Lab 7 – Eukaryotic Microbes
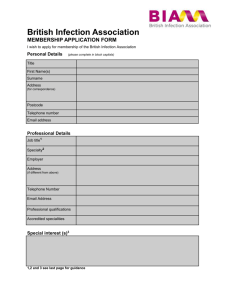
advertisement

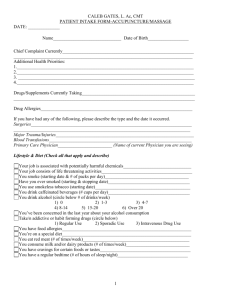
Lab 9 – Eukaryotic Microbes and Serology In this lab you will be examining several eukaryotic organisms of medical and/or commercial importance. Recall that eukaryotic organisms are divided into four kingdoms: animalia, plantae, fungi, and protista. You will view slides from all kingdoms, with the exception of the plant kingdom. We will also be looking at human blood smears in this lab and doing blood typing. Exercise 1: Kingdom Fungi Fungi are non-motile organism that secrete exoenzymes into the environment, and then absorb the digested materials. They can either obtain their nutrients by decomposing dead organic matter (saprophytes) or living plants, animals, or humans (parasites). The life cycle of a fungus usually involves both a sexual and an asexual form. Gametes (sexual reproduction) are produced by gametangia, while spores (asexual reproduction) are produced by sporangia. In lab 1, you viewed unicellular yeast. This week, you will focus on several multicellular, filamentous molds including Rhizopus, Aspergillus, and Penicillium. The individual filaments in these fungi are called hyphae, and are collectively termed mycelium. Rhizoids anchor the hyphae and the sporangia supporting sporangiophores. Rhizopus Rhizopus is a fast-growing species of fungus that darkens with age, giving it a “salt and pepper” appearance. Under the microscope, Rhizopus can be identified by its large, circular sporangia. The sporangium is supported by a hemispherical columella. Rhizopus stolonifer is a common bread mold. Other species of Rhizopus, including, R. arrhizus, are responsible for zygomycosis, a potentially fatal infection. Infection occurs when spores are inhaled and delivered to the tissues by the blood. This may result in necrosis in diabetic and immunocompromised patients. Aspergillus Aspergillus is a common environmental fungus. Species of Aspergillus can be found in a variety of colors, ranging from yellow to green to brown, and sometimes black. Aspergillus forms distinctive chains of spores at the end of hyphae, called conidia. Some species of Aspergillus cause an opportunistic infection called aspergillosis. Symptoms of aspergillosis vary based on conditions of exposure. Pulmonary aspergillosis colonizes bronchial tissue that has been damaged by conditions such as tuberculosis. Allergic aspergillosis causes asthma-like symptoms in individuals sensitized to the spores. Invasive aspergillosis results in necrotizing pneumonia and may spread to other organs. Penicillium Penicillium is also a common environmental fungus. Green, powdery colonies that radiate to a white apron characterize Penicillium when viewed on a plate or other surface. The colonies are a lighter color on the opposite surface. When viewing microscopically, brush-shaped conidiophores are observed. While Penicillium may cause an infection known as penicilliosis, it is better known for the production of the antibiotic penicillin. Penicillium is also used as the fermenting agent in the production of cheese. Objective: To identify each of these fungi based on their appearance and be able to associate each with its medical/commercial importance. Results: 1. Draw a sample of each organism 2. What is the medical/commercial importance of Rhizopus? 3. What is the medical/commercial importance of Aspergillus? 4. What is the medical/commercial importance of Penicillium? Exercise 2: Kingdom Protista The organisms we will examine from this Kingdom are the protozoans. Protozoans are unicellular, heterotrophic microorganisms. The life cycles of protozoans are generally important in their pathogenicity. The basic life cycle consists of a vegetative trophozoite stage and a resting cyst (egg) stage. The differences between life cycles of each protozoan included in this lab can be found in the diagrams below. Protozoans are classified based on their method of locomotion: Members of the subphylum Mastigophora move using flagella. In this lab you will view the flagellate Giardia lamblia and Trypanosoma. Members of the subphylum Sarcodine move using cytoplasmic extensions called pseudopods. In this lab you will view the amoeboid Entamoeba histolytica. Members of the phylum Ciliophora move via cilia covering the cell. In this lab you will view the ciliate Balantidium coli. And members of the phylum Apicomplexa are generally nonmotile. In this lab you will view the Apicomplexa Plasmodium malaria. Giardia lamblia Giardia causes an intestinal illness called giardiasis. Giardiasis is one of the most common waterborne diseases in the United States. It is contracted by ingesting fecally contaminated food or water or by putting objects in the mouth that have come in contact with feces contaminated with Giardia. Symptoms of giardiasis including diarrhea, gas, greasy stools, stomach cramps, and nausea may appear 1 to 2 weeks following infection and may persist for 2 to 6 weeks. Giardia infection is diagnosed by observing trophozoites or cysts in stool samples. In this lab, you will observe Giardia lamblia trophozoites in a fecal smear. Note that because you are viewing a fecal smear, there will be many organisms other than Giardia, which may make it difficult to find the Giardia. Objectives: Identify Giardia trophozoites in a fecal smear. Know the method of transmission for Giardia. Know the symptoms of giardiasis. Know how Giardia infections are diagnosed. Results: 1. How are Giardia infections diagnosed? 2. How is Giardia transmitted to humans? 3. What diseases are caused by Giardia infections and what are the symptoms? Trypanosoma Trypanosoma causes the potentially fatal trypanosomiasis, or sleeping sickness. While there are approximately 25,000 cases reported to the World Health Organization each year, many go unreported because they occur in parts of Africa that lack the infrastructure to get accurate reporting of cases. The only cases seen in the U.S. have been among individuals who had traveled to Africa. Symptoms of sleeping sickness generally begin 1 to 4 weeks after being bit by an infected tsetse fly. The bite may be painful and develop into a chancre. The infected individual may experience fever, severe headaches, irritability, fatigue, swollen lymph nodes, and aching muscles and joints. Untreated, the infected individual will develop confusion, slurred speech, seizures, and difficulty walking and talking due to invasion of the central nervous system. Death will occur in several weeks to months if treatment is not received. Trypanosoma infection is diagnosed by observation of blood samples or spinal fluid. In this lab you will observe Trypanosoma in blood smears. Objectives: Identify Trypanosoma blood smear. Know the method of transmission for Trypanosoma. Know the symptoms of sleeping sickness. Know how Trypanosoma infections are diagnosed. Results: 1. How are Trypanosoma infections diagnosed? 2. How is Trypanosoma transmitted to humans? 3. What diseases are caused by Trypanosoma and what are the symptoms? Entamoeba histolytica Entamoeba causes the intestinal disease amebiasis, which is characterized by loose stool, stomach pain and cramping in most instances. In severe cases, amebic dysentery (bloody stool and fever) can occur. Entamoeba is transmitted by ingesting cysts from fecally contaminated food, water, or other objects. Symptoms of the disease generally set in 1 to 4 weeks following ingestion. Entamoeba infection is diagnosed by observation of trophozoites or cysts in a fecal sample. It should be noted that the pathogenic Entamoeba histolytica looks identical to a more common, and nonpathogenic species of Entamoeba (E. dispar) under the microscope. This leads to false positives in laboratory tests. Objectives: Identify Entamoeba in a fecal smear. Know the method of transmission for Entamoeba. Know the symptoms of amebiasis. Know how Entamoeba infections are diagnosed. Results: 1. How are Entamoeba infections diagnosed? 2. How is Entamoeba transmitted to humans? 3. What diseases are caused by Entamoeba and what are the symptoms? Plasmodium malaria Plasmodium, the causative agent of malaria, is spread to human by the female Anopheles mosquito. As seen in the figure below, Plasmodium has a more complex lifecycle than the other eukaryotic microbes we are examining in this lab. After a mosquito introduces the sporozoite form of the protozoan into a human host, it goes through development stages in both the liver and the blood. The liver stage involves multiplication of the parasite. Once released from the liver, the Plasmodium enters red blood cells, where they multiply and are released to continue invading other red blood cells. It is the blood stage that causes the symptom of malaria, including fever, chills, sweats, fatigue, headaches, muscle pains, nausea, and vomiting. Severe malaria may result in neurological complications, anemia, pulmonary edema, cardiovascular collapse, kidney failure, and death. Plasmodium infections are diagnosed by observing the red blood cells infected with the parasite in a blood smear. While this is a simple procedure, malaria often goes undiagnosed for a number of reasons. In places, such as the United States, where malaria is not endemic, clinicians often do not consider malaria as a possible diagnosis. In places where malaria is endemic, many people are carrying the parasite, but have developed a resistance to it. In this case, illness cannot always be attributed to the malaria. In these same countries, resources may be lacking to make a reliable and timely diagnosis. Objectives: Identify Plasmodium in a blood smear. Know the method of transmission for Plasmodium. Know the symptoms of malaria. Know how Plasmodium infections are diagnosed. Results: 1. How are Plasmodium infections diagnosed? 2. How is Plasmodium transmitted to humans? 3. What diseases are caused by Plasmodium and what are the symptoms? Exercise 3: Kingdom Animalia While worms themselves may not be microscopic, there is often microscopic evidence found in clinical specimens that is used to diagnose an infection, therefore the helminthes are often included in the discussion of eukaryotic microbes. The life cycle of the parasitic worms is often complex, involving several hosts. We will not go into the life cycle of these organisms, but rather focus on their clinical importance and diagnosis. The three major categories of clinically important parasitic worms are the trematodes (flukes), cestodes (tapeworms), and the nematodes (round worms). In this lab we will look at one example of each. Schistosoma mansoni Schistosoma is a parasitic worm that has a complicated life cycle involving both humans and aquatic snails. It causes schistosomiasis when contracted via contact with fecally contaminated water containing juvenile worms. These worms penetrate the skin and enter the body’s circulation, where they continue to develop. Eggs laid by the adults penetrate the intestinal wall and are excreted in the feces. While many infections are asymptomatic, fever, cough, abdominal pain, diarrhea, hepatospenomegaly, and eosinophilia may be experienced. There are over 200 million people infected worldwide. This disease is seen in many parts of the world, including Africa, South America, The Middle East, and Southeast Asia. Diagnosis is made by identification of eggs in stool or urine samples, depending on the species suspected. Objectives: Identify Schistosoma eggs. Know the method of transmission for Schistosoma. Know the symptoms of schistosomiasis. Know how Schistosoma infections are diagnosed. Results: 1. How are Schistosoma infections diagnosed? 2. How is Schistosoma transmitted to humans? 3. What diseases are caused by Schistosoma and what are the symptoms? Taenia Members of the genus Taenia are commonly known as tapeworms. Different species of Taenia infect different animals, such as T. saginata, the beef tapeworm, and T. solium, the pork tapeworm. Like other animal parasites, Taenia has a complex lifecycle involving multiple hosts. Humans may become infected with the tapeworms by ingesting raw or undercooked meat of an infected animal. Inside the human host, the tapeworm develops into an adult. The adult tapeworms head region consists of a structure called a scolex to attach to the small intestine. The length of the tapeworm varies by species, but is typically between 2 and 7 meters. The adult produces proglottids (segments containing both male and female reproductive organs). Near the head of the tapeworm, the proglottids are immature. As you move away from the head, the proglottids become mature and develop sex organs. At the distal end of the tapeworm the proglottids are gravid, meaning they contain fertilized eggs. The gravid proglottids break off from the tapeworm and may exit in the feces. Infection by the tapeworm may cause mild abdominal symptoms, or the infected person may be asymptomatic. The main symptom is often the passage of proglottids in the feces. Diagnosis is made by identification of eggs and proglottids in the feces. This cannot be done in the first 3 months following infection, as time is needed for the tapeworm to mature and produce gravid proglottids. Objectives: Identify the different regions of Taenia. Know the method of transmission for Taenia. Know the symptoms of a tapeworm infection. Know how Taenia infections are diagnosed. Results: 1. How are Taenia infections diagnosed? 2. How is Taenia transmitted to humans? 3. What diseases are caused by Taenia and what are the symptoms? Ascaris lumbricoides Ascaris infections are the most common type of worm infection, occurring worldwide. Infections are found most frequently in areas of poor hygiene and sanitation. People with infections are frequently asymptomatic, but may experience slow growth and weight gain. Infections occur when fecally contaminated soil is ingested. Eggs hatch in the stomach. Larvae migrate to the lungs and up the throat where they are once again swallowed. The larvae develop into in the intestines into adult worms. Eggs laid by the female are passed in the feces. Diagnosis of Ascaris infection is made by identifying eggs in the stool. Objectives: Identify Ascaris eggs. Know the method of transmission for Ascaris. Know the symptoms of an Ascaris infection. Know how Ascaris infections are diagnosed. Results: 1. How are Ascaris infections diagnosed? 2. How is Ascaris transmitted to humans? 3. What diseases are caused by Ascaris and what are the symptoms? Information in this lab modified from: Centers for Disease Control and Prevention. “CDC – Diseases and Conditions.” [Online] 4 April 2008. <http://www.cdc.gov/DiseasesConditions/ >. Exercise 4: Human Blood Smears A human blood smear will consist mainly of erythrocytes or red blood cells (RBC’s), but also contains many leukocytes or white blood cells (WBC’s). Leukocytes, which play very important roles in the immune system, come in a variety of forms. We can divide leukocytes in two main groups, granulocytes (have cytoplasmic granules) and agranulocytes (do not have granules). Each of these groups can be further subdivided. Neutrophils, eosinophils, and basophils are all granulocytes; while lymphocytes and monocytes are agranulocytes. With each playing a different role in the immune system, the relative abundance of each type of leukocytes can often be used as an indicator of a specific type of infection or illness. The abundance of leukocytes is determined by performing a differential blood cell count. Neutrophils, the most abundant type of leukocyte, are phagocytes that respond to bacterial infections. As you may deduce, increased concentrations of neutrophils are indicative of systemic bacterial infections. Anything causing a decrease in neutrophil numbers (congenital disorder, leukemia, chemotherapy, etc) will leave a person more susceptible to bacterial infections. Neutrophils are variable in appearance. Eosinophils, which account for 1-4% of leukocytes, play a role in the immune response in parasitic infections. An increase in eosinophil numbers is indicative of a parasitic infection, while a decrease in eosinophils is seen in conditions that result in increased glucocorticoid production, such as stress. Eosinophils appear as red granular cells with a two-lobed nucleus. Basophils, the least abundant leukocytes, account for 0.1-1% of leukocytes. They participate in the inflammatory response by secreting histamine. Low basophil counts, in conjunction with low neutrophil counts, indicate a high likelihood of leukemia. Basophils appear as purple granular cells with either a two-lobed or unlobed nucleus. Lymphocytes, a relatively abundant agranuloctye, account for 25-33% of leukocytes. There are several varieties of lymphocytes including natural killer cells, B cells, and T cells. Natural killer cells destroy virally infected or cancerous cells, while B and T cells participate in specific acquired immunity. An increase in lymphocyte numbers indicates a viral infection. Decreases in lymphocyte numbers are seen in immune deficiency disorders, such as HIV. Monocytes, like neutrophils, are phagocytic, but also act as antigen presenting cells for the immune system. When found in the bloodstream, these leukocytes are called monocytes, but are referred to as macrophages when they migrate into tissues. These cells are identifiable by their horseshoe-shaped nucleus. Objective: Identify each type of leukocyte. Understand the main functions of each type of leukocyte. Identify disorders/diseases associated with abnormal levels of each leukocyte. Materials: Commercially prepared human blood smears Leukocyte models Blood poster Procedure: 1. View the commercially prepared slide set up at the back of the lab. a. You may wish to refer to the poster available on the wall for “ideal” leukocytes. 2. View the leukocyte models. 3. Draw an example of each type of leukocyte. Results: 1. What are the two main groups of WBCs and which leukocytes fall into each category? 2. What is the major function of each WBC? 3. What is generally the most abundant type of WBC? 4. Which WBCs are phagocytic? 5. Which WBCs are involved in specific acquired immunity? 6. What is indicated by an increased eosinophil number? 7. What is indicated by an increased neutrophil concentration? 8. Which WBCs act as antigen presenting cells in the immune system? 9. What is the difference between a monocyte and a macrophage? Exercise 5: Blood Typing ABO and Rh blood typing are both types of hemagglutination (test in which clumping of red blood cells indicates a positive reaction). ABO blood typing looks for the presence of A and/or B antigens on the surface of red blood cells. Individuals with one type of antigen (antibody generating molecule) will produce antibodies against the other type. Refer to the chart below for the blood type, antigen found on the blood cell, and antibodies produced: Blood Type A B AB O Antigen(s) on RBC’s A B A and B none Antibodies Produced Anti-B Anti-A None Anti-A and Anti-B Notice that people with type AB blood do not produce antibodies against either antigen. This makes them “universal recipients” of blood. People with type O blood produce antibodies against both antigens, meaning they can only receive blood from another type O individual. However, the lack of antigens on their RBC’s make them “universal donors” of blood. Antibodies against a specific antigen cause the blood to agglutinate (clump) when it comes in contact with that antigen. We can determine blood type by adding our blood to both anti-A and anti-B antisera (blood serum that contains antibodies). Refer to the chart below for all possible reactions: Anti-A Antiserum Agglutination Anti-B Antiserum No Agglutination No Agglutination Agglutination Agglutination Agglutination No Agglutination No Agglutination Interpretation A antigen present B antigen absent A antigen absent B antigen present A antigen present B antigen present A antigen absent B antigen absent Blood Type A B AB O The Rhesus factor, or Rh factor, is determined in the same manner. Individuals that are Rh positive have the antigen on their RBC surface, while individuals that are Rh negative do not have the antigen on their RBC surface. Addition of anti-Rh antiserum to an Rh positive sample will cause agglutination. Objectives: Understand the principles behind hemagglutination reactions. Determine an individual’s blood type based on these reactions. Identify which blood types are most abundant in a population and which are least abundant. Materials: Blood typing kits o Lancets o Alcohol wipes o Well plates o Toothpicks o Bandages o Gloves o Sharps container o Anti-A antiserum o Anti-B antiserum o Anti-Rh antiserum o Artificial blood Procedure: 1. This can either be done either on your own blood or using the artificial blood supplied. 2. Extreme caution must be used in this lab. Universal precautions must be taken anytime bodily fluids, such as blood, are present. 3. Place a drop of anti-A antiserum in the well labeled “A”. 4. Place a drop of anti-B antiserum in the well labeled “B”. 5. Place a drop of anti-Rh antiserum in the well labeled “Rh”. 6. If using your own blood, clean the tip of the index finger with an alcohol pad. Let the alcohol dry. 7. Shake the hand you are going to prick and massage the index finger from the base to the tip. 8. Remove the blue tip of the lancet, place the narrow white tip against the side of the clean index finger and depress the button. If you are performing this step on a classmate, you must wear gloves. 9. Squeeze the finger over each of the wells to dispense a drop of blood into each drop of antiserum. Do not touch your finger to the antiserum. a. If you are using the artificial blood, squeeze a drop into each of the wells. 10. Discard the lancet into the sharps container. 11. Put a bandage over the wound. 12. Use a toothpick to mix the blood and antisera. Use a different toothpick for each well. 13. Gently rock the slide back and forth for a few minutes. 14. Look for agglutination in each of the wells. 15. You may use the chart above or the poster on the wall to help in determining your blood type. 16. Collect the class data to determine the percentage of students with each blood type Blood Type A B AB O # of students with blood type Total # of students in class % of students with blood type Results: 1. Which blood type is the universal donor? Why? 2. Which blood type is the universal recipient? Why? 3. What is the difference between an antigen and an antibody? 4. What antigens will present on RBCs of a B+ individual? 5. What type of antibodies will a B+ individual make? 6. What is hemagglutination? 7. If the blood clumps in the well is it positive or negative for that blood type?