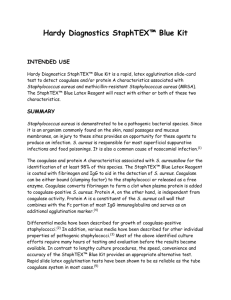
Staphylococcus latex test kit
advertisement

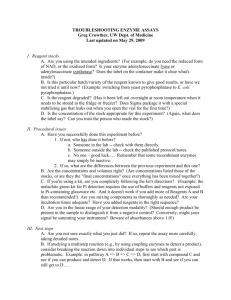
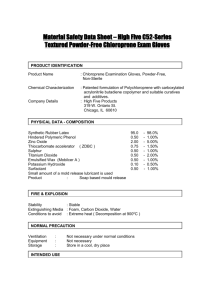
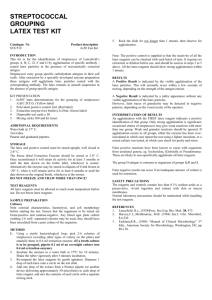
STAPHYLOCOCCUS LATEX TEST KIT Catalogue No STA/010 STA/012 Product description 50 Test kit 100 Test kit INTRODUCTION The Staphylococcus aureus latex test is intended for use in the differentiation of Staphylococcus Aureus possessing clumping factor and/or protein A, from other species of Staphylococci which do not possess these factors. The common method of identification of these species is the plasma coagulase test. There are two distinct factors involved: 1. Cell associated clumping factor which reacts with fibrinogen. The usual test for this is the slide coagulase test. 2. Extracellular free coagulase which activates prothrombin, and in so doing initiates clot formation with the plasma. The usual test for this is the tube coagulase test. In addition, over 95% of pathogenic strains of S. aureus produce protein A, either with or without clumping factor. Protein A has a high affinity for the Fc moiety of IgG. To this end, the S. aureus latex reagent has been designed to react with those species of Staphylococci possessing either clumping factor, protein A or a combination of both. KIT PRESENTATION Each kit should contain the following reagents and accessories:1. Latex test reagent. (Yellow label) 1 x 3.6mls for the 100 test kit or 3 x 5mls for the 300 test kit. 2. Latex control reagent. (Red label) 1ml for the 100 test kit and the 300 test kit. 3. 17 Disposable reaction cards in the 100 test kit size or 51 reaction cards in the 300 test kit. 4. 100 mixing sticks in 100 test kit or 300 in 300 test kit. 5. Product literature. Each latex reagent contains less than 0.1% sodium azide. The test reagent consists of latex particles coated with human fibrinogen and IgG. The IgG and fibrinogen used to sensitise the latex particles have been tested for the presence of H.I.V. and HbSAg and found to be negative. The control reagent consists of blocked latex particles, treated throughout the same as the test reagent, but with the omission of fibrinogen and IgG. STORAGE Store at 2-8 degrees C. Do not freeze. When stored at the recommended temperatures, the reagents should remain active until at least the expiry date on the label. SAMPLE PREPARATION Cultures should be fresh 24hr growths, and may be tested directly from the plate. If there is insufficient growth, sub culture to blood agar base or nutrient agar and incubate overnight at 37 deg C. Organisms grown on high salt media, such as mannitol salt agar, may show signs of stringiness when mixed with the reagents. Any discrepancies can be eliminated by parallel use of the control latex with the test latex. Alternatively, sub culturing to blood agar base or nutrient agar should be sufficient. METHOD 1. Shake the test latex reagent bottle well to expel any air in the dropper tube. Place one drop of reagent in the centre of a 3cm circle on a disposable slide. 2. Using a sterile loop, pick off 2-4 colonies from a fresh overnight culture plate of the organism to be investigated, and emulsify in the drop of reagent on the slide. 3. Rotate the slide gently and observe for agglutination. Do not rotate for more than 1 minute. View only using normal laboratory lighting. Do not employ the use of magnifiers of bench lights. 4. In the case of rough or stringy samples, carry out the above procedure using the control latex and using the same sample culture. RESULTS A POSITIVE RESULT is indicated by the visible aggregation of the latex particles. This will normally occur within a few seconds of mixing. A NEGATIVE RESULT is indicated by a milky appearance without any visible aggregation of the latex particles. However faint traces of granularity may be detected in negative patterns, depending on the visual acuity of the operator. INTERPRETATION OF RESULTS If agglutination with the test reagent occurs, this would indicate the presence of either coagulase or protein A. If no agglutination occurs, this would indicate the absence of coagulase or protein A. In some cases, a culture sample may cause the test latex to appear stringy or speckly, whilst not seeming to be a definite positive reaction. In these instances, the control latex should be used. If the control latex remains smooth (i.e. with a completely milky background), then the sample is likely to be positive for coagulase or protein A. If the control latex gives a rough or stringy appearance, then further biochemical tests may be necessary. QUALITY CONTROL PROCEDURES Periodically check the following: 1. The test reagent agglutinates with a known S. aureus strain. 2. The test reagent and the control reagent do not auto-agglutinate in normal saline solution. LIMITATIONS OF USE Some species of Staphylococcus other than S. aureus, notably S. intermedius, S. hyicus may give positve results in conventional coagulase tests and may also agglutinate latex reagents (1). Rare species such as S. Iugdunensis and S. schleiferi have been reported as clumping factor positive (2). Novobiocinresistance may also give false positive results using latex based tests (3,4,5.). Several species such as E. coli and C. albicans are capable of agglutinating latex particles non-specifically. Organisms that possess immunoglobulin binding factors may also agglutinate latex based reagents. PERFORMANCE CHARACTERISTICS A blind trial was undertaken at the Leicester P.H.L.S. Two hundred and fourteen reference strains were tested. These represented a number of commonly isolated species together with certain rare species. The reagents used in the trial were 12 months old nearing the end of the recommended shelf life. All the strains of S. aureus examined during the study gave the expected positive result. Our kit was considered to be easy to use and the provision of a control was a beneficial feature. The kit was judged to provide a rapid, accurate, easy to read method for detecting S. Aureus in a routine clinical laboratory and was comparable with other rapid slide latex methods commercially available. REFERENCES 1.Philips,W.and Kloos,W.(1981).J.Clin.Microbiol; 14,6671. 2.Freney,J.Brun,Y.Bes,M.(1988)Int.J.Syst.Bacteriol.38,168. 3.Stevens,M,Geary C.(1989).Eur.J Clin.Mic.Inf.Dis.8,153-156 4.Berke A,Tilton R.C.(1986).J.Clin.Mic.23,916-919. 5.GregsonD.B.,LowD.E.,SkulnickM.,Simor A.E.,(1988).J.Clin..Mic.26,13981399. VER1/00STA