Fetal Tracing Review
advertisement
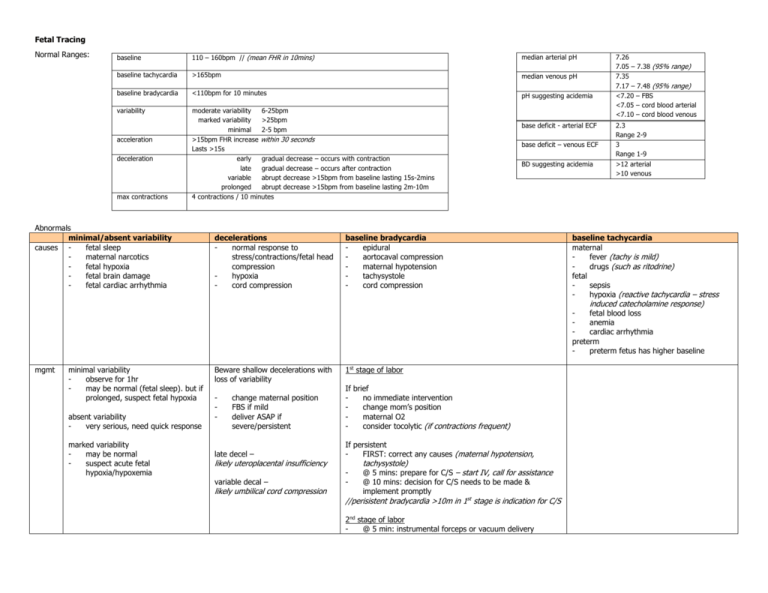
Fetal Tracing Normal Ranges: baseline 110 – 160bpm // (mean FHR in 10mins) median arterial pH baseline tachycardia >165bpm median venous pH baseline bradycardia <110bpm for 10 minutes pH suggesting acidemia variability moderate variability 6-25bpm marked variability >25bpm minimal 2-5 bpm >15bpm FHR increase within 30 seconds Lasts >15s early gradual decrease – occurs with contraction late gradual decrease – occurs after contraction variable abrupt decrease >15bpm from baseline lasting 15s-2mins prolonged abrupt decrease >15bpm from baseline lasting 2m-10m 4 contractions / 10 minutes acceleration deceleration max contractions Abnormals minimal/absent variability causes fetal sleep maternal narcotics fetal hypoxia fetal brain damage fetal cardiac arrhythmia decelerations normal response to stress/contractions/fetal head compression hypoxia cord compression base deficit - arterial ECF base deficit – venous ECF BD suggesting acidemia baseline bradycardia epidural aortocaval compression maternal hypotension tachysystole cord compression 7.26 7.05 – 7.38 (95% range) 7.35 7.17 – 7.48 (95% range) <7.20 – FBS <7.05 – cord blood arterial <7.10 – cord blood venous 2.3 Range 2-9 3 Range 1-9 >12 arterial >10 venous baseline tachycardia maternal fever (tachy is mild) drugs (such as ritodrine) fetal sepsis hypoxia (reactive tachycardia – stress induced catecholamine response) fetal blood loss anemia cardiac arrhythmia preterm preterm fetus has higher baseline mgmt minimal variability observe for 1hr may be normal (fetal sleep). but if prolonged, suspect fetal hypoxia absent variability very serious, need quick response marked variability may be normal suspect acute fetal hypoxia/hypoxemia Beware shallow decelerations with loss of variability - change maternal position FBS if mild deliver ASAP if severe/persistent 1st stage of labor If brief no immediate intervention change mom’s position maternal O2 consider tocolytic (if contractions frequent) late decel – If persistent FIRST: correct any causes (maternal hypotension, variable decal – - likely uteroplacental insufficiency likely umbilical cord compression tachysystole) @ 5 mins: prepare for C/S – start IV, call for assistance @ 10 mins: decision for C/S needs to be made & implement promptly //perisistent bradycardia >10m in 1st stage is indication for C/S 2nd stage of labor @ 5 min: instrumental forceps or vacuum delivery Heart physiology review heart rate determined by o intrinsic heart rate o heart’s nerve supply (vagus) o circulating catecholamines (via adrenal glands) o CNS activity note that these are in turn influenced by o changes in fetal BP o changes in fetal blood gases (pCO2, pO2, pH) Acid/base physiology review fetus uses O2 for glucose production impaired gas exchange leads to o co2 retention o reduced O2 supply CO2 o co2 is a weak acid. if retained, blood pH will fall → respiratory acidemia O2 o if O2 reduced = hypoxemia, fetus adapts well o if O2 reduction prolonged → hypoxia, fetal tissues can’t metabolize → anaerobic metabolism → lactic acid → pH falls → metabolic acidemia o so note: in blood gas analysis, blood O2 may be low, but if the pH is normal, it means the fetus is adapting well and this is reassuring. interpreting 2nd stage tracings decel’s are common. 2nd stage is more stressful for feus. Fetal pH falls more rapidly too mgmt for poor quality tracing o scalp electrode o maternal internal transducer despite decel’s variability and baseline should be maintained Fetal blood gas Fetal blood sample technique mom in left lateral position when is it inappropriate severe tracing – FBS may delay CS 2cm dilation and stable presenting part required 2nd stage – an abnormal tracing in 2nd stage is indication for instrumental delivery, NOT FBS obtain sample from fetal scalp obtain quickly – prolonged exposure of blood to air - allows CO2 diffusion avoid bubbles – again, CO2 diffusion FBS interpretation pH Technically difficult – small dilation/ unstable presenting part Maternal/fetal conditions HIV, Hepatitis (vertical transmission) fetal hemophilia suspected 7.25 = normal 7.20 – 7.25 = borderline; repeat in 30-60min, continue labor 7.20 = indication for delivery keep in mind maternal hyperventilation --> high maternal pH --> high fetal pH may hide a compromise get a maternal venous sample to check if suspected Cord blood gas do you collect arterial or venous blood? Both – arterial better represents fetal condition, but both collected to make sure that the arterial is actually arterial, and not venous arterio-venous difference is usually 0.08 units; <0.03 means likely the same vessel was sampled large a-v difference points to an acute problem (an issue in 2nd stage labor) Analysis – values suggesting acidemia: pH pH-arterial < 7.05 pH-venous < 7.10 base deficit arterial BD-ECF > 12mmol/L venous BD-ECF > 10mmol/L // metabolic acidemia of this degree is associated with higher fetal morbidity low pH & large A-V difference suggests? o acidemia due to acute event, or cord compression low pH & small A-V difference suggests? o acidemia due to chronic condition low pH & very small (<0.3) A-V difference suggests? o both samples are from same vessel Note: base deficit is a measure of how much buffer in blood is used up. The more free acid is being produced (metabolic academia), the more buffers are used up. In respiratory academia, buffer is not being used up (tho it is involved).







