EACTA Survey on Transfusion Policy in European Cardiac Surgery
advertisement
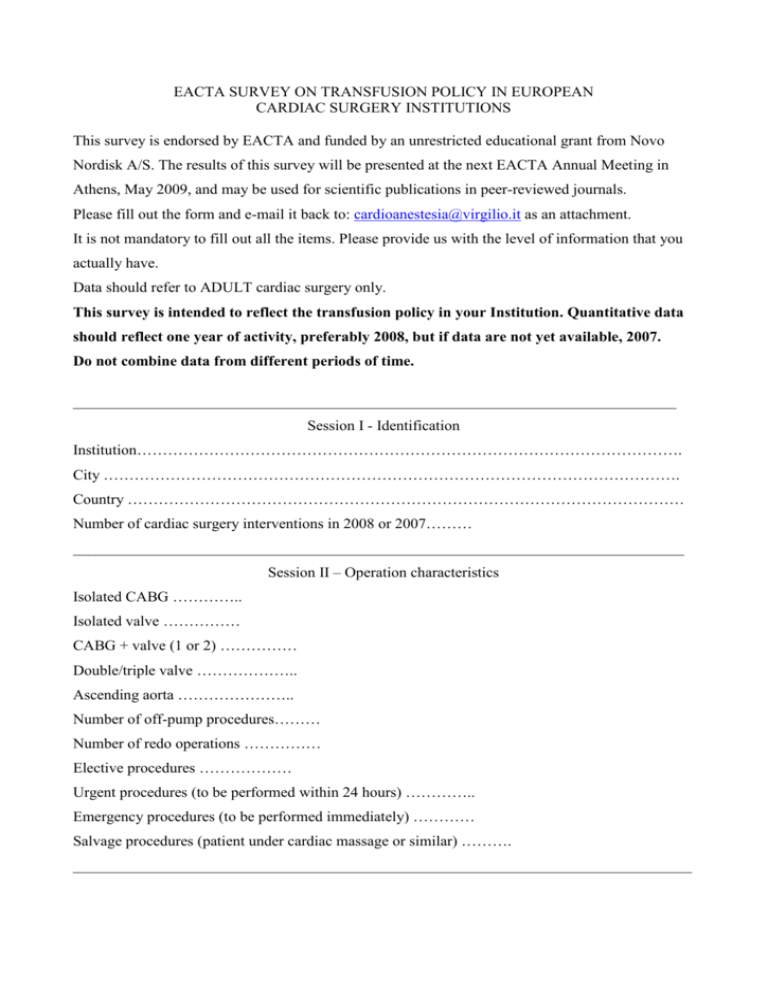
EACTA SURVEY ON TRANSFUSION POLICY IN EUROPEAN CARDIAC SURGERY INSTITUTIONS This survey is endorsed by EACTA and funded by an unrestricted educational grant from Novo Nordisk A/S. The results of this survey will be presented at the next EACTA Annual Meeting in Athens, May 2009, and may be used for scientific publications in peer-reviewed journals. Please fill out the form and e-mail it back to: cardioanestesia@virgilio.it as an attachment. It is not mandatory to fill out all the items. Please provide us with the level of information that you actually have. Data should refer to ADULT cardiac surgery only. This survey is intended to reflect the transfusion policy in your Institution. Quantitative data should reflect one year of activity, preferably 2008, but if data are not yet available, 2007. Do not combine data from different periods of time. ______________________________________________________________________________ Session I - Identification Institution……………………………………………………………………………………………. City …………………………………………………………………………………………………. Country ……………………………………………………………………………………………… Number of cardiac surgery interventions in 2008 or 2007……… _______________________________________________________________________________ Session II – Operation characteristics Isolated CABG ………….. Isolated valve …………… CABG + valve (1 or 2) …………… Double/triple valve ……………….. Ascending aorta ………………….. Number of off-pump procedures……… Number of redo operations …………… Elective procedures ……………… Urgent procedures (to be performed within 24 hours) ………….. Emergency procedures (to be performed immediately) ………… Salvage procedures (patient under cardiac massage or similar) ………. ________________________________________________________________________________ ________________________________________________________________________________ Session III – Patients details Insert absolute numbers in the dashed lines Gender male …………. Age ≥ 65 years ………… BSA ≤ 1.9 m2 …………. Hematocrit < 35% …….. Diabetes on medication ………… Serum creatinine > 1.25 mg/dL ………… Chronic dialytic treatment ……………… ________________________________________________________________________________ Session IV – Preoperative medications Insert absolute numbers in the dashed lines Salycilates in the 7 days before the operation …………………. Tyenopiridines (clopidogrel or ticlopidine) in the 7 days before the operation …………. Oral anticoagulants (warfarin – coumadin) not discontinued ……………… GPIIb/IIIa inhibitors active at the moment of the operation ………………. Subcutaneous LMWH until the operation day ……………………. Intravenous heparin until the operation day ……………………… ________________________________________________________________________________ Session V – Hemostatic drugs used during or after the operation Insert absolute numbers in the dashed lines Aprotinin ……….. Tranexamic acid ………. Epsilon-aminocaproic acid ………….. Desmopressin ………………………. Recombinant activated factor VII ………… ________________________________________________________________________________ ________________________________________________________________________________ Session VI – Packed red cells (PRCs) transfusions ________________________________________________________________________________ Number of patients receiving PRCs ……………… Number receiving 1 –2 units …………………….. Number receiving 3 – 4 units ……………………. Number receiving > 4 units ……………………… Number being transfused during the operation …………… Number being transfused after the operation ……………. ________________________________________________________________________________ Session VII – Fresh frozen plasma (FFP) transfusions ________________________________________________________________________________ Number of patients receiving FFP ……………… Number receiving 1 –2 units …………………….. Number receiving 3 – 4 units ……………………. Number receiving > 4 units ……………………… Number being transfused during the operation …………… Number being transfused after the operation ……………. ________________________________________________________________________________ Session VIII – Platelets (PLTs) transfusions ________________________________________________________________________________ Number of patients receiving PLTs ……………… Number receiving 1 unit …………………….. Number receiving 2 units ……………………. Number receiving > 2 units ……………………… Number being transfused during the operation …………… Number being transfused after the operation ……………. ________________________________________________________________________________ Session IX ________________________________________________________________________________ Number receiving cryoprecipitates …………….. ________________________________________________________________________________ ________________________________________________________________________________ Session X – Postoperative complications ________________________________________________________________________________ Number of re-explorations due to bleeding ………….. Acute renal failure (creatinine > 2.0 mg/dL AND > baseline value x 2) ………….. Acute renal failure requiring renal replacement therapy ………………….. Thromboembolic events (stroke, myocardial infarction, peripheral thromboembolism, pulmonary embolism, mesenteric infarction) …………….. ________________________________________________________________________________ Session XI – Transfusion policy ________________________________________________________________________________ Indicate the trigger value of hemoglobin (hematocrit/3) at which PRCs are transfused in the following different scenarios ________________________________________________________________________________ DURING CARDIOPULMONARY BYPASS Age of the patient < 65 years Trigger value of Hb for transfusions ………………. Age of the patient 66-75 years Trigger value of Hb for transfusions ………………. Age of the patient > 75 years Trigger value of Hb for transfusions ………………. ________________________________________________________________________________ AFTER CARDIOPULMONARY BYPASS, DURING THE OPERATION Patient male, < 65 years , no major inotropic support Trigger value of Hb ………………. Patient male, ≥ 65 years , no major inotropic support Trigger value of Hb ………………. Patient male, < 65 years , with major inotropic support Trigger value of Hb ………………. Patient male, ≥ 65 years , with major inotropic support Trigger value of Hb ………………. Patient female, < 65 years , no major inotropic support Trigger value of Hb ………………. Patient female, ≥ 65 years , no major inotropic support Trigger value of Hb ………………. Patient female, < 65 years , with major inotropic support Trigger value of Hb ………………. Patient female, ≥ 65 years , with major inotropic support Trigger value of Hb ………………. ________________________________________________________________________________ DURING THE ICU STAY Patient male, < 65 years , no major inotropic support Trigger value of Hb ………………. Patient male, ≥ 65 years , no major inotropic support Trigger value of Hb ………………. Patient male, < 65 years , with major inotropic support Trigger value of Hb ………………. Patient male, ≥ 65 years , with major inotropic support Trigger value of Hb ………………. Patient female, < 65 years , no major inotropic support Trigger value of Hb ………………. Patient female, ≥ 65 years , no major inotropic support Trigger value of Hb ………………. Patient female, < 65 years , with major inotropic support Trigger value of Hb ………………. Patient female, ≥ 65 years , with major inotropic support Trigger value of Hb ………………. ________________________________________________________________________________ THANK YOU !