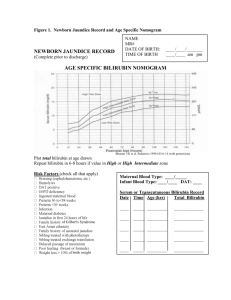
Neonatology
advertisement

Neonatology. Tests (Текстові тестові завдання) 1. Which of the following statements is NOT true of a normal full-term infant on the first day of life? A. * Fluid requirements are 100 ml/kg on the first day B. The average head circumference is 35 cm C. The urinary output is 1-3 ml/kg D. A true blood glucose of 2 mmol/l is within normal range E. The average blood pressure is 50-60 mm Hg 2. Which of the following statements is INCORRECT about fetal growth and development? A. Respiratory movements occure until birth B. Swallowing movements commence as early as 14 weeks gestation C. Haemoglobin is primarily HbF D. * Organogenesis occurs in the second trimester E. The third trimester is one of growth rather than differentiation 3. Routine newborn screening on a filer paper spot is NOT possible for which of the following 4. 5. 6. 7. 8. conditions? A. * Thalassaemia major B. Hypothyroidism C. G-6-PD deficiency D. Cystic fibrosis E. Galactosaemia In a full-term infant weighting 3,5 kg: A. the digestive tract lacks some of the enzymes needed for digestion of milk products B. supplements iron therapy is indicated from the age of 3 weeks C. subconjunctival haemorrhage is most likely to be due to strangulation by cord around the neck D. vaginal bleeding indicates haemorrhagic disease E. * blood volume is about 300 ml Which of the following statements concerning newborn is correct? A. Jaundice occurring on the second day of life is always pathological B. Hydrocele should be drained as early as possible to avoid testicular atrophy C. Eosinophilic rash (erythema toxicum) is an allergic manifestation D. * Ductus arteriousus usually closes physiologically within 48 hours E. Facial petechiae at birth are indicative of haemorrhagic disease Which of the following statements is correct? A. Gestational age of 35 weeks + 5 days should be considered as 36 weeks B. Preterm is defined as a gestation of less than 35 weeks C. Small-for-date babies are more than 42 weeks’ gestation D. * Postmature infants are more than 42 weeks’ gestation E. Neonatal period extends up to 30 days of life Which of the following definitions is correct? A. Stillbirth: death in utero prior to the complete expulsion of products of conception B. Neonatal death: death of a live-born infant in the first 30 days C. Premature infant: an infant weighting 2,5 kg or less at birth D. * Perinatal death: includes both death in utero after 20 weeks’ gestation (or birth weight 400 g or more) and death after delivery in the first 28 days of life E. Neonatal mortality rate: neonatal death devided by 1000 total birth In which of the following conditions is polyhydroamnios a recognized complication of pregnancy? A. Multiply birth B. Bile ducts atresia C. * Maternal diabetes mellitus D. Renal agenesis E. Maternal hypertension 9. Which of the following statements is true of alfa-fetoprotein (AFP)? A. Its concentration in amniotic fluid is normal in congenital nephrosis and in fetal intestinal 10. 11. 12. 13. 14. 15. 16. 17. atresia B. In amniotic fluid its concentration is maximum at 12-14 weeks’ gestation C. In maternal serum its maximum concentration is at 26 weeks’ gestation D. The main site of synthesis of AFP is the fetal spinal cord E. * AFP level is increased in open meningomyelocoeles Which of the following statements is NOT true of second trimester prenatal diagnosis? A. Diagnosis of neural tube defect doesn’t require cultivation of amniocytes B. It is possible to diagnose polycystic disease of kidneys C. * The risk of fetal death (i.e. unintended abortion) associated with amniocentesis is about 10 % in experienced hands D. DNA for diagnostic testing may be obtained from amniotic fluid E. Examination of maternal blood may lead to diagnosis of neural tube defect Central nervous system abnormalities associated with the fetal alcohol syndrome include: A. Mild to moderate mental retardation B. Microcephaly C. Irritability in the neonatal period D. Macroscopic changes in the brain E. * All is correct Perinatal asphyxia has been implicated in the etiology of: A. Necrotizing enterocolitis B. Meconium inhalation C. Hypoglycemia D. * All is correct E. Intraventricular hemorrhage Which of the following conditions is NOT recognized as being associated with respiratory difficulties in newborn infants? A. * Funnel chest (pectus excavatum) B. Oesophageal atresia C. Oligohydramnios D. Bilateral choanal atresia E. Micrognathia (receded chin) with cleft palate Choose the CORRECT statement about diaphragmatic hernia in the newborn: A. It’s more common on the right side than the left B. * It’s associated with pulmonary hypoplasia C. It’s symptomatic always D. Characteristically causes vomiting E. It can not be diagnosed with the help of chest X-ray Which of the following have more than a chance association with the small-for-dates infant? A. A high perinatal mortality B. Congenital malformation C. Permanent physical or mental retardation D. Idiopathic respiratory distress syndrome (hyaline membrane disease) E. * All is correct Which of the following neonatal problems is seen frequently in the infant of diabetic mother? A. Hypoglycemia B. Hyaline membrane disease C. Polycythemia D. Hyperbilirubinemia E. * All is correct Which of the following statements is true? A. Jaundice appearing 12 h after birth would suggest a greatly impaired glucoronyl transferase 18. 19. 20. 21. 22. 23. 24. activity B. During fetal life products of fetal haemoglobin breakdown are cleared by passage into the amniotic fluid C. * There is no risk of kernicterus in biliary atresia D. Biliary atresia is readily distinguished from neonatal hepatitis by liver functioning testing E. In newborn infants, beta-thalassaemia increases risk of hyperbilirubinemia Which of the following statements is NOT true in physiological jaundice? A. It always appears later than 24 hours B. It is due mainly to temporary impaired hepatic clearance of bilirubin C. In premature newborns it may persist for 3-4 weeks D. * Direct bilirubin level may be as high as indirect bilirubin level E. It can not be the reason of kernicterus Which of the following conditions have more than a chance association with non-conjugated hyperbilirubinemia in the first month of life? A. * Hypothyroidism B. Beta-thalassemia major C. Biliary atresia D. Fetal hepatitis E. Cytomegaloviral infection Which of the following conditions have more than a chance association with non-conjugated hyperbilirubinemia in the first month of life? A. Fetal hepatitis B. Beta-thalassemia major C. Biliary atresia D. Congenital syphilis E. * Hemolytic disease of newborn Which of the following conditions have more than a chance association with non-conjugated hyperbilirubinemia in the first month of life? A. Fetal hepatitis B. * Sickle-cell disease C. Biliary atresia D. Congenital syphilis E. All is correct Which of the following conditions have more than a chance association with non-conjugated hyperbilirubinemia in the first month of life? A. Hypothyroidism B. Sickle-cell disease C. Hemolytic disease of newborns D. Exclusive brest feeding E. * All is correct Which of the following conditions have more than a chance association with conjugated hyperbilirubinemia in the first month of life? A. Hypothyroidism B. Sickle-cell disease C. Hemolytic disease of newborns D. * Biliary atresia E. All is correct Which of the following conditions have more than a chance association with conjugated hyperbilirubinemia in the first month of life? A. Fetal hepatitis B. Cytomegaloviral infection C. Biliary atresia D. Toxoplasmosis E. * All is correct 25. In the newborn child was diagnosed physiological jaundice and erythema toxicum neonatorum. What 26. 27. 28. 29. 30. 31. 32. treatment should be performed? A. phototherapy and antibiotics B. antibiotics and sorbents C. antibiotics and local anilin dye D. sorbents and infusions E. *no need treatment In the newborn child was diagnosed transitory dysbacteriosis and physiological jaundice. What treatment should be performed? A. phototherapy and antibiotics B. antibiotics and sorbents C. antibiotics and local anilin dye D. probiotics and infusions E. *no need treatment For conjugative jaundice is typical the presence of: A. Cytolysis syndrome B. Hepatolienal syndrome C. Direct hyperbilirubinemia D. Hemolytic anemia E. *Indirect hyperbilirubinemia What changes in the complete blood test are typical for hemolytic disease of the newborn? A. Leucocytosis, anemia B. Thrombocytopenia, neutrophyllosis C. *Anemia, reticulocytosis D. Leucocytosis, shift of the formula to the left E. Erythropenia, leucopenia A child was born in term with signs of asphyxia. The estimation for Apgar scale on the first minute is 6 points. What is the first step of resuscitation in this case? A. *clearing the airways B. warming of the child C. oxygen therapy D. injection of adrenaline E. tactile stimulation The child was born with signs of meconial aspiration. What is the first step of resuscitation in this case? A. lower the head downwards, tactile stimulation B. suction of the contents from upper respiratory ways C. *intubation of trachea, sanation of airways D. suction of the contents from upper respiratory ways, oxygen therapy E. oxygen therapy, lavage of the tracheobronchial tree The child was born with signs of severe asphyxia. Were performed resuscitation actions by ABCresuscitation. What is the 3rd step of resuscitation? A. tactile stimulation B. suction of the contents from upper respiratory ways C. ventilation support D. oxygen therapy E. *indirect heart massage The decreased incidence of enteric infections noted in breastfed infants compared with formula-fed infants is MOST likely due to the A. more alkaline stool pH in breastfed infants B. nutritional benefits of human milk on the infant's immune system C. predominance of Bacteroides and Clostridium in the gut of breastfed infants D. *presence of protective antibodies against enteric infection in human milk E. sterility of human milk 33. In addition to irritability, sweating, and difficulty breathing with feeding, the symptom that is MOST 34. 35. 36. 37. 38. 39. 40. indicative of congestive heart failure in a 3-week-old infant is A. ascites B. cough C. cyanosis D. *diminished feeding volume E. pretibial edema Early hospital discharge is defined as the discharge of a newborn earlier than 48 hours following vaginal delivery or 96 hours following cesarean delivery. Of the following, the MOST common reason for readmission to the hospital within 7 days following an early discharge is: A. bacterial sepsis B. congenital heart disease C. gastrointestinal malformation D. *hyperbilirubinemia E. metabolic disorders Of the following, erythromycin prophylaxis is MOST likely to prevent ocular infection due to: A. Chlamydia trachomatis B. group B streptococci C. *Neisseria gonorrhoeae D. Staphylococcus aureus E. Trichomonas vaginalis Of the following, the condition that is MOST likely to present with seizures during the first 24 hours of life is: A. fetal alcohol syndrome B. herpes simplex infection C. *hypoxic-ischemic encephalopathy D. organic acidemia E. urea cycle defect Parents who wish to breast feed but want to supplement with formula should (choose the MOST correct statement): A. start supplementation at bedtime immediately after delivery B. *wait several weeks after delivery to supplement to ensure established breast-feeding hormonal atterns C. try a different formula each day until the baby shows a preference D. pump and then mix the formula and breast milk in a one to one ratio E. give only adopted formulas Choose the most correct statement for the first grade hypoxic-ischemic encephalopathy: A. newborn has hyperirritability, hyperreflexia, seazures B. newborn has hyporeflexia, muscle atonia, changes on EEG are absent C. *newborn has hyperirritability, hyperreflexia, tremor, changes on EEG are absent D. newborn has hyporeflexia, muscle atonia, changes on EEG are present E. newborn is in sopor or in coma Choose the most correct statement for the third grade hypoxic-ischemic encephalopathy: A. newborn has hyperirritability, hyperreflexia, seazures B. newborn has hyporeflexia, muscle atonia, changes on EEG are absent C. newborn has hyperirritability, hyperreflexia, seazures, changes on EEG are absent D. newborn has hyporeflexia, muscle atonia, changes on EEG are present E. *newborn is in sopor or in coma Choose the most correct statement for the third grade hypoxic-ischemic encephalopathy: A. newborn has hyperirritability, hyperreflexia, seazures B. newborn has hyporeflexia, muscle atonia, changes on EEG are absent C. newborn has hyperirritability, hyperreflexia, seazures, changes on EEG are absent D. newborn has hyporeflexia, muscle atonia, changes on EEG are present E. *newborn is in sopor or in coma 41. Choose the definition of the intranatal period: A. *begins from the first signs of the delivery, extends until the birth of the baby B. begins from the zygote formation, lasts up to the 8-th week of gestation C. begins from the 8-th week of gestation, continue up to the end of pregnancy D. begins from 28 weeks of gestation, extends until the 7 days after delivery E. begins from the birth of the baby, lasts until 7 days after birth 42. Choose the definition of the embrional development period: A. begins from the first signs of the delivery, extends until the birth of the baby B. *begins from the zygote formation, lasts up to the 8-th week of gestation C. begins from the 8-th week of gestation, continue up to the end of pregnancy D. begins from 28 weeks of gestation, extends until the 7 days after delivery E. begins from the birth of the baby, lasts until 7 days after birth 43. Choose the definition of the placental development period: A. begins from the first signs of the delivery, extends until the birth of the baby B. begins from the zygote formation, lasts up to the 8-th week of gestation C. *begins from the 8-th week of gestation, continue up to the end of pregnancy D. begins from 28 weeks of gestation, extends until the 7 days after delivery E. begins from the birth of the baby, lasts until 7 days after birth 44. Choose the definition of the perinatal period: A. begins from the first signs of the delivery, extends until the birth of the baby B. begins from the zygote formation, lasts up to the 8-th week of gestation C. begins from the 8-th week of gestation, continue up to the end of pregnancy D. *begins from 28 weeks of gestation, extends until the 7 days after delivery E. begins from the birth of the baby, lasts until 7 days after birth 45. Choose the definition of the early neonatal period: A. begins from the first signs of the delivery, extends until the birth of the baby B. begins from the zygote formation, lasts up to the 8-th week of gestation C. begins from the 8-th week of gestation, continue up to the end of pregnancy D. begins from 28 weeks of gestation, extends until the 7 days after delivery E. *begins from the birth of the baby, lasts until 7 days after birth 46. Choose the definition of the late antenatal period: A. begins from the first signs of the delivery, extends until the birth of the baby B. begins from the zygote formation, lasts up to the 8-th week of gestation C. *begins from 28 weeks of gestation, lasts until the 40 weeks of gestation D. begins from 28 weeks of gestation, extends until the 7 days after delivery E. begins from the birth of the baby, lasts until 7 days after birth 47. Choose the definition of the neonatal period: A. *begins from the birth of the baby, extends until 28 days after birth B. begins from the birth of the baby, extends until 60 days after birth C. begins from 28 weeks of gestation, lasts until the 40 weeks of gestation D. begins from 28 weeks of gestation, extends until the 7 days after delivery E. begins from the birth of the baby, lasts until 7 days after birth 48. Choose the definition of the late neonatal period: A. begins from the 14-th day of life, lasts until 28 days after birth B. *begins from the 7-th day of life, lasts until 28 days after birth C. begins from the birth of the baby, extends until 28 days after birth D. begins from the birth of the baby, extends until 60 days after birth E. begins from the birth of the baby, lasts until 14 days after birth 49. Neonatal period consists from the next periods: A. embrional development and placental development late antenatal, intranatal and early neonatal embrional and perinatal *early neonatal and late neonatal perinatal and early neonatal Intrauterine period consists from the next periods: A. *embrional development and placental development B. late antenatal, intranatal and early neonatal C. embrional and perinatal D. early neonatal and late neonatal E. perinatal and early neonatal Perinatal period consists from the next periods: A. embrional development and placental development B. *late antenatal, intranatal and early neonatal C. embrional and perinatal D. early neonatal and late neonatal E. perinatal and early neonatal Select the INCORRECT criterion concerning Apgar scale: A. heart rate B. reflex irritability C. skin color D. *body temperature E. muscle tone What medicines shoul be used for the newborn’s umbilical cord care for the first three days? A. solution of 0.5% chlorhexidine and antibiotic ointment B. *solution of 0.5% chlorhexidine and 70% alcohol (brilliant green, iodine tincture) C. solution of 0.5% chlorhexidine and water-based anylin dyes D. solution of 0.5% chlorhexidine and hydrogen peroxide E. not necessary asage of medecines When umbilical cord should become dry and should naturally fall off in healthy newborn? A. during 1-2 days of life B. *between 5-7-th days of life C. immediately after birth D. between 10-12 days of life E. till the end of the second week of life When is recommended to perform first breast feeding for the healthy newborn? A. *in delivery room immediately after birth B. during first 5 hours of life C. within 2 hours of life D. at the second day of life E. first feeding should be performed with adapted milk formula Choose the INCORRECT reason of the neonatal transient states? A. the environment becomes totally different B. change of barometric pressure C. unstable temperature of surroundings D. *fetal hypoxia E. microbic environment Choose the CORRECT reason of the neonatal transient states? A. intrauterine infection B. pathological delivery C. *unstable temperature of surroundings D. fetal hypoxia E. intrauterine growth restriction For transient weight loss is typical: B. C. D. E. 50. 51. 52. 53. 54. 55. 56. 57. 58. loss of up to 5 % of birth weight which may occur during the first 3 to 5 days loss of up to 15 % of birth weight which may occur during the first 3 to 5 days loss of up to 10 % of birth weight which may occur during the first 7 to 10 days loss of up to 15 % of birth weight which may occur during the first 7 to 10 days *loss of up to 10 % of birth weight which may occur during the first 3 to 5 days For transient weight loss is typical: A. loss of up to 3 % of birth weight B. loss of up to 5 % of birth weight C. *loss of up to 10 % of birth weight D. loss of up to 15 % of birth weight E. loss of up to 20 % of birth weight What is erythema toxicum neonatorum? A. local skin infection B. *transient allergic reaction to the environment C. type of allergic dermatitis D. first stage of flegmona in newborns E. rare complication of neonatal sepsis Choose the INCORRECT reason of physiological jaundice: A. functional immaturity of liver enzymes system B. destroy of hemoglobin F C. transient hypoproteinemia D. *ABO incompatibility E. increased enterohepatic circulation of bilirubin Choose the CORRECT reason of physiological jaundice: A. increased activity of liver enzymes system in newborns B. intensive excretion of bilirubin C. Rh - incompatibility D. ABO - incompatibility E. *increased enterohepatic circulation of bilirubin What is pathogenetic type of physiological jaundice? A. mechanical B. parenchymatous C. hemolytic D. *conjugated E. toxic What is name of the transient stool of the newborn? A. melena B. *meconium C. hematemesis D. lanugo E. “rice water” stool When does appear meconium in healthy newborns? A. during the first few minutes after birth B. *during the first few days after birth C. during the first few weeks after birth D. in the case of infection E. it doesn’t appear in healthy newborns What is typical for transient dysbacteriosis in newborn? A. *frequent watery greenish stool B. meconium during the first few days after birth C. frequent watery bloody stool D. “rice water” stool more then 15 times per day E. yellow soft stool 4-5 times per day A. B. C. D. E. 59. 60. 61. 62. 63. 64. 65. 66. 67. What is NOT typical for transient dysbacteriosis in newborn? A. frequent watery stool B. meconium during the first few days after birth C. greenish color of stool D. *increased body temperature E. normal general well-being 68. What does it mean – “early” discharge from maternity house? A. within 24 hours B. *within 30 hours C. within 48 hours D. within 72 hours E. earlier than 5 days 69. What is NOT contraindication to “early” discharge from maternity house? A. birth asphyxia B. maternal age 16 or younger C. presence of significant congenital anomalies D. congenital infection E. *absence of breast feeding 70. What is NOT contraindication to “early” discharge from maternity house? A. birth asphyxia B. *maternal age 30 or elder C. presence of significant congenital anomalies D. congenital infection E. multiple birth 71. What is contraindication to “early” discharge from maternity house? A. presence of skin erythema in newborn B. maternal age 30 or elder C. presence of meconium in newborn D. *presence of jaundice in newborn E. presence of anemia in mother 72. What should be treatment of physiological jaundice? A. phototherapy B. glucose infusions C. sorbents D. exchange blood transfusion E. *treatment isn’t necessary 73. Erb’s palsy is a result of: A. *C5-C6 injury B. C6-C7 injury C. C7-C8 injury D. C8-T1 injury E. C5-T1 injury 74. Klumpke’s paralyses is a result of: A. C5-C6 injury B. C6-C7 injury C. *C7-C8 injury D. C8-T1 injury E. C5-T1 injury 75. Kerer’s paralyses is a result of: A. C5-C6 injury B. C6-C7 injury C. C7-C8 injury D. C8-T1 injury E. *C5-T1 injury 76. Choose the INCORRECT statement about Horner’s syndrome in newborn: A. Occurs if cervical sympathetic fibers of the Th 1 are involved B. Are typical ptosis, myosis, enoftalmus and ipsilateral anhydrosis of face C. Causes include birth trauma, mediastinal or cervical tumors D. *Always occurs in brachial plexus injuries E. Is a frequent complication of Klumpke’s palsy 77. Clawlike deformity of hand in the newborn is the sign of: A. Kerer's palsy B. Acute osteomyelitis of the arm C. Erb's palsy D. Kofferate syndrome E. *Klumpke’s palsy 78. What is the possible indication for the lumbar puncture in newborns? A. Convulsive syndrome B. Neonatal meningitis C. Subarachnoid hemorrhage D. Hypertensive-hydrocephalic syndrome E. *All is correct 79. What should be treatment of uric acid infarct in newborns? A. antibiotics B. glucose infusions C. sorbents D. diuretics E. *treatment isn’t necessary 80. What should be treatment of hormonal crisis in newborns? A. estrogens B. androgens C. sorbents D. infusions E. *treatment isn’t necessary 81. What does mean early jaundice of newborn? A. Appeared immediately after birth B. Appeared within first 24 hours of life C. *Appeared within first 36 hours of life D. Appeared within first 48 hours of life E. Appeared within first 72 hours of life 82. What is the most frequent reason of “early” jaundice of newborn? A. Hepatitis B. *Hemolytic disease of newborns C. Hemorrhagic disease of newborns D. Allergy E. Sepsis 83. Choose CORRECT statement about early jaundice of newborn: A. *It’s always pathological B. It appears within first 48 hours of life C. It always disappears till 14 days of life D. TSB level doesn’t exceed 200 mkmol/L E. Sometimes it can occur in healthy newborn 84. Choose CORRECT statement about physiological jaundice of newborn: A. It appears within first 48 hours of life B. *It appears after 36 hours of life and lasts till 14 days C. It always disappears within 7 days of life D. There is direct hyperbilirubinemia E. It is typical triad: jaundice, anemia, hepatospleenomegaly 85. Choose CORRECT statement about physiological jaundice of newborn: A. It appears within first 48 hours of life B. It appears after 24 hours of life and lasts till 14 days C. It always disappears within 7 days of life D. *There is indirect hyperbilirubinemia E. It is typical triad: jaundice, anemia, hepatospleenomegaly 86. Choose CORRECT statement about physiological jaundice of newborn: A. It appears within first 48 hours of life B. *Level of TSB usually doesn’t exceed 250 mkmol/L C. It always disappears within 7 days of life D. There is acholic stool E. It should appear on the third day of life 87. Choose INCORRECT statement about early jaundice of newborn: A. It’s always pathological B. It appears within first 36 hours of life C. *It always disappears till 14 days of life D. It can be caused with fetal hepatitis E. It can be caused with neonatal sepsis 88. Choose INCORRECT statement about early jaundice of newborn: A. It’s always pathological B. *It appears within first 48 hours of life C. There is hepatospleenomegaly in most newborns with early jaundice D. It can be caused with fetal hepatitis E. It can be caused with neonatal sepsis 89. What does mean prolonged jaundice of term newborn? A. Lasts longer than 7 days B. *Lasts longer than 14 days C. Lasts longer than 21 days D. Lasts longer than 1 month E. All is correct 90. What does mean prolonged jaundice of preterm newborn? A. Lasts longer than 7 days B. Lasts longer than 14 days C. *Lasts longer than 21 days D. Lasts longer than 1 month E. All is correct 91. What does mean late jaundice of newborn? A. Lasts longer than 7 days B. Appear after 5 days C. *Appear after 7 days D. Appear after 10 days E. Lasts longer than 14 days 92. What can be the reason of prolonged jaundice of newborns? A. Hypothyroidism B. Intrauterine infection C. Brest milk intake D. *All is correct E. All is incorrect 93. What can be the reason of early jaundice of newborns? A. Hypothyroidism B. *Sepsis C. Brest milk intake D. All is correct E. All is incorrect 94. What is significant for the hemolytic jaundice? A. *Anemia, reticulocytosis, hepatospleenomegaly B. Direct hyperbilirubinemia, acholic stool C. Direct hyperbilirubinemia, colored stool, dark urine D. Indirect hyperbilirubinemia, absence of anemia, normal liver size E. Indirect hyperbilirubinemia, anemia, normal liver size 95. What is significant for the conjugated jaundice? A. Anemia, reticulocytosis, hepatospleenomegaly B. Direct hyperbilirubinemia, acholic stool C. Direct hyperbilirubinemia, colored stool, dark urine D. *Indirect hyperbilirubinemia, absence of anemia, normal liver size E. Indirect hyperbilirubinemia, anemia, normal liver size 96. What is significant for the mechanical jaundice? A. Anemia, reticulocytosis, hepatospleenomegaly B. *Direct hyperbilirubinemia, acholic stool C. Direct hyperbilirubinemia, colored stool, dark urine D. Indirect hyperbilirubinemia, absence of anemia, normal liver size E. Indirect hyperbilirubinemia, anemia, normal liver size 97. What is significant for the parenchymatous jaundice? A. Anemia, reticulocytosis, hepatospleenomegaly B. Direct hyperbilirubinemia, acholic stool C. *Direct hyperbilirubinemia, colored stool, dark urine D. Indirect hyperbilirubinemia, absence of anemia, normal liver size E. Indirect hyperbilirubinemia, anemia, normal liver size 98. What does mean “zone 1” according Kramer’s scale? A. *Face, neck B. Chest, abdomen C. Pelvis, buttocks, hips D. Arms, legs E. Hands, palms, feet 99. What does mean “zone 2” according Kramer’s scale? A. Face, neck B. *Chest, abdomen C. Pelvis, buttocks, hips D. Arms, legs E. Hands, palms, feet 100. What does mean “zone 3” according Kramer’s scale? A. Face, neck B. Chest, abdomen C. *Pelvis, buttocks, hips D. Arms, legs E. Hands, palms, feet 101. What does mean “zone 4” according Kramer’s scale? A. Face, neck B. Chest, abdomen C. Pelvis, buttocks, hips D. *Arms, legs E. Hands, palms, feet 102. What does mean “zone 5” according Kramer’s scale? A. Face, neck Chest, abdomen Pelvis, buttocks, hips Arms, legs *Hands, palms, feet 103. What is the criterion of hospitalization of patient with prolonged and late jaundices? A. Worsening of newborn’s state B. Total serum bilirubin > 11,7 mg/dL C. Conjugated serum bilirubin > 1,9 mg/dL (> 20 % of TSB) D. Liver or spleen enlargement E. *All is correct 104. What IS NOT the criterion of hospitalization of patient with prolonged and late jaundices? A. Worsening of newborn’s state B. Total serum bilirubin > 11,7 mg/dL C. Conjugated serum bilirubin > 1,9 mg/dL (> 20 % of TSB) D. Liver or spleen enlargement E. *Presence of jaundice in the 3 zone 105. The child is 5 days of life. In general blood test: RBC 5.2х10^12/l, Hemoglobin 150 g/l, Hematocrit (PCV) 48 %, WBC 11,2х10^9/l. This is typical for: A. DIC-syndrome B. Hemorrhagic disease of the newborn C. *Healthy child D. Sepsis E. Anemia 106. The child is 7 days of life. In general blood test: RBC 5.2х10^12/l, Hemoglobin 140 g/l, Hematocrit (PCV) 42 %, WBC 11,2х10^9/l. This is typical for: A. Polycythemia B. Meningitis C. Healthy child D. Sepsis E. *Anemia 107. Of the following, the MOST important determinant of neurodevelopmental outcome of VLBW infants is A. antenatal obstetric management B. infant gender C. *length of gestation D. maternal education E. socioeconomic status 108. Of the following, the MOST helpful finding to distinguish GBS pneumonia from RDS is: A. a normal C-reactive protein level B. an elevated erythrocyte sedimentation rate C. diffuse alveolar infiltrates on chest radiography D. *increased ratio of bands to segmented neutrophils E. persistent hypoxemia on blood gas analysis 109. A 900 g male infant is delivered vaginally to a woman who had no prenatal care. Of the following, the physical finding that is MOST consistent with prematurity is: A. creases over entire sole of foot B. descended testes with deep rugae of the scrotum C. formed and firm pinna with instant recoil D. *gelatinous translucent skin E. raised areola and 3 mm breast buds 110. The X-ray signs of hyaline membrane disease are the next EXCvvEPT: A. reticulogranular pattern B. “white lights” B. C. D. E. C. *lungs emphysema D. air bronchograms E. absence of cardiac shadow What body weight is typical for the II grade of prematurity: 1000 g *1800 g 2100 g 1200 g 1300 g 112. What are the criteria of prematurity? A. birth weight less than 2000 g, gestational age less tnan 38 weeks B. birth weight less till 2500 g, gestational age less 37-38 weeks C. *birth weight less than 2500 g, gestational age 28-37 weeks D. birth weight less than 2500 g, gestational age less tnan 35 E. birth weight less than 2500 g, gestational age 30-37 weeks 113. What from does depend choice of feeding method for premature newborn? A. prematurity stage B. CNS maturity C. gestational age D. *sucking reflex grade E. birth weight 114. Absence of intercostal spaces retractions during breathing according to Silverman scale can be estimated as: A. *O points B. 1 point C. 2 points D. 3 points E. Shouldn’t be estimated 115. Absence of chin movements during breathing according to Silverman scale can be estimated as: A. *O points B. 1 point C. 2 points D. 3 points E. Shouldn’t be estimated 116. Mild retraction of sternum during breathing according to Silverman scale can be estimated as: A. O points B. *1 point C. 2 points D. 3 points E. Shouldn’t be estimated 117. Surfactant deficiency is the etiological factor of: A. Neonatal pneumonia B. *Respiratory distress syndrome C. Congenital lung atelectasis D. Acidosis E. Asphyxia 118. Choose the diagnostic criteria of the prematurity III grade: A. *Gestational age 29-31 weeks, birth weight 1000-1500 grams B. Gestational age 28 weeks or less, birth weight less than 1500 grams C. Gestational age 35-37 weeks, birth weight 2000-2500 grams D. Gestational age 32-34 weeks, birth weight 1500-2000 grams E. Gestational less than 31 weeks, birth weight less than 1500 grams 111. A. B. C. D. E. 119. A. B. C. D. E. 120. A. B. C. D. E. 121. A. B. C. D. E. 122. A. B. C. D. E. 123. A. B. C. D. E. 124. A. B. C. D. E. 125. A. B. C. D. E. 126. A. B. C. D. E. 127. A. B. C. D. What is usually used for the feeding of newborns whose gestational age is 33-35 weeks? Nasogastric tube *Bottle Teaspoon Mother’s breast Syringe What is usually used for the feeding of newborns whose gestational age is 33-35 weeks? *Nasogastric tube Bottle Teaspoon Mother’s breast Syringe What is gestational age for the 2-nd grade of prematurity? 33-34 weeks *34-32 weeks 36-37 weeks 37-38 weeks 32-33 weeks What is gestational age for the 4-th grade of prematurity? 29-31 weeks 32-34 weeks *less than 28 weeks less than 26 weeks 35-37 weeks For antenatal prophylaxis of the hyaline membrane disease are used: antibiotics surfactant vitamins *glucocorticoids prophylaxis isn’t necessary to perform What is gestational age for the I-st grade of prematurity? 29-31 weeks 32-34 weeks less than 28 weeks less than 26 weeks *35-37 weeks What is gestational age for the 3-rd grade of prematurity? *29-31 weeks 32-34 weeks less than 28 weeks less than 26 weeks 35-37 weeks Which treatment of hyaline membrane disease is the most important? antibiotics *surfactant vitamins glucocorticoids oxygen inhalation For skin changes in premature newborns is typical everything EXEPT: Lanugo presence Visible vessels Hyperemia *Papular rusn E. Presence of jaundice Choose the most typical sign of prematurity: *Opened posterior fontanel Opened anterior fontanel Skin peeling Presence of jaundice All is correct 129. For the premature newborn is typical: A. Opened posterior fontanel B. Opened anterior fontanel C. Skin peeling D. Presence of jaundice E. *All is correct 130. What is the etiology of hyaline membrane disease? A. Bacterial B. Viral C. Hereditary D. *Surfactant deficiency E. All is correct 131. Among the following, the condition that is MOST likely to predispose a pediatric patient to the evelopment of systemic candidosis is: A. history of atopy B. history of prematurity C. *immunosuppression D. presence of an indwelling urinary catheter E. recent tonsillectomy 132. Of the following, erythromycin prophylaxis is MOST likely to prevent ocular infection due to: A. Chlamydia trachomatis B. group B streptococci C. *Neisseria gonorrhoeae D. Staphylococcus aureus E. Trichomonas vaginalis 133. The most common bacterial pathogens for neonatal osteomyelitis are: A. H. influenza, Moraxella catarrhalis and Pneumococcus B. N. gonnorhea, Bacteroides and Enterobacter C. *Group B Streptococcus, E. coli, S. Aureus D. Actinomycetes Isralei, Pseudomonas, Peptostreptococcus E. Salmonella, Shigella, Campylobacter 134. The signs and symptoms of meningitis in an infant can be different than those in an adult. Which of he signs and symptoms of meningitis listed below is more helpful in an adult patient than in a 4-month-old? A. Lethargy B. Jaundice C. Vomiting D. *Brudzinski’s sign E. Hypothermia 135. What are the skin lesions of the herpes? A. Scales B. Papules C. *Vesicles D. Pustules E. Wheals 136. What are the skin lesions of the impetigo? 128. A. B. C. D. E. A. B. C. D. E. 137. A. B. C. D. E. 138. A. B. C. D. E. 139. A. B. C. D. E. 140. A. B. C. D. E. 141. A. B. C. D. E. 142. A. B. C. D. E. 143. A. B. C. D. E. 144. A. B. C. D. E. Scales Ulcers Reddish maculae *Crusts Plaques What is the cause of the plethora? Choose the most correct and complete answer: Vitamins and proteins deficiency *Increased numbers of erythrocytes as a compensatory response to chronic hypoxia Decreased level of hemoglobin Decreased numbers of erythrocytes as a compensatory response to chronic hypoxia Increased level of hemoglobin What are the skin lesions of the nevus? Plaques Patches Papules *Maculae Nodules What are the skin lesions of the second-degree burn? Vesicles Wheals Cysts *Bullae Patch What are the skin lesions of the psoriasis? Scars Crusts *Scales Maculae Pustules What are the skin lesions of the nevus? Plaques Patches Papules *Maculae Nodules What are the skin lesions of the second-degree burn? Vesicles Wheals Cysts *Bullae Patch What are the skin lesions of the psoriasis? Scars Crusts *Scales Maculae Pustules What are the sizes of petechiae? 3 cm or less 1 cm or more *2 mm or less 3 mm or more 2 mm or more What is xeroderma? A. Excessive oily skin B. *Excessive dry skin C. Excessive clammy skin D. Excessive moist skin E. Excessive flabby skin 146. What are the skin lesions of the cavernous hemangioma? A. Patch B. Reddish maculae C. Plaque D. Erosion E. *Tumor 147. What are the skin lesions of the folliculitis? A. Vesicles B. *Pustules C. Cysts D. Bullae E. Wheals 148. Flat area of the skin color change less 1 cm in diameter, neither elevated no depressed and without lteration in the skin texture. What is this? A. Patch B. Petechiae C. Plaque D. *Maculae E. Papule 149. Of the following, the condition that is MOST likely to present with seizures during the first 24 hours f life is A. etal alcohol syndrome B. herpes simplex infection C. *hypoxic-ischemic encephalopathy D. organic acidemia E. urea cycle defect 150. Select the INCORRECT statement concerning congenital syphilis: A. late symptoms of the untreated child include keratitis, blindness, saber shin, and mulberry molars B. placental examination may show mononuclear infiltrate with spirochetes present C. *the tertiary syphilis stage is more likely to infect a fetus than either the primary or secondary stages D. a large percentage of fetuses will die in-utero E. at birth chronic rhinitis and desquamating rash may be the only symptoms 151. Select the TRUE statement for HIV positive mothers (positive before and at the birth of child): A. 90-100% will infect the child during delivery B. must not take zidovudine (AZT) due to its teratogenicity C. *should not breast feed their HIV-negative children D. must insist their HIV positive child be immunized with all vaccines scheduled for a non-HIV positive hild E. for such mothers pregnancy is contraindicated 152. What is the medicine of the choice for congenital CMV-infection treatment ? A. Sumamed B. Chloridin C. Acyclovir D. Ampicillin 145. E. *Ganciclovir 153. A. B. C. D. E. 154. A. B. C. D. E. 155. A. B. C. D. E. 156. A. B. C. D. E. 157. A. B. C. D. E. 158. A. B. C. D. E. 159. A. B. C. D. E. 160. A. B. C. D. E. 161. A. B. C. Approximately 30%-50% of infants born from Chlamydia-positive mothers will have *Conjunctivitis Dermatitis Jaundice Pneumoniae Pyelonephritis What ocular lesion is typical for neonatal toxoplasmosis: *Chorioretinitis Anterior uveitis Keratoconjunctivitis Cataract Optic neuritis Hydrocephalus is the most typical for: Rubella CMV *Toxoplasmosis Lysteriosis Syphilis Select the INCORRECT statement concerning toxoplasmosis: Toxoplasmosis is a parasitic infection Most of the infected pregnant women are asymptomatic *Most of the infected newborns will be asymptomatic Infection rate increases with gestational age Sabin-Feldman dye test is used for diagnostics of maternal toxoplasmosis Choose the clinical feature of TORCH-syndrome: Low birthweight Jaundice Hepatosplenomegaly Seizures *All is correct Toxoplasma gondii belongs to: Viruses Bacteria Fungi *Parasites All is incorrect Cat is the definitive host in the contamination mechanism of: Staphylococcal infection Candidosis Lysteriosis *Toxoplasmosis Syphilis Raw meat can be the source of contamination with: Staphylococcal infection Candidosis Lysteriosis *Toxoplasmosis Syphilis What bacteria can be revealed in darkfield microscopy? Trypanosoma cruzi Toxoplasma gondii *Treponema pallidum D. Listeria monocytogenes E. Cytomegalovirus What changes in the CSF are typical for congenital toxoplasmosis? A. *Xanthochromia, lymphocytic pleocytosis, increased protein concentration B. Increased sugar concentration, high pressure C. Cloudiness, neutrophylic pleocytosis, increased protein concentration D. Xanthochromia, presence of erythrocytes, high pressure E. Changes in CSF are not typical for the congenital toxoplasmosis 163. What is the medicine of choice for the congenital toxoplasmosis treatment in newborns? A. Spiramycin B. *Pyrimethamine C. Penicillin D. Metronidazol E. Ceftriaxon 164. What medicine should NOT be used for the congenital toxoplasmosis treatment in newborns? A. *Spiramycin B. Pyrimethamine C. Sulfadiazin D. Leukovorin E. Prednisolon 165. Choose the most CORRECT statement about neonates of mothers with positive Wassermann reaction: A. They always should be treated with penicillin B. They can be considered healthy if they have not clinical symptoms of syphilis C. *For them should be performed darkfield microscopy of any skin or mucosal lesions and a quantitative ontreponemal serum test D. They should be isolated from mother E. For them should be also performed Wassermann reaction immediately 166. What medicine should be used for the congenital syphilis treatment in newborns? A. Pyrimethamine B. *Penicillin G C. Ampicillin D. Ceftriaxon E. Acyclovir 167. What is the daily dose of penicillin G for the congenital syphilis treatment in newborns during the irst 7 days of life? A. 50000 nits/kg B. *100000 units/kg C. 150000 units/kg D. 100 mg/kg E. 150 mg/kg 168. What is the daily dose of penicillin G for the congenital syphilis treatment in newborns from the 7-th ill 10-th day of life? A. 50000 units/kg B. 100000 units/kg C. *150000 units/kg D. 100 mg/kg E. 150 mg/kg 169. What is the daily dose of procaine penicillin (Bicillin) for the congenital syphilis treatment in ewborns? A. *50000 units/kg B. 100000 units/kg C. 150000 units/kg 162. D. 100 mg/kg E. 150 mg/kg 170. 171. 172. 173. 174. 175. 176. 177. 178. What medicine should be used for the congenital syphilis treatment in newborns? A. Pyrimethamine or spyramycin B. *Penicillin G or procaine penicillin C. Ampicillin or gentamycine D. Ceftriaxon or cefotaxim E. Acyclovir or gancyclovir The fetus is at highest risk for rubella developmental abnormalities when he is infected: A. During the first half of pregnancy B. *During the 1-st ( 16-th week of gestation, particularly between the 8-th and 10-th week D. During the 10-th ( 20-th week of gestation C. During the 12-th ( 24-th week of gestation, particularly between the 16-th and 18-th week E. During the last month of gestation What is the most dangerous period for rubella contacts for pregnant women? A. *The first trimester of pregnancy B. The second trimester of pregnancy C. The third trimester of pregnancy D. The last several days before delivery E. Any period of pregnancy Cardiac defects development in fetus is the most typical for: A. Congenital toxoplasmosis B. CMV infection C. *Congenital rubella D. Herpes E. Congenital syphilis Cataracts development in fetus is the most typical for: A. Congenital toxoplasmosis B. *Congenital rubella C. CMV infection D. Herpes E. Congenital syphilis The classic triad for congenital rubella syndrome is: A. Rush, CNS abnormalities (seizures), eye abnormalities (cataract, microphtalmia) B. Congenital heart defects, jaundice, sensorineural hearing loss C. Eye abnormalities (cataract, microphtalmia), microcefalus, rush D. *Eye abnormalities (cataract, microphtalmia), congenital heart defects, sensorineural hearing loss E. Congenital heart defects, sensorineural hearing loss, CNS abnormalities (seizures) What is the preferred diagnostics technique for newborns in congenital rubella syndrome? A. Enzyme-linked immunosorbent assay (ELISA) for Ig G detection B. Immunofluorescent assay (IFA) for Ig G detection C. *Viral isolation D. Rubella-specific Ig M detection E. CT scanning of the head What is the etiological treatment of congenital listeriosis? A. Ampicillin with Cefatoxim B. *Ampicillin with Amikacin C. Acyclovir D. Pyrimethamine and Sulfadiazin E. There is no etiological treatment What is the etiological treatment of congenital cytomegalovirus infection? A. Ampicillin B. C. D. E. 179. A. B. C. D. E. 180. A. B. C. D. E. 181. A. B. C. D. E. 182. A. B. C. D. E. 183. A. B. C. D. E. 184. A. B. C. D. E. 185. A. B. C. D. E. 186. A. B. C. D. E. 187. *Ganciclovir Acyclovir Pyrimethamine There is no etiological treatment What medicines should be chosen for the treatment of congenital cytomegalovirus infection? Ampicillin and Cefatoxim Ampicillin and Amikacin *Ganclovir and Cytotect Acyclovir and Prednison Pyrimethamine and Sulfadiazin What is the etiological treatment of congenital rubella? Ampicillin Ganciclovir Acyclovir Pyrimethamine *There is no etiological treatment What is daily dose of ganciclovir for the treatment of congenital cytomegalovirus infection? 1 mg/kg *5 mg/kg 10 mg/kg 15 mg/kg 20 mg/kg What is daily dose of foskarnet for the treatment of congenital cytomegalovirus infection? 1 mg/kg 10 mg/kg 20 mg/kg *60 mg/kg 100 mg/kg What is the etiological treatment of congenital HSV infection? Ampicillin Ganciclovir *Acyclovir Pyrimethamine There is no etiological treatment What is the preferred diagnostics technique for newborns in congenital HSV infection? Enzyme-linked immunosorbent assay (ELISA) Immunofluorescent assay (IFA) *Tissue culture CSF analyses Complete blood count What infection is NOT included into TORCH-syndrome? Syphilis Hepatitis B Toxoplasmosis *Tuberculosis HIV-infection What infection is NOT included into TORCH-syndrome? Rubella Herpes simplex Parvovirus *Candidosis HIV infection What infection is included into TORCH-syndrome? Staphylococcal Hepatitis C *Syphilis Tuberculosis Candidosis 188. What infection is included into TORCH-syndrome? A. Streptococcal B. *Hepatitis B C. Klebsiella D. Tuberculosis E. Candidosis 189. What symptom is the most typical for congenital clamidiosis? A. Jaundice B. Hydrocefalus C. Seizures D. *Purulent conjunctivitis E. Maculopapular rash 190. What symptom is the most typical for congenital listeriosis? A. Dyspnea B. Microcefalus C. Purulent conjunctivitis D. Rinitis E. *Maculopapular rash 191. What symptom is the most typical for congenital HSV infection? A. Dyspnea B. *Encephalitis C. Purulent conjunctivitis D. Rinitis E. Maculopapular rash 192. What symptom is the most typical for congenital mycoplasmosis? A. *Dyspnea B. Hydrocefalus C. Purulent conjunctivitis D. Rinitis E. Maculopapular rash 193. What symptom is the most typical for congenital syphilis? A. Cataract B. Meningitis C. Purulent conjunctivitis D. *Rinitis E. Hydrocefalus 194. Of the following, erythromycin prophylaxis is MOST likely to prevent ocular infection due to: A. Chlamydia trachomatis B. group B streptococci C. *Neisseria gonorrhoeae D. Staphylococcus aureus E. Trichomonas vaginalis 195. Of the following, the condition that is MOST likely to present with seizures during the first 24 hours f life is: A. fetal alcohol syndrome B. herpes simplex infection C. *hypoxic-ischemic encephalopathy D. organic acidemia A. B. C. D. E. E. urea cycle defect Which of the following statements is INCORRECT about fetal growth and development? Respiratory movements occure until birth Swallowing movements commence as early as 14 weeks gestation Haemoglobin is primarily HbF Organogenesis occurs in the second trimester The third trimester is one of growth rather than differentiation 197. Routine newborn screening on a filer paper spot is NOT possible for which of the following conditions? A. Thalassaemia major 2. B. Hypothyroidism 3. C. G-6-PD deficiency 4. D. Cystic fibrosis E. Galactosaemia 198. Which of the following statements is NOT true of a normal full-term infant on the first day of life? A. Fluid requirements are 100 ml/kg on the first day B. The average head circumference is 35 cm C. The urinary output is 1-3 ml/kg D. Blood glucose of 2 mmol/l is within normal range E. The average blood pressure is 50-60 mm Hg 199. In a full-term infant weighting 3,5 kg: A. the digestive tract lacks some of the enzymes needed for digestion of milk products B. supplements iron therapy is indicated from the age of 3 weeks C. subconjunctival haemorrhage is most likely to be due to strangulation by cord around the neck D. vaginal bleeding indicates haemorrhagic disease E. blood volume is about 300 ml 200. Which of the following statements concerning newborn is correct? A. Jaundice occurring on the second day of life is always pathological B. Hydrocele should be drained as early as possible to avoid testicular atrophy C. Eosinophilic rash (erythema toxicum) is an allergic manifestation D. Ductus arteriousus usually closes physiologically within 48 hours E. Facial petechiae at birth are indicative of haemorrhagic disease 201. Which of the following statements is correct? A. Gestational age of 35 weeks + 5 days should be considered as 36 weeks B. Preterm is defined as a gestation of less than 35 weeks C. Small-for-date babies are more than 42 weeks’ gestation D. Postmature infants are more than 42 weeks’ gestation E. Neonatal period extends up to 30 days of life 202. Which of the following definitions is correct? A. Stillbirth: death in utero prior to the complete expulsion of products of conception B. Neonatal death: death of a live-born infant in the first 30 days C. Premature infant: an infant weighting 2,5 kg or less at birth D. Perinatal death: includes both death in utero after 20 weeks’ gestation (or birth weight 400 g or more) and death after delivery in the first 28 days of life E. Neonatal mortality rate: neonatal death devided by 1000 total birth 203. In which of the following conditions is polyhydroamnios a recognized complication of pregnancy? A. Multiply birth B. Bile ducts atresia C. Maternal diabetes mellitus D. Renal agenesis 196. A. B. C. D. E. E. Maternal hypertension 204. Which of the following statements is true of alfa-fetoprotein (AFP)? A. Its concentration in amniotic fluid is normal in congenital nephrosis and in fetal intestinal atresia B. In amniotic fluid its concentration is maximum at 12-14 weeks’ gestation C. In maternal serum its maximum concentration is at 26 weeks’ gestation D. The main site of synthesis of AFP is the fetal spinal cord E. AFP level is increased in open meningomyelocoeles Which of the following statements is NOT true of second trimester prenatal diagnosis? A. Diagnosis of neural tube defect doesn’t require cultivation of amniocytes B. It is possible to diagnose polycystic disease of kidneys C. The risk of fetal death (i.e. unintended abortion) associated with amniocentesis is about 10 % in experienced hands D. DNA for diagnostic testing may be obtained from amniotic fluid E. Examination of maternal blood may lead to diagnosis of neural tube defect 206. Central nervous system abnormalities associated with the fetal alcohol syndrome include: A. Mild to moderate mental retardation B. Microcephaly C. Irritability in the neonatal period D. Macroscopic changes in the brain E. All is correct 207. Perinatal asphyxia has been implicated in the etiology of: A. Necrotizing enterocolitis B. Meconium inhalation C. Hypoglycemia D. Intraventricular hemorrhage E. All is correct 208. Which of the following conditions is NOT recognized as being associated with respiratory difficulties in newborn infants? A. Funnel chest (pectus excavatum) B. Oesophageal atresia C. Oligohydramnios D. Bilateral choanal atresia E. Micrognathia (receded chin) with cleft palate 209. Choose the CORRECT statement about diaphragmatic hernia in the newborn: A. It’s more common on the right side than the left B. It’s associated with pulmonary hypoplasia C. It’s symptomatic always D. Characteristically causes vomiting E. It can not be diagnosed with the help of chest X-ray 210. Which of the following have more than a chance association with the small-for-dates infant? A. A high perinatal mortality B. Congenital malformation C. Permanent physical or mental retardation D. Idiopathic respiratory distress syndrome (hyaline membrane disease) E. All is correct 211. Which of the following neonatal problems is seen frequently in the infant of diabetic mother? A. Hypoglycemia B. Hyaline membrane disease C. Polycythemia D. Hyperbilirubinemia E. All is correct 205. Which of the following statements is true? A. Jaundice appearing 12 h after birth would suggest a greatly impaired glucoronyl transferase activity B. During fetal life products of fetal haemoglobin breakdown are cleared by passage into the amniotic fluid C. There is no risk of kernicterus in biliary atresia D. Biliary atresia is readily distinguished from neonatal hepatitis by liver functioning testing E. In newborn infants, beta-thalassaemia increases risk of hyperbilirubinemia 213. Which of the following statements is NOT true in physiological jaundice? A. It always appears later than 24 hours B. It is due mainly to temporary impaired hepatic clearance of bilirubin C. In premature newborns it may persist for 3-4 weeks D. Direct bilirubin level may be as high as indirect bilirubin level E. It can not be the reason of kernicterus 214. Which of the following conditions have more than a chance association with non-conjugated hyperbilirubinemia in the first month of life? A. Hypothyroidism B. Beta-thalassemia major C. Biliary atresia D. Fetal hepatitis E. Cytomegaloviral infection 215. Which of the following conditions have more than a chance association with non-conjugated hyperbilirubinemia in the first month of life? A. Fetal hepatitis B. Beta-thalassemia major C. Biliary atresia D. Congenital syphilis E. Hemolytic disease of newborn 216. Which of the following conditions have more than a chance association with non-conjugated hyperbilirubinemia in the first month of life? A. Fetal hepatitis B. Sickle-cell disease C. Biliary atresia D. Congenital syphilis E. All is correct 217. Which of the following conditions have more than a chance association with non-conjugated hyperbilirubinemia in the first month of life? A. Hypothyroidism B. Sickle-cell disease C. Hemolytic disease of newborns D. Exclusive brest feeding E. All is correct 218. Which of the following conditions have more than a chance association with conjugated hyperbilirubinemia in the first month of life? A. Hypothyroidism B. Sickle-cell disease C. Hemolytic disease of newborns D. Biliary atresia E. All is correct 219. Which of the following conditions have more than a chance association with conjugated hyperbilirubinemia in the first month of life? A. Fetal hepatitis 212. 220. 221. 222. 223. 224. 225. 226. 227. 228. B. Cytomegaloviral infection C. Biliary atresia D. Toxoplasmosis E. All is correct What is the possible indication for the lumbar puncture in neonates? A. Convulsive syndrome B. Neonatal meningitis C. Subarachnoid hemorrhage D. Hypertensive-hydrocephalic syndrome E. *All is correct The most frequent reason of neonatal phlegmona development is: A. *Infection B. Overcooling C. Compression D. congenital immunodeficiency E. All is correct For the neonatal phlegmona is typical: A. Erosive skin surfaces B. Hemorrhagic bullae C. *Intoxication syndrome D. Positive Nikolsky’s sign E. All is correct The typical symptom of the neonatal phlegmona is: A. Soft tissues infiltration B. Intoxication syndrome C. Deep scars on the skin D. "Creeping infiltration" E. *All is correct In the child with neonatal phlegmona on the skin usually appear: A. Phlyctena B. Vesicles C. Bullae D. All is correct E. *All is incorrect The typical symptom of the neonatal phlegmona is: A. Hypertermia B. Skin hyperemia C. Deep traumatic surface D. Soft tissues infiltration E. *All is correct What problems should be differentiated neonatal phlegmona with? A. Bullous epidermolysis B. Mongolian spot C. Cellulitis D. Allergic dermatitis E. *All is correct For the Ritters dermatitis are typical the next symptoms: A. Hyperthermia B. Skin erythema C. Presence of the bullas on the skin D. Positive Nikolsky's sign E. *All is correct The typical symptom of the SSS-syndrome is: A. B. C. D. E. 229. A. B. C. D. E. 230. A. B. C. D. E. 231. A. B. C. D. E. 232. A. B. C. D. E. 233. A. B. C. D. E. 234. A. B. C. D. E. Skin infiltration Palms hyperkeratosis Deep scars on the skin Bullae with bloody content *Positive Nikolsky’s sign For the Ritter’s dermatitis are typical: Tonic seizures Feet hyperkeratosis Hydrocephalus Ektropion *Erosive skin changes The most frequent etiological factor of the Ritter’s dermatitis is: Chlamydia trachomatis Group B streptococci Neisseria gonorrhoeae *Staphylococcus aureus Trichomonas vaginalis The SSS-syndrome should be differentiated with: Congenital syphilis Bullous epidermolysis Pemphygus neonatorum Allergic dermatitis *All is correct The most frequent etiological factor of the Ritter’s dermatitis is: Chlamydia trachomatis Group B streptococci Neisseria gonorrhoeae *Staphylococcus aureus Trichomonas vaginalis The acholic stool in neonate is typical for the: Physiological jaundice Haemolytic jaundice *Mechanical jaundice Parenchymatous jaundice All is incorrect The acholic stool in neonate is one of the typical symptoms for the: Physiological jaundice Haemolytic disease of newborns *Bile ducts atresia Fetal hepatitis All is correct Ситуаційні задачі. 1. A 2.1 kg full-term infant of drug addicted mother becomes irritable and develops coarse tremors at 36 h of age. He feeds poorly and has diarrhoea and nasal stuffiness. Which of the following statements is true? A. The most likely diagnosis is hypoglycemia B. The most appropriate treatment for this infant is 10% calcium gluconate C. The patient should be isolated D. * The mother should be tested for hepatitis B antigen and AIDS E. Child should be separated from mother and hospitalized to ICU 2. A 1 kg baby whose mother was given anesthesia just before delivery is presented to you in the 3. 4. 5. 6. 7. 8. delivery room for resuscitation. He is cyanosed, his heart rate is 40/min and he is limp and has apnea. Which of the following is appropriate? A. Intravenous atropine B. Intracardiac adrenalin C. Intravenous bolus of molar sodium bicarbonate D. Intravenous nalorphine should be the first procedure E. * External cardiac massage A newborn has an assymetrical Moro reflex. The grasp reflex is presented for the affected arm, which is weak. There is limitation in abduction and external rotation movements of the shoulder and supination of the forearm. The neurological lesion involves: A. Motor cortex on contralateral side B. 3-rd and 4-th cervical nerves C. * 5-th and 6-th cervical nerves D. 7-th and 8-th cervical nerves E. First and second thoracic nerves A full-term infant weighting 2.4 kg develops tachypnoea, grunting and intercostal recession. Full blood count shows haematocrit 75, WBC 25000/ml (62 % neutrophils, 30 % lymphocytes, 8 % monocytes). Which of the following statements is correct? A. Chest X-ray is likely to show a reticulogranulat (snow storm) appearance B. The white cell count supports a diagnosis of sepsis C. The infant is dehydrated D. The high haematocrit ha sno any relation to the respiratory distress E. * The infant is at risk of developing pulmonary hemorrhage An infant delivered at 32 weeks’ gestation develops respiratory distress soon after birth with marked chest recession. At the age of 4 hours he has a cyanotic episode. Chest X-ray shows ground-glass appearance with an air bronchogram. This presentation is the most consistent with the diagnosis of: A. * Hyaline membrane disease B. Meconium aspiration C. Wet lung D. Bacterial infection E. Tracheo-oesophageal fistula A baby of 40 weeks’ gestation is born weighing 2000g. Which of the following statements is likely to be true of this infant? A. He is premature B. * He is at risk of developing hypoglycemia C. His mother is a prediabetic D. He has an extremely low birth weight (ELBW) E. His head circumference is likely to be on a similar percentile to his weight A female infant, birth weight 1.2 kg, required intermittent positive pressure ventilation from birth. She needed 60-80 % oxygen for the first 5 days and subsequently required 40-50 % oxygen. She was extubated at the age of 1 month but remained oxygen-dependent for another 90 days. Which of the following statements apply to this infant? A. In the early stages of the disease parenteral dexamethasone has been shown to improve the espiratory status B. Histology of the bronchi would show mucosal hyperplasia and metaplasia C. The chest X-ray findings will demonstrate “air bronchogram” D. The infant is likely to require multiple hospital admission after discharge E. * All is correct A full-term infant weighing 3.5 kg has had respiratory distress from birth. His oxygen requirements ncreased progressively over the first 12 h and arterial blood gases show pH 7.26, P CO2 30 mm Hg, P O2 35 m Hg in 100 %. Echocardiogram shows no evidence of congenital heart disease other than a patent ductus rteriosus. Which of the following statements is correct? The most likely diagnosis is hyaline membrane disease * The patient should be hyperventilated The patient should be given indomethacin Treatment with extracorporeal membrane oxygenator (ECMO) isn’t effective Patient should be operated because of PDA as soon as possible A 25-years-old mother gave birth to twin boys at 38 weeks’ gestation. Twin A weighed 3200 g and win B weighed 2400 g at birth. Which of the following statements is correct? A. The weight of twin B is appropriate for gestational age and twin A is large for gestational age B. * The weight of twin A is appropriate for gestational age and twin B is small for gestational age C. Neither infant is appropriate weight for twins at 38 weeks’ gestation D. Both twins are large for twins at 38 weeks’ gestation E. Twin B needs parenteral feeding (TPN) because of his weight A newborn girl was born with body weight 3,400 g., length 50 cm. Pregnancy and birth were physiological. She cried immediately. She was breastfed in 2 hours after birth. In 1 and 2 days urination was 5-6 times per day, diaper has seeped in a small amount. On the 3rd day after urination on diaper remained yellow-red spot. What treatment is necessary in this case? A. diuretics B. hormons C. *does not require the treatment D. intravenous infusion E. antibiotics In the newborn with weight 3,500 g, assessment by Apgar score – 8 points, from mother with blood type B(III), rh (+), on the 2nd day of life has appeared jaundice of the skin. The general condition of the child is normal. Indirect bilirubin in the blood serum is 50 mkmol/l. What is the most possible diagnose? A. *transitory physiological jaundice B. hemolytic disease of newborn C. biliary atresia D. fetal hepatitis E. intrauterin infection In a newborn with weight 3,400 g., that was born with assessment by Apgar score – 9 points, were noted frequent defecation approximately 4-6 times per day, feces are liquid, yellow-green with admixture of mucus. General condition of the child is normal; the weight loss does not exceed physiological value. During microscopy of excrements was found mucus, leukocytes near 10 in a field, fat acids. Put the diagnosis. A. salmonellosis B. dysentery C. *physiological dyspepsia D. congenital infection E. alactasia In the newborn with weight 3,550 g with assessment by Apgar score – 9 points, on the 3rd day on anteriol surfaces of the limbs; buttocks, back has appeared hyperemia with gray-yellow papules in the centre. Papules have whitish content. The general condition of the child is normal. Put the diagnosis. A. erythema neonatorum B. atopic dermatitis C. chiken pox D. *erythema toxicum neonatorum E. rubella The newborn girl was born from physiological pregnancy and delivery with weight 3,200g, length 50cm, without signs of the asphyxia. On the 3rd day slight desquamation appeared on skin. The A. B. C. D. E. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. skin is dry, pink. What is necessary to do? A. wipe the skin with physiological saline solution B. wipe the skin with boiled oil C. wipe the skin with iodine solution D. wipe the skin with brilliant green E. *nothing The newborn girl was born from physiological pregnancy and delivery with weight 3,200g, length 50cm, without signs of the asphyxia. On the 3rd day hyperemia and peeling had appeared on skin. The skin is dry, pink. Put the diagnosis. A. the diaper rash B. erythema toxicum neonatorum C. vesiculopustullosis D. *erythema neonatorum E. ichthyosis The newborn boy was born from 1st physiological pregnancy, without complications, delivery was physiological, with weight 3,200 g, length 51 cm., estimation for Apgar score is 9 points. On the 3-rd day small peeling and hyperemia had appeared on skin. The skin is dry, pink. Put the diagnosis. A. pemphigus of the newborn B. ichthyosis C. *erythema neonatorum D. erythema toxicum neonatorum E. vesiculopustullosis Newborn girl was born with assesment by Apgar score - 9 points, weight 3,500 g. She was placed in a ward, the temperature in the ward was 27 ?С, and child’s bed was situated near the window, on the direct sun. On the 4th day the child became exited, thirst appeared, was noted dryness of the visible mucous membranes. The body temperature is 38 ?С. In internal organs pathology was not revealed. Defecation is normal. What diagnosis is the most possible? A. meningitis B. upper respiratory tract viral infection C. *transitory hyperthermia D. congenital infection E. cerebral hemorrhage In the newborn with weight 3,500 g, assesment by Apgar score – 8 points, from mother with blood type B (III), Rh (-), on the first day of life has appeared jaundice of the skin. Indirect bilirubin in the umbilical blood is 68 mkmol/l. What diagnosis is the most possible? A. congenital infection B. transitory physiological jaundice C. fetal hepatitis D. sepsis E. *hemolytic disease of the newborn In the newborn boy on the 3rd day of life has appeared edema around nipples. The skin color in this area is not changed. There’re whitish discharges from nipples. The body temperature is normal. The general condition of the child is satisfactory. It was diagnosed sexual (hormonal) crisis. What should physician do? A. put aseptic bandage on breasts with antibiotic B. wipe breasts with aniline dye-staffs C. put compress with spiritus aethilicus D. swab breasts by boiled oil E. *put warm sterile bandage on breasts In the newborn boy on the 3rd day of life has appeared edema around right nipple. The skin in this area is hyperemic. The babie’s body temperature is 38,5 (C). The child is restless, excited. What physicians’ actions are the most preferable? put warm sterile bandage on breasts prescribe antibiotic and infusions wipe breast with aniline dye *prescribe antibiotic and wipe breast with aniline dye prescribe antibiotic and apply on nipple compress with spiritus aethilicus The infant was born from the second in-term pregnancy, the second delivery in mother, who has blood type A (II) Rh(-). The blood type of the child is 0 (I) Rh(+). Total bilirubin level in u blood is 160 mkmol/l. In 3 hours total bilirubin level in his blood serum become 190 mkmol/l, had appeared jaundice. What is the probable diagnosis? A. hemolytic disease of the newborn, ABO-incompartibility, icteric type B. *hemolytic disease of the newborn, Rh-incompartibility, icteric type C. fetal hepatitis D. bile ducts atresia E. transitory physiological jaundice The child was born from the first delivery, in 39 weeks of gestation, with early rupture of amniotic fluid sac (waterless period 14 hours), birth weight - 3,500 g. The jaundice had appeared in 18 hours. Total serum bilirubin level was 120 mkmol/l. Perinatal complications were absent. What is the least posible diagnose? A. fetal hepatitis B. hemolytic disease of the newborn C. sepsis D. congenital hemolytic anemia E. *physiological jaundice In the newborn child on the 3rd day of life was revealed expressed jaundice with serum bilirubin level 456 mkmol/l. Mother's blood type is O (I) Rh-positive, child's blood type is A(II) Rhpositive. What complication is the most dangerous for this child? A. intrauterine infection B. hepatonecrosis C. sepsis D. *nuclear jaundice (kernicterus) E. DIC-syndrome The preterm child was transported to the hospital on the 10th day of life with expressed jaundice of the skin and mucous membranes. During examination: liver is enlarged, spleen is not palpable. In biochemical blood test: total serum bilirubin is 144,28 mcmol/l (indirect – 64,10, direct – 80,18 mkmol/l). The child's blood type is O (I) Rh-negative. What diagnosis the most probable? A. *Fetal hepatitis B. Hemolytic disease of the newborn C. Physiological jaundice D. Hypothyroidism E. Sepsis The child is 5 days old. Mother's blood type is A(II) Rh(+), child's blood type is B(III), Rhnegative. Skin jaundice appeared 2 days before. In biochemical blood test: total serum bilirubin is 120 mkmol/l, direct - 28 mcmol/l, indirect - 98 mcmol/l, protein - 68 g/l, AST - 0,28, ALT - 0,33. This is typical for: A. Hemolytic disease of the newborn B. *Transitory physiological jaundice C. Biliary atresia D. Fetal hepatitis E. Intrauterine infection After birth the newborn has heart rate 110 per minute, he is crying, has active movements, sneezing in answer to the clearing of airways, skin of body has pink color, extremities are blue. What will be 1-st minute Apgar score? A. 6 A. B. C. D. E. 21. 22. 23. 24. 25. 26. 7 8 *9 10 After birth the newborn has heart rate 90 per minute, he is crying, has active movements, sneezing in answer to the clearing of airways, skin of body has pink color, extremities are blue. What will be 1-st minute Apgar score? A. 6 B. 7 C. *8 D. 9 E. 10 After birth the newborn has heart rate 90 per minute, he has irregular breathing, has active movements, sneezing in answer to the clearing of airways, skin of body has pink color, extremities are blue. What will be 1-st minute Apgar score? A. 6 B. *7 C. 8 D. 9 E. 10 After birth the newborn has heart rate 26 per minute, he doesn’t breathe, doesn’t move, there is no answer to the clearing of airways, skin of body is pale. What will be 1-st minute Apgar score? A. *1 B. 2 C. 3 D. 4 E. 5 After birth the newborn has heart rate 110 per minute, he is crying, has weak movements, sneezing in answer to the clearing of airways, skin of body has pink color, extremities are blue. What will be 1-st minute Apgar score? A. 6 B. 7 C. *8 D. 9 E. 10 After birth the newborn has heart rate 126 per minute, he is crying, has active movements, sneezing in answer to the clearing of airways, skin of body has pink color. What will be 1-st minute Apgar score? A. 6 B. 7 C. 8 D. 9 E. *10 After birth the newborn has heart rate 85 per minute, he has irregular breathing, weak movements, grimace in answer to the clearing of airways, skin of body has pink color, extremities are blue. What will be 1-st minute Apgar score? A. *5 B. 6 C. 7 D. 8 E. 9 After birth the newborn has heart rate 80 per minute, he has irregular breathing, extremities are hanging down, grimace in answer to the clearing of airways, skin of body has blue color. What B. C. D. E. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. will be 1-st minute Apgar score? A. *4 B. 5 C. 6 D. 7 E. 8 After birth the newborn has heart rate 96 per minute, he is crying, has active movements, sneezing in answer to the clearing of airways, skin of body has pink color. What will be 1-st minute Apgar score? A. 6 B. 7 C. 8 D. *9 E. 10 After birth the newborn has heart rate 116 per minute, he is crying, has active movements, grimace in answer to the clearing of airways, skin of body has pink color, extremities are blue. What will be 1-st minute Apgar score? A. 6 B. 7 C. *8 D. 9 E. 10 After birth the newborn has heart rate 84 per minute, he is crying, muscle hypotonia, grimace in answer to the clearing of airways, skin of body has pink color, extremities are blue. What will be 1-st minute Apgar score? A. *6 B. 7 C. 8 D. 9 E. 10 The newborn with expressed acrocyanosis had cried immediately after birth. The muscular tone is reduced. During nosal catheter usuge he is crying. Cardiac rate is 128 in a minute. Estimate the child’s Apgar score. A. *8 points B. 7 points C. 9 points D. 6 points E. 5 points The Child was born from 1st pregnancy, 1st delivery. Pregnancy was on background of anemia II st., chronic fetoplacentary insufficiency. The delivery was in time. The birth weight is 3,200 g., estimation for Apgar score is 5/6 points. During objective examination - the child is hyperirritable, reflexes are decreased, muscular tone is increased in distal flexor muscles, perioral cyanosis, acrocyanosis, limbs' and chin's tremor are present. Heart rate is 158 per minute, breathing rate is 52 per minute. What is previous diagnosis? A. birth trauma B. *moderate asphyxia C. brain hemorrhage D. severe asphyxia E. congenital pneumonia The Child was born from 2nd pregnancy, 2nd delivery. Pregnancy was on background of the threat of interruption in 1st, and 2nd half, and anemia. The delivery - at 42 weeks of gestation with weakness of delivery activity; estimation for Apgar score is 3/5 points. Amniotic fluid is dirty, with meconial admixtures. What the physician have to do? tactile stimulation, oxygen therapy to blow mucus from nasopharynx, perform heart massage *intubation, sanation of trachea and bronchi oxygen therapy, indirect massage of the heart injection of epinephrin The child was born from 1st pregnancy, 1st delivery. The delivery was in time. The birth weight is 3,600 g. The estimation for Apgar score is 8/9 points. 2 hours after birth the child became sharply wilted, reflexes are suppressed, convulsive readiness is present. The skin is pale, moist, perspiration on the face. What investigation should be the first? A. neurosonography B. general blood test C. measure of the body temperature D. lumbar puncture E. *determination of sugar in the blood The child is 3 days old. He was born from 1st pregnancy, 1st delivery. Delivery is in 32 weeks of gestation, mother is 17 years old. During objective examination: the child is weak, has inadequate reaction on irritants, reflexes are suppressed, muscular tone is reduced. Cerebrospinal fluid: high pressure, yellowish, cytosis is 18 cells in 1 mkl, protein is 0.38 g/L, fresh erythrocytes 14-16 in field. What is the previous diagnosis? A. Meningitis B. Asphyxia C. Encephalitis D. *Intracranial hemorrhage E. Sepsis The child was born with cardiac rate 89 per minute; skin is pale, like wax. On nose catheter reaction is absent. The muscular tone is sharply reduced. Breathing rate is 14-16 in 1 minute, irregular. Estimate the child by Apgar scale: A. 2 points B. *3 points C. 1 points D. 4 points E. 5 points The Child was born from 3rd pregnancy, 3rd delivery. Pregnancy was on background of the threat of interruption, and preeclampsia. The delivery - at 36 weeks of gestation; estimation for Apgar score is 4/6 points. The weight is 2300. During objective examination: skin is cyanotic, reflectory excitability is weakened. The muscular tone is reduced. Heart rate is 156 in 1 minute. Thermoregulation is poor. Seizures are absent. What pathology has this child? A. congenital meningitis B. birth trauma C. *moderate asphyxia D. congenital pneumonia E. severe asphyxia A female infant born to a 24-year-old woman has been diagnosed clinically as having Down syndrome. The mother is concerned about her risk of having another child who has a chromosomal abnormality. The statement that you are MOST likely to include in your discussion is that her risk: A. can be estimated by determination of maternal serum alpha-fetoprotein in all future pregnancies B. *cannot be estimated until her infant's chromosome complement has been determined C. is increased for Down syndrome, but not for any other chromosomal abnormality D. is no greater than that of any other woman her age E. is not increased until she reaches the age of 35 During delivery of an infant who has an estimated gestational age of 42 weeks, you note that the A. B. C. D. E. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. amniotic fluid looks like pea soup and contains thick particles of meconium. Of the following, the MOST important initial step in resuscitation of the infant is to: A. aspirate the gastric contents B. determine the Apgar score C. *initiate tracheal intubation foor deep suction D. provide positive pressure ventilation E. warming of baby A newborn who weighs 600 g and whose estimated gestational age is 24 weeks at birth is admitted to the neonatal intensive care unit after successful resuscitation in the delivery room. Arterial blood gas measurements on room air are: pH, 7.35; PCO2, 42 mm Hg; PO2, 68 mm Hg; base deficit, 2 mEq/L. Of the following, the MOST appropriate initial management is to: A. begin intravenous vancomycin B. begin phototherapy C. initiate enteral feeding D. provide bicarbonate infusion E. *provide glucose infusion You are examining a term newborn in the nursery. His weight is 3.27 kg (50th percentile), and his length is 50.5 cm (50th percentile). The pregnancy, labor, and delivery were unremarkable. There are no significant findings on physical examination. The MOST likely head circumference in this child, if it is consistent with his other growth parameters, is A. 30 cm B. 32 cm C. *34 cm D. 36 cm E. 38cm You are examining a term newborn in the nursery. His weight is 3.27 kg (50th percentile), and his length is 50.5 cm (50th percentile). The pregnancy, labor, and delivery were unremarkable. There are no significant findings on physical examination. The MOST likely chest circumference in this child, if it is consistent with his other growth parameters, is A. 29 cm B. *33 cm C. 36 cm D. 38 cm E. 40 cm A newborn infant is delivered by emergent cesarean section at 41 weeks' gestation following a pregnancy complicated by a prolapsed umbilical cord and meconium-stained amniotic fluid. At 6 hours of age, the infant has a generalized tonic-clonic seizure. Of the following, the MOST likely explanation for this seizure is A. hyponatremia B. *hypoxic-ischemic encephalopathy C. intracranial hemorrhage D. meningitis E. pyridoxine dependency A newborn is delivered by emergent cesarean section because of fetal distress following acute abruption of the placenta. The infant is resuscitated and transferred to the nursery. On physical examination, she appears pale, and her extremities are cold to touch. Results of an arterial blood gas analysis show a PO2 of 48 mm Hg. Of the following, the MOST likely additional finding is A. *decreased bicarbonate concentration B. hypercalcemia C. hyperglycemia D. hyponatremia E. normal anion gap You are attending the emergency delivery by cesarean section of a primiparous woman. The 52. 53. 54. 55. 56. gestation was complicated by pregnancy-induced hypertension. Deep variable fetal heart rate decelerations were noted during labor. At delivery, the infant is acrocyanotic with poor tone; spontaneous movement and minimal respiratory effort are present. Of the following, your INITIAL management is to A. place the infant in an incubator B. begin tactile stimulation and provide blow-by oxygen supplementation C. *dry all skin surfaces and clear the oropharynx D. initiate bag-mask ventilation E. insert an umbilical catheter and administer naloxone A vigorous, normal-appearing term male newborn has not urinated by 18 hours after delivery. Perinatal history is negative for maternal illness or medications. Amniotic fluid volume was reportedly normal, and the delivery was uneventful, with Apgar scores of 6 and 9 at 1 and 5 minutes, respectively. Of the following, the MOST likely reason why this 18-hour-old infant has not urinated is: A. bilateral ureteropelvic junction obstruction B. intravascular volume depletion C. neurogenic bladder D. posterior urethral valve E. *undocumented urination in the delivery room A term infant is placed under a radiant warmer, the skin is dried, and the oropharynx and nose are suctioned. After tactile stimulation, there is minimal respiratory effort, dusky color, and a heart rate of 86 beats/min. Bag/mask ventilation is performed for 30 seconds with 100% oxygen at a rate of 40 to 60 breaths/min. The heart rate increases to 100 beats/min. Of the following, the NEXT best step is to: A. administer sodium bicarbonate B. continue bag/mask ventilation at a rate of 20 to 40 breaths/min C. continue ventilation and begin chest compressions D. *observes for spontaneous respiration and discontinues ventilation E. perform endotracheal intubation On the third day of life in the newborn appeared red blotchy rash, associated with whitish papules which look like pustules but without puss, contain eosinophiles. Rash is localized on the trunk, extremities, and the face. General well-being of the newborn is normal. The most probable diagnose is: A. local skin infection B. congenital syphilis C. allergic dermatitis D. congenital herpes E. *erythema toxicum neonatorum On the third day of life in the newborn appeared dark orange spots on the diapers after urination. General well-being of the newborn is normal. The most probable diagnose is: A. hemorrhagic disease of newborns B. urine tract infection C. renal malformation D. *uric acid infarct E. birth trauma In the newborn on the 3-th day of life appeared symmetrical breast engorgement, nipple discharge (white transparent fluid). General well-being of the newborn is normal. The most probable diagnose is: A. purulent mastitis B. diffuse mastopathy C. *hormonal crisis D. adreno-genital syndrome E. tumor of breasts 57. 58. 59. 60. 61. 62. 63. In the newborn girl on the 3-th day of life appeared mucous vaginal discharge during first 3 days of life. General well-being of the newborn is normal. The most probable diagnose is: A. purulent vaginitis B. urine tract infection C. *hormonal crisis D. adreno-genital syndrome E. clamidiosis A male infant is delivered after a pregnancy complicated by breech presentation. Physical examination reveals internally rotated shoulders, decreased muscle mass, extended elbows, contractures of the hands, flexion contractures at the knees, and bilateral equinovarus deformities. Of the following, the MOST likely outcome for this infant is A. *ambulation after initiation of early physical therapy and surgery B. death during the first year of life due to respiratory failure C. death in the first days of life due to renal disease D. progressive contractures and scoliosis E. severe psychomotor retardation and failure to attain motor milestones A newborn infant is delivered by emergent cesarean section at 41 weeks' gestation following a pregnancy complicated by a prolapsed umbilical cord and meconium-stained amniotic fluid. At 6 hours of age, the infant has a generalized tonic-clonic seizure. Of the following, the MOST likely explanation for this seizure is A. hyponatremia B. hypoxic-ischemic encephalopathy C. *intracranial hemorrhage D. meningitis E. pyridoxine dependency A 1-day-old infant who was born by a difficult forceps delivery is alert and active. She does not move her left arm, however, which she keeps internally rotated by her side with the forearm extended and pronated; she also does not move it during a Moro reflex. Grasp reflex is present in both arms. The rest of her physical examination is normal. This clinical picture most likely indicates A. Fracture of the left clavicle B. Fracture of the left humerus C. *Left-sided Erb-Duchenne paralysis D. Left-sided Klumpke paralysis E. Spinal injury with left hemiparesis Choose the most possible diagnosis for a 6-month-old comatose infant with multiple broken bones in various stages of healing, bulging anterior fontanelle, and retinal hemorrhages. A. Intraventricular hemorrhage B. Caput succedaneum C. *Subdural hemorrhage D. Subarachnoid hemorrhage E. Cephalohematoma Choose the most possible diagnosis for a previous premature infant born at 27 weeks’ gestation and now 6 months of age presenting with macrocephaly and hydrocephalus on ultrasonogram. A. *Intraventricular hemorrhage B. Caput succedaneum C. Subdural hemorrhage D. Subarachnoid hemorrhage E. Cephalohematoma The tonic-clonic seizures have appeared in the newborn age 1.5 day. Pregnancy was on background of the fetoplacentary insufficiency. The birth is in term. The body weight is 4,100 g. The estimation by Apgar score is 5/7 points. At the first day Hb - 156 g/l, RBC 4.0x10??/l. Of the following, the MOST likely explanation for this seizure is Hypoglycemia Hypoxic-ischemic encephalopathy Purulent meningitis *Intracranial hemorrhage Vitamin B6 deficit The term boy was born with estimation by Apgar score 3 points. In 6 hours after birth his condition became severe: generalized seizures, hyperexcitability, hyperesthesia, high-pitch cry. Cerebrospinal fluid is hemorrhagic, flows with high pressure. What is the previous diagnosis? A. Meningitis B. *Subarachnoid hemorrhage C. Intraventricular hemorrhage D. Hemorrhagic stroke E. Encephalitis In the newborn child was diagnosed hemolytic disease, Rh-factor incompatibility, icteric type. Till the end of the 1st day blood bilirubin level was 190 mkmol/l, because of indirect hyperbilirubinemia, level of the blood hemoglobin was 120 g/l, reticulocytes - 5%. What is your tactics? A. *Phototherapy B. Exchange blood transfusion C. Prescription of phenobarbital D. Sorbent agents E. Infusion therapy In the newborn girl on the 3rd hour of life serum blood bilirubin level is 180 mkmol/l. From anamnesis: she was born from 2nd pregnancy, with birth weight 3,300 g., length 54 cm. Mother has 0 (I) Rh(+) blood type; child has A (II) Rh(+) blood type. Bilirubin level in umbilical blood is 85 mkmol/l. Choose the treatment: A. Prescription of phenobarbital B. Observation C. *Exchange blood transfusion D. Infusion therapy E. Phototherapy Previously healthy 5-day-old male who was born at home develops bruising and melena. The pregnancy, delivery, and postnatal course were unremarkable. The infant is breastfeeding vigorously every 2 hours. Findings on physical examination are unremarkable except for several large bruises. Laboratory testing reveals: hemoglobin, 81 g/L; WBC 9.4 x 109/L; prothrombin time 37 seconds; partial thromboplastin time 98 seconds; platelet count 242 x 109/L; and fibrinogen 2.34 g/L. Of the following, the MOST likely cause of the bleeding is A. disseminated intravascular coagulation B. factor VIII deficiency hemophilia C. liver disease D. *vitamin K deficiency E. von Willebrand disease A 10-day-old infant who weighed 1,750 g at birth and whose gestational age was 34 weeks is jaundiced. His total serum bilirubin concentration is 10.0 mg/dL and the direct fraction is 0.8 mg/dL. He is receiving intermittent orogastric feeding of expressed human milk and supplemental parenteral nutrition. Of the following, the MOST likely explanation for these findings is A. Crigler-Najjar syndrome B. jaundice due to parenteral nutrition C. neonatal hepatitis D. *physiologic jaundice E. pyloric stenosis A newborn is noted to be quite jaundiced at 3 days of age. Which of the following factors is NOT associated with an increased risk of neurologic damage in a jaundiced newborn? A. B. C. D. E. 64. 65. 66. 67. 68. 69. Metabolic alkalosis Usage of drugs such as sulfisoxazole Hypoalbuminemia Neonatal sepsis *Maternal ingestion of phenobarbital during pregnancy A full-term infant is born after a normal pregnancy; delivery, however, is complicated by marginal placental separation. At 12 h of age, the child, although appearing to be in good health, passes a bloody meconium stool. For determining the cause of the bleeding, which of the following diagnostic procedures should be performed first? A. A barium enema B. *An Apt test C. Gastric lavage with normal saline D. An upper gastrointestinal series E. A platelet count, prothrombin time, and partial thromboplastin time A primiparous woman whose blood type is O positive gives birth at term to an infant who has Apositive blood and a hematocrit of 55%. A serum bilirubin level obtained at 36 h of age is 12 mg/dL. Which of the following laboratory findings would be characteristic of ABO hemolytic disease? A. A normal reticulocytes count B. *A positive direct Coombs test C. Crescent-shaped red blood cells in the blood smear D. Elevated haemoglobin E. Petechia You are speaking to a couple who are expecting their first baby in about 2 weeks. They are concerned about the safety of childhood immunizations and also about “unneeded” medications given to newborns in the hospital. They ask about the purpose of the routine administration of intramuscular vitamin K. You explain to them about hemorrhagic disease of the newborn, stating that the untreated baby can manifest: A. A deficiency of factor V B. *A prolonged prothrombin time and a risk of serious haemorrhage in the days following delivery C. Development of hemorrhagic manifestations within 24 h of delivery D. More severe symptoms in a male than a female child E. Hemorrhagic symptoms at a much higher rate if the infant is fed cow’s milk rather than breast milk You are called to the normal newborn nursery to see a baby who was noted to be mildly jaundiced and has a total serum bilirubin concentration of 12 mg/dL at 48 h of age. The baby is a 3500-g boy who was born at term to a 27-year-old O-positive, Coombs-test-negative primigravida 2 h after membranes ruptured. There were no prenatal complications, and the mother had regular prenatal care. Breast-feeding has been well tolerated, and the baby’s vitals have been normal. The most appropriate additional diagnostic studies to evaluate the cause of this infant’s jaundice are A. Direct serum bilirubin, complete blood count, liver ultrasound, liver transaminases B. Direct serum bilirubin, complete blood count, red blood cell glucose-6- phosphate dehydrogenase evels (G6PD), baby blood type C. *Complete blood count, direct serum bilirubin, baby’s blood type and Coombs test, peripheral smear D. Blood cultures, liver transaminases, red blood cell osmotic fragility, direct serum bilirubin E. Abdominal radiograph, urine bilirubin, complete blood count, direct serum bilirubin A woman gives birth to twins at 38 weeks’ gestation. The first twin weighs 2800 g and has a hematocrit of 70%; the second twin weighs 2100 g and has a hematocrit of 40%. Which of the following statements is correct? A. The second twin is at risk for developing respiratory distress, cyanosis, and congestive heart failure A. B. C. D. E. 70. 71. 72. 73. 74. 75. 76. 77. 78. 79. 80. B. *The first twin is more likely to have hyperbilirubinemia and convulsions C. The second twin is at risk for renal vein thrombosis D. The second twin probably has hydramnios of the amniotic sac E. The second twin is likely to be pale, tachycardic, and hypotensive In the newborn child was diagnosed hemolytic disease, ABO incompatibility, icteric type. In four hours after phototherapy initialization bilirubin level became 173 mkmol/l (before it was 190 mkmol/l), because of indirect hyperbilirubinemia, level of the blood hemoglobin 135 g/l. What is your tactics? A. *Phototherapy continuation B. Exchange blood transfusion C. Prescription of phenobarbital D. Sorbent agents E. Infusion therapy Parents bring a 5-day-old infant to your office. The mother is O negative and was Coombs positive at delivery. The term child weighed 3055 g at birth had haemoglobin 160 g/L and a total serum bilirubin 3 mg/dL. He passed a black tar-like stool within the first 24 h of life. He was discharged at 30 h of life with a stable axillary temperature of 36.5°C . Today the infant’s weight is 3000 g, his axillary temperature is 35°C, and he is jaundiced to the chest. Parents report frequent yellow, seedy stool. You redraw labs and find his haemoglobin is now 140 g/L, and his total serum bilirubin is 13 mg/dL. The change in which of the following parameters is of most concern? A. Haemoglobin B. *Temperature C. Body weight D. Bilirubin E. Stool In the newborn girl on the 1st hour of life serum blood bilirubin level is 210 mkmol/l. From anamnesis: she was born from 2nd pregnancy, with birth weight 3,300 g., length 54 cm. Mother has 0 (I) Rh(-) blood type; child has A (II) Rh(+) blood type. Total bilirubin level in umbilical blood is 90 mkmol/l. What is your tactics? A. Prescription of phenobarbital B. Observation C. *Exchange blood transfusion D. Infusion therapy E. Phototherapy In the newborn girl on the 2nd hour of life serum blood bilirubin level is 160 mkmol/l. From anamnesis: she was born from 2nd pregnancy, with birth weight 3,300 g., length 54 cm. Mother has 0 (I) Rh(+) blood type; child has A (II) Rh(+) blood type. Total bilirubin level in umbilical blood is 60 mkmol/l. What is your tactics? A. Prescription of phenobarbital B. Observation C. Exchange blood transfusion D. Infusion therapy E. *Phototherapy In the newborn girl on the 3rd hour of life serum blood bilirubin level is 80 mkmol/l. From anamnesis: she was born from 2nd pregnancy, with birth weight 3,300 g., length 54 cm. Mother has AB (IV) Rh(-) blood type; child has A (II) Rh(-) blood type. Indirect bilirubin level in umbilical blood is 25 mkmol/l. What is your tactics? A. Prescription of phenobarbital B. *Observation C. Exchange blood transfusion D. Infusion therapy E. Phototherapy In the newborn girl on the 14th hour of life appeared jaundice, serum blood bilirubin level is 110 81. 82. 83. 84. 85. 86. mkmol/l. From anamnesis: she was born from 2nd pregnancy, with birth weight 3,300 g., length 54 cm. Mother has AB (IV) Rh(+) blood type; child has A (II) Rh(+) blood type. What is your tactics? A. Prescription of phenobarbital B. Observation C. Exchange blood transfusion D. Infusion therapy E. *Phototherapy In the newborn boy on the 7th hour of life appeared jaundice, serum blood bilirubin level is 170 mkmol/l. From anamnesis: he was born from 3nd pregnancy, with birth weight 3,200 g., length 52 cm. Mother has B (III) Rh(+) blood type; child has A (II) Rh(+) blood type. In four hours after phototherapy initialization bilirubin level became 193 mkmol/l. What is your tactics? A. Prescription of phenobarbital B. Observation C. *Exchange blood transfusion D. Infusion therapy E. Phototherapy The boy was born in term. The anticoagulants of the indirect action were used in the last trimester of pregnancy to mother because of thromboflebitis. On the third day of the life in the child has appeared umbilical bleeding, multiple hemorrhages in skin and subcutaneous tissues, vomiting with blood, melena. Apt’s test is negative. What diagnosis is the most reliable? A. Hemophilia B. Syndrome of maternal blood swallowing C. *Hemorrhagic disease of the newborn D. Idiopathic thrombocytopenic purpura E. DIC-syndrome The boy was born from 2nd in term pregnancy, with weight 3,300 g., Apgar score 7/8 points. On the 2nd day of life have appeared the nasal bleeding, plural haemorrhages in skin and subcutaneous tissues. What is the treatment of the first choice? A. Prednisolon B. Aminocapronic acid C. Albumin D. *Vitamin K E. Fresh frozen plasma A male infant is born at an estimated gestational age of 34 weeks. His measurements at birth are: weight, 1,200 g (<10th percentile); crown-heel length, 40 cm (10th percentile); and head circumference, 31.5 cm (50th percentile). Of the following, the MOST likely explanation for the growth pattern of this infant is: A. chromosomal abnormality B. congenital viral infection C. gestational diabetes D. hereditary constitution E. *intrauterine growth restriction A newborn whose estimated gestational age is 42 weeks is stained with meconium. Tracheal intubation reveals meconium in the hypopharynx as well as below the vocal cords. The infant has respiratory distress. A chest radiograph is obtained. Of the following, the MOST likely radiographic finding is: A. *homogenous "ground glass" opacity B. decreased lung volumes C. mediastinal shift D. pleural effusion E. reticulogranular pattern An 18-year-old primigravida at 32 weeks' gestation has a blood pressure of 148/96 mm Hg, 87. 88. 89. 90. 91. 92. proteinuria, oliguria, and visual disturbances. Labor is induced, and the infant is delivered. His weight is 850 g (<10th percentile), crown-heel length is 38 cm (10th percentile), and head circumference is 30 cm (50th percentile). Of the following, the MOST likely complication in this infant is A. anemia of prematurity B. *hyaline membrane disease C. hyperglycemia D. meconium aspiration E. congenital infection An infant is born at 27 weeks' gestation following a pregnancy complicated by preterm labor that progressed despite administration of a tocolytic agent. Of the following, the most appropriate INITIAL management is to: A. measure transcutaneous oxygen saturation B. perform endotracheal intubation C. place an umbilical arterial catheter D. *place the infant in an incubator E. provide nasal continuous positive airway pressure A 10-day-old infant who weighed 1,750 g at birth and whose gestational age was 34 weeks is jaundiced. His total serum bilirubin concentration is 10.0 mg/dL and the direct fraction is 0.8 mg/dL. He is receiving intermittent orogastric feeding of expressed human milk and supplemental parenteral nutrition. Of the following, the MOST likely explanation for these findings is: A. Crigler-Najjar syndrome B. jaundice due to parenteral nutrition C. neonatal hepatitis D. *physiologic jaundice E. pyloric stenosis A full-term newborn infant is having episodes of cyanosis and apnea, which are worse when he is attempting to feed, but he seems better when he is crying. The most important next step to quickly establish the diagnosis is: A. Echocardiogram B. Ventilation perfusion scan C. *Passage of catheter into nose D. Hemoglobin electrophoresis E. Bronchoscopic evaluation of palate and larynx A 2-week-old infant has had no immunizations, sleeps 18 h a day, weighs 3.5 kg, and takes 60 mL of standard infant formula four times a day, but no solid food and no iron or vitamin supplements. Of most concern is A. Immunization status B. *Caloric intake C. Iron levels D. Levels of vitamins A, C, and D E. Circadian rhythm A mother delivers a term neonate with meconium staining and Apgar scores of 3 at 1 and 5 min of life. She had no prenatal care and the delivery was by emergency cesarean section for severe fetal bradycardia. Which of the following sequelae could be expected to develop in this intubated neonate with respiratory distress? A. *Congenital pneumonia B. Hyaline membrane disease C. Microcephaly with micrognathia D. Cataracts E. Leukocytosis As you are about to step out of a newly delivered mother’s room, she mentions that she wants to breast-feed her healthy infant, but that her obstetrician was concerned about one of the medicines 93. 94. she was taking. Which of the woman’s medicines, listed below, is clearly contraindicated in breast-feeding? A. Ibuprofen as needed for pain or fever B. Labetolol for her chronic hypertension C. *Lithium for her bipolar disorder D. Carbamazepine for her seizure disorder E. Acyclovir for her HSV outbreak The nurse from the level II neonatal intensive care nursery calls you to evaluate a baby. The infant, born at 32 weeks’ gestation, is now 1 week old and had been doing well on increasing nasogastric feedings. This afternoon, however, the nurse noted that the infant has vomitted the last two feedings and seems less active. Your examination reveals a tense and distended abdomen with decreased bowel sounds. As you are evaluating the child, he has a grossly bloody stool. Your management of this infant should include A. Surgical consultation for an emergent exploratory laparotomy B. Continued feeding of the infant, as gastroenteritis is usually self-limited C. Stool culture to identify the etiology of the bloody diarrhea and an infectious diseases consultation D. *Stopping feeds, beginning intravenous fluids, ordering serial abdominal films, and initiating systemic ntibiotics E. Upper GI series and barium enema to evaluate for obstruction An infant weighing 1400 g is born at 32 weeks’ gestation in a delivery room that has an ambient emperature of 24 C. If left in an open crib for a few minutes, this child is likely to demonstrate A. Skin hyperemia B. Shivering C. Hypertension D. *Increased respiratory rate Metabolic alkalosis A 3-day-old infant born at 32 weeks’ gestation and weighing 1700 g has three episodes of apnea, ach lasting 20 to 25 s and occurring after a feeding. During these episodes, the heart rate drops from 140 to 10 beats per min, and the child remains motionless; between episodes, however, the child displays normal ctivity. Blood sugar is 5 mmol/L and serum calcium is normal. The child’s apneic periods most likely are A. *Due to an immature respiratory center B. A part of periodic breathing C. Secondary to hypoglycemia D. Manifestations of seizures E. Evidence of underlying pulmonary disease An infant who appears to be of normal size is noted to be lethargic and somewhat limp after birth. The mother is 28 years old, and this is her fourth delivery. The pregnancy was uncomplicated, with normal fetal monitoring prior to delivery. Labor was rapid, with local anesthesia and intravenous meperidine administered for maternal pain control. Which of the following therapeutic maneuvers is likely to improve this infant’s condition most rapidly? A. Intravenous infusion of 10% dextrose in water B. *Administration of naloxone (Narcan) C. Administration of vitamin K D. Measurement of electrolytes and magnesium levels E. Neurologic consult At 43 weeks’ gestation, a long, thin infant is delivered. The infant is apneic, limp, pale, and covered with “pea soup” amniotic fluid. The first step in the resuscitation of this infant at delivery should be A. *Suction of the trachea under direct vision B. Artificial ventilation with bag and mask E. 95. 96. 97. Artificial ventilation with endotracheal tube Administration of 100% oxygen by mask Catheterization of the umbilical vein After an uneventful labor and delivery, an infant is born at 32 weeks’ gestation weighing 1500 g. Respiratory difficulty develops immediately after birth and increases in intensity thereafter. At 6 h of age, the child’s respiratory rate is 60 breaths per min. Examination reveals grunting, intercostal retraction, nasal flaring, and marked cyanosis in room air. Physiologic abnormalities compatible with these data include A. Decreased lung compliance, reduced lung volume, left-to-right shunt of blood B. *Decreased lung compliance, reduced lung volume, right-to-left shunt of blood C. Decreased lung compliance, increased lung volume, left-to-right shunt of blood D. Normal lung compliance, reduced lung volume, left-to-right shunt of blood E. Normal lung compliance, increased lung volume, right-to-left shunt of blood An infant born at 35 weeks’ gestation to a mother with no prenatal care is noted to be jittery and irritable, and is having difficulty feeding. You note coarse tremors on examination. The nurses report a high-pitched cry and note several episodes of diarrhea and emesis. You suspect the infant is withdrawing from A. Alcohol B. Antibiotics C. *Heroin D. Glucocorticoids E. Tobacco A term, 4200-g female infant is delivered via cesarean section because of cephalopelvic disproportion. The amniotic fluid was clear, and the infant cried almost immediately after birth. Within the first 15 min of life, however, the infant’s respiratory rate increased to 80 breaths per min, and she began to have intermittent grunting respirations. The infant was transferred to the level 2 nursery and was noted to have an oxygen saturation of 94%. The chest radiograph showed fluid in the fissure, overaeration, and prominent pulmonary vascular markings. The most likely diagnosis in this infant is A. Diaphragmatic hernia B. Meconium aspiration C. Pneumonia D. Idiopathic respiratory distress syndrome E. *Transient tachypnea of the newborn A 1-month-old infant presents to the clinic in the month of December with a several-day history of cough and rhinorrhea, and has now developed difficulty breathing. On examination, the child has marked intercostal and subcostal retractions. There are both crackles and wheezes diffusely on auscultation, and the infant is mildly hypoxic. The child’s radiograph displays a diffuse interstitial infiltrate with some air trapping. The child has been placed on oxygen. A rapid RSV antigen test is positive. What is the next step in initial management? A. *Nebulized epinephrine B. Nebulized steroids C. Systemic steroids D. Chest physiotherapy E. Emergent intubation An infant born an hour ago to a mother with severe pregnancyinduced hypertension was floppy at birth and required bag-mask ventilation for several minutes. The infant is now in distress and seemingly agitated, with tachypnea, tachycardia, and hypoxia. Perfusion is poor. Diminished breath sounds are noted on the left side of her chest, and her heart sounds are displaced to the right. What is the best initial step in management? A. *Needle aspiration of the chest B. Nebulized epinephrine C. Chest physiotherapy C. D. E. 98. 99. 100. 101. 102. Emergent intubation Chest radiograph, two views A term infant delivered via scheduled cesarean section develops, at 15 min of age, tachypnea, grunting, flaring, and retractions. A chest radiograph reveals well-aerated lungs with fluid in the fissure on the right, prominent pulmonary vascular markings, and flat diaphragms. The child is mildly hypoxic on room air with 89% oxygen saturation. Over the next 6 h she improves and no longer requires oxygen. What is the diagnosis? A. Respiratory distress syndrome (hyaline membrane disease) B. Pneumothorax C. Asthma D. *Transient tachypnea of the newborn E. Bacterial pneumonia A postterm infant is born at home after a prolonged and difficult labor. The maternal grandmother brings the infant to the hospital at 1 h of life because of fast breathing. Grandmother notes that the child spit up some dark brown particulate fluid shortly after birth. Physical examination reveals an infant in marked respiratory distress. Other findings include both an umbilical cord and flaking skin with a yellow-green hue. Chest radiograph reveals patchy infiltrates bilaterally. What is the diagnosis? A. Respiratory distress syndrome (hyaline membrane disease) B. Bronchiolitis C. Pneumothorax D. *Meconium aspiration E. Transient tachypnea of the newborn The premature infant who suffered from hyaline membrane disease is now 7 weeks old. She has been extubated for 2 weeks and still requires oxygen to maintain her saturation above 93%. Her chest radiograph now reveals patchy, fluffy infiltrates with areas of lucency. She requires daily diuretic treatment. What is the diagnosis? A. Asthma B. *Bronchopulmonary dysplasia C. Pneumothorax D. Bronchiolitis E. Bacterial pneumonia A 2-day-old infant with meconium aspiration syndrome is worsening. The delivered FiO2 is 100%, and yet his arterial PaO2 is 40 mmHg on the most recent arterial blood-gas analysis. You have increased his ventilator pressures without success. What is the next step in this patient’s management? A. Needle aspiration of the chest B. *Extracorporeal membrane oxygenation C. Nebulized epinephrine D. Chest physiotherapy E. Systemic steroids A 3-week-old infant has a 1-week history of a mild cough with thick nasal secretions. In the last 12 h she has developed spasmotic coughing fits during which she becomes cyanotic. When not coughing, she appears tired. She has lost weight since the 2-week visit. The family has not taken her temperature, but she has been feeding less and has not voided in about 16 h. You decide to admit her for observation and rehydration. What is the most appropriate first management consideration for this patient? A. Nebulized epinephrine B. Systemic steroids C. Chest physiotherapy D. Emergent intubation E. *Respiratory isolation (droplet precautions) A 7-day-old infant has copious purulent discharge from both eyes. The 17-year-old mother D. E. 103. 104. 105. 106. 107. 108. 109. 110. 111. 112. 113. 114. currently complains of a yellowish vaginal discharge. The only medications received by the infant were vitamin K and topical erythromycin prophylaxis following delivery. After obtaining appropriate diagnostic studies, the BEST management includes treatment with: A. *oral erythromycin B. oral penicillin C. topical erythromycin D. topical gentamicin E. topical sulfonamide A 1-week-old black infant presents to you for the first time with a large, fairly well-defined, purple lesion over the buttocks bilaterally, as shown in the photograph. The lesion is not palpable, and it is not warm or tender. The mother denies trauma and reports that the lesion has been present since birth. This otherwise well-appearing infant is growing and developing normally and appears normal upon physical examination. The most likely diagnosis in this infant is: A. Child abuse B. *Mongolian spot C. Subcutaneous fat necrosis D. Vitamin K deficiency E. Hemophilia A 3-weeks-old white infant presents to you for the first time with a pustules on the face with seropurulent discharge that dries to form thick golden-yellow crust, as shown in the photograph . This otherwise well-appearing infant is growing and developing normally and appears normal upon physical examination. The most likely diagnosis in this infant is: A. Moniliasis B. Vesiculopustulosis C. Subcutaneous fat necrosis D. *Impetigo E. Ritter's disease The 26-days old boy has delayed healing of umbilical wound, granulations 1-3 cm in diameter under the crust on umbilical region (look on the picture); the baby is active, he demonstrates good appetite. The most likely diagnosis is: A. *Phungus B. Catarrhal omphalitis C. Purulent omphalitis D. Omphalocele E. Healthy baby A mother delivers a term neonate with meconium staining and Apgar scores of 3 at 1 and 5 min of life. She had no prenatal care and the delivery was by emergency cesarean section for severe fetal bradycardia. Which of the following sequelae could be expected to develop in this intubated neonate with respiratory distress? A. *Congenital pneumonia B. Hyaline membrane disease C. Meningitis D. BPD E. Cataracts In the 3 days old newborn boy, who demonstrated hyperirritability, poor feeding, regurgitation and subfebrile temperature, was revealed patchy, asymmetric pulmonary opacities and hyperaeration on the chest photograph. What is the most possible diagnosis? A. Respiratory distress syndrome (HMD) B. *Congenital pneumonia C. Acquired pneumonia D. Bronchopulmonary dysplasia (BPD) E. Bronchial asthma A 2-year-old boy is being followed for congenital cytomegalovirus (CMV) infection. He is deaf 115. 116. 117. 118. 119. 120. and developmentally delayed. The child’s mother informs you that she has just become pregnant and is concerned that the new baby will be infected. Which of the following is true? A. *The mother has antibodies to CMV that are passed to the fetus B. The mother’s infection cannot become reactivated C. The likelihood that the new baby will become clinically ill is approximately 80% D. Termination of pregnancy is advised E. The new infant should be isolated from the older child A term infant is born to a known HIV-positive mother. She has been taking antiretroviral medications for the weeks prior to the delivery of her infant. Routine management of the healthy infant should include A. Admission to the neonatal intensive care unit for close cardiovascular monitoring B. HIV ELISA on the infant to determine if congenital infection has occurred C. *A course of zidovudine for the infant D. Chest radiographs to evaluate for congenital Pneumocystis carinii E. Administration of IVIG to the baby to decrease the risk of perinatal HIV infection You are advised by the obstetrician that the mother of a baby he has delivered is a carrier of hepatitis B surface antigen (HBsAg-positive). The most appropriate action in managing this infant would be to A. Screen the infant for HBsAg B. Isolate the infant for enteric transmission C. Screen the mother for hepatitis B “e” antigen (HBeAg) D. *Administer hepatitis B immune globulin and hepatitis B vaccine to the infant E. Do nothing because transplacentally acquired antibody will prevent infection in the infant The 5 days old infant is presented with hepatosplenomegaly, anemia, persistent rhinitis, and a maculopapular rash. The most likely diagnosis for this child is A. Toxoplasmosis B. Glycogen storage disease C. Congenital hypothyroidism D. *Congenital syphilis E. Cytomegalovirus disease The girl was born in term, with body weight 1,800g with signs of patient ductus arteriosus, hepatomegaly, and glaucoma. Later was revealed deafness, mental retardation. What is the most probable diagnosis? A. Toxoplasmosis B. Syphilis C. *Rubella D. Chlamydiosis E. Lysteriosis . General condition of the baby is normal. What is the most possible etiologic agent? A. Staphylococcus B. Escherichia coli C. Herpes virus D. Chlamydia E. *Streptococcus The child was born from the 1st premature delivery. The gestational age is 30 weeks. The birth weight is 1100 g. In 4 hours after birth respiratory distress syndrome has appeared. The Apgar score is 7/8 points. There is heavy breathing through the nose, body temperature is 37,8 0C, baby is restless, he has poor appetite. What instrumental examination should be performed the first? A. Spinal puncture B. CT-scan of head C. *X-ray of chest D. MRI of head E. Echoencephalography 121. 122. 123. 124. 125. 126. The child is 4 days old. Mother was not observed during pregnancy. Delivery is in term. The birth weight is 2200 g. During examination: skin is pale-gray; on palms and soles - multiple bullae size 2-5 cm, with serous-hemorrhagic contents. The nasal breathing is poor. The child is anxious, has chin tremor, convulsive readiness. The liver is thick; its margin is on the umbilical level. Put previous diagnosis. A. *Syphilis B. Rubella C. Toxoplasmosis D. Lysteriosis E. Chlamydiosis The child is from 3rd pregnancy, 1st delivery. Previous pregnancies finished with intrauterine fetal death. The child’s weight at birth was 2900 g. The head circumference is 38 cm, chest - 33 cm. On the 2nd day body temperature has increased, tonic-clonic seizures, jaundice, turbidity of the cornea and head enlargement have appeared. What pathology is possible in this child? A. Rubella B. Herpetic infection C. *Toxoplasmosis D. Lysteriosis E. Syphilis The 10 days old child is hospitalized with complains of the decreased appetite, periodic regurgitation, meteorism, liquid feces after each feeding, malaise, seizures. Body temperature is 37 0C. During examination: skin is yellowish, subcutaneous tissue is thin on abdomen, limbs; the liver margin is near umbilical level. Ophthalmologist diagnosed cataract. Put previous diagnosis. A. *Galactosemia B. Cytomegalovirus C. Toxoplasmosis D. Hemolytic disease of the newborn E. Necrotizing enterocolitis The newborn child aged 5 days was hospitalized with diagnosis: Generalized form of infection: pneumonia, meningitis, enterocolitis, kidneys damage. During bacteriological investigation of blood, cerebro-spinal fluid, feces were revealed streptococcus group B. Neonatal sepsis was diagnosed. What antibacterial therapy is the most recommended in this case? A. *Ampicillin + Gentamycin B. Cefazolin + penicillin C. Keflex + Gentamycin D. Tienam + spiramycin E. Laevomycetin + Oxacillin The newborn child is 7 days old. He was born from 1st pregnancy, 1st delivery. Delivery was in term. Birth weight is 3500 g. In objective examination: skin is pink, vesicular elements 0.5 – 1,0 cm in diameter, with serous contents in cervical folds, on shoulders. General condition of child is normal. What is the previous diagnosis? A. Syphilis B. *Vesiculopustullosis C. Rubella D. Lysteriosis E. Pemphigus A newborn infant becomes markedly jaundiced on the second day of life, and a faint petechial eruption first noted at birth is now a generalized purpuric rash. Hematologic studies for hemolytic diseases are negative. Acute management should include which of the following steps? A. Liver ultrasound B. *Isolation of the infant from pregnant hospital personnel C. Urine drug screen on the infant D. Discharge with an early follow-up visit in 2 days to recheck bilirubin Thyroid hormone assay The child was born from 2nd pregnancy at 37 weeks of gestation. Previous child in this family has hydrocefalus. This pregnancy was on background of polyhydramnion. The birth weight is 2800 g. Objectively: significant hepatosplenomegaly, jaundice, enlargement of the head. In the head CT scan was revealed calcification. What is previous diagnosis? A. Rubella B. Syphilis C. Cytomegalovirus D. *Toxoplasmosis E. Lysteriosis In the newborn whose gestational age is 37 weeks with weight 3200 g with assessment by Aggar score – 7/8 points, on the second day has appeared dyspnea, intercastal muscles retractions, acrocyanosis. In auscultation was weak breathing and in percussion was ban box sound above both lungs surface. What is the most possible diagnosis? A. Respiratory distress syndrome (HMD) B. *Congenital pneumonia C. Acquired pneumonia D. Bronchopulmonary dysplasia (BPD) E. Bronchial asthma In the 15 days old boy appeared fluid-filled blisters on the trunk, legs and buttocks. The skin around the blisters is red and itchy but not sore. The blisters are large and small, breaks and scab over with a yellow-colored crust. What is the possible diagnosis? A. Vesiculopustulosis B. Pemphigus C. *Bullous impetigo D. Flegmona E. Moniliasis Girl was born from the first pregnancy. Her birth weight is 2900 g. Head circumference 62 cm. She has hepatospleenomegaly, muscle hypertonia, jaundice. What of the following symptoms is the most typical for the congenital toxoplasmosis? A. Small birth weight B. *Hydrocefalus C. Jaundice D. Muscle hypertonus E. Hepatospleenomegaly The child has eczema on the face and trunk which appeared immediately after birth. His mother has cold sore on lip. What is the most probable diagnose? A. Rubella B. Staphylococcal infection C. *Herpes D. Pemphigus E. Allergic dermatitis A newborn was born from 2nd pregnancy, 2nd delivery at 38 weeks of gestation. The Apgar score is 7/8; body weight is 3,100, length – 51 cm, head circumference 34 cm, chest circumference – 33 cm. Large fontanel is 2x2cm, sutures are closed. After delivery a macular, copper-colored rash on the palms and soles and papular lesions around the nose and mouth and in the diaper area appeared. There is generalized lymphadenopathy and hepatosplenomegaly. There are mucopurulent nasal discharges. In age of 2 days were registered seizures. What’s the most reliable diagnose? A. Listeriosis B. Toxoplasmosis C. Cytomegalovirus infection D. *Congenital syphilis E. 127. 128. 129. 130. 131. 132. Congenital rubella A newborn was born from 1st pregnancy, 1st delivery at 39 weeks of gestation. The Apgar score is 7/8; body weight is 3,200, length – 52 cm, head circumference 31 cm, chest circumference – 33 cm. Large fontanel is 2x3cm, sutures are closed. After delivery vesicles against a hyperaemic background on the baby’s trunk have appeared. There is generalized lymphadenopathy and hepatosplenomegaly. During ophthalmic examination chorioretinitis was found. What’s the most reliable diagnose? A. *Herpes B. Toxoplasmosis C. Cytomegalovirus infection D. Congenital syphilis E. Congenital rubella On the third day of life in the newborn appeared red blotchy rash, associated with whitish papules which look like pustules but without puss, contain eosinophiles. Rash is localized on the trunk, extremities, and the face. General well-being of the newborn is normal. The most probable diagnose is: A. local skin infection B. congenital syphilis C. allergic dermatitis D. congenital herpes E. *erythema toxicum neonatorum A newborn was born from 3rd pregnancy, 1st delivery at 37 weeks of gestation. Previous pregnancies finished with miscarriage. During this pregnancy in first trimester mother had lymphadenopathy of unknown genesis. Body weight is 2900 g, length – 49 cm, head circumference 32 cm, chest circumference – 34 cm. Large fontanel is 2x2 cm, sutures closed. There are seizures, tremor of the extremities. Muscular tonus is increased. On the 2nd day after birth jaundice has appeared. There is hepatosplenomegaly. On the baby’s skin there are disseminated petechiae. Urine test: specific gravity 1.009, leukocytes 4-5/field, erhytrocytes 45/field, were revealed unusual big cells, high amount of uric acid salts. What’s the most reliable diagnose? A. Listeriosis B. Toxoplasmosis C. *Cytomegalovirus infection D. Congenital syphilis E. Congenital rubella A 2.1 kg full-term infant of drug addicted mother becomes irritable and develops coarse tremors at 36 h of age. He feeds poorly and has diarrhoea and nasal stuffiness. Which of the following statements is true? A. The most likely diagnosis is hypoglycemia B. The most appropriate treatment for this infant is 10% calcium gluconate C. The patient should be isolated The mother should be tested for hepatitis B antigen and AIDS D. E. Child should be separated from mother and hospitalized to ICU A 1 kg baby whose mother was given anesthesia just before delivery is presented to you in the delivery room for resuscitation. He is cyanosed, his heart rate is 40/min and he is limp and has apnea. Which of the following is appropriate? A. Intravenous atropine B. Intracardiac adrenalin C. Intravenous bolus of molar sodium bicarbonate D. Intravenous nalorphine should be the first procedure External cardiac massage E. E. 133. 134. 135. 136. 137. 138. 139. 140. 141. 142. 143. A newborn has an assymetrical Moro reflex. The grasp reflex is presented for the affected arm, which is weak. There is limitation in abduction and external rotation movements of the shoulder and supination of the forearm. The neurological lesion involves: A. Motor cortex on contralateral side B. 3-rd and 4-th cervical nerves 5-th and 6-th cervical nerves C. D. 7-th and 8-th cervical nerves E. First and second thoracic nerves A full-term infant weighting 2.4 kg develops tachypnoea, grunting and intercostal recession. Full blood count shows haematocrit 75, WBC 25000/ml (62 % neutrophils, 30 % lymphocytes, 8 % monocytes). Which of the following statements is correct? A. Chest X-ray is likely to show a reticulogranulat (snow storm) appearance B. The white cell count supports a diagnosis of sepsis C. The infant is dehydrated D. The high haematocrit ha sno any relation to the respiratory distress The infant is at risk of developing pulmonary hemorrhage E. An infant delivered at 32 weeks’ gestation develops respiratory distress soon after birth with marked chest recession. At the age of 4 hours he has a cyanotic episode. Chest X-ray shows ground-glass appearance with an air bronchogram. This presentation is the most consistent with the diagnosis of: Hyaline membrane disease A. B. Meconium aspiration C. Wet lung D. Bacterial infection E. Tracheo-oesophageal fistula A female infant, birth weight 1.2 kg, required intermittent positive pressure ventilation from birth. She needed 60-80 % oxygen for the first 5 days and subsequently required 40-50 % oxygen. She was extubated at the age of 1 month but remained oxygen-dependent for another 90 days. Which of the following statements apply to this infant? A. In the early stages of the disease parenteral dexamethasone has been shown to improve the respiratory status B. Histology of the bronchi would show mucosal hyperplasia and metaplasia C. The chest X-ray findings will demonstrate “air bronchogram” D. The infant is likely to require multiple hospital admission after discharge All is correct E. A full-term infant weighing 3.5 kg has had respiratory distress from birth. His oxygen requirements increased progressively over the first 12 h and arterial blood gases show pH 7.26, P CO2 30 mm Hg, P O2 35 mm Hg in 100 %. Echocardiogram shows no evidence of congenital heart disease other than a patent ductus arteriosus. Which of the following statements is correct? A. The most likely diagnosis is hyaline membrane disease The patient should be hyperventilated B. C. The patient should be given indomethacin D. Treatment with extracorporeal membrane oxygenator (ECMO) isn’t effective E. Patient should be operated because of PDA as soon as possible A baby of 40 weeks’ gestation is born weighing 2000g. Which of the following statements is likely to be true of this infant? A. He is premature He is at risk of developing hypoglycemia B. C. His mother is a prediabetic D. He has an extremely low birth weight (ELBW) E. His head circumference is likely to be on a similar percentile to his weight 144. 145. 146. 147. 148. 149. 150. A 25-years-old mother gave birth to twin boys at 38 weeks’ gestation. Twin A weighed 3200 g and twin B weighed 2400 g at birth. Which of the following statements is correct? A. The weight of twin B is appropriate for gestational age and twin A is large for gestational age The weight of twin A is appropriate for gestational age and twin B is small for B. gestational age C. Neither infant is appropriate weight for twins at 38 weeks’ gestation D. Both twins are large for twins at 38 weeks’ gestation E. Twin B needs parenteral feeding (TPN) because of his weight A 2.1 kg full-term infant of drug addicted mother becomes irritable and develops coarse tremors at 36 h of age. He feeds poorly and has diarrhoea and nasal stuffiness. Which of the following statements is true? A. The most likely diagnosis is hypoglycemia B. The most appropriate treatment for this infant is 10% calcium gluconate C. The patient should be isolated D. * The mother should be tested for hepatitis B antigen and AIDS E. Child should be separated from mother and hospitalized to ICU The newborn child suffered from severe asphyxia. Right after the birth appeared the next symptoms: absence of sucking reflex, regurgitation, “sunset” symptom and restlessness. What syndrom has the child? A. Convulsive B. Intoxication C. Oppression D. *Hypertensive-hydrocephalic E. Irritation A 2-weeks-old has a red spot on the back. The lesion is warm and tender. The mother denies trauma and reports that the lesion appeared day before. This otherwise well-appearing infant is growing and developing normally and appears a little bit excited upon physical examination. The most likely diagnosis in this infant is: A. Child abuse B. Mongolian spot C. Subcutaneous fat necrosis D. *Necrotic phlegmona E. Ritter’s dermatitis A 7-days-old girl presents to you for the first time with a red spot on the chest. The lesion is warm, dry and tender. Skin is not damaged. The mother denies trauma and reports that the lesion appeared day before. This otherwise well-appearing infant is growing and developing normally and appears a little bit excited upon physical examination. It was diagnosed flegmona of newborn. What stage of disease is the most possible to diagnose? A. *Initial B. Exudative C. Alternative-necrotic D. Exfoliative E. Reparation The 7-days old boy has a copious amount of yellowish umbilical discharge, umbilical wound has no epitelization signs, periumbilical area is tender, red and painful, the baby is excited, he cries and refuse from meal. The most likely diagnosis is: A. Phungus B. Catarrhal omphalitis C. *Purulent omphalitis D. Omphalocele E. Healthy baby The 17-days old white boy has a copious amount of serous umbilical discharge, umbilical wound 151. 152. 153. 154. 155. 156. 157. has poor epitelization signs, periumbilical area is soft, pink and painless; the baby is active, he demonstrates good appetite. The most likely diagnosis is: A. Phungus B. *Catarrhal omphalitis C. Purulent omphalitis D. Omphalocele E. Healthy baby The child was born from 2nd pregnancy at 37 weeks of gestation. Previous child in this family has hydrocefalus. This pregnancy was on background of polyhydramnion. The birth weight is 2800 g. Objectively: significant hepatosplenomegaly, jaundice, enlargement of the head. In the head CT scan was revealed calcification. What is previous diagnosis? A. Rubella B. Syphilis C. Cytomegalovirus D. *Toxoplasmosis E. Lysteriosis Boy was born from the first pregnancy. Her birth weight is 2700 g. Head circumference 61 cm. He has hepato-splenomegaly, muscle hypertonia, jaundice. What of the following symptoms is the most typical for the congenital toxoplasmosis? A. Small birth weight B. *Hydrocefalus C. Jaundice D. Muscle hypertonus E. Hepatospleenomegaly On the examination of patient’s placenta were revealed atypical gigantic cells with big nucleus (“owl eyes”). What is the probable diagnose? A. Rubella B. *Cytomegalovirus C. Toxoplasmosis D. Lysteriosis E. Syphilis On the micrograph of placenta the characteristic cell with large nucleus is seen. What congenital infection is it typical for? A. Herpes B. Toxoplasmosis C. *Cytomegalovirus D. Congenital syphilis E. Congenital rubella The characteristic cells with large nucleus are present on the placenta. What congenital infection is it typical for? A. Herpes B. Toxoplasmosis C. *Cytomegalovirus D. Congenital syphilis E. Congenital rubella During the ophthalmological examination in newborn girl cataract of both eyes with the “salt and pepper” symptom was revealed. These changes are the most typical for: A. Toxoplasmosis B. Glycogen storage disease C. *Congenital rubella D. Congenital syphilis E. Cytomegalovirus infection The boy presented in the picture was born from 1st pregnancy, 1st delivery at 37 weeks of 158. 159. 160. 161. 162. gestation. Mother of child is working in kindergarten. In first trimester of pregnancy she suffered from some allergy and had fever during few days. On the 2nd day after birth jaundice and petechial skin rush has appeared. There is generalized lymphadenopathy and hepatosplenomegaly. What is the most possible diagnose? A. Congenital toxoplasmosis B. Congenital herpes C. CMV infection D. *Congenital rubella E. Congenital syphilis The girl was born from 2nd pregnancy, 2nd delivery at 36 weeks of gestation. On the 2nd day after birth jaundice and petechial skin rush has appeared. There is generalized lymphadenopathy and hepatosplenomegaly. During ophthalmic examination cataracts of both ayes was found. During heart auscultation there is intensive systolic murmur on all points of auscultation. What is the most possible diagnose? A. Congenital toxoplasmosis B. Congenital herpes C. CMV infection D. *Congenital rubella E. Congenital syphilis The child was born from 3rd pregnancy at 33-34 weeks of gestation. Previous pregnancies finished with miscarriages. This pregnancy was on background of early gestosis, polyhydramnion. The birth weight is 1,800 g. Objectively: hepatosplenomegaly, jaundice, plural petechia, expressed dyspnea, cyanosis, oppression syndrome. Gigantic cells are revealed in the urine. What is previous diagnosis? A. Rubella B. Galactosemia C. *Cytomegalovirus D. Hemolytic disease of the newborn E. Prematurity Newborn child has generalized maculopapular rush, hepatospleenomegaly, myocarditis, generalized lymphadenopathy. Level of platelets in blood is 135x10^9/L. From anamnesis it’s known that at his mother’s house is living cat. What diagnose should be checked first of all: A. Herpes B. Rubella C. CMV D. Syphilis E. *Toxoplasmosis Girl is 2 days old. She has generalized maculopapular rush, hepatospleenomegaly, myocarditis, generalized lymphadenopathy, decreased level of platelets and anemia. From anamnesis it’s known that her mother is veterinary surgeon. What diagnose should be checked first of all: A. Rubella B. *Toxoplasmosis C. CMV D. Syphilis E. Herpes A 3-day-old girl of low birth weight had generalized purpura. Physical examination revealed a continuous murmur at the left upper sternal border and hepatospleenomegaly. What’s the most reliable diagnose? A. Congenital heart defect B. Congenital pneumonia C. CMV infection D. *Congenital rubella E. Congenital toxoplasmosis 163. 164. 165. 166. 167. 168. 169. Choose the diagnosis for a 1-day-old healthy infant with a superficial swelling over the left parietotemporal region that does not cross the suture lines: A. Intraventricular hemorrhage B. Caput succedaneum C. Subdural hemorrhage D. Subarachnoid hemorrhage E. *Cephalohematoma The child is 6 days old. He was born with body weight 3,800 g., length 52 cm., from the 1st, prolonged delivery, assesment by Apgar score - 7/8 points. In left parietal region was revealed edema, and fluctuation. The jaundice has appeared on the 5th day. Sclera and mucus membranes are pink. Cardiac rate is 152 in 1 minute; breathing rate is 48 in a minute. What is the most possible reason of the jaundice? A. Conjugative jaundice B. Sepsis C. *Resorption of cephalomatoma D. Hemolytic disease of the newborn E. CMV-infection The boy was born from 3-rd pregnancy, 3rd prolonged labor. The prolonged arrest of the head on the entry in small pelvis took place during the delivery. During examination: head has dolichocephalic shape, there’s oedema of soft tissues in occipital region. Fluctuation symptom is negative. What is the probable diagnosis? A. Cephalohematoma B. *Caput succedaneum C. Cerebral hemorrhage D. Subarachnoid hemorrhage E. Intraventricular hemorrhage In the 1-day old girl after the birth in head presentation is palpated edema of the head. It is soft, elastic, spreads through skull sutures, painless. The upper skin is cyanotic with plural petechia and ecchymosed. In 2 days these changes disappeared without treatment. Put the diagnosis. A. *Caput succedaneum B. Subaponeurotic hemorrhage C. Cephalohematoma D. Skull fracture E. Perinatal encephalopathy What birth trauma should be diagnosed in case of C5-C6 and (sometimes) T1 plexus brachialis injury? A. Kerer's palsy B. *Erb's palsy C. Klumpke’s palsy D. Horner’s syndrome E. Kofferate syndrome The 3-days old newborn girl’s left arm is held in the characteristic posture of adduction with internal rotation. The elbow is extended and the forearm is pronated, she has “waiter's tip” hand. Wrist and hand movements are preserved. The biceps stretch reflex is absent, but the triceps reflex is spared. What is the possible diagnose? A. Kerer's palsy B. Acute osteomyelitis of the right arm C. *Erb's palsy D. Kofferate syndrome E. Klumpke’s palsy The boy was born from the 1st pregnancy in 37-38 weeks of gestation with the secondary weakness of the birth activity, double loop of cord around the neck. The birth weight is 4,350 g., length 54 cm., Apgar score is 6/7 points. During examination: large fontanel is 2.5x3.0 cm. Left 170. 171. 172. 173. 174. hand hangs down along the trunk; motions are absent, positive scarf syndrome. What is the probable diagnosis? A. *Birth trauma, total palsy of the left shoulder (Kerer's palsy) B. Acute hematogenous osteomyelitis of the left shoulder C. Birth trauma, upper palsy of the shoulder (Dushen-Erb's palsy) D. Birth trauma, rupture of the sterno-cleido-mastoideus muscle on the left side E. Traumatic-hypoxic encephalopathy The 1-day old newborn girl’s left arm is held in the characteristic posture of adduction with internal rotation, she has “waiter's tip” hand. Wrist and hand movements are maintained. The biceps stretch reflex is absent, but the triceps reflex is spared. What is the possible diagnose? A. Kerer's palsy B. Acute osteomyelitis of the left arm C. *Erb's palsy D. Kofferate syndrome E. Klumpke’s palsy An infant is born via emergent cesarean section. Birth weight was 1150 g. The infant has poor respiratory effort and you egin bag-mask ventilation but find it extremely difficult to cause chest wall movement. A chest radiograph eveals diffuse whiteout of both lungs, with an occasional air bronchogram. What is the diagnosis? A. *Respiratory distress syndrome B. Bronchopulmonary dysplasia C. Pneumothorax D. Meconium aspiration E. Bacterial pneumonia You were called to examine the 9 days old newborn girl. Day before in her appeared jaundice; baby is excited, crying. During examination is revealed hepatomegaly. What is your tactics? A. Prescription of phenobarbital B. Further observation for the child at home C. To give recommendations to parents about feeding and care for baby D. *Immediate hospitalization of child E. Hospitalization after performing of abdominal USD A 5-day-old baby is seen in the Emergency Department one day because of lethargy, poor feeding, vomiting. His skin is cold and mottled, and his temperature is 38,8 0C. After stabilization, which one of the following is the most appropriate investigation? A. *Lumbar puncture B. Blood gases C. Chest X-ray D. Serum electrolytes E. Cranial ultrasound A newborn girl was born from 3-rd pregnancy, 1st delivery at 35 weeks of gestation. The Apgar score is 6/7; body weight is 2,700, length – 50 cm, head circumference 34 cm, chest circumference – 33 cm. Large fontanel is 4x3 cm, sutures are soft, unclosed. Temperature is 38,5 0C, there are seizures, tremor of the extremities. Muscular hypertonia. On the 2nd day after birth jaundice has appeared. There is generalized lymphadenopathy and hepatosplenomegaly. During ophthalmic examination cataracts of both ayes was found. She has skin rush. What is the most possible diagnose for the girl? A. Fetal hepatitis B. Toxoplasmosis C. Cytomegalovirus infection D. Congenital syphilis E. *Congenital rubella Тести до малюнків 1. 2. 3. 4. 5. 6. 7. 8. 9. What pathology is presented in the X-ray (figure 42)? A. Congenital bone malformation B. Humerus osteomyelitis C. *Humerus fracture D. Femur fracture E. Radius fracture What pathology is presented in the figure 47? A. Musculoskeletal injuries B. Clavicle fracture C. Ribs fracture D. Birth trauma E. *All is correct What changes are present in the newborn’s MRI (figure 53)? A. Intraventricular hemorrhage B. Caput succedaneum C. *Cephalohematoma D. Subarachnoid hemorrhage E. Subdural hemorrhage In the figure 25 is presented the newborn child who suffered from severe asphyxia. Right after the birth appeared the next symptoms: absence of sucking reflex, regurgitation, “sunset” symptom and restlessness. What syndrom has the child? A. Convulsive B. Intoxication C. Oppression D. *Hypertensive-hydrocephalic E. Irritation What symptom is present in newborn pictured in figure 26? A. Mobius's symptom B. *Graefe's sign C. Kocher's sign D. Kernig's symptom E. Brudzinski’s sign What clinical signs are presented in the figure 27? A. Muscle dystonia B. Assymetric locomotor activity C. Reflexes suppression D. *All is correct E. All is incorrect What is the possible indication for the investigation pictured in figure 28? A. Convulsive syndrome B. Neonatal meningitis C. Subarachnoid hemorrhage D. Hypertensive-hydrocephalic syndrome E. *All is correct What pathology is presented in the X-ray (figure 41)? A. Intraventricular hemorrhage B. Caput succedaneum C. Subdural hemorrhage D. Subarachnoid hemorrhage E. *Cephalohematoma A 1-week-old white infant presents to you for the first time with a red spot on the back, as shown in the photograph 84. The lesion is warm and tender. The mother denies trauma and reports that the lesion appeared day before. This otherwise well-appearing infant is growing and developing 10. 11. 12. 13. 14. 15. 16. normally and appears a little bit excited upon physical examination. The most likely diagnosis in this infant is: A. Child abuse B. Mongolian spot C. Subcutaneous fat necrosis D. *Necrotic phlegmona E. Ritter’s dermatitis A 1-week-old white infant presents to you for the first time with a red spot on the back, as shown in the photograph 84. The lesion is warm and tender. The mother denies trauma and reports that the lesion appeared day before. This otherwise well-appearing infant is growing and developing normally and appears a little bit excited upon physical examination. It was diagnosed flegmona of newborn. What stage of disease is presented? A. *Initial B. Exudative C. Alternative-necrotic D. Exfoliative E. Reparation The most frequent reason of this pathological state development (figure 84) is: A. *Infection B. Overcooling C. Compression D. congenital immunodeficiency E. All is correct For the disease presented in the figure 84 is typical: A. Erosive skin surfaces B. Hemorrhagic bullae C. *Intoxication syndrome D. Positive Nikolsky’s sign E. All is correct The typical symptom of the disease presented in the figure 84 is: A. Soft tissues infiltration B. Intoxication syndrome C. Deep scars on the skin D. "Creeping infiltration" E. *All is correct In the child with the disease which is presented in the figure 84 on the skin usually appear: A. Phlyctena B. Vesicles C. Bullae D. All is correct E. *All is incorrect The typical symptom of the disease presented in the figure 84 is: A. Hypertermia B. Skin hyperemia C. Deep traumatic surface D. Soft tissues infiltration E. *All is correct What disease is presented in the figure 84? A. *Phlegmona B. Bullous impetigo C. Pemphygus neonatorum D. Cellulitis E. Ritter’s dermatitis 17. 18. 19. 20. 21. 22. 23. 24. 25. What disease is typical sign presented in the figure 84 for? A. *Phlegmona B. Bullous impetigo C. Pemphygus neonatorum D. Physiological erythema E. Ritter’s dermatitis What problems should be differentiated pathological state presented in the figure 84 with? A. Bullous epidermolysis B. Mongolian spot C. Cellulitis D. Allergic dermatitis E. *All is correct For the disease of the newborn baby which is presented in figure 82 are typical the next symptoms: A. Hyperthermia B. Skin erythema C. Presence of the bullas on the skin D. Positive Nikolsky's sign E. *All is correct The typical symptom of the disease presented in the figure 82 is: A. Skin infiltration B. Palms hyperkeratosis C. Deep scars on the skin D. Bullae with bloody content E. *Positive Nikolsky’s sign For the disease presented in the figure 82 are typical: A. Tonic seizures B. Feet hyperkeratosis C. Hydrocephalus D. Ektropion E. *Erosive skin changes What disease is presented in the figure 82? A. Flegmona neonatorum B. Erythema toxicum neonatorum C. Bullous impetigo D. *Ritter’s dermatitis E. Physiological erythema The most frequent etiological factor of the disease presented in the figure 82 is: A. Chlamydia trachomatis B. Group B streptococci C. Neisseria gonorrhoeae D. *Staphylococcus aureus E. Trichomonas vaginalis The disease presented in the figure 82 should be differentiated with: A. Congenital syphilis B. Bullous epidermolysis C. Pemphygus neonatorum D. Allergic dermatitis E. *All is correct What stage of the disease is presented in the figure 86? A. Initial B. Exudative C. *Alternative-necrotic Exfoliative Reparation What stage of the disease is presented in the figure 88? A. Initial B. Exudative C. *Alternative-necrotic D. Exfoliative E. Reparation What pathology is presented in the figure 98? A. Congenital bones anomaly B. *Femoral osteomyelitis C. Congenital hip dislocation D. Femoral fracture E. Rickets What changes are presented in the figure 102? A. Intestinal dilatation B. Pneumatosis intestinalis C. Ascites D. *All is correct E. All is incorrect What disease are typical presented X-ray changes (figure 102) for? A. Volvulus B. Intra-abdominal tumor C. *Necrotizing enterocolitis D. Meconium peritonitis E. Physiological dyspepsia What symptom is presented in figure 79? A. Kernig’s symptom B. *Nikolsky’s symptom C. Graefe's symptom D. Trousseau's sign E. Kocher's sign What is the possible diagnosis for the baby presented in the figure 80? A. Bullous impetigo B. Vesiculopustulosis C. Subcutaneous fat necrosis D. *Ritter’s dermatitis E. Necrotic phlegmona The 9-days old girl has a copious amount of yellowish cacodorous umbilical discharge, umbilical ound has no epitelization signs, periumbilical area is tender, red and painful (figure 96); the baby is excited, he cries and refuse from meal. The most likely diagnosis is: A. Phungus B. Catarrhal omphalitis C. *Purulent omphalitis D. Omphalocele E. Healthy baby This is the contamination mechanism of (figure 121): A. Staphylococcal infection B. Candidosis C. *Toxoplasmosis D. Lysteriosis E. Syphilis The 14-days old white boy has a copious amount of serous umbilical discharge, umbilical wound D. E. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. has poor epitelization signs (figure 97), periumbilical area is soft, pink and painless; the baby is active, he demonstrates good appetite. The most likely diagnosis is: A. Phungus B. *Catarrhal omphalitis C. Purulent omphalitis D. Omphalocele E. Healthy baby On the figure 120 is pictured: A. Trypanosoma cruzi B. *Toxoplasma gondii C. Treponema pallidum D. Listeria monocytogenes E. Cytomegalovirus The child presented in the picture 123 was born from 2nd pregnancy at 37 weeks of gestation. revious child in this family has hydrocefalus. This pregnancy was on background of polyhydramnion. The birth weight is 2800 g. Objectively: significant hepatosplenomegaly, jaundice, enlargement of the head. In the head CT scan was revealed calcification. What is previous diagnosis? A. Rubella B. Syphilis C. Cytomegalovirus D. *Toxoplasmosis E. Lysteriosis Girl presented in the picture 123 was born from the first pregnancy. Her birth weight is 2900 g. Head circumference 62 cm. She has hepatospleenomegaly, muscle hypertonia, jaundice. What of the following symptoms is the most typical for the congenital toxoplasmosis? A. Small birth weight B. *Hydrocefalus C. Jaundice D. Muscle hypertonus E. Hepatospleenomegaly On the examination of patient’s placenta were revealed atypical gigantic cells with big nucleus (“owl eyes”) – figure 110. What is the probable diagnose? A. Rubella B. *Cytomegalovirus C. Toxoplasmosis D. Lysteriosis E. Syphilis On the micrograph of placenta the characteristic cell with large nucleus is seen off-centre at the bottom-right of the image 111. What congenital infection is it typical for? A. Herpes B. Toxoplasmosis C. *Cytomegalovirus D. Congenital syphilis E. Congenital rubella The characteristic cells with large nucleus are present on the placenta micrograph (figure 118). What congenital infection is it typical for? A. Herpes B. Toxoplasmosis C. *Cytomegalovirus D. Congenital syphilis E. Congenital rubella During the ophthalmological examination in newborn girl cataract of both eyes with the “salt and 42. 43. 44. 45. 46. pepper” symptom was revealed (look on the figure 126). These changes are the most typical for: A. Toxoplasmosis B. Glycogen storage disease C. *Congenital rubella D. Congenital syphilis E. Cytomegalovirus infection The boy presented in the picture was born from 1st pregnancy, 1st delivery at 37 weeks of gestation. Mother of child is working in kindergarten. In first trimester of pregnancy she suffered from some allergy and had fever during few days. On the 2nd day after birth jaundice and petechial skin rush has appeared (figure 104). There is generalized lymphadenopathy and hepatosplenomegaly. What is the most possible diagnose? A. Congenital toxoplasmosis B. Congenital herpes C. CMV infection D. *Congenital rubella E. Congenital syphilis The newborn girl presented in the figure 125 was born from 2nd pregnancy, 2nd delivery at 36 weeks of gestation. On the 2nd day after birth jaundice and petechial skin rush has appeared. There is generalized lymphadenopathy and hepatosplenomegaly. During ophthalmic examination cataracts of both ayes was found. During heart auscultation there is intensive systolic murmur on all points of auscultation. What is the most possible diagnose? A. Congenital toxoplasmosis B. Congenital herpes C. CMV infection D. *Congenital rubella E. Congenital syphilis The child presented in the figure 107 was born from 3rd pregnancy at 33-34 weeks of gestation. revious pregnancies finished with miscarriages. This pregnancy was on background of early gestosis, polyhydramnion. The birth weight is 1,800 g. Objectively: hepatosplenomegaly, jaundice, plural petechia, expressed dyspnea, cyanosis, oppression syndrome. Gigantic cells are revealed in the urine. What is previous diagnosis? A. Rubella B. Galactosemia C. *Cytomegalovirus D. Hemolytic disease of the newborn E. Prematurity Newborn child presented in the picture 108 has generalized maculopapular rush, hepatospleenomegaly, myocarditis, generalized lymphadenopathy. Level of platelets in blood is 135x10^9/L. From anamnesis it’s known that at his mother’s house is living cat. What diagnose should be checked first of all: A. Herpes B. Rubella C. CMV D. Syphilis E. *Toxoplasmosis Girl presented in the figure 108 is 2 days old. She has generalized maculopapular rush, hepatospleenomegaly, myocarditis, generalized lymphadenopathy, decreased level of platelets and anemia. From anamnesis it’s known that her mother is veterinary surgeon. What diagnose should be checked first of all: A. Rubella B. *Toxoplasmosis C. CMV D. Syphilis Herpes The triad presented in the figure 127 is typical for: A. *Rubella B. Herpes C. CMV D. Syphilis E. Toxoplasmosis A 3-day-old girl of low birth weight had generalized purpura. Physical examination revealed a continuous murmur at the left upper sternal border and hepatospleenomegaly. Here is her eye changes (figure 115). What’s the most reliable diagnose? A. Congenital heart defect B. Congenital pneumonia C. CMV infection D. *Congenital rubella E. Congenital toxoplasmosis The typical symptom of the disease presented in the figure 83 is: A. Skin infiltration B. Palms hyperkeratosis C. Deep scars on the skin D. Bullae with bloody content E. *Positive Nikolsky’s sign For the disease presented in the figure 83 are typical: A. Tonic seizures B. Feet hyperkeratosis C. Hydrocephalus D. Ektropion E. *Erosive skin changes What disease is presented in the figure 83? A. Flegmona neonatorum B. Erythema toxicum neonatorum C. Bullous impetigo D. *Ritter’s dermatitis E. Physiological erythema The most frequent etiological factor of the disease presented in the figure 83 is: A. Chlamydia trachomatis B. Group B streptococci C. Neisseria gonorrhoeae D. *Staphylococcus aureus E. Trichomonas vaginalis The disease presented in the figure 83 should be differentiated with: A. Congenital syphilis B. Bullous epidermolysis C. Pemphygus neonatorum D. Allergic dermatitis E. *All is correct Choose the diagnosis for a 1-day-old healthy infant with a superficial swelling over the left parietotemporal region that does not cross the suture lines (figure 40). A. Intraventricular hemorrhage B. Caput succedaneum C. Subdural hemorrhage D. Subarachnoid hemorrhage E. *Cephalohematoma The child is 2 days old. He was born with body weight 4,200 g., length 52 cm., from the 1st, E. 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. prolonged delivery, assesment by Apgar score - 5/7 points. In left parietal region was revealed edema, and fluctuation (figure 48). The jaundice has appeared on the 5th day. Sclera and mucus membranes are pink. Cardiac rate is 152 in 1 minute; breathing rate is 48 in a minute. What is the most possible reason of the jaundice? A. Conjugative jaundice B. Sepsis C. *Resorption of cephalomatoma D. Hemolytic disease of the newborn E. CMV-infection Choose the most possible diagnosis for the baby in figure 48. A. Subgaleal hematoma B. Caput succedaneum C. *Cephalohematoma D. Subarachnoid hemorrhage E. Skull fracture The child was born from 2nd pregnancy, 2nd prolonged labor. The prolonged arrest of the head on the entry in small pelvis took place during the delivery. During examination: head has dolichocephalic shape, there’s oedema of soft tissues in occipital region (figure 38). Fluctuation symptom is negative. What is the probable diagnosis? A. Cephalohematoma B. *Caput succedaneum C. Cerebral hemorrhage D. Subarachnoid hemorrhage E. Intraventricular hemorrhage In the 1-day old child after the birth in head presentation is palpated edema of the head. It is soft, elastic, spreads through skull sutures, painless. The upper skin is cyanotic with plural petechia and ecchymosed (figure 38). In 2 days these changes disappeared without treatment. Put the diagnosis. A. *Caput succedaneum B. Subaponeurotic hemorrhage C. Cephalohematoma D. Skull fracture E. Perinatal encephalopathy What birth trauma should be diagnosed in case of C5-C6 and (sometimes) T1 plexus brachialis injury (figure 54)? A. Kerer's palsy B. *Erb's palsy C. Klumpke’s palsy D. Horner’s syndrome E. Kofferate syndrome What birth trauma should be diagnosed in case of C7-C8 plexus brachialis injury (figure 54)? A. Kerer's palsy B. Erb's palsy C. *Klumpke’s palsy D. Horner’s syndrome E. Kofferate syndrome What birth trauma should be diagnosed in case of C5-C8 plexus brachialis injury (figure 54)? A. *Kerer's palsy B. Erb's palsy C. Klumpke’s palsy D. Horner’s syndrome E. Kofferate syndrome What birth trauma should be diagnosed in case of C7-C8, T1 plexus brachialis injury (figure 54)? Kerer's palsy Erb's palsy and Horner’s syndrome *Klumpke’s palsy and Horner’s syndrome Horner’s syndrome Kofferate syndrome What does indicate number 1 in the Fig. 46? A. Caput succedaneum B. *Cefalohematoma C. Subgaleal hemorrhage D. Epidural hemorrhage E. Subarachnoid hemorrhage What does indicate number 2 in the Fig. 46? A. Caput succedaneum B. Cefalohematoma C. Subgaleal hemorrhage D. *Epidural hemorrhage E. Subarachnoid hemorrhage What does indicate number 3 in the Fig. 46? A. *Caput succedaneum B. Cefalohematoma C. Subgaleal hemorrhage D. Epidural hemorrhage E. Subarachnoid hemorrhage What does indicate number 4 in the Fig. 46? A. Caput succedaneum B. Cefalohematoma C. *Subgaleal hemorrhage D. Epidural hemorrhage E. Subarachnoid hemorrhage The 2-days old newborn girl’s left arm is held in the characteristic posture of adduction with internal rotation. (Fig 44)The elbow is extended and the forearm is pronated, she has “waiter's tip” hand. Wrist and hand movements are preserved. The biceps stretch reflex is absent, but the triceps reflex is spared. What is the possible diagnose? A. Kerer's palsy B. Acute osteomyelitis of the right arm C. *Erb's palsy D. Kofferate syndrome E. Klumpke’s palsy The boy was born from the 1st pregnancy in 41-42 weeks of gestation with the secondary weakness of the birth activity, double loop of cord around the neck. The birth weight is 4,500 g., length 52 cm., Apgar score is 5/7 points. During examination: large fontanel is 2.5x3.0 cm. Left hand hangs down along the trunk; motions are absent (figure 45), positive scarf syndrome. What is the probable diagnosis? A. *Birth trauma, total palsy of the left shoulder (Kerer's palsy) B. Acute hematogenous osteomyelitis of the left shoulder C. Birth trauma, upper palsy of the shoulder (Dushen-Erb's palsy) D. Birth trauma, rupture of the sterno-cleido-mastoideus muscle on the left side E. Traumatic-hypoxic encephalopathy The 1-day old newborn boy’s left arm is held in the characteristic posture of adduction with internal rotation, he has “waiter's tip” hand (figure 44). Wrist and hand movements are maintained. The biceps stretch reflex is absent, but the triceps reflex is spared. What is the possible diagnose? A. Kerer's palsy A. B. C. D. E. 63. 64. 65. 66. 67. 68. 69. Acute osteomyelitis of the left arm *Erb's palsy Kofferate syndrome Klumpke’s palsy The 1 day old boy is presented on the figure 43 after prolonged labor with forceps usage. What is the probable diagnosis? A. Horner’s syndrome B. *Right facial nerve paralyses C. Left facial nerve paralyses D. Both sides facial nerves paralyses E. Kofferate syndrome The typical symptom of the disease presented in the figure 79 is: A. Skin infiltration B. Palms hyperkeratosis C. Deep scars on the skin D. Bullae with bloody content E. *Positive Nikolsky’s sign For the disease presented in the figure 79 are typical: A. Tonic seizures B. Feet hyperkeratosis C. Hydrocephalus D. Ektropion E. *Erosive skin changes What disease is presented in the figure 79? A. Flegmona neonatorum B. Erythema toxicum neonatorum C. Bullous impetigo D. *Ritter’s dermatitis E. Physiological erythema The most frequent etiological factor of the disease presented in the figure 79 is: A. Chlamydia trachomatis B. Group B streptococci C. Neisseria gonorrhoeae D. *Staphylococcus aureus E. Trichomonas vaginalis The disease presented in the figure 79 should be differentiated with: A. Congenital syphilis B. Bullous epidermolysis C. Pemphygus neonatorum D. Allergic dermatitis E. *All is correct What symptom is typical for the disease presented in the figure 80? A. Skin infiltration B. Palms hyperkeratosis C. Deep scars on the skin D. Bullae with bloody content E. *Positive Nikolsky’s sign For the disease presented in the figure 80 is specific: A. Tonic seizures B. Feet hyperkeratosis C. Hydrocephalus D. Ektropion E. *Erosive skin changes B. C. D. E. 70. 71. 72. 73. 74. 75. 76. 77. 78. 79. 80. 81. 82. 83. 84. 85. 86. The most frequent etiological factor of the disease presented in the figure 80 is: A. Chlamydia trachomatis B. *Staphylococcus aureus C. Neisseria gonorrhoeae D. E. Candida albicans E. Group B streptococci The disease presented in the figure 80 should be differentiated with: A. Congenital syphilis B. Bullous epidermolysis C. Pemphygus neonatorum D. Allergic dermatitis E. *All is correct The most frequent reason of this pathological state development (figure 86) is: A. *Infection B. Overcooling C. Compression D. congenital immunodeficiency E. All is correct For the disease presented in the figure 86 is typical: A. Erosive skin surfaces B. Hemorrhagic bullae C. *Intoxication syndrome D. Positive Nikolsky’s sign E. All is correct The typical symptom of the disease presented in the figure 86 is: A. Soft tissues infiltration B. Intoxication syndrome C. Deep scars on the skin D. "Creeping infiltration" E. *All is correct In the child with the disease which is presented in the figure 86 on the skin usually appear: A. Phlyctena B. Vesicles C. Bullae D. All is correct E. *All is incorrect The typical symptom of the disease presented in the figure 86 is: A. Hypertermia B. Skin hyperemia C. Deep traumatic surface D. Soft tissues infiltration E. *All is correct What disease is presented in the figure 86? A. *Phlegmona B. Bullous impetigo C. Pemphygus neonatorum D. Cellulitis E. Ritter’s dermatitis What disease is typical sign presented in the figure 86 for? A. *Phlegmona B. Bullous impetigo C. Pemphygus neonatorum D. Physiological erythema Ritter’s dermatitis What problems should be differentiated pathological state presented in the figure 86 with? A. Bullous epidermolysis B. Mongolian spot C. Cellulitis D. Allergic dermatitis E. *All is correct The most frequent reason of this pathological state development (figure 88) is: A. *Infection B. Overcooling C. Compression D. congenital immunodeficiency E. All is correct For the disease presented in the figure 88 is typical: A. Erosive skin surfaces B. Hemorrhagic bullae C. *Intoxication syndrome D. Positive Nikolsky’s sign E. All is correct The typical symptom of the disease presented in the figure 88 is: A. Soft tissues infiltration B. Intoxication syndrome C. Deep scars on the skin D. "Creeping infiltration" E. *All is correct In the child with the disease which is presented in the figure 88 on the skin usually appear: A. Phlyctena B. Vesicles C. Bullae D. All is correct E. *All is incorrect The typical symptom of the disease presented in the figure 88 is: A. Hypertermia B. Skin hyperemia C. Deep traumatic surface D. Soft tissues infiltration E. *All is correct What disease is presented in the figure 88? A. *Phlegmona B. Bullous impetigo C. Pemphygus neonatorum D. Cellulitis E. Ritter’s dermatitis What disease is typical sign presented in the figure 88 for? A. *Phlegmona B. Bullous impetigo C. Pemphygus neonatorum D. Physiological erythema E. Ritter’s dermatitis What problems should be differentiated pathological state presented in the figure 88 with? A. Bullous epidermolysis B. Mongolian spot C. Cellulitis E. 87. 88. 89. 90. 91. 92. 93. 94. 95. Allergic dermatitis *All is correct For the disease which is presented in the figure 92 is typical presence of: A. Erosive surfaces B. Hemorrhagic bullas C. *Intoxication syndrome D. Positive Nicolsky’s sign E. All is correct The most frequent reason of this pathological state development (figure 92) is: A. *Infection B. Overcooling C. Compression D. congenital immunodeficiency E. All is correct The typical symptom of the disease presented in the figure 92 is: A. Intoxication syndrome B. Skin hyperaemia C. Deep scars on the skin D. Soft tissues infiltration E. *All is correct For the child with the disease which is presented in the figure 92 is typical the presence of: A. Phlyctena B. Vesicles C. Bullae D. All is correct E. *All is incorrect The typical symptom of the disease presented in the figure 92 is: A. Hypertermia B. Skin hyperaemia C. Positive local fluctuation symptom D. Soft tissues infiltration E. *All is correct What disease is presented in the figure 92? A. Phlegmona B. Bullous impetigo C. Hormonal crisis D. *Mastitis E. Pemphygus neonatorum What disease is typical sign presented in the figure 92 for? A. *Mastitis B. Bullous impetigo C. Hormonal crisis D. Phlegmona E. Pemphygus neonatorum What problems should be differentiated pathological state presented in the figure 88 with? A. Tumor B. Adiposonecrosis C. Cellulitis D. Sepsis E. *All is correct In the figure 2 is presented: A. Tachypnea B. Apnea D. E. 96. 97. 98. 99. 100. 101. 102. 103. 104. Grants *Retractions Paradoxical respiration Retractions demonstrated in the figure 2 according to Silverman scale can be estimated as: A. O points B. 1 point C. *2 points D. 3 points E. Shouldn’t be estimated Look on the chest X-ray of 1-day old premature newborn (figure 4) and put diagnosis: A. Left-side pneumonia B. Both-sides pneumonia C. *Hyaline membrane disease D. Emphysema E. Meconium aspiration syndrome An infant of uncertain dates is born via emergent cesarean section after the mother was critically injured in a motor vehicle accident. Birth weight was 1075 g. The infant has poor respiratory effort and you begin bag-mask ventilation but find it extremely difficult to cause chest wall movement. A chest radiograph reveals diffuse whiteout of both lungs, with an occasional air bronchogram (figure 4). What is the diagnosis? A. *Respiratory distress syndrome (hyaline membrane disease) B. Bronchopulmonary dysplasia C. Pneumothorax D. Meconium aspiration E. Bacterial pneumonia What is another name of X-ray “white lung” (figure 4) in hyaline membrane disease? A. Total inflamation B. *Air bronchogram C. Pseudoemphysema D. Abscess E. Pneumothorax The newborn girl presented in figure 24 was born with weight 900 g, her gestational age is 30 weeks. What grade of prematurity is this? A. Grade I B. Grade II C. *Grade III D. Grade IV E. Grade V The newborn girl presented in figure 22 was born with weight 700 g, her gestational age is 27weeks. What grade of prematurity is this? A. Grade I B. Grade II C. Grade III D. *Grade IV E. Grade V The newborn girl presented in figure 124 was born with weight 1200 g, her gestational age is 3weeks. What grade of prematurity is this? A. Grade I B. Grade II C. *Grade III D. Grade IV E. Grade V The nasogastric tube for the feeding of premature newborns (figure 17) should be replaced: C. D. E. 105. 106. 107. 108. 109. 110. 111. 112. After every feeding Within 24 hours Within 48 hours *Within 72 hours Within 96 hours The acholic stool (figure 68) is typical for the: A. Physiological jaundice B. Haemolytic jaundice C. *Mechanical jaundice D. Parenchymatous jaundice E. All is incorrect The acholic stool (figure 68) is one of the typical symptoms for the: A. Physiological jaundice B. Haemolytic disease of newborns C. *Bile ducts atresia D. Fetal hepatitis E. All is correct You were called to examine the 12 days old newborn boy. Day before in him appeared jaundice; aby is excited, crying (figure 69). During examination is revealed hepatomegaly. What is your tactics? A. Prescription of phenobarbital B. Further observation for the child at home C. To give recommendations to parents about feeding and care for baby D. *Immediate hospitalization of child E. Hospitalization after performing of abdominal USD What method of phototherapy can be performed with the help of the lamp pictured in the figure 71? A. Fiber-optical B. *Classic C. Intensive D. Spotted E. Is possible to perform any method Choose what jaundice in newborn IS NOT “dangerous” according Kramer’s scale evaluation (figure 67): A. Appeared within 48 hours of life at zone 4 B. Appeared within 24 hours of life anywhere at the body C. Appeared after 48 hours of life at zone 5 D. *Appeared after 48 hours of life at zone 3 E. Appeared within 24 hours at zone 1 Choose what jaundice in newborn can be called “dangerous” according Kramer’s scale evaluation (figure 67): A. Appeared within 48 hours of life at zone 4 B. Appeared within 24 hours of life anywhere at the body C. Appeared after 48 hours of life at zone 5 D. Appeared within 48 hours of life at zone 5 E. *All is correct What method of phototherapy is demonstrated in the figure 62? A. Forced B. Fiber-optical C. Classic D. Intensive E. *Spotted A 4-day-old baby is seen in the Emergency Department one evening because of lethargy and poor A. B. C. D. E. 113. 114. 115. 116. 117. 118. 119. 120. 121. feeding (figure 99). His skin is cold and mottled, and his temperature is 36,8 0C. After stabilization, which one of the following is the most appropriate investigation? A. *Lumbar puncture B. Blood gases C. Chest X-ray D. Serum electrolytes E. Cranial ultrasound A newborn girl was born from 2nd pregnancy, 2nd delivery at 37 weeks of gestation. The Apgar score is 7/8; body weight is 3,000, length – 50 cm, head circumference 34 cm, chest circumference – 33 cm. Large fontanel is 4x3 cm, sutures are soft, unclosed. Temperature is 38,5, there are seizures, tremor of the extremities. Muscular hypertonia. On the 2nd day after birth jaundice has appeared. There is generalized lymphadenopathy and hepatosplenomegaly. During ophthalmic examination cataracts of both ayes was found. She has skin changes which are presented in the figure 112. What is the most possible diagnose for the girl? A. Fetal hepatitis B. Toxoplasmosis C. Cytomegalovirus infection D. Congenital syphilis E. *Congenital rubella