Emanuel Resident Manual
advertisement

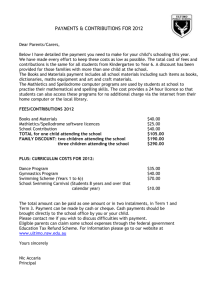
RESIDENT ORIENTATION TO THE PEDIATRIC WARD AT THE CHILDREN’S HOSPITAL AT LEGACY WELCOME Welcome to TCH. We hope you have a fun and educational experience. The following manual is a good reference for your roles and responsibilities while you are here. WHO CAN HELP? Dr. Lauren Rose, Pediatric Hospitalist; Clinical Director Pediatric Graduate Medical Education; Pager: 503-938-0954; lrose@lhs.org Dr. Ann Loeffler: Emanuel Site Medical Director; ID/Peds attending. Pager 503-938-0960; aloeffle@lhs.org Angela Cacchioli Graduate Medical Education Coordinator 3-4656; Can help with badges, computer access, parking, PACS access, meal cards, call room issues, scrubs, etc. CONFERENCES Noon Conference: (Monday-Friday 12:15-1:15, Rm 3317, 3rd floor Conference Room) Radiology Rounds (Thursday 11:45-12:15, Rm 3317, 3rd floor Conference Room): with Dr. Paul Marten or James Gilmore, pediatric radiologists. If they are late, page Dr. Marten at 503-938-1035 or call radiology at x32527. Friday Case Conference (7:30am, MOB West Conf Room): The attendings (often Lauren Rose or Eve Golden) are primarily responsible for choosing the cases which are presented as an unknown or interesting case for general discussion. The senior resident can help choose cases as well. Medical students and residents usually present the case. Coffee and pastries are served. Emanuel Pediatric Grand Rounds: (7:30am on the 3rd Tuesday of each month, Lorenzen Conf Center) Residents do not have to prepare for this. Coffee and pastries are served. HOLIDAYS While on rotation at Emanuel you will follow the Legacy holiday schedule. Below is a list of the official holidays: July 4th (observed on the calendar day on which it falls) Labor Day Thanksgiving (Thursday and Friday are holidays) Christmas and New Year’s are covered by the OHSU holiday schedule with half of the team taking time off over Christmas and half taking time off over New Year’s Memorial Day THE TEAM There are two main ward teams, a Blue team and a Green team. For the busiest several months of the year, we may also have a Gold team. Each team has a hospitalist who supervises the care of pediatric patients admitted to the ward service. The Blue team is the teaching team and is lead by a senior pediatric resident (R2) from OHSU, and has 3-4 pediatric and family practice interns on it (and sometimes a FM R2); the Green team includes a Pediatric Certified Nurse Practitioner (CPNP) and a pediatric hospitalist attending. The Gold team consists solely of a hospitalist who triages admission phone calls, helps with admissions, attends on some of their own patients, and helps when the senior is post-call or in clinic. The Blue and Green teams admit hospitalist patients, subspecialty patients, and patients with D:\106741209.doc private attendings every day. Whoever hold the admission phone (3-1155) whether it’s the Gold attending, NP, or swing shift attending, decides which team will accept each admission. PICU transfers to the ward team are accepted by the Blue team on Mon, Wed, Fri, and Sun; and by the Green team on Tues, Thurs, and Sat. Phone calls about questions or issues on new overnight admissions are directed to the Blue team attending on Mon, Wed, Fri, and Sun; and to the Green team attending on Tues, Thurs, and Sat. If a patient is already known to an attending, then that attending should be called if important issues or questions develop overnight. New admissions overnight will be divided equally between the Blue and Green team by the nurse practitioner every weekday morning. If the admitting team has talked to one of the attending about a new admission, the patient should be placed on that team. Make sure the CPNP knows about the communication so that the patient can be appropriately assigned. Students should put their initials next to any patient they helped admit and hope to follow so that you know to prioritize assigning that patient to them The nurse practitioner can also choose to give some new patients to the Gold attending each morning. SCHEDULE OVERVIEW DAILY SCHEDULE: 7:00-7:30am: SIGN-OUT from night team to the daytime residents. Please see your patients in the mornings by 9:30am. If you see a kid in the morning you think is ready to go, assist in completing discharge work, and notifying the ward attending well before rounds in order to expedite their discharge. (Please see Discharge section) 9:30-11:00am: WALK ROUNDS: Blue Team starts on Infant/Toddler side A (near room 3634). A medical student or intern presents each patient. If a medical student is following a patient, they will most likely be the one to present. The presentations are typically more complete the first day the patient is being presented (reviewing the H+P) and more focused on subsequent days. When the volume is high, the presentations will need to be truncated and very pertinent. The senior resident takes a leadership role during rounds with their team (directing which patient to start with, listening and commenting on presentations, suggesting management plans, and teaching as time allows). A hospitalist supervises the presentations and management decisions, and teaches during this time. When time allows, the team rounds at the bedside. Invite the parents to come to the door if bedside rounding is impractical due to isolation precautions, double room, short time, etc. These rounds are multidisciplinary. Nurses are included during rounds and should be notified prior to their patient being discussed (you can highlight a patient assignment list and ask the unit secretary or a nurse to call the nurses and let them know that your team will be coming around. Alternatively, a team member can call the RN when the patient before theirs is being discussed—an RN list is at each nursing station). Other key providers (respiratory therapy, social work, case managers) can also be included. Orders can be written during rounds – bring one of the “workstation on wheels.” 11am-12:15: Work/Subspecialty and Private Patient Rounds/Sign-out: Discharge patients, complete notes, do general ward work. Also, if the team has not yet rounded with private or subspecialty attendings, then this should be done during this time; your senior will “run the list” with the team and decide who will call the various subspecialty and private attendings to round on their patients. Sign-out should occur before noon conference for anyone who needs to leave for the afternoon. 12:15-1:15: Noon conference/Lunch. 1:15 -5:30pm: WORK: Take care of cross-cover work on your patients from the morning (follow-up on studies, labs, call consults, etc), admit new patients, discharge patients. Page 2 of 19 6:00 EVENING SIGN-OUT & ROUNDS: Interns give pertinent sign-out on their patients. Convey the specific plan for care to the on-call physician. If the IV falls out, does it have to be restarted? Any dietary changes? Try to anticipate problems that might arise. You can also outline these in the orders; the nurses often like more detailed information since it makes it easier for them to know what to do. If you are at home and remember something about a child or want to make sure things are going OK call the ward or admitting doc (413-1155 all the time). Subspecialist patients that are not followed by residents in the day, but will be covered by residents at night, will be listed as “FYI” patients. The attendings for these patients will give comprehensive sign-out directly to the night team after team sign-out. See subspecialty section below for more details. EVENING WALK ROUNDS: It is expected that the senior/hospitalist, intern and student will do walk rounds with the charge nurse at night, about 10pm or so to review issues with all the children. A lot of questions can be dealt with then, decreasing night phone calls to the intern. Unstable children can be assessed as well, and other calls made or a transfer to the PICU, if needed. WEEKEND SCHEDULE: On the weekend, the post-call team divides the entire census and pre-rounds on their patients prior to 8am. The goal is to know the status of each patient and be able to signout the pertinent details and work that needs to be done. Labs and vitals should be reviewed on every patient. Patients should be examined or checked on. Notes are not a priority and do not need to be written on every ward patient and Kartini patient. Subspecialist and private attendings like notes written on their patients since they may not see you in the morning, so the note is a good form of communication with them. If you have time (census is very low), go ahead and write notes on ward patients; otherwise, only write notes if you need to convey something about the patient to the ward attending (a significant event, significant vital sign change, etc). The weekend call team arrives at 8am for sign-out. The post-call team should come to the call room as close to this time as possible, briefly update the list, and sign-out. Unlike weekday morning sign-out, the weekend team may know NOTHING about the kids on the service. You must give introductory remarks before giving overnight events, morning labs and VS and the day’s “to-do list.” The on-call team members will then pair up with one of the 2 ward attendings to complete work for their patients. The attending-resident pair will “divide and conquer” the work that needs to be done for all of the ward patients for the day. New admissions or issues that need attention for non-hospitalist patients may take priority, just communicate with your attending and keep checking in with them throughout the day. WORK HOURS: No intern will work more than 16 hours at a time or 80 hours in a week. No senior resident will work more than 28 hrs at a time. Residents will clean up loose ends and sign-out efficiently in order to leave the hospital promptly. If you are working more than the above, please talk to your senior resident or to Dr. Rose so that we can resolve the issue. INTERN CALL SCHEDULE: When you are on night float M-F, come to the call room promptly at 6pm for signout. You will leave on weekdays after signout at approx 7:30am. Saturday morning signout starts at 8am. After your Friday night call, you will pre-round on the Blue team (or ½ the patients overall), and leave after signout. If you are on call Saturday night, signout starts at 6pm and you will leave after prerounding and signing your patients out Sunday morning at 8am. If you are on call Sunday night, signout starts at 8pm. You will stay and round with the team Monday morning and leave the hospital by noon. Page 3 of 19 OHSU PL-1/FP RESIDENT RESPONSIBILITIES: Welcome to your intern pediatric experience at Emanuel. You will be the primary responder and caregiver to the inpatients assigned to you. This includes doing the initial history and physical, writing orders, performing diagnostic procedures, writing daily progress notes (even if the attending or student has already written one), arranging discharges, and typing discharge summaries. The senior resident, nurse practitioner, and each attending are resources for you. On the Blue team, the senior resident, is your medical supervisor in addition to the attending for each patient. It is important to remember that the senior resident and any hospitalist or subspecialty attending on the floor can help with a patient who is decompensating. You will have the best experience if you make proposed management plans early and follow through on plans before the attending does it. Text message your attending if things should get done before rounds. You will receive a packet from the graduate medical education office on the first day of your rotation that includes important information for your successful rotation here, including computer log-on codes, meal tickets, dictation codes, etc. The graduate medical education office is located on the fourth floor of the hospital in room 4123 in the southern most wing. Interns will do one week of night shifts and approx 3 weeks of day shifts with a couple weekend night shifts. Any schedule requests/conflicts should be discussed with Dr. Lauren Rose (lrose@lhs.org). Nighttime responsibilities are similar to those during the day except you will be the primary responder to all the patients on the service, not just your assigned patients. You will be expected to teach the medical students based on the experiences you had as a medical student yourself. This mostly involves teaching the basics of H and P's, writing progress notes, writing orders, etc. OHSU PL-2 RESIDENT RESPONSIBILITIES Welcome to your senior resident experience at TCH. Please re-read the entire orientation as things may have changed since you were here last. Your primary responsibilities are supervising and teaching the interns and students on your team. You will teach the fundamentals of pediatric inpatient care and the strategies that you have learned to make your work more effective and efficient. Your role includes supervising the interns and students during admissions, discussing differential diagnoses, assisting interns with management decisions, ensuring that medical orders are correct, helping interns and students prioritize their work, and leading rounds with your team. Your daily schedule: 1. Morning: Arrive by 7am: The nurse practitioner will distribute the new patients that were admitted overnight between the teams. Assign patients to residents and medical students for each team. Residents (if they aren’t on night float) and students should put their initials next to any patient they helped admit and hope to follow so that you know to prioritize assigning that patient to them. The hospitalist patients (patients followed by general pediatric ward attendings) should be split equally based on number and complexity between the Blue and Green teams (unless the Green NP is holding the admitting phone—in this case Green team will have a couple Page 4 of 19 fewer patients). If there is a Gold team, they can follow a few easy patients as well. Subspecialty and private patients can be assigned to either team, but the balance is variable based on the above variables. The CPNP will make all these assignment decisions in the morning and the person holding the x31155 admitting phone the rest of the day will make all assignment decisions. If you feel the need to share some information about the patient distribution, do so gently, remembering that the team assignments are complicated and thankless. No intern should be assigned more than 10 patients. If there are more patients on the lists than the residents can see, the extra hospitalist patients should be assigned to the hospitalist to see by him/herself. Print out a copy of the lists and have someone run to make extra photocopies for the team. 2. 7:00-7:30 have the on call resident/moonlighter and intern go through each list for signout. It is your job to keep people on track and try to make this as efficient as possible. Signout should take about 30 min total. 3. At conclusion of sign-out make sure that all pts have been assigned to residents/students (as census allows) and assign the Blue team (both hospitalist and resident blue team), your team attending, and the appropriate residents to the patient’s treatment team in EPIC. This allows RN’s and consultants to know who is following each patient. To do this, right click on the patient’s name on the unit list and select treatment team. Add Blue team Resident, and Blue team Hospitalist, and the correct intern caring for them. If the intern’s phone number listed on the treatment team isn’t the actual phone they are carrying, make a comment with the correct phone #. This is how the nurses know who and what # to call. 4. 7:30-9:30 Let attendings know about any concerning patients or patients that don’t seem to be as billed. Also let them know about probable discharges. Help with admits/discharges, especially the discharge paperwork. Help coordinate care for patients by calling consults, calling for lab results, etc. Look through labs and vitals. Try to see as many patients as possible (but in a supervisory fashion), prioritize the sickest kids and kids with respiratory problems. Don’t look in patients’ ears for the 4th time. Listen to the lungs of the respiratory kids, look at cellulitis, do an abdominal exam on kids in pain and with ongoing emesis, etc. 6. 9:30-11:00/11:30 Rounds: walk rounds with your team. Blue team starts on Infant/Toddler Side A. Take a leadership role on rounds. Tell your attending where you’d like to start. We try to do bedside rounds but this is time-permitting. If there is not enough time to go into all of the patient rooms, pick the patients who are most interesting or have the best exams. Invite all of the parents to join rounds at the doorway if time, privacy or infectious isolation prohibits bedside rounds. Ideally, the patient’s nurse will also join rounds. Unfortunately, it’s hard to get each nurse to rounds. There is a nursing assignment sheet at each nursing station with their phone numbers listed. You can highlight your patients on the list and ask the unit secretary or any free person at the desk call the nurses ahead and let them know you’re coming around. Alternatively, you can have a team member call the nurses before we reach their patient to notify them that we are rounding on their patient. This is time consuming, disruptive and has a low yield. Page 5 of 19 Your job is to listen to each medical student or intern present, ask probing questions, think about each case, and suggest or agree with a management plan. The attending will supervise you and make the final management decisions. These rounds are intended to include teaching by both the attending and senior resident. There is often only time to make small teaching points, so we will schedule separate noon conference teaching time for you (see below in 12:15-1:15 section). You should be aware of the time, and keep attendings on track so that you finish by 11 or 11:30am. 7. 11:30am-12:15: Your team should round with subspecialty/private attendings. If this is done at a separate time, then you should “run the list” now as a whole team on these patients so everyone is updated. You supervise the interns during this time, commenting on management of these patients and helping them implement the attending’s plan. This is also time for discharges, calling consults, other ward work, and sign-out for those who are leaving for the afternoon. When you, the senior, are gone in the afternoon, you should sign-out ward kids to your attending and the subspecialty kids to whoever is holding the 3-1155 phone (often the NP before 1). 8. 12:15-1:15: Noon conference in the 3rd floor conference room. All residents are expected to be there unless they must leave for clinic or are post-call. We will reserve at least one to two conferences each month that can be used as informal senior teaching time (see noon conference schedule in conference room, or one of the NPs or attendings will notify you of these dates). 1 of these conferences can be used for medical student presentations. These should be short (5-10 min), informal talks relating to a patient they’ve seen. Your or the attending can suggest a topic for this. Your role is to listen, comment, and provide informal teaching points that complement their talks. The other noon conference is free for you to do whatever type of teaching you think would be valuable to the team. You are not expected to create a formal didactic lecture, though certainly, you may do so if you wish. You could discuss interesting patients you’ve seen that week, talk about a specific topic that interests you, teach students how to give effective presentations…anything is acceptable. There are great teaching materials on the v-drive in the peds_resi folder, then in the education folder; feel free to use these. There is even a Jeopardy game you can use if you wish. 9. Afternoons: In 2011, we added an attending shift called Swing Shift. This person holds the admitting x31155 phone and works from (roughly) 1 – 11 pm. Communicate with the Blue and Gold/Swing Shift attendings about what patients are coming and going. Your Blue attending will get transfer phone calls from the PICU; the Gold/Swing shift attending will get all other admission phone calls. Divide up the PICU transfers and admits already on the floor. Encourage students/residents to take care of cross-cover/ follow up on their patients. This is a good opportunity to teach and to observe students doing admissions. If you had two admissions at once late in the afternoon, and you have one intern, you could eyeball both kids, then have the intern do one admission while you see the other. In addition, remember the ward attending and often the Gold/Swing Shift attending will also help with admissions. Make your team availability known to the Gold/Swing Shift attending so that they will include your team in the great afternoon admissions. Don’t let them forget you! If there is a Gold attending, they sign out to the NP or swing shift attending at 4:30. 10. Sign-out: It should begin promptly at 6:00 with Green team signing out first. Please encourage interns/students to place patients/take patients off both lists as soon as they are admitted/or have left the hospital, so the list is up-to-date at the time of sign-out. Remember to save the list EVERYTIME you make a change. Page 6 of 19 Please try to have the interns (or you) touch base with their attendings before this time so that sign-out is not interrupted by attendings coming to give updates on their patients. If this hasn’t happened and an attending still have information to pass on to the team, you can kindly ask the attending to wait until after sign-out to give further updates (we have instructed them to do this, but sometimes a gentle reminder is needed). They can leave the hospital and call the nighttime senior after sign-out. The NP or an attending who has taken the admission phone calls will start sign-out by quickly telling the night team about the patients that are coming. Then the interns give brief sign-out about their patients. Radiology Rounds: We have radiology rounds most Thursdays with Drs Marten / Gilmore from 11:4512:15 in the 3rd floor conference room. It helps if you have been thinking of cases to review during the week. If the radiologist is late, page Dr. Marten at 503-938-1035 or call radiology at x32527. Triage phone calls/admits: All admissions should be triaged by the senior resident, pediatric hospitalist, NP, or moonlighter. When the senior resident takes admission calls, they should conference their moonlighter or the staff who is supervising them. Typically, the senior only holds the phone while they are on call. The moonlighting attending can hold the intern phone. See the “Phones/Pagers” section for more details. You should call the charge nurse 3-1147 (Infant/Toddler) or 3-1148 (School age) with every admission. The charge nurse should be notified of the isolation needs. If the phone call does not come through the transfer center, you will need to notify bed control at 3-2175 as well. If a phone call comes through the ED or “One-Call,” bed control has already been notified. The severity of illness, nursing acuity, and isolation requirements of the child should be assessed immediately. If you are not sure whether the child should be admitted to the ward or ICU, you should confer with the charge nurse, ward attending, or ICU attending regarding staffing or care needs. If there are questions of transport safety, contact the PICU attending. You can sometimes get them in a conference call for this with the admitting doctor or clinic. We have a children’s transport team called the “KIDS team” (equivalent to PANDA at OHSU) that the PICU can dispatch for sicker kids. See “Talking Points for Taking Admit Calls” in the Peds Resi drive, Orientation folder in the call room computer. If the pager says 812, dial 812 on the phone, and you will be immediately connected to a person holding for you. This is almost always an admission, so please answer in a professional manner, such as “ Hello, this is Carrie Smith, pediatric admitting resident”. Ask appropriate questions to determine the acuity of the patient. For example, ask for the BP, other vital signs, and cap refill in a patient who might be septic. Or, ask for the respiratory rate in a child with asthma. Do they need transport via ambulance or our transport team? Do they need isolation? Your job is not to block admission, but we want the kids to be safe and arrive on the floor stable (and on the best service for their problem). If you have questions/concerns about a patient who sounds sick, please ask, the ward attendings, the PICU attendings, or the Charge Nurse. If you feel like you are accepting an inappropriate admission, please call someone. For the most part, we don’t except traumas onto our service--with rare exceptions, they usually are on the trauma or peds surg service. If you don’t feel comfortable with a transfer, call the attending, or consider ED to ED transfer. Another example is a kid who is a r/o acute abdomen coming in for eval or for observation from the outside (clinic or ED). They should almost always start in our ED as it is much easier to get studies and a surgery c/s down there, and then they get admitted to the proper service. Another example, would be a private attending wanting to send in a lethargic, febrile 4 d/o for a r/o sepsis work-up straight from home as a direct admit, but you have 6 others on the way, it would be safer for the baby to go through the ED first. Page 7 of 19 Please think about kids who might need to be NPO, ex: kid with abscess in arm, kid who aspirated foreign body, kid who needs a sedated MRI, and tell the person sending them to make them NPO. This will save a lot of hassle. Also, call ahead to MRI/Sedation services before they get here. This takes a lot of practice. Please ask a lot of questions. Try to anticipate problems. We have an admission sheet that includes all of the information that you need to obtain for each admission, including name, date of birth, referring doctor, admitting doctor, brief history, and any infectious control measures that we should be aware of prior to the child coming into the hospital, e.g., pertussis, rotavirus, meningococcus, etc (see isolation section). It is also helpful to get the name of the referring physician and a phone number. Additionally, please identify the primary care giver and their phone number. After completion, these admission sheets should be stacked in the call room cupboard. One important detail about admissions: you must CONFIRM who the admitting attending is. If the patient has a physician who admits here, he or she must be contacted and agree to accept the admission before the child is accepted to the pediatric service. You may not know if a doctor admits here or not and you may need to call the private attending and confirm that they know about the admission and that someone from their office will round on the patient in the morning. Take the time to know who the attending actually is. If the official attending is a private pediatrician, they should be called after admission (unless ED doctor said that doctor said there was no need to call), and for all changes in plan, significant clinical changes or events, and always before discharge. For the most part, only East Portland Pediatric group (Davis, Matthieu, Skau, Sequeira, Stillwell, Zimmerman) and occasionally Sunset pediatrics (DeVoe, Ericksen, McCloskey, Snyder) admit their own patients. Also, Metropolitan Pediatrics offices on the Eastside (Clackamas and Gresham) want to be called directly and notified after one of their patients is admitted to the hospitalist service. They will not be attending on them, but like to be updated after you’ve seen them. Every PCP should know that their patient has been admitted to our hospital. If the ED has not already discussed the case with the PCP, please call and leave a message for the PCP that their patient has been admitted to Emanuel. Admissions of patients whose physicians do not admit here go to the hospitalist service. Know who the admitting hospitalist is when you are on call. In general, the hospitalist does not need to be notified of routine admissions at night, but is available for consultation. They should be notified for any questions you have about management, sick patients, patients who have a significant change in clinical status (including patients who might need to go to the PICU!) patients whom you think need subspecialty involvement at night, etc. PICU Transfers: the PICU attending will call the admitting hospitalist directly to transfer a patient. SPECIAL CIRCUMSTANCES Methamphetamine exposures: If you get an admit call about accepting a kid who may have had a methamphetamine ingestion/exposure they should get referred directly to our ED as there is a very elaborate procedure used for these kids (involving in evidence collection/chain of command), so unless the ED sending the kid has the workup completely done, the child needs to be transferred to Emanuel ED. Any questions or problems with this should be directed to the attending. Psych Admits: We do not accept medically stable psych patients from any ED except Legacy hospitals (Good Sam, Salmon Creek, Meridian Park, Emanuel, Mt. Hood). (i.e 15 y/o girl thinking about hurting Page 8 of 19 herself, but is medically stable and awaiting psych bed could only be accepted if she is from a Legacy hospital and once we have a sitter arranged if appropriate). Call Caremark (x34848) prior to admitting a psych patient if there is any question about whether it’s a patient that we should accept. A patient who does not have a medical indication for admission should only be admitted to the acute peds unit if they are coming from a Legacy ED AND the psychiatrist on call expects that they are a candidate for inpatient psych admission once a bed opens up. Do not admit the patient if the psychiatrists have not been queried or don’t think the child qualify for admissions. ICU admissions should be admitted and managed entirely by the intensivist. Sometimes, a child being transported is found to be stable by the transport team and will be diverted to the acute peds unit (and not go to the PICU). The PICU attending should call the admitting phone to give the details. Call the charge nurse (x31147 or x31148) and One Call to give them the new information. Suspected Abuse Patients: in general any patient with suspected sexual abuse should be evaluated in our ED. Patient with suspected physical abuse can be admitted directly to the floor depending on the circumstances. Our CARES doctors will be consulted on these patients. If this admission happens at night, call your attending with any concerns. There is always a CARES social worker who is on call for the ED at night if there are immediate issues that need to be addressed. Surgery Patients: We do not admit surgical patients. Trauma Patients: Trauma patients are on the surgical service until specifically transferred to either the rehab service or the pediatric service (with a private or hospitalist attending as the supervising staff). If you receive a phone call from the ED about a patient who sustained a trauma (ie: head injury) and needs to be admitted, ask them if they were seen and evaluated by the trauma team. The trauma team or peds surgery is usually the admitting service for these patients. Talk to your attending if you are getting pressure to admit a trauma patient. Sometimes it’s appropriate to observe these kids on our service. Hyperbilirubinemia Admissions **Please call ward attending for any ward hyperbili admits** Please get the following information as soon as possible: Prenatal info: [ ] Mother’s blood type, [ ] antibody screen Perinatal info: [ ] Birth time [ ] gestation [ ] baby’s blood type & Coombs [ ] perinatal asphyxia, infection, bruising Postnatal info: [ ] T bili levels & the baby’s age in hours at each draw [ ] Direct Bili **At the time the first call is received, assess risk based on bili level, current age, and any risk factors. If the baby is near or above the line on the exchange transfusion graph, contact the NICU attending and peds attending to discuss the possibility of direct admit to the NICU. Warn family, if possible, that this is the plan. If our NICU is full, consider admission to our PICU or some other NICU in the city. If the floor if pretty crowded, especially with viral kids, consider admission to the nursery. **Regardless of the outside bili level, if the child is admitted to the ward, draw total bilirubin upon arrival and send Stat, as it may be significantly higher than the outside bilirubin level. Exchange Transfusion Guidelines, Pediatrics, 2004: Page 9 of 19 TEAM RESPONSIBILITIES FOR SELECTED PATIENTS HEMATOLOGY/ONCOLOGY PATIENTS Residents do not formally follow routine chemotherapy patients, patients with brain tumors, or palliative care cases. Pediatric residents will continue to follow all hematology cases, but no longer follow new diagnosis cancer patients or patients with fever and neutropenia. However, they will still be responsible for nighttime and weekend coverage of these patients. This includes admissions, and some questions from nurses. The heme-onc attendings will therefore notify the team of any new daytime admissions and updates on their patients which well be kept as “FYIs” on the patient list. They will sign-out their patients to the night team every day around 6:30. Family practice residents will have the option to continue to follow new diagnosis and fever and neutropenia patients, especially if they admitted the patient overnight. They can follow 1-2 of these patients at a time, for up to a week typically, unless they have interesting educational value beyond that time. OTHER SUBSPECIALTY PATIENTS Pediatric residents will not routinely follow new onset diabetics (family practice residents will still have the option of following these patients). No residents will routinely follow trach/vent patients on the pulmonary service (they will be followed by residents if they are on the hospitalist service), video EEG patients, cardiology, or routine cleanout or PEG placements on the GI service. Other GI patients, renal, pulmonary, neurology, rheumatology, infectious disease, and Kartini patients will be followed by all residents. Residents will continue to cover all medical pediatric patients at night and on the weekend (with the exception of cardiology and rehabilitation patients). These subspecialty patients will be listed as “FYI” on Page 10 of 19 the list. Residents will not see them or write daily notes, but nurses will still call the residents on nights and weekends for problems or questions about these patients. The attendings for these patients will give the nighttime team appropriate sign-out every day. EATING DISORDER PROGRAM/PATIENTS Emanuel has a number of children in the hospital with eating disorders. They will often be on the Kartini Clinic service (Eating Disorder specialists), but will sometimes be on the hospitalist service as well. The detailed standing orders are located on the School Age/Rehabilitation unit / in Epic. Please review them quickly so you will have an idea what the parents are expected to do, know, etc. It is a difficult problem and the Kartini Clinic has a specialized approach. Residents do medical H and P's on the children and follow the medical issues daily in case there are significant problems. You are not to discuss food, weight, body image, etc. after the admit day. Any questions or treatment changes should be discussed with Dr. O’Toole or Dr. Moshtael. If possible, you should try to round with Dr. O’Toole or Dr. Moshtael in the mornings (T, Wed, Thur) on your children to get an idea of the plan for the day or week. A good way to do this is to ask the pt’s RN to call you when one of the Kartini doctors arrives. They dictate the charts at discharge. SURGERY PATIENTS We do not admit or follow surgical patients except if they have asked for a general pediatric consult. This includes patients of Dr. O’Hollaren (urologist), Dr. Lashley (urologist), Dr. Achterman (ortho), Dr. Barmada (Ortho), and Dr. Cuyler (ENT). Dr. Wehby, pediatric neurosurgery, will often notify the pediatric residents about her patients on the floor. These are “FYI” patients. The involvement is minimal- scan the chart, eyeball the child to get a baseline if needed, and put them on the patient list. You do not write notes, “follow” them, or do discharge work for them. The residents may be notified at night if the patient has a significant problem and needs to be seen. If this is the case, Dr. Wehby, her NP, Jenny Hume, or the covering neurosurgeon should be contacted after you assess them. We do not dictate d/c summaries or fill out d/c paperwork on any post-op patients. If the surgery resident or staff surgeon request a formal medical consult, the senior resident is responsible, with the hospitalist as staff. The hospitalist serves as the backup staff pediatrician for medical questions. CODES “Pediatric Codes” are automatically sent by the operators to several pagers at the same time. The team includes the senior, pediatric hospitalist, the charge nurse, the PICU doctor, the peds transport team, the “code” anesthesiologist, the RT supervisor, on-call chaplain, a peds PICU RN, an ED nurse and peds IV therapy. The call is set as an alpha pager and the message is put in “Peds code team to _______ location.” It is also called overhead to the code location. The page itself has the same tone as all pages. Remember that the senior resident pager (830-4501) and the intern pager (830-4505) are code pagers, so look at all pages immediately when thesepagers goes off. The hospital policy is that the most senior pediatric doctor present runs it until an attending level pediatric provider arrives. Starting October 1, 2011, the pediatric hospitalist is expected to be the code team leader until the PICU attending arrives. Any emergency involving a child should be called to the operators as a Peds code, since the medicine residents do not respond to this. Please review your resuscitation meds and protocol periodically. There are PALS code cases on the computers in the intern call room and attending call room. There are also occasional mock codes at Emanuel. You are expected to respond and perform as if it were a real code. Page 11 of 19 ATTENDINGS This hospital admits children from all over the region. A few private pediatricians have admitting privileges here and will manage their patients with the residents/students. If the patient’s primary care provider does not want to or cannot attend, then the patient will go to the hospitalist service which is covered by the Emanuel staff hospitalists. The hospitalist or moonlighter is not the official attending for any of the children whose private attendings have accepted the patient to their service. MOONLIGHTERS Moonlighting pediatricians or hospitalists function as the supervisor of interns when there is no senior on call at night. When a PL2 is the senior resident, a moonlighter or hospitalist is on overnight as well. They are here to help with admissions, staff the admissions to the ward team, help with procedures, answer questions, provide second opinions for all pts, etc. They do not replace the official attending, who should be called for all significant changes (PICU txfr, change in status, need to consult subspecialist, etc) or lab results, problems, consults, etc. CONSULTANTS In some specialties, consultants are in separate practices (including Neurology, ENT, Urology, Gen Surgery, Ophtho). When an attending/PCP asks for a consult, you should ask them if they have a preference. Please ask. If they don’t know, ask the senior resident or hospitalist on service whom to contact. If a private attending wants a consult, someone needs to call, don’t assume they did. As professional courtesy, consults are physician to physician, and not just a written order. PHONES / PAGERS Residents and attendings will carry portable phones. Medical students will not carry these phones; instead they will be expected to wear OHSU pagers or Western students should carry a cell phone. Please continue to wear your regular pager as well and make sure your number is listed at the top of the team lists. Typically, Blue team OHSU peds intern carries 3-1151, SWW FP intern carries 3-1152, Prov resident carries 3-1153; SHS resident carries 3-1154. When there is a second Prov resident, he/she will carry 31154. Green team CPNP carries 3-3324. The senior resident phone is 3-1149. The Blue Team attending carries 3-1156 and the Green team attending carries 3-1157. These two phones can be forwarded to outside numbers such as pagers or personal cell phones. The Swing shift or Gold attending carries 3-1155 (or NP if no Gold). Every Monday morning and Friday morning BEFORE ROUNDS if a new attending is starting on the Blue team for the weekend, the 3-1156 phone needs to be unforwarded from the prior attending’s contct number and newly forwarded to the oncoming Blue team attending’s pager so that the PICU will be able to reach the correct attending for phone calls about transfers. Please work with the NP to ensure this happens. Someone in charge of each team should be responsible for the 3-1149 and 3-3324 phones at all times. These are the official team phones. This is so that any consultant or private attending can easily contact someone from the appropriate team about their patients. Whoever is functioning as the team leader will answer this phone. If they have a personal phone, then the leader phone can be forwarded to their personal phone #. When the senior is post-call they should forward their phone to their attending. Page 12 of 19 The general admitting phone is 3-1155. The NP carries the phone until a Gold/Swing Shift attending arrives on weekdays; and a hospitalist or moonlighter carries this phone at night and on weekends when they are here. The intern on call always carries the 3-1151 phone at night. Other interns forward their phone to the 31151 phone at night. Make sure you take this phone during your call night, and try dialing it to make sure it is not forwarded to another phone. The intern also always carries the 830-4505 pager (a code pager). The senior resident should try to carry the 3-1155 phone and conference in their moonlighter for admission phone calls. The moonlighter should carry the 3-1149 phone. The senior also carries code pager 503-830-4501. The portable phones work most of the time on the floor, but are not reliable on other floors or in the Friday case conference room. Please replace your batteries if they are low. To forward the phones: turn on, dial *22, then the number you are forwarding to i.e. 3-1151. To un-forward the phone: turn on, then dial #22. Please check that this is done correctly. Also, please remember to un-forward your phone every morning. If your phones are not working, call 5-5888 and get help or a new phone from telecommunications. CONFERENCE CALLS: This is convenient to do when you need an attending to listen in or want to conference in a subspecialist, moonlighter, etc. Hit "Conf" button on large desktop phones or the tiny conf “dot” on the portable phones. The first party is on hold. You now have a dial tone. Dial the next number normally, including long distance, When the person answers, ask them to hold on, and hit "Conf" again. You are now on line with the original party and the new one. You can get up to 6 (six) people on the same call. TO TRANSFER CALLS: Hit “Transf” (one side of a small button on the mobile phone) Dial the number you want to transfer the call to Then hit “Transf” again EPIC Please call the EPIC help line at 5-5888 your first morning at The Children’s Hospital after signout. They will send someone to help you set up your EPIC preferences and give you a brief orientation before you pre-round. ADMISSIONS Admission H+P may be typed into EPIC, or may be dictated. Medical students have been instructed to type H+Ps on patients they plan to follow. The resident needs to write a separate note and have it cosigned by whichever attending is “staffing” it with them. This will likely be their attending or the Gold attending during the day, and the moonlighter at night. Page 13 of 19 Be a good Epic citizen: put the correct PCP into Epic, fill in the surgical and history elements, update the problem list, do a good medication reconciliation, etc. If you are having trouble finding the PCP in Epic, you might have the wrong spelling. Ask the family for the provider phone number and call the number and ask for the spelling of the provider name. There is a pink phone book on each unit called the Hospitalist Resource book. You can take the book into the patient room (if the child is not in contact precautions) and show the family the various clinics and practice lists. They often recognize their provider. If the provider is truly not in Epic – you can sometimes just list the county clinic. Ask the CPNP how to add a provider to Epic so that we can keep a very comprehensive list. Please begin evaluation and therapy as soon as possible. Try to anticipate what will be needed – e.g., bili lights for a baby admitted for jaundice, an IV and a purple and red top tube for a severe diarrhea, and MDI or neb for a known asthmatic. The long delays between office visit and initial medical therapy are frustrating for parents and physicians. We recognize this is often difficult, but it is possible with communication and planning. Our goal is to have the basic orders written on a patient within 40 minutes of their arrival. For most families, acute hospitalization is a major event in their life and they expect something to be done quickly when they arrive. The charge nurse may want to place an IV, draw blood, give a fluid bolus, etc. immediately. It is best to let them get started with this since they may have another admission coming. After the initial evaluation by an intern, the plans should be discussed with the senior first and then the attending or moonlighter. When an attending is notified of an admission, interns should have a timely two-way conversation with that attending to discuss the assessment and plan. Provide the parents with the team structure : Attending------------------Consulting Attending (if applicable) I I Senior Res/NP Resident I Intern I Med student Nursing needs: The nurses may not be able to staff a child on the ward if they need a lot of care. They know the staff availability and expertise. They may request or demand that the child be placed in the ICU. This should almost always be honored. This should be discussed with the family, private doctor and ICU team. If the private physician disagrees with this assessment, (s)he must discuss it personally with the charge nurse or nurse manager. A conference call with the attending , the charge nurse and the Intensivist may be needed. If the child is ill enough to be moved to the PICU, the Intensivist takes over responsibility, but each case is different and this should be discussed also with all parties. WAYS TO STREAMLINE ADMISSIONS 1. Before going to admit a child, look through EPIC at any prior documentation.The ED physician’s H and P is often there immediately now, and gives a lot of the info we need to ask. You can start filling in your own H and P from this. Notes from our peds clinic are in here also. 2. Look for papers sent with the child from another ED or clinic, etc. It may contain a lot of information. Page 14 of 19 3. Try to coordinate with the nurses if you can take the history with them; they ask a lot of the same questions we do. Note that they need to know some things we don’t in order to complete their admission so you might help them do this, or let them have a minute to ask this during the history, then they can begin getting vitals on the child while you continue with your history. 4. Tell the parents when you introduce yourselves that you have spoken with their doctor, reviewed the records from the ED or clinic, etc. to get acquainted with the child’s problem, but need to review other details or get some additional information. Like when the dentist says, “I’m sorry but this will hurt a bit”. At least saying “I’m sorry” first conveys some empathy! This is not the classic “medical student H and P approach,” in which everything has to be obtained firsthand, but this is an outdated approach that is not necessary for a lot of information and irritating to the people we are trying to help. Be very careful when asking about allergies. If there is one thing to ask repeatedly, maybe this would be it. ORDERS Order set templates are available in EPIC, please use them routinely. Type ip peds to search for them. Please assign the attending of the day to the pt if pt admitted overnight (Blue on M, W, F, Sun; Green on T, TH, Sat) Observation vs. inpatient status: If we are mostly watching to see how the patient evolves, rather than providing specific care (oxygen, IVF, antibiotics), we should admit the patients to observation status. If we can justify doing “stuff,” the inpatient status has a better reimbursement rate. Isolation: Any proved or possible tuberculosis, varicella, measles, or SARS cases, must be in the special negative pressure isolation rooms. There is only one true TB/SARS high neg pressure room on the floor on the adolescent side, and any case with possible active pulmonary TB or SARS must be wearing a mask and be admitted into that room immediately. If you are not sure, isolate them, call the on-all infection control coordinator or ID consult, then discuss the diagnosis. SARS masks, N –95, are available when needed as well as a vented hood for those with facial hair. Common isolations: contact isolation (gloves as entering the room, gowns if your clothes will touch ANYTHING in the patient’s room) for RSV, croup, diarrheal illnesses, varicella, enterovirus in young children, lice, scabies, primary herpes etc; droplet isolation (surgical mask as you enter the room) for influenza, mycoplasma, bacterial meningitis, pertussis, strep; droplet and contact: adenovirus in young children, respiratory illness when you’re not sure (ie: viral vs. mycoplasma vs. pertussis), meningitis when you’re not sure (enterovirus vs. meningococcus) ****** Anytime you touch anything moist: patient’s mouth, diaper, wound, blood, CSF etc – you should be wearing gloves. We have laminated isolation signs on each door that list the organisms and indications on the back. Suspected swine flu cases, require droplet and contact isolation with the door closed to their room. N95 or PAPR masks should be worn if suctioning, intubating, or otherwise getting close to their secretions. Family members with a cough should wear a mask when they leave the room. Monitors/BP checks are often used unnecessarily. Do not use continuous monitors unless really needed for small infants (< 3-6 months old, perhaps) with true apnea risk or for children with rapidly Page 15 of 19 changing O2 needs, etc. Spot checks with vital signs is generally fine, and most children do not need monitors hooked up while awake. Also think about how often each child really needs a BP, often q12 is fine. Tell the nurse about most orders even if they are routine, and definitely notify bedside or charge RN about STAT orders. REQUIRED ELEMENTS IN YOUR NOTE All notes and orders must include date and time of service—PLEASE WRITE THIS INTO YOUR NOTE in EPIC—legible name, professional title (M.D. or D.O.) and year of training (PGY-1, PGY-2, etc.). This is a legal requirement for charting and is reviewed continuously. Verbal orders must be co-signed within 24 hours. They appear in your in-basket. PICU TRANSFERS When a patient is deemed to need a higher level of care in the PICU, the patient’s attending should be notified immediately. The attending or resident should then notify the intensivist or charge nurse about the requested transfer, a brief summary should be written in EPIC about the patient and the reason for transfer, and the transfer orders should be completed in EPIC. If there is not time to complete the PICU transfer summary before the patient leaves the unit, you must type a single summary paragraph stating the change in circumstances that led to the transfer. You can write a more comprehensive PICU transfer note after the patient goes to the PICU. The resident should stay with the patient until they are physically moved to the ICU. When a pt is transferred out of the ICU, please review all orders and write an accepting note. If a medical student writes a note, a resident needs to complete a separate note to be cosigned by the attending. DAILY NOTES Interns and students should examine patients before work rounds and accept their notes in EPIC as soon as they’re done, preferably right after rounds. All patients should have a resident note in the chart daily M-F, even if a medical student or attending does one as well. Resident must always write separate notes whether it is SOAP note, PICU transfer note, H+P, or DC summary. Select an attending to cosign your note and “accept” your note when you are finished. Notes can be pended until then. CROSS COVER NOTES In addition, if you see a child (EVEN if we are not following them) in the evening or make an assessment, it is always best to write a brief note regarding that encounter to document what you did or thought. In general, “If it is not documented, you didn’t do it”. Example: Peds Cross-Cover note: Called for seizure. Nurses report tonic-clonic jerking lasting 30 seconds, w/ no desaturation, self-resolved. Upon my arrival, patient appeared normal. T:37.6, P:120, R:26, BP:100/46, SaO2:99% RA, Babe interactive happy, NAD; CV/Resp/Abdomen: nl; Neuro: MAE, good tone, DTR’s symmetric; Discussed patient w/ Dr Pohowalla who is covering for neurology, felt episode consistent w/ patient’s known seizure d/o and recommends loading w/ 15mg/kg fosphenytoin and stopping future seizures w/ ativan as well as checking Dilantin level in am. Discussed plan w/ nurse and mother. DISCHARGES Discharge planning should be made as early as possible to allow the nursing staff to plan admissions. Discharge summaries can be started DURING the admission if it is a patient that you expect can go Page 16 of 19 home the same or next day. The nurses must know who is definitely going home by about noon, which is the latest time they can cancel requests for evening nurses. Orders for medication and follow-up appointments should be written for the definite discharges before rounds if possible and immediately after rounds before noon conference otherwise. Ward attendings should be notified as soon as possible about potential discharges. Then they might be able to see and discharge them before rounds. Do not wait until rounds to plan for discharges. Discharged patients should often have follow-up with a clinic physician or a health care provider. When a specific follow-up appointment is made, make the appropriate notation in EPIC. All important information should be communicated on the discharge summary please use .resdc template or another good peds dc summary template for your notes and “share” them once you’ve started them. Once you’ve completed them, notify your attending, but you can continue to “share” them. For ward, patients PCP communication is usually done by the ward attending. Children from our well child clinic (located across the street) or one of the county clinics, are at special risk of not returning. A PCP should be personally notified about the return visit plans; this may be done by phone call or fax from the ward. Our clinic docs will automatically receive an in-box notification of the admission / discharge if they have been correctly identified in Epic. They do not need a separate call or note if things are pretty straightforward. DISCHARGE SUMMARIES *** A few notes on DC summaries: The final diagnosis is the reason the child brought in for his/he symptoms – the unifying diagnosis for the initial admission (examples: a vomiting child had rotavirus gastroenteritis or viral meningitis). There can be no abbreviations on this line. Other diagnoses might include underlying diagnoses (Trisomy 21) or other things which made things more complicated (dehydration, metabolic acidosis, hypoglycemia….). Procedures performed include IV fluids, IV antibiotics, consults, imaging studies, surgeries, etc. Be as thorough as possible; if a consult was obtained include the name of the consultant Hospital course –one paragraph about course leading up to admit – then info about the admission Discharge exam: if you include a discharge exam with pertinent elements (weight, lung exam, etc), you will not need to write an additional progress note that day. Discharge information - be thorough – appts, meds, pending labs, etc Look at your note and make sure it actually describes what happened during the admission. Sometimes the Epic templates miss the big picture. Every patient who is discharged with the diagnosis of asthma or reactive airways disease is now required to have an "Asthma Action Plan" documented in the record. In the discharge instructions, type .resasthmaplan. This will bring up the asthma action plan template. Look at Ann Loeffler or Sayonara Mato’s templates for a Spanish Asthma Action form which can be pulled into the patient’s after visit summary. The required elements include a SCHEDULED followup appointment date, time, and name of the provider, and the name and amount of controller medication the patient is on. If a specific appointment cannot be made with the patient’s provider at the time of discharge (for whatever reason), there is a default plan for scheduling a specific slot with the Emanuel pulmonologist. Please see the transparent folder attached to the bulletin board in the call room if this is needed. Page 17 of 19 MISCELLANEOUS DRESS CODE Nametag, Professional Dress- no tank tops, or open-toed shoes. White coat encouraged for all students Scrubs only if you are on call or post-call (should wear white coat over them). Wear a blue lanyard to match your team color. If there are no more blue lanyards in the hall outside the call room, have someone ask Ann Loeffler for more (or any hospitalist can fetch them from the box under her desk). CONSENTS/PROCEDURE NOTES The physician performing the procedure must review the PARQ (plan, alternatives, risks, questions) with the parents and have a signed consent scanned in the chart. An LP is the most common procedure for which we use a PARQ. Immediately after the procedure (most commonly LP), write a brief procedure note in the chart. I usually start w/ “PARQ reviewed w/ Mother of child, questions answered.” LABORATORY Most lab results are available in EPIC. Other results can be obtained by calling the lab (send outs). Blood cultures are read automatically every 10 min; positive blood and CSF culture are called to the floor and the ordering physician immediately. It is not necessary to call the Legacy lab for blood or CSF culture results. If you have not heard, they are negative. Most of the other labs are read by the early afternoon. Do not call the micro lab until mid-afternoon – and even this should be very rare. It only slows down their work. If a culture was obtained at an outside laboratory, you will need to call to check on results. Phone numbers for these labs are found in the black “HOSPITALST RESOURCE” binder on each floor. Some tests are sent out to Utah by plane Mon - Fri, and they leave our lab about noon. If it is a special test, try to make sure it gets done and sent to our lab by 11 am or so, in case it has to be sent out. Send out results can be queried at X31234 – Customer service (#1). RADIOLOGY Routine studies are kept in radiology and on the PACS system which is accessible thru EPIC. Outside images that are scanned into PACS can be seen on the PACS system, usually in the “OT synapse.” There are PACS stations in the “fishbowl” (physician workroom) on Infant/Toddler side A, in the PICU, and at one of the computer workstations on Unit 35. We have many radiologists to review films and two pediatric radiologist—Paul Marten and Jim Gilmore. They are located on the first floor of the hospital across the atrium from the Heart Beat Café. Many hospitals have contracted with Legacy to be able to electronically transfer films to our PACS system. Contact radiology if you need this done. PACS: You will need a sign on for the PACS system unless someone has already logged on. The PACS log-in user name is on your grey card w/ all of your codes given to you at orientation. Your initial password is “begin”. You will have access to ALL Legacy hospitals on this. Be sure to select the correct “synapse” for where the study was obtained (Emanuel, Salmon Creek, Mt. Hood, etc.) Ask Angela Cacchioli Graduate Medical Education 3-4656 if you are having trouble accessing PACS. If the patient needs a copy of a film for their doctor, it can be made. Contact radiology. Outside films should be taken to radiology with a patient sticker on them. They will be scanned into PACS. Do not leave outside films lying around on the wards or in call rooms. They will disappear, and then the team will waste a lot of time trying to track them down the next morning. Page 18 of 19 Outside films can be brought to the radiology department to be scanned into PACS. However, if you wish to obtain a formal radiology read, please write an order for this and contact the radiologist. BOOKS, RESOURCES, etc On the v-drive, under peds_resi folder, there is an Emanuel Reading List folder that lists recommended reading and has PDF’s in the folder of the referenced articles. This is a good place to start. There are also several basic texts on the floor next to the charge nurse desk and above the computer in the call room. There are developmental screening forms in the same area. The Legacy intranet homepage has a links to the library page under “clinical resources.” This page then has links to key references (micromedex, Peds in Review, Redbook, etc) as well as a number of journals and OVID search engine. STORING PERSONAL BELONGINGS Never leave valuables, checkbooks or credit cards in an unlocked place. Call rooms are not secure; too many people can access them. Please do not leave food, etc. in the common charting areas on the ward. There are combination lockers on the fourth floor if you would like to use one. Call Angela Cacchioli 3-4656 in the GME office for the combinations. CALL ROOM The call room for the senior resident and the intensivist are outside the PICU, and the intern and student call rooms are on the fourth floor. FOOD Lunches are provided each weekday. Please call Debbie Balchin at x34385 if you do not plan to partake in the cuisine for the month. Also tell her if you have special dietary needs (vegetarian, gluten-free, etc.) although there is no guarantee that all needs can be provided here. If there is a consensus that a certain type of lunch is terrible, please tell Debbie and she will relay it to the kitchen. Residents are given meal tickets for on-call meals. These can be used at the hospital cafeteria which is open Mon-Fri 6am-4pm, or the Heartbeat Café located in the atrium open 24h/day (this is your only food option in the evenings and on Sun). The meal tickets are accepted at both locations. Revised 9/5/11 Page 19 of 19