Spirometry - The SEARCH initiative
advertisement
Spirometry
What is a spirometry?
Spirometry is a test that can help diagnose various lung conditions, most commonly COPD
(Chronic Obstructive Pulmonary Disease). It is also used to monitor the severity of certain lung
conditions (mostly Asthma), and their response to treatment.
A spirometer is a device to measure timed expired and inspired volumes, and hence indicate how
quickly and effectively the lungs can be emptied and filled.
There are various spirometer devices made by different companies, but they all measure the same
thing. They all have a mouthpiece that you use to blow into the device. A doctor or nurse may ask
you to blow into a spirometer ('spirometry') if you have chest or lung symptoms.
How is it done?
You breathe in fully and then seal your lips around the mouthpiece of the spirometer. You then
blow out as fast and as far as you can until your lungs are completely empty. This can take several
seconds. You may also be asked to breathe in fully and then breathe out slowly as far as you can.
A clip may be put onto your nose to make sure that no air escapes from your nose. The above
routine may be done two or three times to check that the readings are much the same each time you
blow into the machine.
What does the spirometer measure?
The most common measurements used are:
FEV1 - Forced Expiratory Volume in one Second. This is the amount of air you can blow
out within one second. With normal lungs and airways you can normally blow out most of
the air from your lungs within one second.
FVC - Forced Vital Capacity. This is the total amount of air that you blow out in one breath.
FEV1 divided by FVC (FEV1/FVC). This is the proportion of air in your lung which you
can blow out in one second.
What can the measurements show?
Spirometry readings show four main patterns.
Normal
Normal readings vary, depending on your age, size, and sex. The range of normal readings are
published on a chart, and doctors and nurses refer to the chart when they check your spirometry
readings.
Narrowed airways (obstructive) pattern - low FEV1, but normal or near normal FVC
If your airways are narrowed, then the amount of air that you can blow out quickly is reduced. So,
your FEV1 is reduced and the ratio FEV1/FVC is lower than normal. As a rule, you are likely to
have narrowed airways ('obstructive lung disease') if your FEV1 is less than 80% of the predicted
value for your age, sex and size, or if your FEV1/FVC ratio is 0.7 or less. But, the total capacity of
your lungs is often normal or near normal and so your FVC is likely to be normal or near normal.
The main conditions that cause narrowing of the airways are asthma and chronic obstructive
pulmonary disease (COPD). So, spirometry can help to diagnose these conditions. It can also help
to assess if treatment (inhalers etc) 'open up' the airways as the readings will improve if the
narrowed airways become wider.
A restrictive pattern - normal FEV1, but low FVC With a restrictive spirometry pattern you have
normal airways (normal FEV1), but your FVC is less than the predicted value for your age, sex and
size. This is caused by various conditions that affect the lung tissue itself, or affect the capacity of
the lungs to expand and hold a normal amount of air. For example, conditions that cause fibrosis or
scarring of the lung such as pneumoconiosis. Or, a physical deformity that restricts the expansion of
the lungs.
A combined obstructive/restrictive pattern With this you may have two conditions (for example,
asthma plus another lung disorder). Also, some lung conditions have features of both an obstructive
and restrictive pattern. For example, cystic fibrosis causes excess mucus production (causing
narrowed airways) and damage to the lung tissue.
What preparation is needed before having spirometry?
You should get instructions from the doctor, nurse, or hospital department that does this test.
Always follow these carefully. The instructions may include such things as not to use your
bronchodilator inhalers for a set time before the test (several hours or more, depending on which
inhaler you use). Also, not to have alcohol, a heavy meal, or do vigorous exercise for a few hours
before the test. Ideally, you should not smoke for 24 hours before the test.
Is there any risk in having spirometry?
Spirometry is a very low risk test. However, blowing out hard can increase the pressure in your
chest, abdomen and eye. So, you may be advised not to have spirometry if you have:
unstable angina.
had a recent pneumothorax (air trapped beneath the chest wall).
had a recent heart attack or stroke.
had recent eye or abdominal surgery.
coughed up blood recently and the cause is not known.
By using spirometry to assess lung function it is possible to diagnose asthma or chronic obstructive
pulmonary disease (COPD) with greater confidence and accuracy. Spirometry is vital for assessing
the severity and reversibility of COPD.
There are many different devices available: volume-displacement devices (piston, bellows or water
sealed bell) or flow sensing (measuring pressure drop across resistance, turbine rotation or the
cooling of a heated wire). The better devices present the results graphically (a spirogram).
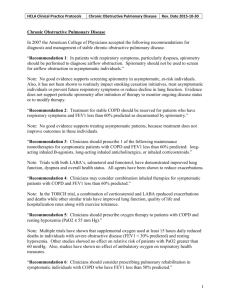
Measurements made in Spirometry
Abbreviation Measurement
Description
Vital capacity
(Slow vital capacity)
Maximal amount of air exhaled steadily from full
inspiration to maximal expiration (not time
dependent). It should be >80% of predicted,
reduced in restrictive disease.
FVC
Forced vital capacity
Volume of lungs from full inspiration to forced
maximal expiration. It is reduced in restrictive
disease, and in obstructive disease if air trapping
occurs.
FEV1
Volume of air expelled in the first second of a
Forced expiratory
forced expiration. Reduced in both obstructive and
volume in one second
restrictive disease.
FEV1%
(FER)
Forced expiratory
ratio
(FEV1/FVC)x100
VC (SVC)
Percentage of FVC expelled in the first second of
a forced expiration.
Normal in restrictive disease - reduced in
obstructive disease.
FEF 25-75%
Forced Expiratory
Flow between 2575%
Average expiratory flow rate at the middle part of
forced expiration. It is a more sensitive indication
of what is happening in the middle/lower airways,
but is not as reproducible as FEV1. Normal in
restrictive disease.
PEFR
Peak expiratory flow
rate
Maximum rate of airflow achieved during
expiration
Electronic devices have the advantage of automatically correcting values for body temperature,
barometric pressure and water vapour saturation (BTPS).
International guidelines recommend that spirometers:
Will need calibrating (volume devices weekly and flow devices daily, with a 3 litre syringe)
Should produce a hard copy which should be large enough to check values manually
Volume/time plots are mandatory, flow/volume plots are optional
Adequately trained staff are essential if inaccurate or misleading results are to be avoided
Electronic devices without hard copy tracing may lead to underestimation of FEV1 and FVC
because it is not possible to verify the reliability of the test (best done by looking at shape of
graph).
Instructions (standing is not required, but if sitting, sit straight up, and keep head slightly
extended):
1.
Breath in maximally
2.
Hold mouthpiece between teeth, then apply lips for an airtight seal.
3.
Breath out as fast as possible. (The patient should aim for maximal flow at the moment
expiration starts: with handheld devices - watch the vane rotating, and make sure it does
not start rotating while the spirometer is brought to the lips, thus avoiding artifacts).
4.
Keep breathing out until the lungs are maximally empty.
Before interpretation, there should be
at least three satisfactory readings
graphs should be smooth and free from irregularities
at least two FEV1 readings should be consistent within 100mls (or 5%)
recording should be continued until volume/time graph reaches a plateau (make take >15
sec)
best readings should be compared with predicted normal value (for age, sex and height)
Interpretation: For a full assessment you need to consider the values: FEV1, FVC, PEFR;
calculate the FEV1/FVC ratio; and how these compare with the individual's predicted values
from the charts.
FEV1 is strongly recommended as the measurement of choice in COPD as:
It is reproducible and objective with well defined normal ranges
It can be measured quickly and easily at all stages of disease
Variation on different occasions on the same patient is low (<170mls)
FEV1 is a good predictor of future morbidity and mortality (better than FEV1/VC)
Serial measurements provide evidence of disease progression
Peak flow measurements do not distinguish between obstruction and restriction of airflow,
and may seriously underestimate the degree ofairway obstruction in COPD
FVC = forced vital capacity
In some patients with advanced COPD, forced expiration may result in closing of airways
and trapping of air, so relaxed vital capacity (VC) may be a better measure of lung function.
There is likely to be a reduction in FVC in patients with moderate to severe COPD, which is
caused by the alveolar damage and coalescence, together with loss of elasticity of the lung
tissue.
Patients with chronic asthma may have a reduction in FVC
FEV1/FVC ratio:
If there is a lung abnormality, >70% suggests a restrictive defect and <70% implies
obstructive (COPD or moderate to severe asthma.
In the elderly, the FEV1/FVC may fall to <70% in the absence of airways obstruction (so
use tables), but in everyone, if the value is >70%, obstruction is effectively excluded.
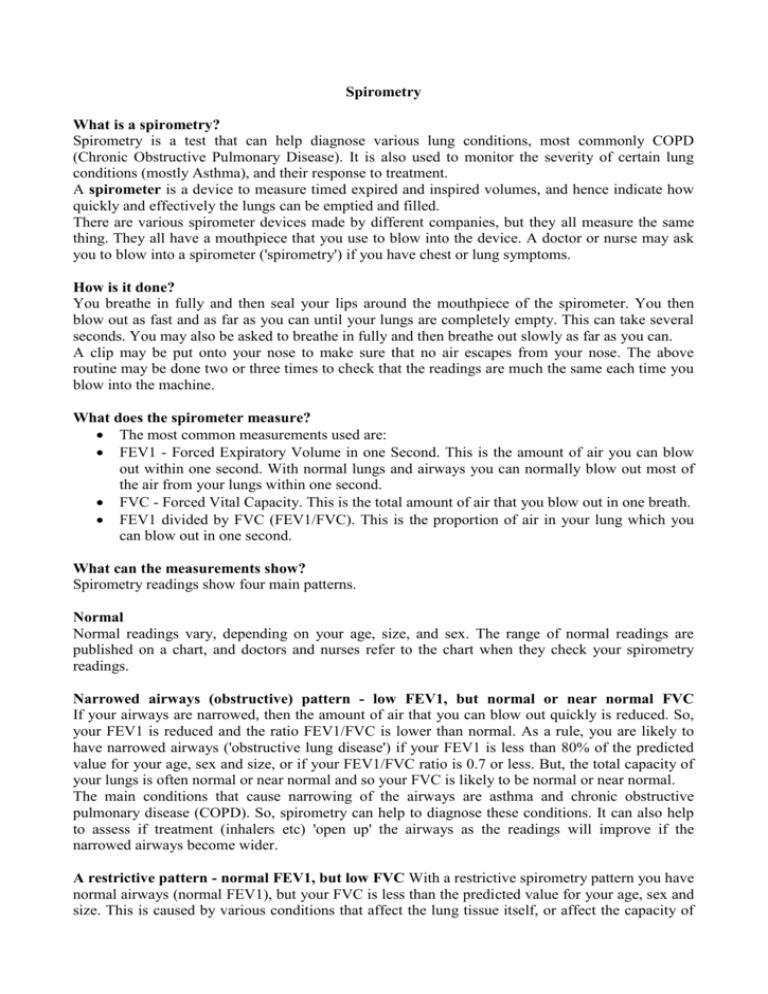
Uses of spirometry in primary care All patients with either suspected asthma or COPD should
ideally have spirometry performed.
Asthma patients Spirometry is not essential for the diagnosis of asthma. However, the diagnosis
can be confirmed by the demonstration of 15% reversibility or more in either PEFR or FEV1 post
bronchodilator and/or following a two week course of high dose prednisolone.
COPD patients The grade of COPD is important in deciding on appropriate treatment for COPD
patients (see above). If patients have mild symptoms but their spirometry result confirms mild or
moderate COPD then they might be more persuaded to stop smoking. Smoking cessation is the
single most important intervention in controlling progression of COPD . All patients with COPD
should have their FEV1 monitored annually to assess progression of their disease. The level of
FEV1 is related to complications such as development ofrespiratory failure or pulmonary
hypertension. Serial measurements over a few years allow assessment of rate of decline of FEV1,
an indicator of mortality risk in COPD.
Restrictive and Obstructive Ventilatory Defects Abnormalities of ventilatory function measured
by spirometry are classified as either 'obstructive' or 'restrictive'.
The hallmark of an obstructive defect is slowing of expiratory flow, so that a low proportion of the
FVC is expired in the first second and the FEV1/FVC ratio is reduced. This is seen in patients with
diffuse airway narrowing of any cause, eg asthma, COPD,emphysema, extensive bronchiectasis,
cystic fibrosis, lung tumours.
If the patient has a restrictive ventilatory defect the FEV1 and FVC are both reduced, but in
proportion, so the FEV1/FVC ratio remains normal (greater than 75% - but this falls with age and
more precise prediction of normal is possible).
Restrictive ventilatory defects are seen with various intrapulmonary diseases, eg pulmonary
fibrosis, pulmonary oedema, collapse orconsolidation of the lung, and also importantly with extrapulmonary conditions, eg large pleural effusion, rib cage deformity (scoliosis ), after lung surgery,
and weakness of the respiratory muscles. Clearly the measurements need to be interpreted in the
clinical context and if a restrictive abnormality is discovered a chest x-ray is usually essential for
interpretation.
References
Brusasco V, Crapo R, Viegi G; American Thoracic Society; European Respiratory Society. Coming
together: the ATS/ERS consensus on clinical pulmonary function testing Eur Respir J. 2005;
26(1):1-2.
Wanger J, Clausen JL, Coates A, Pedersen OF, Brusasco V, Burgos F, Casaburi R, Crapo R,
Enright P, van der Grinten CP, Gustafsson P, Hankinson J, Jensen R, Johnson D, Macintyre N,
McKay R, Miller MR, Navajas D, Pellegrino R, Viegi G. Standardisation of the measurement of
lung volumes. Eur Respir J. 2005; 26(3):511-22.
Miller MR, Crapo R, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Enright P, van der
Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen
OF, Pellegrino R, Viegi G, Wanger J; ATS/ERS Task Force. General considerations for lung
function testing. Eur Respir J. 2005; 26(1):153-61.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der
Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen
OF, Pellegrino R, Viegi G, Wanger J; ATS/ERS Task Force. Standardisation of spirometry. Eur
Respir J. 2005; 26(2): 319-38.
Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten
CP, Gustafsson P, Hankinson J, Jensen R, Johnson DC, MacIntyre N, McKay R, Miller MR,
Navajas D, Pedersen OF, Wanger J. Interpretative strategies for lung function tests. Eur Respir J.
2005; 26(5):948-68.
Internet useful addresses
British Lung Foundation http://www.lunguk.org/
GINA Global INitiative for Astma conducted in collaboration with the US National Heart, Lung,
and Blood Institute (NHLBI) and the World Health Organization (WHO)
http://www.ginasthma.com/
Global Initiative for Chronic Lung Disease (GOLD) conducted in collaboration with the US
National Heart, Lung, and Blood Institute (NHLBI) and the World Health Organization (WHO)
http://www.goldcopd.com/
Correction for room temperature and environmental variables:
Volume (BTPS) = Vol (ATPS) x {310 (BP - WVPrt) / [(BP - 47)(273 + rt)]}
BTPS= body temperature and pressure saturation
ATPS= ambient temperature and pressure saturation
BP = barometric pressure in mmHg
WVPrt = saturated water vapour pressure at room temperature
rt = room temperature in degrees celsius
47 = saturated WVP at 37 degrees celsius (body temperature)
Images of Spirometers
2 different Spirometers