Neonatal Pharmacokinetics and Drug Therapy:
advertisement

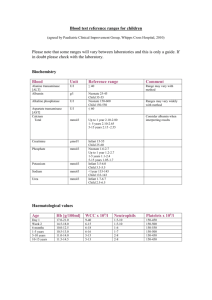
Neonatal Pharmacokinetics and Drug Therapy: (1-13) 1. Gestational Age Postnatal Age Preterm Term Neonate - # weeks after mothers last menstrual cycle age after live birth <38 gestational weeks old 38 – 42 gestational weeks old <1 month of age after birth 2. Parameter Gastric acid production Gastric Emptying time Intestinal motility Intestinal permeability Intestinal surface area Biliary function Microbial flora Neonate Infant Child N N + irregular irregular N immature immature N ? N N N N N (+) prolonged, (-) reduced, (N) normal 3. Increased absorption through the skin compared to adults. - increased BSA to body size ratio (3:1 neonate) - thinner stratum corneum - increased skin hydration Iodine – thyroid dysfunction and abnormal growth Hydrocortisone – can result in Cushing’s syndrome (hyperglycemia, hypertension, diabetes, decreased bone growth, etc…) 4. Total Body Water Fat Stores Plasma Protein Neonate 70-80% 1-2% less Infant 60% 10-15% ? Adult 50-60% 20-25% normal 5. The staining and subsequent damage of the brain by bile pigment (bilirubin) Caused by displacing bilirubin from albumin sites. Drugs: sulfonamides & ceftriaxone 6. Vd differs Normal Vd (L/kg) Preemie increased 0.5 – 1.2 Neonate Infant increased mid 0.5 0.4 Child low 0.35 Adolescent Adult low lowest 0.3 0.2-0.25 Vd differs Preemie increased Neonate Infant increased mid Child low Adult lowest 7. Neonates need a higher loading dose 15-20mg/kg vs adults 10-15mg/kg 8. Phase I Reactions Neonates: Oxidation – takes 2 - 4 weeks to get to adult values Reduction – present and fully functional Hydrolysis – takes 1 – 12 months to get adult values Demethylation – reduced but present, takes 2 – 3 months till adult values 9. Phase II Neonates: Glucuronidation – limited ability takes 6 – 18 till adult values Sulfation – present and fully functional Glycination – decreased but increases by 8 weeks Methylation – present and fully functional Chloramphenicol – Acetaminophen Morphine Tetracycline glucuronidation, causes Gray Baby Syndrome Sulfation, used till glucuronidation develops Sulfation, used till glucuronidation develops teeth can become permanently stained 10. Do not use for the first 2-6 months or it causes Gasping Syndrome. Benzyl alcohol is a preservative used in some IVs. Cleared by Glycination. 99mg/kg is a toxic level. 11. Glomerular filtration – lower at birth, reach adult values ~ 5 months Tubular secretion lower at birth, reach adult values ~ 12 months Reabsorption lower at birth, increases with age 12. BSA to body size ratio is much higher than adults (3:1) so may get 3 times the level you would in an adult which can be toxic. 13. Bacteremia Systemic signs of infection (ie. temp) Apnea Poor feeding Temperature instability Lethargy Principles of Pediatric Pharmacotherapy: (1-4) 1. Preemie Vd Aminoglycoside increased Vd Phenytoin increased Neonate Infant increased mid increased mid Child low low 2. Get levels after steady state has been reached. Vancomycin: half-life ~ 6hr (ss about 4th dose) Peak drawn 30 min after a 60 min infusion Trough drawn within 1 hour prior to next dose Aminoglycosides: half-life ~ 3 hrs (ss about 3rd dose) Peak drawn 30 min after a 30 min infusion Adolescent Adult low lowest ? lowest Trough drawn within 1 hour prior to next dose 3. If trough to high: If trough to low: If high peak and trough: If high peak and low trough: increase interval between doses (ie. q 8hr change to q 12 hr) increase dose (ie. 25mg q 8hr change to 50mg q 8hr) increase interval between doses (ie. q 8hr change to q 12 hr) decrease dose and decrease interval (ie. 25mg q 8hr change to 15mg q 6hr) Vancomycin Goal: Peak 20-40 Trough 5 - 15 Aminoglycoside Goal: Peak 6-8 Trough <2 4. Drug clearance is unpredictable in peds vs. adults, depending on the age of the child and drug they may have increased clearance or decreased clearance.