Informed Consent and Autonomy – A Sui Generis Dilemma In The
advertisement
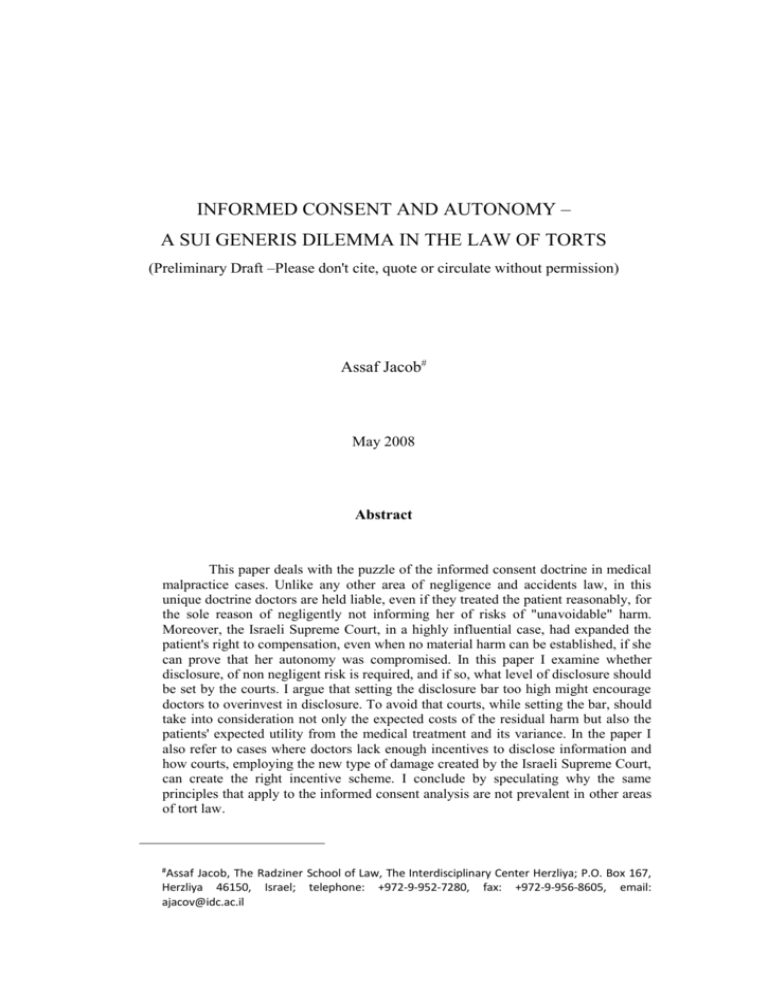
INFORMED CONSENT AND AUTONOMY – A SUI GENERIS DILEMMA IN THE LAW OF TORTS (Preliminary Draft –Please don't cite, quote or circulate without permission) Assaf Jacob# May 2008 Abstract This paper deals with the puzzle of the informed consent doctrine in medical malpractice cases. Unlike any other area of negligence and accidents law, in this unique doctrine doctors are held liable, even if they treated the patient reasonably, for the sole reason of negligently not informing her of risks of "unavoidable" harm. Moreover, the Israeli Supreme Court, in a highly influential case, had expanded the patient's right to compensation, even when no material harm can be established, if she can prove that her autonomy was compromised. In this paper I examine whether disclosure, of non negligent risk is required, and if so, what level of disclosure should be set by the courts. I argue that setting the disclosure bar too high might encourage doctors to overinvest in disclosure. To avoid that courts, while setting the bar, should take into consideration not only the expected costs of the residual harm but also the patients' expected utility from the medical treatment and its variance. In the paper I also refer to cases where doctors lack enough incentives to disclose information and how courts, employing the new type of damage created by the Israeli Supreme Court, can create the right incentive scheme. I conclude by speculating why the same principles that apply to the informed consent analysis are not prevalent in other areas of tort law. # Assaf Jacob, The Radziner School of Law, The Interdisciplinary Center Herzliya; P.O. Box 167, Herzliya 46150, Israel; telephone: +972-9-952-7280, fax: +972-9-956-8605, email: ajacov@idc.ac.il Introduction The Informed consent doctrine is Sui Generis in the area of malpractice law. Having its origins in the law of battery, protecting the patient's autonomy, the doctrine was transformed over time into a branch of negligence law. Thus, the doctrine protects the patient's right to be properly informed of the risks involved in a medical procedure and the alternative treatments to the one the patient is about to undergo. If doctors don't comply with the reasonable disclosure standard (which is often times, highly debatable) they are considered to be negligent. Unlike the typical medical malpractice cases, here the doctors' negligence lies only in the fact that they do not comply with the right level of discovery. According to the traditional informed consent analysis, to win an informed consent case the plaintiff must substantiate five elements, only the first of which deals with the omission to provide the required information. The other elements are: actual damage to the patient; that results from risks he was not informed of; cause in fact (had the patient received the information he would have chosen not to undergo the clinical procedure) and proximate cause (a reasonable person, being properly informed, would have rejected the proposed treatment). This traditional informed consent analysis has unique and interesting characteristics. Unlike other areas of tort law, where the overall conduct of the professional is evaluated, in the area of medical malpractice two separate questions are posed. The first is whether there was negligence in the selection and performance of the medical treatment. The second is whether the disclosure was negligent as such. Thus, the doctors' behavior is examined in two independent aspects, each creating a separate duty. Both aspects, however, are conditioned upon the materialization of an actual damage to the patient. The common wisdom is that informed consent, as an independent action, adds only little, if at all, to typical malpractice cases, in which the plaintiff can establish the physician's negligence in the selection or the performance of the medical treatment. In such cases, the patient can win compensation without establishing the lack of informed consent. Thus, one rarely sees discussions of informed consent when negligence in the performance of the treatment is clearly established. Informed consent is therefore important when it is the patient's last resort. In other words, when the treatment itself was not negligent, common law courts can still rule the plaintiff is entitled to compensation due to lack of informed consent. In such a case, the physician will be held liable even if he operated with the consummated skill. Thus, the doctor, although considered to have provided a non-negligent treatment will still be liable for not providing the information (or for not providing it in the right manner) which is required to obtain informed consent. The uniqueness of the informed consent analysis The negligence regime allows people to expose others to reasonable risks. This means that once the damage materializes, the defendant will only have to pay its costs if he created an unreasonable risk. If the defendant acted reasonably, the plaintiff will carry the residual loss. This is the major difference between negligence and strict liability, where the defendant carries the burden of both non-reasonable and reasonable risks, regardless of the costs of precautions. Translating the standard of reasonableness to economic terms, via the Hand formula, yields the following: the plaintiff will win the case if he can establish, at the margin, that defendant's Burden of taking additional measures of precaution was cost effective and despite that it was not taken. Economic wise, if B<PL the defendant could have done more to reduce the expected loss. Not taking such measures deviates from the conduct of the reasonable person and therefore considered to be negligence. Negligence law, however, is not intended to promote inefficient investment in precautions. Thus, if the defendant shows he took the necessary precautions (B), no less no more, he will not be considered liable. Consider the following example: A patient with a heart problem approaches the doctor. The doctor knows that from a medical perspective, the right treatment for that patient is an open heart surgery. This operation has an expected loss of 150 (PL). By taking precautions the doctor can reduce the expected loss by 100. These precautions would cost him 100. Assume that avoiding the residual risk (50) is inefficient because open heart surgery has unavoidable inherent risks. The doctor takes the necessary precautions (100). The open heart surgery was successful, but the patient loses her leg which is the materialization of one of the unavoidable risks. The standard negligence analysis will find the doctor not liable. In economic terms - society does not require the doctor to further invest in preventive measures (50) because these measures are not cost effective. Given a negligence regime, once the doctor acted reasonably, the patient should carry the burden of the residual harm. This is a typical negligence paradigm, a situation with which courts deal almost in every negligence case. As mentioned above, however, in medical malpractice cases, this is only part of the story. Negligently withholding information about the risks involved in the procedure, will expose the doctor to pay for the residual loss provided the plaintiff can substantiate the elements of informed consent or, for simplicity, where the patient would have changed his mind, not taking the procedure, had he received proper disclosure. In other words, not revealing the necessary information in a negligent manner, the doctor will pay for the materialized harm even if the treatment itself was flawless. The question is whether this legal regime provides doctors with the right incentives? Where should the law set the liability standard for not revealing the information? At first glance, it is not at all clear that disclosure should be required. After all, in "regular" negligence cases all we ask the defendant is to take the right level of precautions. Withholding information, as such, does not impose any liability upon the injurer. One can only assume that almost in every tortious encounter, had A asked B if he would agree that A would hurt him, in a non negligent manner, B would have answered in the negative. And yet, A is not obligated, under negligence law, to obtain B's informed consent to the risk he exposes him to. Even when the law imposes a duty to disclose, this duty is examined as part of the overall conduct and not independently. Scenarios in which the court declares the conduct to be flawless and yet finds the injurer liable for the entire damage for not revealing the information rarely exist. The rationale behind this common law rule is that society does not wish to encourage investment in the precautions of unavoidable risks. Thus, one can argue that since by definition, in a non negligent action, revealing the information ex ante does not prevent the damage from materializing but only shifts the costs of the residual risk, investing more resources in collecting and disclosing information is undesirable. The malpractice cases, however, are different from the paradigmatic negligence case in several aspects. One of the important differences is the existence of a relationship between the parties before treatment is provided. Providing the information may lead the patient to forgo the treatment altogether, avoiding the expected loss. Namely, providing information might enhance utility, based on the specific utility of the patient, even when the doctor acted in a non negligent manner. The question remaining is how much information should the doctor reveal. Assuming arguendo (as I will later establish) that disclosure has its costs1 – we need to determine how much society wants the doctor to invest in revealing information to the patient. Unlike the typical application of the Learned Hand formula, where the limit to the costs of precautions is derived from the expected loss, when disclosure is involved, setting the bar is more complicated. What is the scope of the damage from non disclosure that could have been prevented had the doctor provided more information? The damage is derived from the loss of utility in undergoing the operation, which would have been avoided, had the information been provided. Setting the bar too high may prove to be counterproductive since doctors may over invest in disclosure. The higher the bar the more the doctor would invest in "shifting" disclosure rather than "preventing" disclosure. For the purpose of this analysis I will assume that the more information provided the more accurate the patient's decision whether to undergo the surgery and therefore the lesser the chance of loss of utility for choosing the wrong treatment. As in damage prevention, the first bits of information are the most useful and cost effective, while the information that follows is more costly to produce and less effective. (Too much information may even turn out to be counterproductive2). I will also assume that if no information is provided the patient will estimate no risk is involved in the procedure and no other alternatives exist and therefore will undergo 1 2 There are several types of costs – the first is the cost of collecting the information by the care taker. The second is the cost of communicating it to patient. The third is the cost of patients dealing with the information. the procedure even when its benefits are smaller than its costs (Do notice however that lack of information can also work in the opposite manner – it may lead the patient to avoid a medical treatment he should have taken). Consider the following 3 examples: Example 1: The expected residual damage from an open heart surgery is 50. This risk is unavoidable. Even if no negligence is involved, once in every several surgeries, the risk materializes. The patient's expected utility from the operation is high, say 250. A patient undergoes the surgery and the residual damage materializes. The patient files an informed consent suit arguing that the doctor did not provide him with information about the residual risk involved in the operation, and therefore his consent was invalid. Should the patient prevail? What should be, if any, the scope of the duty to disclose information and is the doctor, by not providing the information, in breach of such duty? Given the patient's high utility from the operation and the fact that the risk is much smaller and unavoidable, the doctor should win the informed consent suit. The intuition is rather simple: while collecting and delivering the information is costly, the patient will not benefit from it, in the sense that it will not affect the way he acts (if at all, the information may have a negative effect, causing patients to avoid necessary treatment3). Therefore, revealing the information in this case is a social loss and should not be required. 3 Setting the doctor's disclosure bar, at any level above zero, causes a social cost. This cost produces no corresponding benefits since the patient is not making any use of the revealed information.4 While the doctor will comply with the imposed disclosure standard to avoid liability for the residual harm, there is no economic justification for doing so. The disclosure is made by the doctor for achieving a pure allocative/re-distributive effect. Unlike the typical negligence paradigm, where the patient carries the costs of a non negligent residual harm, here not disclosing information about the residual risk would shift the costs to the doctor. Knowing it ex ante, the doctor will over invest in disclosure. Thus, for example, setting the disclosure bar at 20, the doctor will invest 20 to avoid negligent liability. However, since the expected residual damage cannot be eliminated the overall cost will be 70, instead of 50. The higher the bar, the more the doctor will invest and the greater the social loss will be.5 It seems the legal rule follows this path to the extent that it insists, as one of the elements of the informed consent doctrine, on proving that had the patient received the information, he would have changed his mind about undergoing the procedure. Thus, if the doctor knows that the patient's utility from the procedure is greater than the residual harm, he can rest assure that not providing the information will not expose him to tortious liability. A slight variation on the first example is where the residual harm is greater than the patient's utility. Assume the residual damage is 250 and the patient's utility from the operation is only 50. Knowing the costs and the patient's utility, disclosure by the doctor is not required in this case either. Even though the treatment is not 4 5 Narrow definition of making use of the information… The upper limits on the doctor's disclosure expenses will be the expected residual damage. Setting the legal bar above that level the doctor will not invest more resources in disclosure for he will prefer to pay the costs of the residual harm, if materialized. negligent to the extent that at the margin, extra precautions will not reduce the expected harm, given the patient's utility/residual damage ratio, the doctor should not perform the operation altogether. Since it is within the doctor's discretion not to proceed with the operation, disclosing information is a social waist. If, after giving the patient a thorough and expansive explanation, the patient will pursue the same path as the doctor recommended (i.e. not undergoing the operation) revealing the information to him means incurring costs without providing correlative benefits and therefore should be avoided.6 Example 2: The expected residual damage from a cosmetic surgery (nose job) is 50. As in the first example, this risk is unavoidable. Even if no negligence is involved, once in every several surgeries, the risk materializes. A patient attends the doctor's office and asks about the clinical procedure. Assume there are two types of patients – A and B. Type A patient really suffers from the way his nose looks and therefore will have high expected utility from the operation, say 75. Type B patient cares about his nose but not as much as type A. Therefore his expected utility from the operation is 25. Assume there are equal amount of type A and type B among the doctor's patients and that there are no other types besides them. Also assume there is no way, ex ante, to tell whether a patient is type A or type B. Thus, the expected utility from the activity is 50 ((75+25)/2). Should the doctor disclose the information about the residual risk involved in the procedure? Where should the disclosure bar be set? At first glance no disclosure should be made. Remember that the doctor is assumed to act in a non negligent manner. Therefore, adding extra precautions at the 6 Explain why informed consent suit due to non disclosure followed by no treatment rarely exists… margin will not prevent the residual damage. Since the expected utility from the treatment equals the expected residual harm, one can argue that no legal intervention is needed and the parties should continue with their practice. One can analogize this to the application of the learned hand formula. Once at the margin B=PL, no negligence is involved and the law does not interfere with the activity. This analysis however, does not take into consideration the fact that by providing information the doctors can sort the two types of patients, allowing them to better choose between taking the treatment or avoiding it altogether. The assumption was that not knowing about the risks, (i.e. if no information whatsoever is provided), patients will undergo the surgery. Providing information may cause some of them to make a better and more accurate decision. While the information may not help type A patients make the right decision, since they will take the clinical procedure anyway, the information may convince type B patients to avoid it. Thus, for every type A patient, revealing the information is a social waist while for every type B patient the information may produce real benefits. Even though the residual risk cannot be further reduced, it can be eliminated altogether by avoiding the procedure. In our example there are two types of patients, some with expected utility of 75 and some with expected utility of 25 and the doctor cannot tell them apart –– providing information to a type A patient (expected utility of 75) has a social cost without corresponding benefits. On the other hand, providing information to type B patient (expected utility of 25) might affect their decision enhancing the chances they will make the right choice. The question is how much information should be provided, or in other words, where should the disclosure bar be set? I will address this question in two phases. First, I will examine what is the maximum utility derived from full disclosure. In other words, what is the "expected damage" resulting from not collecting and revealing the information. As in the Learned Hand formula, where the expected damage sets the upper bar for the costs of prevention, here too, the loss of utility will set bar for the maximum costs of disclosure. Next, I will try to suggest the right standard for minimizing the utility loss. Assume the doctor is not revealing any information. In such a case there is a 50% chance that the patient is type A and 50% chance the patient is type B. For every type A patient the benefit from the activity is 25 (75-50). For every type B patient the loss from taking the operation is -25 (25-50). Since there are equal chances for type A and type B patients, these two balance each other and result in a net benefit of 0. Now assume the doctor provides full disclosure. Type A patients will not alter their decisions. They will still undergo the same procedure. Thus, their net benefits are still 25. Things will be different for type B patients. Giving type B full disclosure will lead them to avoid the procedure altogether. Thus, they will have neither losses nor benefits and their payoff will be 0. Since there is a 50% chance for type A and a 50% chance for type B, the expected utility of revealing the information sums up to 12.5 ((25-0)/2). Given all the available options, by switching from no disclosure to full disclosure society gains 12.5 (12.5-0). The result of subtracting the expected utility upon no disclosure from the expected utility upon full disclosure should set the upper bar for disclosure. Indeed, when more information is provided to the patient, the chances are better he will make the right decision. On the other hand, providing information to Type A patients does not alter their behavior. Given the costs of providing information, doctors should not invest above a certain level in disclosure, even if type B patient is able to show in court, ex post, that had he been provided with more information, he would have changed his mind about the operation skipping it altogether. In our case 12.5 is the maximum level at which the bar should be set. Setting the bar at a higher level, say 50 (the expected residual damage), is by definition a social waste. If the doctor complies with this standard and makes this investment in disclosure, a major part of the investment will only be made for allocative reasons (to escape liability) promoting no social value. Assume that the B type patient in example 2 has undergone the operation. He argues that the doctor has provided him with only some information (15) and proves that had the doctor provided him with more information (say 20) he would have skipped the operation altogether (hence, the requirement of cause in fact can be established). Based on the above mentioned analysis, courts should allow no compensation. And indeed, the informed consent doctrine follows this path to some extent. It is true that the cause in fact element requires, as a prerequisite for compensation, that the patient would have changed his mind, had he been provided with the information. But the patient must also establish a breach of the duty to disclose as well as legal causation. The problem therefore is not with the set of legal tools but with the level of which the disclosure standard is set. It seems the courts have set the disclosure standard too high – sometimes as high as the expected non residual damage, not taking into account the utility that many patients derive from the operation as well as the fact that to many patients disclosure will not make any difference. Moreover, and this brings us to the second point the courts should address, setting the maximum amount to be spent on disclosure does not mean that this amount should be spent in any given case. The doctors should only spend on disclosure sums that are cost effective. In other words – before imposing liability courts should be convinced that at the margin investing an extra dollar in disclosure enhances utility by more than a dollar. Changing the legal regime from negligence to strict liability - would it bring the right incentives? Example 3: The expected residual damage from a clinical procedure is very small, say 0, but the patient's utility is negative, say -100. To think of a real life example consider a simple clinical procedure with no physical risks involved, which is made in a community of Jehovah Witnesses. Even though the residual damage from the clinical procedure is 0, society would still want to encourage doctors to provide information about it, due to the patients' negative utility. This example is more complicated due to the fact that ex ante, doctors don't have enough incentives to provide information. Since the traditional informed consent doctrine, as a branch of negligence law, requires actual damage, when no material damage is involved, doctors will not see the need to reveal any information. (Another example is that of an orthodox Jew who is not told that he is eating non kosher food. No physical harm is done, but the patient's utility is negative). The question is then how to form the right incentive scheme? Nearly nine years ago, in a landmark decision, the Supreme Court of Israel ruled that a patient who undergoes a consented, non negligent, medical procedure, without being fully informed of its consequences (and thereby lacking "real" consent), is entitled to compensation under the law of negligence and the doctrine of informed consent. The importance of this decision and its precedential value lie in the fact that The Supreme Court "created" a new type of damage – harm to the patient's autonomy. The court ruled that negligently inflicting harm to the patient's autonomy, as such, entails her to monetary compensation. This decision was, and still is, a ground breaking decision not only in Israel but in all common law countries. The concept that a patient is compensated although no "real" damage was suffered makes Israel, to the best of my knowledge, the first, and maybe the only country in the world, in which this sui generis scheme applies. This mechanism of compensating for harm to the patient's autonomy can help doctors reach the right decisions in cases where no actual damage occurred. Thus, doctors will have to take the patient's decreased utility into account. This new "damage" imposes real costs upon doctors and therefore deters them from providing too little information. Whether this practice works depends, among other things, on whether courts and doctors are able to assess the patient's overall decreased utility. Evaluating the damage to the patients' autonomy too high may result in excessive deterrence, which in this case would translate to excessive disclosure. It should be remembered that based on the above mentioned examples, we do not want to abandon the causation requirement. Policy concerns require that in order to receive compensation, plaintiff must prove the doctor's omission had some influence on her choices. Also remember that the "additional cost" imposed by this new type of damage (inflicting harm to the patient's autonomy) is applied only when the expected residual damage is small and the expected patients' utility is negative. In all other cases the risk of paying the residual damage creates the right incentive for the doctor to behave in the correct manner. With this in mind it seems the Supreme Court went too far in creating the harm to a patient's autonomy. Indeed, Justice Or guided the lower courts that compensations for this new type of damages should be rather limited, in order to avoid over deterrence. Still, the court also ruled that no causal relation must be established between the withheld information and the inflicted harm. Thus, the court accepted the fact that even when, upon doctors providing all required information, the patient would not have changed her mind about the clinical procedure, she is nonetheless entitled to compensation for the harm inflicted to her autonomy. According to the court, damages are granted in such a case due to the fact that withholding information from the patient comprises her integrity per se. The link between physical harm and patient's utility. Can we generalize and highlight the guidelines the court should follow when dealing with informed consent cases? First, the bigger the patients expected utility and the lower the expected residual damage, the lesser the need for disclosure. Assume a life threatening situation and a medical procedure with minor residual risk – when the gap between the two is substantial, minimum disclosure, if any, is required. The informed consent doctrine follows this path by saying that the reasonable patient would not have changed his mind, had he been provided with the information about the operation. Thus the bar is actually set at a very low level. Second, when the residual harm is high and the utility low, the disclosure bar should be set higher. Thus, a plastic surgery that generally corresponds to a lower level of utility, which carries high residual risks, will justify a much higher degree of disclosure. If, for the majority of the patients, the expected utility is lower than the expected damage, and the surgeon still performs the surgery, we want every patient to have plenty of information in order to accurately decide whether he still wants to undergo the procedure. In such cases, requiring the doctors to pay for the actual harm if full disclosure is not made is understandable. The court might even extend the disclosure to include information on remote alternative treatments that can be taken by the patient. Third, often times the courts use the expected physical harm as a proxy for disclosure. The more risky the procedure the more information the doctors should provide. Given a constant utility this makes sense. Since the damage in non disclosure is affected by two components - the patient's expected utility in undergoing the procedure and the expected residual damage - the higher the expected damage the more the doctors should disclose. Sometimes, however, this method may not produce the right outcome. There are scenarios in which the loss of utility is high even when there is no expected physical damage to the patients or when this damage is limited. In these cases the court can use the damage of inflicting harm to the patient's autonomy, in addition to the actual damage, to correct under-disclosure and to set the right incentives scheme. A pregnant woman, who may lose her child due to an intrusive examination, may not be at a high risk but still lose a lot in term of losing her fetus. Paying only for the material damage may not be enough to provide doctors with the right incentives. Thus, adding the damage of harm to autonomy is the right thing to do. Adding this damage does not mean that causation should be compromised. Hence, only if the mother would have changed her mind had she been told about the risks, she is entitled to compensation. Informed consent, disclosure and inflicting harm to the patient's autonomy. Having said that, it is a puzzle that this new damage of inflicting harm to the autonomy is almost exclusively restricted to the area of medical treatment. It is also a puzzle that we don't see a similar duty to disclose non negligent risks in other areas of tort law. Juxtaposing medical treatment with other areas of tort I wonder whether medical malpractice entitles patients to benefits they don't deserve almost anywhere else, and if so, why? Almost all accidents happen without the permission of the injured party. In the vast majority of cases, plaintiffs will rightfully argue that had they known about the risks, they would not have approved it. And yet, harm to autonomy is not prevalent, to say the least. Plaintiffs are the ones who carry the burden of the residual harm. Thus, the question why the negligence paradigm, that allows A to risk B so long as he does not act in a negligent manner applies to two strangers, where the chances one of them will consider the interests of the other are rather slim, and not to doctors and patients, where the chances the doctors will take the patients interest into account are much higher, should be further explored…