Mohamed Ibrahim Abd Elfatah Mohamed_STUDY OF PLASMA
advertisement

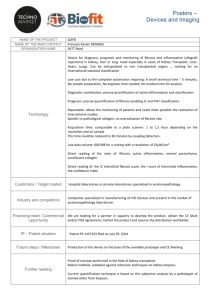
STUDY OF PLASMA OSTEOPONTIN IN PATIENTS WITH RHEUMATOID ARTHRITIS AND SYSTEMIC LUPUS ERYTHEMATOSUS WITH AND WITHOUT EVIDENCE OF LUNG FIBROSIS By Mahmood Alsalahy*MD, Mohammad Hassan**MD, Refaat Altanawy***MD, Anas Yosof****MD, Mohammad Abdelfatah*****MD *Chest, ***Rheumatology, ****Clinical pathology, *****Clinical bacteriology and immunology Departments, Benha Faculty of Medicine, **Internal Medicine Department, Zagazig Faculty of Medicine ABSTRACT: To study the relation of the newly discovered proinflammatory cytokine osteopontin (OPN) to lung fibrosis in patients with rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE), we selected 18 RA patients ( 7 ♂ and 11♀; 29.28 ± 10.42 years ) and 17 (6 ♂and 11♀, 37.7 ± 7.11 years) and 10 normal controls ( 27.3 ± 9.01 years). 7 of RA and 6 of SLE patients have clinical and radiological evidence of lung fibrosis. FEV1 % predicted, ESR, serum CRP and plasma osteopontin were measured. FEV1 % predicted was significantly lower in patients than controls and in those with fibrosis than in those without in both groups (p< 0.001 and <0.05 respectively) while CRP and OPN were significantly higher than in controls (p<0.001 & <0.05 for CRP and <0.001 for OPN respectively). No significant difference seen between RA and SLE patients in all parameters (p>0.05 for all). OPN showed significant negative correlation to FEV1 % predicted and significant positive correlation to ESR and CRP in both patients groups (r = -0.83 , = 0.93 and 0.87 in RA respectively, p<0.001for all, while in SLE, r = -0.66, 0.47 and 0.51 respectively, P< 0.001 for FEV1 % predicted and <0.05 for ESR and CRP). Conclusion : plasma OPN could be a useful marker for disease activity and could predict those who at risk of developing lung fibrosis in RA and SLE patients. INTRODUCTION: Osteopontin, a newly discovered cytokine (OPN, also known as Eta-1) is a phosphorylated acidic glycoprotein secreted by a variety of cells including osteoclasts, activated T cells and activated macrophages(1). OPN contains an arginine–glycine– aspartate (RGD)-binding motif that binds to the integrin family of adhesion molecules and it functions as a proinflammatory cytokine that causes cellular adhesion and chemotaxis of different cell types, such as inflammatory leukocytes and vascular smooth muscle cells(2,3). The potential role of OPN in interstitial fibrosis in different granulomatous lung diseases as well as drug induced alveolitis was elucidated by many authors(4,5,6). We carried out this study to evaluate the relation between OPN and lung fibrosis in rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) which are the two most common collagen vascular diseases associated with lung fibrosis. 1 SUBJECTS AND METHODS: We selected 18 (7♂ and 11♀) RA and 17 (6♂ and 11♀) SLE patients from rheumatology, internal medicine and chest outpatient clinics. We selected patients complaining of dyspnea especially on exertion and who did HRCT of chest to investigate the cause of their dyspnea. Ten of both patients groups showed no evidence of fibrosis (normal or near normal FEV1% predicted as well as absent evidence of fibrosis (ground glass opacity, reticulations and micro nodules) on CT (7), while 8 of RA and 7 of SLE patients showed evidence of fibrosis. 10 healthy subjects of the same age group were selected from patients relatives as normal controls. Full clinical history and examination, revision of CT chest and medications were done to all patients. A recent X-ray chest also was done to all patients to exclude recent lung events developed after CT imaging. Smokers, diabetics, cardiac and renal impairment patients as well as those on steroids or cytotoxic immunosuppressant drugs were excluded to avoid the effect of these conditions on plasma osteopontin levels as well as on erythrocyte sedimentation rate (ESR) and serum C-reactive protein (CRP) the other inflammatory markers to be studied. Patients were only on their ordinary antiinflammatory therapy (8). The following were done to all patients and subjects: 1.Ventilatory function was measured using a pneumotachometer spirometer (MIR, Italy) and FEV1 % predicted was used to measure any present ventilatory defects. 2.ESR measured by Westergren method as mm in the 1st hour. 3.CRP measured by latex agglutination test using Plasmatec UK kits as follows (9): fresh serum was obtained by centrifugation of clotted fresh morning blood samples. After warming of reagents to room temperature a drop of undiluted serum is then put on the circle of the test slide using the disposable pipette provided. A drop of latex reagent is then added next to the serum and both drops are then spread on the whole circle by the other end of the pipette and the test slide is then tilted gently forwards and backwards every 2 seconds for 2 minutes comparing with positive and negative controls. 4.Plasma osteopontin measured by an enzyme-linked immunosorbent assay (ELIZA)(8) using Promokine® Bioscience alive (UK) kits. The kit contains: human OPN microtiter plate, one plate of 96 Wells; human OPN labeled antibody, 1 vial; assay buffer, 30 ml; labeled antibody diluent, 10 ml; wash buffer concentrate, 50 ml; human OPN standard, 1 vial; substrate buffer, 5 ml; peroxide solution, 5.5 ml; TMB tablets, 2 tablets; stop solution, 11 ml; human OPN assay layout sheet, 1 each; plate sealer, 2 each. The plate washed by adding 400 µL of wash solution to each well. Wash repeated 1 more time for a total of 2 washes. After the final wash, wells were emptied or aspirated, and the plate firmly tapped on a lint free paper towel to remove any remaining wash buffer. 100 µL of assay buffer was pipeted into the S0 (0 ng/ml Standard) wells then pipet 100 µL of standards #1 through #7 into the appropriate wells and 100 µL of patient plasma (obtained by centrifugation of morning blood samples) into the appropriate wells and the plate tapped gently to mix the contents. The plate then sealed and incubated at 37 °C for 1 hour then the wells emptied and washed by adding 400 µL of wash solution to every well. The wash repeated 6 more times for a total of 7 washes. After the final wash, wells were emptied or aspirated, and the plate then firmly tapped on a lint free paper towel to remove any remaining wash buffer. 100 µL of the labeled antibody was then pipeted into each well, except the blank and the plate sealed and incubated at 4 °C for 30 minutes. Substrate then prepared and the wells emptied and washed by adding 400 µL of wash solution to every well and the wash repeated 8 more times for a total of 9 washes. After the final wash, the wells were emptied or aspirated, and the plate firmly tapped on a lint free paper towel to remove any remaining wash buffer then 100 µL of the substrate solution was added to each well and the plate 2 incubated at room temperature for 30 minutes in the dark. 100 µL of stop solution was then added to each well and the plate reader blanked against the blank wells. The optical density then read at 450 nm, preferably with correction between 570 and 590 nm or the mean optical density of the blank wells subtracted manually from all readings. Finally results were read using the provided table and curve. Results were tabulated and statistically analyzed using a statistical software (KyPlot, Kioshi Yoshioka, Japan 1999-2001v2) RESULTS: Clinical characteristics of patients and control subjects are shown in table 1. The table shows that patients of both RA and SLE as well as controls are comparable as regard age and sex. Comparison of FEV1% pred showed statistically highly significant difference between patients as whole groups as well as those with and without fibrosis and controls in both of RA and SLE (p < 0.001 for all) while the difference was non significant between RA and SLE patients as a whole or in sub groups (p > 0.05). A significant difference was found between patients with fibrosis and those without in both RA and SLE (P <0.05) which reflects the restrictive ventilatory effect of lung fibrosis in these patients (table 2) Comparison of CRP between patients as whole groups and controls showed a highly significant difference in both of RA and SLE ( p< 0.001 for all) reflecting the active systemic inflammation in these patients. Also, a significant difference was seen between patients with fibrosis and those without in each disease group (p < 0.05) indicating a more active inflammatory process in those with fibrosis but a non significant difference was found between similar subgroups of the two diseases (p > 0.05) reflecting a comparable degree of inflammation in the two patients groups ( tables 3). Comparison of plasma OPN between patients and controls also showed highly significant difference in both RA and SLE as well as in those with and without evidence of fibrosis (p <0.001 for all). Moreover, a highly significant difference was found between those with fibrosis and those without in both groups (p < 0.001). No statistically significant difference seen between RA and SLE patients whether as a whole group or in those with and without evidence of fibrosis (table 4), again reflecting a comparable degree of inflammation in the two groups. Correlation between OPN and FEV1% pred showed statistically highly significant negative correlation in both RA and SLE patients (r = - 0.83 and r = - 0.66, p < 0.001 for both respectively)(table 5, fig 1&2). Correlation between OPN and ESR and CRP showed highly significant positive correlation in RA patients (p <0.001, r = 0.93 and r = 0.87 respectively) (table 5, fig 3,5). In SLE patients the relation was only significant (p < 0.05, r = 0.47 and 0.51 respectively) (table 5, fig 4,6). This means that higher levels of plasma OPN is associated with higher inflammation and more restriction (i.e. fibrosis). 3 Table (1): Clinical characteristics of all groups included in the study Age in years Sex Smoking FEV1% predicted Rheumatoid arthritis Systemic lupus 29.28 ± 10.05 No fibrosis With fibrosis 29.3 ± 10.42 29.25 ± 10.3 7 ♂ , 11 ♀ No fibrosis With fibrosis 4 ♂, 6 ♀ 3 ♂, 5 ♀ No 68.5 ± 7.68 No fibrosis With fibrosis 70 ± 4.85 63.63 ± 3.96 33.88 ± 7.88 No fibrosis With fibrosis 37.7 ± 7.11 29.86 ± 6.89 6 ♂ , 11 ♀ No fibrosis With fibrosis 3 ♂, 7 ♀ 2 ♂, 5 ♀ No 66.94 ± 8.63 No fibrosis With fibrosis 69.8 ± 3.76 58.57 ± 6.19 Controls 27.3 ± 9.01 6 ♂, 4 ♀ No 83.7 ± 3.35 40.833 ± 9.332 39.11 ± 11.385 ESR No fibrosis With fibrosis 34.9 ± 5.82 48.25 ± 10.57 31.11 ± 7.967 No fibrosis With fibrosis 34.4 ± 10.57 45.857 ± 9.06 28.058 ± 7.277 CRP No fibrosis 26.7 ± 6.429 Total With fibrosis 36.625± 6.209 18 No fibrosis 24.45 ± 6.52 Total With fibrosis 33.21 ± 4.965 17 3.75 ± 1.253 No fibrosis 10 No fibrosis 10 10 With fibrosis 8 With fibrosis 7 Number 8.31 ± 2.63 Table (2): Comparison of FEV1 % predicted between different groups included in the study Rheumatoid Arthritis patients Controls With fibrosis Whole No fibrosis With fibrosis 70.5 76 63.63 66.94 72.8 58.57 83.7 7.68 1.81 4.85 2.25 3.69 3.81 8.63 3.17 3.76 1.92 6.19 3.14 3.3 1.04 Versus controls Versus controls Versus controls Versus controls Versus controls Versus controls 2.55 < 0.05 S 2.625 < 0.05 S 2.83 < 0.001 HS 2.106 < 0.05 S 2.207 < 0.05 S 2.886 < 0.001 HS Whole M SD± SE± Systemic Lupus patients No fibrosis No fibrosis versus fibrosis RA Comparison No fibrosis versus fibrosis SLE t p Sign t p Sign 2.459 < 0.05 S 2.601 < 0.05 S Whole RA versus whole SLE t P Sign No fibrosis RA versus no fibrosis SLE With fibrosis RA versus with fibrosis SLE t P Sign t P Sign t P Sign 1.290 > 0.05 NS 1.647 > 0.05 NS 1.409 > 0.05 NS Sign = significance NS = non significant S = significant HS = highly significant 4 Table (3): Comparison of serum CRP in mg/L between different groups included in the study Rheumatoid Arthritis patients M SD± SE± Comparison Systemic Lupus patients Whole No fibrosis With fibrosis Whole No fibrosis With fibrosis 31.111 7.969 1.878 26.7 6.426 2.035 36.625 6.209 2.195 28.058 7.277 1.765 24.45 6.525 2.063 33.214 4.965 1.876 Versus controls Versus controls Versus controls Versus controls Versus controls Versus controls 10.695 < 0.001 HS 11.078 < 0.001 HS 16.449 < 0.001 HS 10.390 < 0.001 HS 9.851 < 0.001 HS 18.189 < 0.001 HS No fibrosis versus fibrosis RA t 3.303 t 1.81 Sign = significance P > 0.05 t 2.988 p < 0.01 No fibrosis RA versus no fibrosis SLE Whole RA versus whole SLE Sign NS 3.75 1.253 0.396 t P Sign No fibrosis versus fibrosis SLE Sign S p < 0.01 Controls t 0.776 NS = non significant P > 0.05 Sign NS S = significant Sign S With fibrosis RA versus with fibrosis SLE t 1.162 P > 0.05 Sign NS HS = highly significant Table (4): Comparison of plasma osteopontin in ng/ml between different groups included in the study Rheumatoid Arthritis patients M SD± SE± Comparison Systemic Lupus patients Whole No fibrosis With fibrosis Whole No fibrosis With fibrosis 973 483.36 113.93 666.4 254.45 80.464 1356.25 426.62 150.833 873.111 404.18 98.013 667.7 276.43 87.346 1166.57 387.635 146.512 Versus controls Versus controls Versus controls Versus controls Versus controls Versus controls 5.412 < 0.001 HS 6.474 < 0.001 HS 9.042 < 0.001 HS 5.694 < 0.001 HS 5.994 < 0.001 HS 8.745 < 0.001 HS No fibrosis versus fibrosis RA t 4.269 p < 0.001 Whole RA versus whole SLE t 0.661 Sign = significance P > 0.05 Sign NS Controls 136.6 46.987 14.858 t P Sign No fibrosis versus fibrosis SLE Sign HS t 3.111 p < 0.001 No fibrosis RA versus no fibrosis SLE t 0.011 NS = non significant P > 0.05 Sign NS S = significant Sign HS With fibrosis RA versus with fibrosis SLE t 0.896 P > 0.05 Sign NS HS = highly significant 5 Table (5): Correlation between plasma osteopontin and FEV1% pred., ESR and CRP in RA and SLE patients Parameter Osteopontin with FEV1% pred. Osteopontin with ESR Osteopontin with CRP RA SLE RA SLE RA SLE FEV1% OSP FEV1% OSP ESR OSP ESR OSP CRP OSP CRP OSP Σ Σ2 1269 17154 1138 13644 735 17154 655 13644 560 17154 477 13644 90467 21012959 77370 12654668 31493 21012954 28087 12654668 18502 21012954 14231.5 12654668 Reg Q SE ± Reg Q r - 0.8285 0.134 - 0.83 - 0.6622 0.193 - 0.66 0.9257 0.094 0.93 0.4732 0.247 0.47 0.8684 0.123 0.87 0.5091 0.245 0.51 P /Sign <0.001 HS <0.001 HS <0.001 HS <0.05 S <0.001 HS <0.05 S 6 DISCUSSION: Osteopontin (OPN), a newly discovered proinflammatory cytokine, is now under extensive evaluation for its rule in different inflammatory disorders within and outside the lung (10). We carried out this study to find the relation of OSP to lung inflammation and fibrosis in patients with rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE), the most common collagen vascular disorders. We have found a highly significant difference in FEV1% of predicted between patients of both groups and controls (p<0.001) reflecting the restrictive ventilatory defect in these patients. Patients of both groups with evidence of fibrosis on CT showed more reductions in FEV1% of predicted (table 2), a well known finding in such patients (11). Also ESR and CRP were significantly higher in both groups of patients than controls (p< 0.001) with no significant difference seen between them which reflects the active inflammatory process in these patients. In RA patients plasma OPN was found to be significantly higher than in controls (p<0.001) and to correlate significantly and positively to plasma CRP levels and ESR and negatively to FEV1% of predicted. This means that OPN almost has a role in the inflammatory process or at least secreted by the activated inflammatory cells in these patients. Although after extensive search we found no paper that studied OPN in RA patients with lung fibrosis, yet we have found important data in papers that studied it in RA and idiopathic lung fibrosis (IPF). Oshima et al (2002)(12) found increased production of OPN in plasma and synovial fluid of RA patients than those with osteoarthritis and normal controls and also found significant positive correlation to the severity to the joint affection. Because lung lesions in rheumatoid arthritis have the same pathology as that in the synovial membrane (13), osteopontin almost plays the same role in the lung. Also, the pathology of lung fibrosis in RA is identical to and cannot be differentiated from that in IPF in which plasma OPN levels were found by Kadota et al (2004)(8) to be significantly elevated. These authors also showed by immunohistochemical staining of surgical lung biopsy specimens obtained from 2 patients with IPF and 2 with NSIP (non specific interstitial pneumonitis) that OSP is localized mainly in alveolar macrophages and airway epithelium and concluded that this cytokine plays an important role in development of lung fibrosis in these patients. Using microarrays for gene expression, Prado et al (2005)(14) studied the effects of OPN on lung fibroblasts and alveolar epithelial cells in 13 lung samples obtained from IPF patients and found that it induced a significant increase in migration and proliferation in both fibroblasts and epithelial cells. However, although the effect on 7 fibroblast migration/proliferation was dependent mainly on integrins, in epithelial cells proliferation was mainly dependent on CD44 and migration was dependent on CD44 and integrin signaling. Also they found OPN to have profibrotic-relevant effects on molecules involved in extra cellular matrix remodeling as in fibroblasts it increased TIMP-1 and type I collagen and inhibited MMP-1 expression, whereas in alveolar epithelial cells it induced MMP-7. In a murine model, Yamamoto et al (2003)(15) showed that antibodies to the SLAYGLR epitope of OPN (the most active portion of the molecule named M5) inhibited synovial membrane cell proliferation and inflammatory cell infiltration and that M5 antibodies prevented the development of arthritis in pretreated mice which constitutes a strong evidence of the involvement of OPN in the inflammatory process of RA.. In SLE patients also we found plasma OPN levels to be significantly higher than in controls and in patients with fibrosis than in those without. A significant positive correlation between OPN and both of ESR and CRP and a significant negative correlation with FEV1% of predicted was seen although correlation to ESR and CRP was less stronger than in RA (table;5, figs; 3-6). These findings suggest a role for OPN in lung fibrosis in these patients like in RA. This agrees with Wong et al ( 2005)(16) who showed significantly higher concentrations of plasma OPN in SLE patients especially those with renal affection and those levels positively correlated to disease activity score and IL-18 which is an important marker of disease activity. The authors also found excess production of OPN from monocytes ex-vivo and concluded that the cytokine almost has a relation to inflammation in these patients and could serve as a potential marker for disease activity. Not only OPN was shown to be related to disease activity in collagen vascular diseases but also to disease susceptibility. Using polymerase chain reaction and restriction fragment length polymorphism (PCR-RFLP), An-Ping et al (2007)(17) found OPN gene polymorphism to be associated with significantly higher incidence of RA in Chinese people. In our study we found no significant difference in ESR, CRP or plasma OPN levels between RA and SLE groups whether with or without fibrosis which reflects a comparable degree of inflammation in these patients. Finally, we can conclude that plasma OPN could be a good marker for disease activity and could be used to predict those who at risk of developing lung fibrosis in RA and SLE patients. We also recommend more studies that measure OPN in broncho-alveolar lavage fluid and lung biopsy samples in these patients. REFERENCES: 1. Rodan G. Osteopontin overview. Ann NY Acad Sci 1995;760:1–5. 2. Giachelli CM, Lombardi D, Johnson RJ, et al. Evidence for a role of osteopontin in macrophage infiltration in response to pathological stimuli in vivo. Am J Pathol 1998;152: 353–8. 3. Okada H, Moriwaki K, Kalluri R, et al. Osteopontin expressed by renal tubular epithelium mediates interstitial monocyte infiltration in rats. Am J Physiol Renal Physiol 2000;278: F110–21. 4. Nau GJ, Guilfoil P, Chupp GL, et al. A chemoattractant cytokine associated with granulomas in tuberculosis and silicosis. Proc Natl Acad Sci USA 1997;94:6414–9. 8 9