the employer of the workers' compensation authority's decision on each claim when the provincial authority does not do so directly. This service can only be provided satisfactorily when accidents are reported promptly. Failure to do so will in many cases cause a disruption in the injured employee's pay. When it is decided to stop granting injury-on-duty leave with pay to an employee who is still disabled, the employer should notify the appropriate Regional Injury Compensation Unit of Human Resources and Skills Development Canada at once. The office will promptly arrange for the employee to receive the applicable workers' compensation benefits until the claim is settled. 72 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Accident investigation report At least two distinct and separate procedures and reports are required where there is an accidental injury in the work place. Some confusion exists because of the overlap of these two reports. One is generated for compensation purposes and is injury oriented and it is the one referred to as the compensation form. The other report details the accident causes and recommends corrective action to make the work place safer. This second report is an "accident investigation report". Because of the differing purposes of these reports the employer is cautioned that a totally different approach must be used in completing the accident investigation report. Place of usual employment A claim for compensation is adjudicated by the province in which the employee is usually employed. For the purposes of the Act, this would be the province in which the employee has been appointed or engaged to work. For instance, an employee who is hired in Ottawa to work in Alberta would be considered to be usually employed in Alberta, whereas a person who usually works in Ottawa but who is sent to Alberta on a temporary assignment would still be considered to be usually employed in the province of Ontario. Also, the place of usual employment is not always the place of residence: for example, for an employee who resides in Gatineau, Quebec, but who is employed in Ottawa, Ontario, the province of usual employment is Ontario. Employee has a choice of action A workers' compensation law principle recognized in the Act is that workers' compensation is a substitute for common law action taken by an injured worker against his or her employer. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 73 However, when an employee's injury is caused by a third party, that is, a person who is not the employer or employer's servant or agent acting in the course of employment, the employee or his or her dependents have the right to elect (a) to claim compensation under the Act, or (b) to bring an action against the third party. Employee takes action Under the Act, an employee is protected up to the full amount of compensation to which he or she is entitled whether he or she elects to claim compensation or to bring an action against the third party. If an employee, as a result of an action, recovers less than the amount to which he or she was entitled under the Act, he or she may be paid the difference between what was actually obtained through the action and the amount of compensation for which he or she was eligible. If the case is to be settled out of court, then the employee must, before making a final settlement with the third party, submit the proposed settlement to Human Resources and Skills Development Canada for approval by the Minister of Labour to be eligible for this difference. However, if the settlement is by a court judgment, then no prior approval by the Minister is required. Employee claims compensation In most cases, the injured employee chooses to claim compensation under the Act and thereby subrogates Her Majesty to the rights under it. Where the circumstances appear favourable, Human Resources and Skills Development Canada endeavours by various means to obtain a settlement directly with the third party. In the more serious and complicated cases, action for recovery may be taken in the courts by the Department of Justice. Should the amount recovered and collected from the third party exceed the amount of compensation to which the employee or his/her dependents are entitled under the Act, Human Resources and Skills Development Canada may pay to the employee or dependent’s a portion of the excess. 74 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 However, this payment may be deducted from any subsequent benefits to which the employee or dependents might become entitled under the Act for the same accident. Full information is required To institute a court action or to make a demand for payment from a third party; a complete description of the incident must be supplied promptly to Human Resources and Skills Development Canada. It is essential to a proper evaluation of the case that these details include the following: A written statement from the claimant which includes the time, date, place and full description of the accident. Statements from witnesses (photographs taken at the scene if possible). A police report where applicable, which is treated as confidential. A coroner's report, if the accident was fatal and an inquest was held. Except in provinces with no-fault legislation, if an automobile accident is involved, the name and address of the owner of the car and of the driver if it was operated by someone other than the owner, the registration number, the province and year of issue, and a statement about the insurance carried on the vehicle involved. If injuries are caused by an accident on private property and the injured person is lawfully on the property at the time, give the particulars of the hazard or defect causing the slip, fall or other condition, or the event leading to the injuries. State if there had been a previous complaint to the owner or occupant of the premises about the hazard or defect. Describe the weather conditions if they were a factor. If, as in the case of a letter carrier, there was an attack by a dog, state whether the dog is considered vicious and had been known to attack another person. State if liability insurance is carried on the property. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 75 ANOTHER EMPLOYEE BENEFIT ADD ON Many employee benefit plans are now carrying some form of an additional add on medical referral system. There are a few operating in the Canadian marketplace today. Best Doctors Best Doctors® was founded in 1989 by renowned professors of medicine affiliated with Harvard Medical School and by a 16-year survivor of a serious illness. This unique partnership of medical expertise and patient insight created a company committed to providing services to help people with serious medical conditions. Today, Best Doctors® is the world leader in connecting people with the best medical care. Using its renowned database of over 50,000 doctors recognized as the best by top specialists, Best Doctors® provides immediate access to the best medical knowledge and peace of mind to millions of people around the world. Best Doctors® services are available worldwide, serving more than 10 million lives in 30 countries. Through access to top-ranked hospitals, the latest technologies, opinions of worldclass specialists and personal care management, Best Doctors® can help people make informed decisions about your healthcare when it matters most. Best Doctors can help the employee: Have an expert take another look at the employee’s diagnosis, without the employee having to leave home. Identify an appropriate treatment. Support the employee with information to make the right choices. Best Doctors does not replace your relationship with your current physician and health plan. Rather, they offer additional resources, education and support to you and your treating doctor. Best Doctors services are included as part of your benefits plan and it’s strictly confidential. 76 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Membership is sponsored by the employer or health plan. The Right Expertise is Available An employee can harness the expertise of the exclusive Best Doctors database, bringing the clinical knowledge of world class experts to the problems of people with serious illnesses. They provide specific diagnosis and treatment recommendations. The employees enjoy valuable insights from top experts and constant guidance and support from Best Doctors dedicated nurses – without leaving home. The Right Outcome Best Doctors works with the patient’s treating doctor to ensure that recommendations are implemented. By making sure that employees get the right care, Best Doctors reduces complications and helps avoid ineffective treatments: Treatment modified 61% of the time. Diagnosis changed 22% of the time. 67.3% of members avoided one or more invasive surgical procedures. $287,567 average reduction of inappropriate medical costs on catastrophic cases. $69,200 average savings on rehabilitation expenses on catastrophic cases. What types of services does Best Doctors offer? Best Doctors provides a unique combination of information and access to the best medical care to members faced with a serious illness or injury. Services include a comprehensive review of a patient’s medical records to reaffirm or redefine the original diagnosis and to recommend treatment protocols, as well as access to the most qualified specialists and facilities worldwide. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 77 How does Best Doctors determine who “the best” are? Best Doctors believes that physicians are the most qualified to evaluate the experience and skill sets of other physicians. The Best Doctors survey asks physicians, “If you or a loved one needed a doctor in your specialty, to which you would refer them?” The responses form the basis of the Best Doctors global database, which is consistently recognized by doctors, patients and the public for its quality, integrity and independence. So What Does the Best Doctors® services provide? INTERCONSULTATION™ An in-depth review of the member's medical files to assist in the development and confirmation of the diagnosis and to help develop a treatment plan. Members and their physicians will have access to the latest technologies and opinions of world class specialists. With a fast and detailed turnaround of results, the InterConsultation process can reduce potentially serious complications that can result from a misdiagnosis and help the member's treating physician determine the proper course of action. FINDBESTDOC™ A customized search across a constantly updated global database of over 50,000 specialists who are best qualified to meet the member's specific medical needs. Members will have access to a Personal Advocate, who will work with physicians affiliated with the world's leading medical institutions, to help explain their options and determine the best care provider for the member's specific condition. FINDBESTCARE® While the member is receiving medical care, Best Doctors will review the necessary information provided by the medical specialists involved and will continually monitor the treatment process to help ensure the member's medical priorities are met. 78 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 If the member travels away from home to receive treatment, Best Doctors will assist with reservations and accommodations for the member and family. This can help reduce the stress of receiving the care the member needs while away from home. What medical conditions are covered? Best Doctors services are available for the following Medical Condition(s): AIDS, Alzheimer’s disease, Blindness, Benign Brain Tumor, Cancer, Cardiovascular Conditions, Coma, Deafness, Kidney Failure, Loss of Speech, Multiple Sclerosis, Major Organ Transplant, Major Trauma, Motor Neuron Disease, Parkinson’s disease, Paralysis, Severe Burns, and Stroke. ADMINISTRATIVE SERVICES ONLY (ASO) An arrangement whereby an insurer agrees to provide services to a self-insured entity, such as providing printed claim forms, and processing and auditing claims. The insurer does not assume any insurance risk under an ASO arrangement. An ASO plan enables large employers to assume the costs of their health insurance, dental care and short-term disability insurance benefits. These benefits can even include insurance that limits the employer’s liability in the event that one or more exceptional disasters strike the company. An Administrative Services Only (ASO) Plan is basically a self-funded insurance plan. The employer is totally liable for all financial and legal aspects of the employee benefits plan. In other words there is no insurance element under these plans. Employers recognize the high degree of risk associated with "true" ASO plans. This is the very reason that most employers would use a combination plan that would eliminate the "risk" part of the group benefit plan. Specifically, Life Insurance, AD&D, Dependent Life and Long Term Disability would be insured using one of the insurance carriers. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 79 The so-called "experienced" benefits including Extended Health Care, Dental Care and Short Term Disability would be covered using ASO. Please note that ASO plans would not include Out of Province/Country Insurance. Plan Administration and Adjudication Typically it is the insurer, Third Party Administrator and/or broker who can administer and adjudicate the benefit plan. Liability or Risk There is no insurance element in these types of plans and therefore it is the employer bearing full liability for claims incurred under the plan and any claims litigation that could result from it. In case of an insured plan any legal liability would be directed against the insurer; in the case of an ASO plan any lawsuit would be directed against the employer. Advantages of ASO Introduction of an ASO plan may present the employer with substantial savings. First of all there is no premium tax charged on the ASO part of the premium. The employer would also save the "risk" charge ranging typically at 0.5% to 2%. Further, because there is no liability to the insurance company upon plan termination, the so-called Incurred But Not Reported (IBNR) reserve is eliminated. Stop-Loss Arrangement Insurance carriers offer Stop-Loss Insurance as a protection against unfunded financial liability that employers would be faced with when using ASO plans. Claims that would be in excess of the agreed limit (stop-loss) would become the responsibility of the insurer. The use of a Stop-Loss provision however does not change the self-funded principle/status of an ASO Plan. 80 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Conclusion Group Benefit plans that include ASO are growing in popularity given the fact that health and dental premiums are constantly rising. COST PLUS PROGRAMS Cost plus is a claims payment service used by an employer to reimburse an employee for claims not covered under their current benefit plan. Rather than amend a plan for an uncovered claim, the plan administrator pays for the "Cost" of the claim "Plus" an administrative fee. In simple terms, Cost Plus is merely a claims payment facility used by a plan sponsor to reimburse an employee for claims not covered under the terms of their current benefit plan. Traditionally, Cost Plus is used, as an executive perk on an as needed, claim-by-claim basis. As an example, an executive of the company spends $4,000 for major dental work, and their current plan covers major dental at 50% to an annual maximum of $1,500. Therefore, a $4,000 claim will be submitted and the insurer will pay only $1,500, forcing the executive to pay the dentist the remaining $2,500. Rather than amend the plan to cover this particular claim, the plan administrator can opt, to have the balance of the claim paid on a Cost Plus basis. In turn the insurer will invoice the company for the cost of the claim, administration (typically 10% - 15%) and applicable taxes. Once paid, the insurer will issue a reimbursement check to the claimant. As is the case with group insurance premium, the Company’s expenditure for the Cost Plus claim is an eligible business expense. Furthermore, the executive would receive the additional $2,500 on a tax-free basis, allowing for 100% coverage of the claim. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 81 Assuming the executive’s marginal tax rate is 50%, the Company would have to expend $5,000 plus any applicable payroll taxes to provide enough after tax dollars to the executive to pay the claim. Through the use of Cost Plus facilities, the Company’s expenditure can be reduced to $2,500 plus a 10% administration fee and any applicable taxes. HEALTH CARE SPENDING ACCOUNTS (HSCA’s) Unlike the Cost Plus programs that are used at the Company’s discretion, a Health Spending Account is a Company paid annual allowance to be used at the employee’s discretion. A Health Spending account is simply an allowance that is given to employees to supplement their current benefit plan, to cover items that are not covered or partially covered under the existing plan. These allowances cannot be subjectively based; rather they must be established by pre-determined criteria such as a predefined calculation or formula created by the employer. Formulas can be a simplistic as a flat amount or determined by such factors as class, single / family, years of service or percentage of payroll, just to name a few. Based on these limits, a monthly rate will be established for invoicing purposes, to ensure complete funding of the Company’s Limited Cost Plus commitments. Health Care Spending Account (HCSA) is growing in popularity with both employers and employees. Unlike traditional group insurance plans that offer little or no flexibility HCSAs are considered to be the ultimate in flexibility that benefits programs can offer. Setting up a Health Care Spending Account Like other employer sponsored benefit plans; a Health Care Spending Account must resemble a true form of insurance in that some element of insurance risk must be incorporated into the account. In addition, a Health Care Spending 82 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Account must be structured like a Private Health Services Plan in order to meet the requirements of Canada Revenue Agency (CRA). A Private Health Services Plan must: Be the undertaking of one person that is used, To reimburse another person, For an agreed consideration, From a loss or liability in respect of an event, That is not certain to happen. As with Health and Welfare Trusts there is no formal registration procedure for a flex program and no requirements that the plan documents be submitted to Canada Revenue Agency (CRA) for approval prior to implementation. Tax rules require that benefits plans be implemented and administered in accordance with written document, typically in the form of a benefit guide that specifies certain information. Employees must have access to this document. Depending on the particular benefit and how it is paid for, it may result in a taxable benefit to the employee or a non-taxable benefit. As long as the Health Care Spending Account meets the requirements of the private health services plan (as previously defined by CRA) then employer contributions are excluded from employee’s income and it can retain preferential tax status as an insurance plan. Health Care Spending Accounts do not trigger E.I. or C.P.P. premium/contributions and if employee already paying maximum, offering a Health Care Spending Account will not reduce cost to organization. Health Care Spending Accounts do not earn interest. If the employer is thinking of offering a Health Care Spending Account in house, they need to be aware that the new federal privacy legislation will place heavy obligations on in-house staff to keep health information private & confidential. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 83 For this reason, it may be advantageous to seek the assistance of a third party administrator to assist you in implementing your Health Care Spending Account. Funding a Health Care Spending Account According to Canada Revenue Agency (CRA), if a Health Care Spending Account is offered as a stand-alone item in a traditional plan that offers no other element of choice making, it must be funded through direct employer contributions. Health Care Spending Accounts within a full choice-making flexible benefit program, can be funded by both employer and employee contributions. As part of a full flexible benefit plan, employees fund their Health Care Spending Account with unused flex credits from their flexible benefit plan. Revenue Canada views flexible credits as employer benefit premiums, not employee earnings. About Employee Funding If employees supplement their Health Care Spending Account by making payroll contributions, it defeats the purpose of the Health Care Spending Account with respect to purchasing power. This is because payroll deductions are subtracted from an employee’s pay cheque after tax has been deducted from income. For example, if an employee wishes to have $240 in payroll deductions deposited into the Health Care Spending Account, the $240 in after-tax money, in reality represents $400 that the employee had to earn, assuming a 40% tax bracket. If employees are funding their Health Care Spending Account through flex credits, They must decide once annually how many credits they will allocate to their account. The employer must consider if a limit should be imposed on the number of flex credits that can be deposited into an account. Once the decision has been made, this allocation decision is irrevocable, unless employee’s family status has changed due to reasons such as a marriage or birth of a child. 84 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 About Employer Funding Generally employers choose a defined contribution approach to funding Health Care Spending Accounts, whereby a set amount or percentage of salary is deposited into the Health Care Spending Account. Some alternatives for employer funding include the following: Increase the corporate budget to enhance employee benefits; Reduce other elements of the group insurance plan, if applicable (e.g. coinsurance from 100% to 80%); Changes in cost sharing arrangements of existing employer sponsored group insurance plans so that employees pay the health care premium and the employer contributes an equal amount to a Health Care Spending Account; Option for an employee annual bonus; The employer in lieu of a raise provides funding for a Health Care Spending Account It is not necessary for money to be deposited in a trust fund nor assets separated. The employer may create a book account for an employee’s Health Care Spending Account in which credits and debits can be tracked. When are Flex Credits Allotted? It is at the discretion of the employer as to whether the entire allotment of credits will be deposited into the account at the beginning of the year, or over intervals (monthly or quarterly). There are advantages and disadvantages of each method. The most common method is the annual allotment of flex credits. In addition to easier administration of an annual allotment of flex credits, the entire amount is available at the beginning of the year for those employees who need it. If flex credits were deposited monthly or quarterly, the employee may be required to pay out of their pocket for expenses that exceed their account balance, consequently, if the entire amount is available, the employee may use all of his/her credits at the beginning of the year and have nothing left to draw on for the rest of the year. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 85 In addition, if all of the credits are allocated to the account at the beginning of the year, the employer could be at financial risk of an employee exhausting all of his/her funds in the account and then terminating employment before the end of the year. Conditions and Requirements for Health Care Spending Account Funds Funds allocated to a Health Care Spending Account must be used to reimburse expenses incurred during that year. There can be no “cash out” of the plan. Unused flex credits can be dealt with in one of two ways Use it or lose it” 1. Any remaining amount in the account at the end of the plan year is forfeited and returned to the employer OR 2. Carry-Over or Rollover Feature Unused flex credits will be rolled over for the following 12 months (without any tax consequences to the employee). Unused flex credits can be rolled over a maximum of one year. Flex credits rolled-over from the prior plan year are used up first before the flex credits deposited for the current plan year. This minimizes the chances of forfeiting the rolled-over flex credits at year-end. The Health Care Spending Account must incorporate a “use-it-or-lose it” feature for unused flex credits for all terminations, retirements, deaths and leaves of absence that last longer than 30 days. Claims Administration The Employer, a Third Party Administrator or the Insurer can handle the Claims Administration process. All claims must first be submitted through the Employee’s or Spouse’s Group Insurance plan and through the Coordination of Benefits process prior to being submitted to the Health Care Spending Account. Regardless who incurred the expense, the employee must sign the claim form. 86 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Claim form and proof of payment is submitted to the employer for reimbursement. (If claim has gone through group insurance, attach “Explanation of Benefits” from Insurer). Employer evaluates if the claim meets requirements (expense is eligible and if there is enough flex credits to cover and claim is either approved or rejected). If it is approved, they send the cheque. It is rejected; they then send an explanation to employee. Employers typically provide covered persons with a grace period of usually one to three months after the year-end to submit expenses for reimbursement. Once claims are no longer accepted, any unused balance in the account is either forfeited or rolled over the following year, depending on the design of the account. Employees are given a certain length of time to submit all year-end claim expenses. The norm is 90 days. Quarterly reports can be provided to an employer by the Third Party Administrator or Insurer, indicating claims paid out of the spending account, account balances, and any unused account dollars forfeited at year-end. The Employer has the option to decide how reimbursements will be made from the Health Care Spending Account, the frequency and the minimum amount of expenses that should be submitted (i.e. $50.00 minimum). Costs The costs of the plan will include the cost of medical services and products plus premium tax and sales tax. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 87 In addition, the following expenses are required if your plan has Third Party Administration: Claims administration – set by insurer/plan administrator General administration – set by insurer/plan administrator Claims and general administration costs would include: Ongoing administration by insurer/plan administrator; Standard reports; Ongoing inquiry/service through plan administrator; ASO (Administrative Services Only)/Cost Plus accounting and reconciliation (if administration is provided through insurance company); Monthly tape updates of credit/eligibility information from plan sponsor, as applicable; Production of employee cheques; Year-end listings (where applicable) of payments made to members from accounts covering taxable items. The Employer is usually responsible for paying the administration expenses; otherwise, they must be deducted from the employees’ spending account dollars, giving them less to spend. Sample Tax Calculation for Health Care Spending Account Benefits Paid Jane Doe submitted a claim for $300 under her Health Care Spending Account. The tax would be calculated as follows: Premium Tax $300 X 2% = $6.00 Retail Sales Tax $300 X 13% = $39.00 Total Tax = $45.00 88 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Jane Doe will be reimbursed $300 and the Health Care Spending Account will be debited $345.00 Covered and Ineligible Expenses Covered Expenses If a Health Care Spending Account is added to an employer's existing Group Insurance Plan, flex credits can be used to pay for co-insurance not paid by the employer benefit plan, deductibles, or amounts that exceed plan maximums. In addition, a Health Care Spending Account may cover expenses that are generally not covered under a conventional plan. A partial list includes: Insurance premiums paid by the employee or the individual’s spouse for private health and dental plans; Cosmetic medical and dental treatment; Over the counter drugs, provided they are prescribed by a physician; Drugs for conditions sometimes excluded under conventional plans such as erectile dysfunction, fertility, obesity and hair loss; Laser eye surgery; Professional services of a dietician, acupuncturist or Christian Science practitioner. Dental Care (preventative/restorative/orthodontic); Facilities and Services – alcohol/drug addiction, nursing home care, special school, institution for mental or physical handicap, licensed private hospital, semi-private or private charges in a hospital, care of a person who has been certified as mentally incompetent, care of a blind person, full-time attendants in a nursing home; Medical Equipment and Devices. A complete list of eligible expenses is available through the Canada Revenue Agency (CRA). Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 89 Ineligible Expenses Ineligible expenses will include any medical expenses that are not considered to be deductible from income under the Income Tax Act, such as: Premiums paid to provincial medical or hospitalization plans; Medical costs for which the employee is reimbursed or is entitled to be reimbursed through other plans; Air Conditioners, humidifiers, dehumidifiers, heat pumps or heat or air exchangers; Non-prescription birth control devices; Antiseptic diaper services. Who can be covered as a dependent? According to CRA, a wide range of dependents is covered under Health Care Spending Accounts. A dependent can be another relative who resides in Canada at any time during the year, for whom the employee is claiming a tax credit that year. This individual must be the plan member’s parent, grandparent, grandchild, brother, sister, uncle, aunt, niece or nephew. Factors to consider before starting a Health Care Spending Account: Is a Health Care Spending Account the right fit for the organization? Will setting up a Health Care Spending Account align with corporate objectives? Will Health Care Spending Accounts meet the needs of your workforce? Do employees expect and want their plan sponsor to take care of all their healthcare needs, or are they looking for more flexibility and control? Is your objective benefit enhancement or cost control? Will the employees' perception of the value of the benefit be worth the amount of administrative effort a Health Care Spending Account will require? Where will the funds come from? (new employer money or flex credits freed up from benefit trade-offs, or both) How much is available? Are there any limits that should be set on accounts? How will you handle any forfeiture? 90 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 What limits will you place on the flex credits that employees can deposit (only applicable if the Health Care Spending Account is part of a full flexible benefit plan). Limiting the number of flex credits an employee can contribute can limit the risk to the employee of individual forfeitures or rollovers of flex credits. How will you handle unused funds at year-end - use it or lose it...or a rollover? Method of reimbursement – employers should incorporate features that will facilitate administration. Generally, a limit on how often reimbursement may be received and a minimum total of expenses that should be submitted will ease the work of the plan administrator. How will you communicate the plan? Communication is essential to the success of any benefit plan. Advantages of the HCSA Increased flexibility allows employees to have more control over their benefits, better meeting their needs and consequently increasing morale and job satisfaction. Employers can use Health Care Spending Accounts as an Attraction and Retention tool in today’s competitive marketplace. Employers can offer new types of health related benefits to employees without being locked into potentially expensive benefits. Employers can deliver benefits tax effectively. Employees can claim for expenses which otherwise may not have been covered. A wider range of dependents can be covered under the plan. A Defined Contribution approach allows employers to have better control and predictability over their costs. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 91 Unlike some conventional plans, Health Care Spending Accounts generally reimburse 100% of allowable expenses for a broad range of dependents with the only maximum being the flex credit limit of the Health Care Spending Account. If being used in conjunction to a conventional plan, the implementation of a Health Care Spending Account can soften the impact of employee cost sharing in the conventional plan. There are no renewals, reserves or inflation factors to contend with. Because dollars in a Health Care Spending Account are limited, employees are more accountable and are motivated to spend wisely. Disadvantages of the HCSA Stand-alone Health Care Spending Account may not meet the requirements of an employee who has significantly high medical expenses. Administration time and costs could be high with implementation of a Health Care Spending Account. PRIVATE HEALTH SERVICES PLANS (PHSP) FOR THE NEW MILLENIUM Employee benefits are constantly changing as to what benefits to provide and how best to set them up for Employees. Traditional health benefit plans could appear to be restrictive by their nature and tend to force employers into a pre-designed package that may or may not be right for each employee. Premiums are constantly rising; coverage is being restricted as well as tax consequences for group plans may not be available for the small business market. In Canada, certain employment benefits are not taxable even though they may be deductible to the employer. There is now an incentive to employers to provide these benefits since after tax returns are greater than straight salary to the employee. Dental and health benefit plans provided by an employer to an employee are considered tax-free benefits. 92 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Small companies can now offer health benefits tax-free to their employees, while deducting this cost as a business expense, without having a complex Employee Benefit package. Many companies now offer plans designed in accordance with Canada Revenue Agency (CRA) guidelines. A cost-plus health plan that allows pre-tax corporate dollars to pay for its employee’s health care costs. This type of plan maximizes the opportunity to fully utilize virtually 100% of all health and dental services and, at the same time, merge with existing Canadian tax laws. The term, private health services plan, ordinarily applies to some or all of the following: Extended medical insurance, such as prescription drugs and semi-private hospital rooms. Dental benefits, Vision or eye care benefits. In order to be considered a benefit the plan must cover either medical or hospital expenses such as: Payments to a medical practitioner, nurse, dentist, public or private hospital for medical or dental services, Remuneration for attendant care or the cost of full-time care in a nursing home or other institution, Transportation of patients to or from hospitals, by ambulance, A patient, and if required an attendant, has to travel to obtain medical services not available locally; Fares paid for trips in excess of 40 kilometers, Reasonable costs where no such transport was available, for trips of 40 to 79 kilometers, or reasonable costs for trips of 80 kilometers or more, Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 93 Medical aids such as artificial limbs or eyes, wheel chairs, crutches, braces, trusses, speaking or hearing aids, iron lungs or oxygen tents or artificial kidney machines, Products, such as diapers, required because of incontinence caused by illness or injury, Prescription eye glasses or contact lenses, Seeing eye dogs for blind, deaf or impaired persons, including maintenance and training, Reasonable expenses for bone marrow or organ transplants, including a person to accompany the patient and costs to arrange the transplant, Reasonable renovation costs related to access to or mobility within the home of a patient who lacks normal physical development or who has a severe or prolonged mobility impairment Reasonable expenses for the rehabilitation of a person suffering hearing or speech loss, including lip reading or sign language training, A wide variety of medicines, equipment, aids, devices prescribed by a medical practitioner and related to physical impairments, conditions or syndromes (see Federal Income Tax Regulation Section 5700 for a full list), Laboratory tests, radiography or other diagnostic procedures as prescribed by a medical practitioner, and Payments to a dental mechanic, or elective surgery. To be a formal plan there must be an element of risk. Under federal jurisdiction employer contributions to private health care plans are not taxable. Neither is benefits received by the employee from the plan. In Quebec, the employer contribution to private health plans is taxable. Traditional premium paying health and dental plans offer true insurance with various degrees of coverage, depending on the specific plan the client expects to use. The Insurance Company is most often inclined to insure the larger groups. As a result, the smaller companies have ineffective plans in place. 94 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 In some scenarios, Employee Benefits may not even be made available to them, while the only alternative would be an Individual insurance plan to cover the expenses. This can result in a higher premium cost. Comparison of a Traditional Employee Benefit Plan and a Private Health Services Plan Traditional Plan Private Health Service Plan High cost premiums No premiums – No monthly payments Regardless of use, you pay premiums No medical bills – No cost to you Enrollment requirements are set by insurer Employer sets requirements Yearly and lifetime limits No limits Reimbursement limits No deductible Clauses – you set limits Numerous health costs not covered 100% coverage on all health service costs Dental premiums are 70% of premiums Delete high cost dental premiums with pre-set limits. Refusal of claims Easy claims process Up to six weeks claim process Usually a quick turnaround Premiums MAY be deductible All payments for medical services are 100% deductible. These types of plans would interest the following groups of individuals: A one-person corporation or a processional corporation. Small business corporation (2-10 employees). Mid-size firms (10-30 employees). Large companies (30+ employees). Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 95 It would also be a benefit to consider the level of income. The higher the income, the greater the benefit to the Insured individual. What determines if a plan is a PHSP? According to the regulations as set out in the Income Tax Act of Canada, a Private Health Services Plan qualifies if it meets the following criteria: Under Section 6(1)(a)(I) of the Income Tax Act a plan qualifies if expenses that are allowed to be paid also qualify for a medical expense tax credit (IT-519R). Coverage for dependent as defined in the Tax Act (same sex spouses). Benefit elections must be made prospectively. If choices are made after the Plan Year starts, some amounts may be subject to tax. Benefit elections are irrevocable for the Plan Year – prospective changes are allowed for changes in family status. Tax consequences to Employer and Employee Employer Contributions made to the Plan by an employer using the accrual method of accounting will be deductible for tax purposes in the taxation year in which the legal obligation to make the contributions arose. Employee The employee will not be considered to have received a taxable benefit from employment so that there will be not tax consequences as a result of being a member of the Plan. 96 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Conditions that must be followed to be a PHSP In order to meet the definition of a PHSP as set out in the Act, several conditions must be met by the Plan: 1. The funds of the PHSP must not revert to the employer or be used for any purpose other than providing qualifying benefits to the employees. 2. Customs Revenue Agency (CRA) has indicated that the non-reversion and exclusive use requirements of a PHSP effectively require the relative trust document: 3. “Contains a clause that no property of the trust, whether such property is acquired from the capital or income of the trust, shall be invested in the shares, notes, bonds, debentures or similar indebtedness issued by: The employer, A person who does not deal at arm’s length with the employer, or A person who is a member of a group of persons not dealing at arm’s length with the employer. Nor shall any such property of the trust be invested in property which is or will be used directly or indirectly, solely or otherwise, by the employer or any person who does not deal at arm’s length with the employer or who is a member of a group of persons not dealing at arm’s length with the employer.” The plan does not specifically address the reversion issue although that because the employer contributions do not exceed the amounts required to provide the benefits, there would normally be no excess funds that could revert to the employer. The trustee must act independently of the employer; that is, the employer must not have control over the trust. The employer’s contributions may not exceed the amount required to provide the benefits. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 97 The payments by the employer cannot be gratuitous but must be legally enforceable by the trustees of the arrangement. Employees in the Plan have a legally enforceable claim against the employer by virtue of their contract of employment. The Plan must have an element of insurance. CRA has accepted that a selfinsured arrangement similar to the Plan may qualify as a PHSP. CRA has indicated that where employees are reimbursed up to a certain dollar maximums each year and are permitted to carry forward excess claim or unused reimbursement room to subsequent years, such a plan may not qualify as a PHSP. However, where the Plan permits the carry forward of either the unused allocation or eligible medical expenses for a period of up to twelve months, the Plan will be considered to have the necessary element of insurance. The Plan allows the carry forward of unused benefits for a maximum of one plan year. Therefore, this requirement is met. CRA will recognize a PHSP that provides any or all of the coverages for expenses, which would normally qualify as medical expenses under the relevant provisions of the Act. The amounts paid by the Plan must be paid for one or more of: The employee The employee’s spouse, and Any member of the employee’s household with whom the employee is connected by blood relationship, marriage or adoption. In order to be deductible by the employer, the amount of coverage must be reasonable in the circumstances taking into consideration such factors as employment status and term of service of the employee. 98 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 If non-arm’s length employees are included in the plan, then coverage should be comparable to that which normally is offered to employees in an arm’s length situation. If it is in fact necessary to be a shareholder in order for the corporation to pay for coverage under the plan and employees who are not shareholders are not provided with similar coverage. It will normally be reasonable to conclude that the employee-shareholder has obtained the benefit by reason of his or her shareholdings and not by reason of employment. The normal exclusion for benefits under a PHSP would not apply and the individual would be considered to be in receipt of a taxable benefit. “On the other hand, when equivalent coverage under a PHSP is extended to all employees, including the employees who are shareholders, the benefit provided to the employee-shareholder from such coverage is normally considered to be an employment benefit rather than a shareholder benefit. Similarly, when all employees of a corporation are shareholders and it is reasonable to conclude, based on the particular facts of the situation that the RHSP has been provided as a part of a reasonable remuneration package the benefit from such coverage is also considered an employment benefit rather than a shareholder benefit.” The result would be that the benefit is excluded from the income of the employeeshareholder. PHSP’S are not for everybody, but they really do offer an alternative for anybody who is self-employed or who owns a business of any size. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 99 The result is that these plans could be used either on their own, or in combination with existing Employee Benefit Plans to complement their coverage’s, and at the same time control premiums. Future Health Care Costs Still Worry Many Canadian Employers A survey by Morneau Sobeco shows that rising health care costs is a prime concern for 58 percent of Canadian employers. Rising health care costs are prompting 18 percent to review cost sharing, and 27 percent plan to review disability benefits. Some employers are now offering their employees more money to purchase Health and Dental Insurance on their own. INDIVIDUAL HEALTH & DENTAL INSURANCE PLANS The health-care system in Canada ensures that virtually everyone living here has access to medical services in any part of the country. You likely have a provincial health card that gets you into doctors' visits, hospitals, covers various blood tests, X-rays, and other medical procedures. As lauded as the Canadian system is, it doesn't cover everything. With a few exceptions, provincial plans don't cover dental care or pay for medications received outside of a hospital. These plans also won't pay for glasses or contact lenses. That's why many of us turn to private plans purchased by our employers or, increasingly, to individual private health-care plans. Unlike the emergency health insurance you may consider buying when you go out of the country on vacation, regular individual health insurance is designed for the day-to-day troubles, surgeries, and treatments that, while routine, can add up to big bills. Responding in part to the changing workforce where more people are working on short-term contracts or for themselves, insurers are offering a variety of healthcare packages to cover the needs of individuals and their families. 100 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 What started as a basic plan has become a virtual buffet of services where consumers can choose which benefits they want and need. If you work for a company that offers health-care but not dental-care benefits, for instance, you can purchase your own dental benefits. If you have prescription needs but can't afford a full package, choose a basic health plan including a drug plan, and skip the dental or vision portions. If you have a growing family and want as much coverage as possible, order the works. There are also some packages designed for health-care catastrophes that would pay much more than the regular plans for serious illnesses that would result in substantial drug or therapy charges. The choices are improving and, for some people, the cost of health insurance can be used as a tax deduction. Of course, wanting insurance and getting it are two different things. Insurers will have you think that everything is simple. One brochure insists you can enroll in a plan in five easy steps and in less than 10 minutes. Well, maybe it's that simple if you are young, in excellent health, want very basic service, and have no interest in the details. For the rest of us, it makes more sense to pick up the phone and ask questions. Lots of them. You won't want to be sorting out misunderstandings when you are sick. Take care of it before you sign up and keep notes, so you will remember your understanding of what you bought. Health insurance plans usually provide coverage for serious diseases that by their very nature can be unpredictable and catastrophic. Medical treatment can be extremely expensive and a purchased individual health insurance plan can help relieve tension to some extent. This is not say that health insurance plans do not cover routine check-ups and common ailments. The point is that even if companies provide group insurance plans, it is better to safeguard yourself for the future. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 101 Most plans provide limited coverage and if you decide to opt for the ones with greater benefits, the cost factor might become an issue. This is a situation that calls for utmost discretion and it is for you to perform the balancing act between cost and coverage- you cannot go beyond the budget, but good health too is of utmost importance. Most companies provide group dental insurance coverage to their employees as a major perk to keep their employees happy. Because of the large number of employees, the insurance companies are able to provide greater coverage at reduced rates. People with group dental insurance plans do not require additional individual dental coverage. This is not so with health insurance. Even if the company provides medical coverage, buying individual health insurance is a safer option that will prove beneficial in the long run. For many reasons, millions of Canadians are without an employer group health plan, and therefore vulnerable to health care costs not covered by their Government Health Insurance Plans so supplemental health care coverage should concern them. ALL PLANS ARE NOT THE SAME All health plans are not created equal. And there's no rule of thumb for which ones are good and which ones aren't. The best plan for one person may not work at all for another. The best plan for you will depend on just what kind of health care you need, whether you have family members and what their needs are, and a few other personal factors. Features and options vary widely among types of plans more so than among companies providing the plans. Where things vary among companies is usually cost - depending on your personal circumstances, some companies' rates may be less than others. 102 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 But you don't need to be an expert, or even spend a lot of time, to figure out which plan type is best for your needs. Understanding which type of plan offers the things you want should make a decision pretty easy. INDIVIDUAL HEALTH & DENTAL COVERAGES It doesn’t matter if you choose Blue Cross, Manulife, Green Shield or one of the many Managing General Agents who market Individual Insurance coverage’s as the core products are going to be the same. Of course as mentioned earlier, premiums and coverage’s will vary from supplier to supplier. Extended Health Benefits Extended Health Benefits include coverage in Canada for: accidental dental; ambulance and ambulance attendants; diabetic supplies and equipment; hearing aids; medical supplies and equipment; orthopedic shoes; ostomy supplies; other practitioners such as physiotherapists, psychologists, chiropractors and speech therapists; oxygen and oxygen equipment; private-duty nursing; prosthetic appliances and speech aids. Hospital Benefits Some plans will pay the eligible expenses for a semi-private room, in excess of the amount paid by provincial health care plans for Blue Cross cardholders. Traditional Dental Benefits Traditional Dental Benefits include annual recall exams; cement restorations; crowns and fixed bridges; dentures; extraction of teeth and other surgical services; fillings; fluoride treatments; scaling and polishing; major repairs and restorations; root canal therapy and X-rays. Traditional Drug Benefits Eligible expenses include medically-necessary drugs prescribed by a recognized health care professional licensed to prescribe. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 103 Traditional Vision Care Benefits Traditional Vision Care Benefits include the following as eligible expenses when prescribed or performed by a licensed optometrist, ophthalmologist or optician: eye examinations; lenses; frames; contact lenses; and visual training/remedial eye exercises. With some of the carriers, you can add: 1. Travel Insurance 2. Visitors to Canada Insurance Some of the Medical Assistance Services Available: 1. Emergency response in any major language. 2. Referral to an appropriate physician, clinic or hospital. 3. Confirmation of coverage with the hospital or physician. 4. Guarantee or arrangement of payment to the hospital or physician. 5. Assistance in contacting immediate family members, business partners or family physician. 6. Supervision of medical treatment and keeping the immediate family members informed. 7. Arrangement of transportation of an immediate family member to the patient's bedside. 8. Arrangement for transportation to identify the deceased. 9. Arrangement for transportation home of the patient, if medically permissible. Non-Medical Assistance Services Available: 1. Arrangement for local care of dependent children. 2. Coordination of the return home travel for dependent children if you are hospitalized. 3. Transmission of urgent messages to family members or business partners. 4. Assistance in the event of loss of passports or airline tickets. 104 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 5. Referral to legal counsel in the event of a serious accident. 6. Coordination of claims processing and negotiation of health care provider discounts. 7. Provision of pre-departure information concerning visas and vaccines. TAXATION OF INDIVIDUAL HEALTH & DENTAL INSURANCE As of the February 1998 Federal Budget, your individually owned personal health insurance may be tax deductible: Self-employed and unincorporated A. Your own personal health insurance may be deducted as a business expense reducing your taxable income. B. Any health and dental premiums paid on behalf of employees is tax deductible for employers and is not considered a taxable benefit for employees for federal tax purposes. C. If your primary source of income is through self-employment or income from other sources does not exceed $10,000, you could realize an income tax saving of up to 54 percent on the Personal Health Insurance premiums you pay. Your savings will depend on the level of your income and the province in which you live. D. If you have no permanent, full-time employees, there is an annual deduction limit of $1,500 for you, your spouse and each supported adult child and $750 for each other child. E. If you have one or more permanent, full-time employees with at least 3 months of service, the amount deductible is limited only by the cost of equivalent coverage for those employees, provided that 50% or more of those employees receiving coverage are not related to the owner. If less than 50% of those employees receiving coverage are arm’s length, the deduction is limited to the lesser of the cost of equivalent coverage for employees and the limits outlined above. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 105 F. All deductions are further reduced where the cost is shared between the employee and employer. For example, if the deduction determined above was $1,700 and your company only covers 30% of your employees’ premium, your deduction would be limited to $510 or 30% of $1,700. If you qualify for the medical expenses tax credit, the remaining $1,190 may be claimed as a part of that credit. Incorporated Businesses Any health and dental premiums paid on behalf of employees continues to be tax deductible for employers and is not considered a taxable benefit for employees for federal tax purposes. Owner employees may be entitled to deduct their own premiums if the benefits are received by virtue of employment rather than ownership. For example, if the owner employee received more generous benefits than the other employees, these benefits could be considered to be received by virtue of ownership rather than employment. Other Individuals (not included in the above categories) Include health and dental coverage as part of other medical expenses when calculating tax credits. On your tax return, include your personal health insurance premium for the year as a medical expense. Either spouse can claim the medical expense tax credit on their return based on medical expenses for any 12 month period ending in the taxation year. HOW ARE GROUP INSURNACE RENEWALS CALCULATED? Two Major Considerations Pooled benefits based on demographic and market factors - Life, Accidental Death and Dismemberment, and Long Term Disability. 106 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Experience benefits based on the companies usage or claims rate - Short Term Disability, Health and Dental benefits. A. POOLED BENEFITS The experience of the plan is an important factor in determining the renewal premium rates. However, for some benefits, even a single claim can have a significant impact on costs. For those benefits, premiums and claims are “pooled” to establish an average, more stable premium rate. Life insurance The cost of life insurance for an employer group is directly affected by the size of your company, the demographic make-up of your employees, and an aging population. 1. Company size Generally speaking, larger groups, as administrative costs are lower achieve greater economies of scale. This, in turn, lowers the cost of insurance and ultimately the premium that is paid. 2. Demographics The age and gender of a group also has a direct impact on the life insurance rates. As the group gets older, the likelihood of death among the employee’s increases, and thus a higher premium must be charged. In addition, the ratio of males to females will also play a role in determining premium rates for the group. 3. Aging population Besides the demographics of the group, Canada’s aging working population places upward pressure on the pricing of most benefit lines, and in particular the pricing of life insurance. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 107 Disability Insurance Like life insurance, the cost for disability insurance is affected by a number of factors, including the size of a group, the demographic make-up of the employees, and an aging population. In addition, disability insurance premiums are also affected by incidence rates, reserves, and Canada Pension Plan offsets. Incidence The rate at which people become disabled - or incidence rate is a key factor that affects disability pricing. The pricing of disability benefits will fluctuate up or down depending on the number of employees in the “pool” of insured group clients who are disabled. Over the last few years, incidence rates have increased. The rise in incidence rates is, in part, the result of a greater number of claims being made for mental and nervous disabilities such as depression and stress leaves. Reserves Disability reserves are the amount of money that must be set aside in order to pay for claims of a long-term nature. Consider, for a moment, two factors that affect reserves and, therefore, the pricing of the long-term disability benefit. Interest Rates In the case of a disability, the duration of a claim can be long enough to make interest rates a factor. When interest rates increase, less premium is needed to stock the reserves. Falling interest rates have the opposite effect. Termination Rates The termination rate is the rate at which employees are no longer considered disabled. When termination rates decrease (meaning more employees stay disabled for prolonged periods), greater reserves are required to pay for benefits. This is why managed disability claims adjudication is so important. 108 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Integration & Offsets Most group plans have a CPP / QPP offset or other integration clauses. This means that any long-term disability benefits paid to an employee are reduced by any benefits the employee receives from other sources. If CPP / QPP benefits do not increase over time (assuming inflation), a greater percentage of the total disability benefit is paid by your private plan. B. EXPERIENCE RATED BENEFITS Healthcare, dental care; vision and short-term disability are known as experience-rated benefits. An experience-rated benefit is: Characterized by a high volume of claims and low to moderate dollar claim amounts. Provides a good opportunity for you to directly control the costs of your plan. The only way to ensure that the future claims of your employees are adequately funded is to apply these trend factors to your group plan at renewal. The largest impact on health plans is the cost of medications as this represents 71.3% of all health claims (in real dollar terms) and 88.9% of all claims incidence incurred. Your Experience Your claims experience is determined by comparing the premium you have paid to the claims that have been submitted and approved. Incurred claims include those claims actually paid out plus reserves (required by law). Paid Claims Claims that have been submitted and approved by the insurance company, and paid out, or reimbursed, for services covered. This category represents the dollar amount paid back to the insured for claims. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 109 Reserves It is necessary to establish a reserve requirement in order to ensure that funding is available to pay for claims that were incurred, but not submitted. The ratio of claims incurred to premium is then compared to the target loss ratio, the ratio at which the insurance company has covered both claims and the cost of administering your policy. Credibility The extent to which the experience of your group determines your renewal rates depends on the number of employees covered under the plan and the number of years of experience there is to evaluate. This is known as the credibility of the experience. Generally speaking, the larger the size of the group and the greater the number of years of experience there is to evaluate, the higher the credibility. Smaller groups have a lower credibility factor since it is more difficult to predict claiming patterns from year to year. Demographics The age of the employees and the ratio of males to females are two demographic factors that will affect the health and dental rates. As with life and disability insurance, the size of the group will also have an impact on the premium paid. Health and Dental Trend Factors To ensure that premium will accurately reflect future claims; renewals attempt to predict the cost of today’s claims at tomorrow’s prices. Some trends that Insurance companies like to look at when renewal time comes are: Overall utilization Inflation Offloading from the government plans. 110 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 HOW DO THEY CALCULATE DRUG INFLATION NEW DRUGS are designed to counter new diseases, but also replace chronic use drugs. When dealing with drug plans only, utilization and aging demographics have an enormous impact on the costs. It must be noted, however, increasing drug therapy has a positive impact in overall health costs. It is estimated that for every $18 spent on drug therapies, $111 dollars is saved in other health services. Some factors for developing new drug therapies include: Cost of developing a new drug therapy is approximately $250 million. Out of a 20-year patent cycle, average of 13 years to get a drug therapy approved. Therefore, only 35% of the life of a patent remains in order to recuperate investment and R & D costs. More and more drugs are being replaced by new, more effective and more expensive drug therapies. As an example of this trend let us examine an arthritis sufferer as a case study. Celebrex (new drug therapy) cost $1.45 (2x / day) vs. Naproxen (old drug therapy) $0.32 (2x / day). Offloading of government services by the public sector impacts negatively on drug costs. Shortened stays in hospital mean that individuals must buy drugs for themselves sooner after an illness. An estimated 30% of services have been offloaded by the government and have therefore increased costs directly and indirectly for drug plans. In Quebec, private insurers must include all medications on the RAMQ (Québec, the Régie de l'assurance maladie plays a key role in Québec's healthcare system) list, which continues to be modified. Another example of the increased offloading, the RAMQ plans original premium was $175 in 1997, and now is $563. As well all the other elements of the plan, deductibles, co-insurance and out of pocket maximums, have been adjusted upward. Overall, the programs costs have risen by at least 18% per year. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 111 Deterioration of plan cost controls occur due to the impact of inflation on your deductible, stop-losses, and co-insurance. As inflation increases, the purchasing power of your “fixed dollar” amount of deductibles or cost controls in your plan deteriorate, and have less of an overall impact on maintaining the cost sharing relationship with the insured. UTILIZATION AND DEMOGRAPHIC TRENDS Even if drug prices have remained steady, it should be noted that demographics have an enormous impact on utilization. Health care costs tend to be fairly steady until age 50, at which point they start rising steeply with age. Furthermore, usage per individual has increased. In 1998 adherents to the RAMQ between the ages of 18 - 65, made an average of 12.5 drug prescriptions per year. In 2003, they made 17.1, a 36.8% increase. In those same periods, adherents age 65 and over, claimed an average of 39 times a year in 1998’ compared with 62.5 in 2003’, a 60% increase. DENTAL CARE TRENDS Utilization Like healthcare, an aging workforce and the overall impact of aging on claims affect dental care utilization. The average cost per dental service and the average number of dental services covered both tends to be higher for those over age 35. The inclusion of dependents also increases the utilization of dental services per employee. During the child-rearing years (between 25 and 45), the average covered amount rapidly increases. As plan member’s age, they also tend to require major dental services more often for themselves. Fee Guides and Inflation Your dental plan is designed to reimburse dental procedures based on provincial dental fee guides, prepared by provincial dental associations. While a dentist can charge more, most insurers reimburse procedures based on the provincial fee guide. 112 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Fee guides are reviewed annually and increases are usually absorbed by employer-sponsored plans. Although fee guides vary by province, most provincial dental associations increase their fees on average 2 - 2.5% from year to year. Approximately 10% of procedures are not subject to fee guide maximums. As well more and more dentists are charging up to the maximum allowed by the fee guide. PROVISIONS OF AN EMPLOYEE BENEFIT PLAN MASTER CONTRACT Resident This is a person who is legally entitled to be or to remain in Canada and who makes his home, and is ordinarily present, in a province or territory of Canada and who satisfies the requirements for a Government Health Insurance Plan. Employee An employee is a Resident who is directly and permanently employed on a full time basis by the Policyowner at the policyowners place of business in Canada, or at such other place or places in Canada as such person may be required to be to carry on the policyowners business and: Is regularly scheduled to work a minimum of 30 hours per week for at least 8 weeks in each calendar year quarter, and Is employed on the Effective Date of the Policy, or commences Employment after the Effective Date and has completed the eligibility period, and who is also in a Class shown in the Schedule of Benefits. Employment Refers to employment as an Employee of the Policyowner. Actively at Work This term usually means, any day an Employee is actively at work performing all the usual and customary duties of his / her job with the Policyowner for the scheduled number of hours for that day. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 113 Person Insured This is the Insured Employee and an Insured Dependent. Child Is a Resident who is a natural child, stepchild, or legally adopted child or ward of the Employee or of the Spouse, and who normally resides with the Employee or with the Spouse in a regular parent-child relationship and who is being claimed as a dependent of the Insured Employee or of the Spouse for Income Tax purposes. Spouse Spouse is defined as your legal or common-law (opposite or same sex) spouse, subject to the conditions listed below: A spouse can be married to the Insured Employee, or A common-law spouse must have been living with you for at least 1 year on a continuous basis, must not be related to you by blood, and must be recognized as your spouse in the community in which you live. (completion of a commonlaw declaration is required.) A spouse from whom you are legally separated is not eligible for coverage; Usually upon written request by the Insured Employee, the insurance under the Policy will be extended immediately for the named person upon the birth of a child that comes from this union. Dependent An unmarried Child, who is dependent on the Employee or on the Spouse for support, provided that the Child is over the age of 24 hours and: Is under the age of 22 years or Is under the age of 26 years and is a full-time student at an accredited educational institute, and 114 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 For the purpose of Extended Health Benefits coverage, if provided in the Policy, Child who is alive at birth and is under the age of 24 hours will be insured. The Dependent Life, Extended Health Benefits and/or the Dental Benefit, if provided under the Policy, will continue beyond the limiting age of 22, for an unmarried Child if: The Child became handicapped prior to reaching the limiting age; and The Child is incapable of self-sustaining Employment by reason of mental or physical handicap and is wholly dependent on the Insured Employee or on the Spouse for support and maintenance; and If the Child became mentally or physically handicapped after age 18, application for coverage and proof of disability is submitted to the Company within 31 days of reaching the limiting age as previously outlined. Eligibility Period This period is outlined on the Schedule of Benefits. Eligibility Date This will be the later of the Effective Date of the Benefit and the date that the Employee completes the Eligibility Period for the Benefit. Physician A physician or surgeon or a specialist medical doctor duly qualified and legally licensed by the jurisdiction in which they operate. One who prescribes and administers medical treatment and drugs professionally or performs any surgery within the scope of their license. One who specializes in a particular branch of medicine and who is neither insured for benefits under the Master Policy, nor related by blood or marriage to the Person Insured. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 115 Government Health Insurance Plan The provincial or federal legislation and the regulations, which provide government, sponsored hospital, drug, and dental or other medical care benefits for Residents of Canada. In Ontario, OHIP would be the governing legislation that affects people in Ontario. Institution Refers to a hospital, convalescent hospital, a rest home, a nursing home, a home for the aged, or any other place that would provide similar care. Reasonable and Customary This term refers to the charges for medical or dental services, supplies or treatments incurred by the Insured individual. These charges cannot be in excess of the general level of charges made by other providers of similar services in the locality or geographical area where the charge is incurred. Plan Refers to the Policy and any other policy, contract or arrangement other than the Master Policy, which will provide benefits or services for medical or dental care or treatment. This will include Employee Benefits in addition to any other employer, union, trustee, employee benefit association or professional association. Evidence of Insurability The written health information that is provided to determine whether a person satisfies the Company’s medical underwriting requirements. No Evidence Limit The amount of insurance an eligible Employee and an eligible Dependent may obtain without providing Evidence of Insurability. At each rate, re-calculation the Company may establish a new No Evidence Limit. 116 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 Pregnancy / Parental Leave of Absence Any formal pregnancy or parental leave taken pursuant to Provincial or Federal Law or pursuant to mutual agreement between the Insured Employee and the Policyowner. Incontestability Clause Any Policy as it relates to the Policyowner and the Person Insured is always voidable by the Company for fraud. In the absence of fraud, if the Policyowner fails to disclose or misrepresents a fact in any statements made in application for the Policy, the Policy may be voidable by the Company, except if the Policy has been in existence for a continuous period of two years. Disability Insurance is always voidable by the Company for failure to disclose or misrepresentation in all provinces except Quebec. In Quebec, if disability insurance has been in effect for a period of two years or more, the insurance cannot be voidable by the Company for not disclosing or misrepresentation. Suicide Most contracts do not contain a suicide two-year exclusion clause and suicide is not considered Accidental death. Currency and Place of Payment Every amount payable to or by the Company under a Master Policy will be in lawful money of Canada and will be payable at its Head Office. However, payments complying with any other arrangement agreed to in writing in advance by the Company may be made elsewhere. Evidence of Age The Insurance Company always reserves the right to request proof of the age of any Person Insured. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 117 WHAT CAN COMPANIES DO TO CONTROL THE COST OF EMPLOYEE BENEFITS? Take a look into the future to see what the trends of employee benefits will look like. For starters, employers should get a better handle on how their own costs are expected to change in the next few years. This is not as difficult as it sounds since rising costs depend largely on demographic changes, which can be predicted with a high degree of confidence. By reviewing data on new hires and turnover, an actuary can project the future demographics of an organization’s workforce and use it to estimate future costs. This knowledge can help prepare employers for what to expect and to plan accordingly. Change the cost-sharing equation - No one likes to pay more, but surveys show that employees are fairly open to increasing their share of benefits costs if this is what it takes to maintain health coverage. Before making any changes, an employer will probably want to benchmark current practices against their peer group. Better governance - More diligent oversight of the benefits program is likely to reap some savings. A good place to start is with a claims audit. Some findings from past audits have uncovered unauthorized expenditures such as: Co-ordination with Medicare being ignored for retirees, hence the employer plan paying for benefits that should have been covered by government. Paramedical limitations not coded into the system. Out-of-pocket maximums being ignored resulting in the employer’s plan paying more than promised. Reimbursement for drugs not eligible for coverage under the plan. Reimbursement of eye glasses that were not an eligible expense. Review rationale for providing post-retirement life, health and dental coverage Many organizations committed to providing post-retirement benefits when they thought the cost was minimal. As the cost has become better understood, postretirement benefits coverage has been declining. 118 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 A recent Trends and Projections survey showed that the number of companies providing post-retirement health coverage is declining. The one hurdle preventing an even more rapid decline is that the courts consider post-retirement benefits to be vested at the point of retirement. Hence, they cannot be easily taken away from retirees. Post-retirement benefits are similar to defined benefit pension plans in that both take many years to phase out and few organizations are launching new plans. Focus on wellness - The traditional emphasis of the medical system and by extension of employer sponsored benefits programs has been on diagnosing and treating illness, not on prevention. This is changing. A growing number of employers have implemented wellness programs. Approximately a third of companies have an employee wellness program. Most practitioners are convinced that wellness programs can improve the health of the workforce and hence improve productivity. The challenge is to quantify it. Doing so is critical since this is one of the few benefits areas where intervention might significantly reduce claims without cutting back on benefits or increasing costs. This area is sure to evolve rapidly in the next few years. Partner with employees - Consider having employee representatives on an advisory committee to deal with benefits issues. This may be the best way to get employees to buy in to remedies that may involve cut-backs in coverage or increasing cost-sharing on the employees’ part. IT’S AN ONGOING EVOLUTION Pension plans seem to go through a major overhaul every five to ten years because of external events such as provincial pension reform in the late 1980s and tax reform in the early 1990s. In the case of benefits programs, changes tend to be less dramatic but occur more frequently, so change is almost certain to be a constant. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 119 Here are some reasons why organizations will constantly need to review their benefits programs: Government downloading of costs - As governments pass along the responsibility for certain benefits, employers need to be diligent in managing the impact on their own plans. The default can be an automatic increase in employer costs that could have been avoided. The most recent Ontario budget, for instance, introduced individual healthcare “premiums”. In some cases, employers may be required to bear the cost because of inadvertent wording in their collective bargaining agreements dating back to the 1980s, when Ontario last had OHIP premiums. Changing demographics - The effect of demographic change on benefits programs is profound, but is masked by the fact it seems to occur at a glacial pace. Employers need to review their coverage in light of their changing demographics every five years or so. New health problems - Although they are not new problems, factors such as obesity, Type 2 diabetes, and stress-related health issues are becoming increasingly prominent. The prevalence of these conditions will trigger changes in coverage. New treatments - The emergence of employee health risk assessments and various wellness programs can assist employees in improving their own health outcomes. To be successful, employers need to be clear on their objectives when they introduce new programs. New technology - Access to the Internet (and employer Intranets) is now commonplace. Perhaps the biggest impact of technology in terms of benefits program design is that it facilitates flexible benefits programs and healthcare spending accounts. Online enrolment, for example, has proven to be much more effective than paper-based enrolment. Technology can also be effective in improving the communication of plan changes and wellness programs to employees. 120 Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 AND NOW, FOR SOME THE GOOD NEWS! It is easy to see the gloom in the current situation. We have identified the rather daunting challenges employers face in delivering an effective benefits program to their employees at a manageable cost. There is, however, some good news. The vast majority of Canadians believe we have an effective healthcare system. According to a healthcare survey, 86% of Canadians would rate the quality of services in our healthcare system as good to excellent. This is a higher percentage than we have seen in years. In the same survey, 94% of plan members say their employer benefits program meets their needs either “somewhat well” or “extremely/very well”. Canadians are living longer than ever. There are fewer illnesses that cannot be treated effectively. And for some illnesses, new treatment (e.g. via drugs) is less invasive and more effective than it once was (e.g. surgery). A Final Note The information compiled in this course is for information and educational purposes only. You are advised when dealing with your prospects and clients, that you recommend they seek the advice of their Accountants and Lawyers. Employee Benefits / SSC # 3 Pro-Seminars Limited © r01/12 121