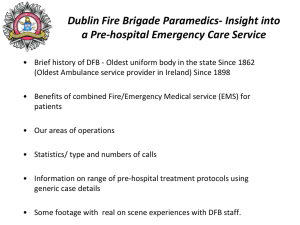
Community Paramedic Practitioners
advertisement

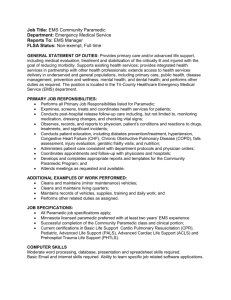
2014-19 Business Planning Template (QIPP, Cost Pressures, Integration Transformation Fund) Name of Initiative Community Paramedic Practitioners Benefit type Cost avoidance / Patient experience / Primary Care experience / Ambulance service experience High level description of Initiative The primary role of the Paramedic Practitioner is the delivery of unscheduled (urgent and emergency) care to patients, integrated with primary care and based in the community, by an appropriately trained health care professional. CCG priorities Transforming the community system. Description of how meets CCG priorities Provides care closer to home Reduces Non-Elective admissions Integration of community services to help provide seamless service closer to home Improve productivity within primary care Improvement to local 999 red call performance Confirmation of how addresses ITF priorities Joint assessments and accountable lead professional Lead GP Member Dr Charles Parker Integrated Commissioning Board priorities Improving quality of care / Improving patient experience / Working more effectively across services boundaries / Improving health and wellbeing Lead Manager (+ email) John Darley (john.darley@nhs.net) Size of net financial benefit £0 Overall description/scope As the dynamics of the NHS change the realisation that our A&E departments and hospitals are under ever increasing pressure to cope with the increased volume of patient attendances we need to actively seek out new strategies (such as community based Paramedic Practitioners) to manage demand in the local community while simultaneously reducing demand on A&E departments and conveyance rates to hospital for the ambulance service. Timescales and Milestones Service specification and job description for the Paramedic Practitioner role – completed August 2013. Agreement from GP Practices in Northallerton (suggest working across both Mowbray House and Mayford Surgery) and Whitby (suggest Whitby Group Practice) localities to host a PP (based on existing models in Catterick (Harewood practice) and Sleights/Sandsend – March 2014. Recruitment by YAS of 4 Paramedic Practitioners – 2 from each local area – Latest figures provided by the NHS suggest at least one million people are currently taken to an emergency department every year, could be treated at scene. The primary role of the Paramedic Practitioner is the delivery of unscheduled care to patients in the community by an appropriately trained health care professional through integration with GP Practices in the Northallerton and Whitby localities. The role of a paramedic practitioner (more advanced role to a paramedic) utilizes Time to project delivery (contract award) Time to steady state (from contract award) 6 months from agreement and formal confirmation of the proposal with YAS Within 3 months of commencement. the skills of paramedics and other professionals (such as specialist nurses with additional skills) to support the first contact needs of patients in unscheduled care. Paramedic Practitioners also independently provide definitive care that does not require intervention of a GP/doctor. Paramedic Practitioners are normally employed by the local ambulance service. Based on a working pattern of 10 hours per day (0800 – 1800hrs) Monday – Friday at two locations (Northallerton & Whitby) the scope of the Paramedic Practitioner (PP) usually covers (but is not limited to) the following: Administering medications within the remit of local PGD. Prescribing medications to patients in line with local PGD. Undertake routine assessments of patients with long term conditions in their home. This helps people with such conditions to better manage their own health and avoid unnecessary visits to hospital Ordering x-rays and requesting further investigations Take a holistic approach to patient care, bringing together their medical, social and psychological needs Encouraging the promotion of health education in the community Treating minor illness and minor injury within an unscheduled care environment or in the patient’s home. Referring patients to alternative health and/or social services Breaking down existing professional boundaries and encourage collaboration. Empowering patients to take responsibility for managing their own care and treatment where it is safe and appropriate to do so Undertaking an in-depth patient examination and assessment beyond existing JRCALC (current practice framework for paramedics) guidelines Identifying and providing alternative care pathways for the provision of emergency care June 2014. New service planned go “live” October 2014 in Northallerton and Whitby. Undertake audit and research be personally responsible for self directed learning Carrying out and interpreting diagnostic tests Responding to Red 999 calls in the local area to their GP Practice base. Patient Acceptability & Experience The service should, based on existing scheme evidence from the Harewood and Sleights/Sandsend practice models, lead to a better patient experience as more patients are treated closer to home and do not require conveyance to an A&E department. Complexity of stakeholder engagement / providers working together The model would require the agreement of up to three GP Practices to host a YAS Paramedic Practitioner within their practice premises. Resources required to implement project The model can be delivered within existing management resources from the CCG (Urgent Care Lead and GP Lead) and YAS (locality manager with North Yorkshire Assistant Director for A&E Operations support). Certainty of service continuity Continuity of service provision is assured while extended skills paramedic roles exist within the ambulance service. The Paramedic Practitioner will also provide a faster and more local response to 999 Red calls in the local area. Patient Safety Clinical Effectiveness Treating more patients closer to home more often and reducing the need to attend A&E departments for treatment improves the care available to those patients and other patients who need the advanced clinical skills only available through A&E. Existing identical models of care already exist in the CCG area at Catterick and Sleights/Sandsend. Feedback from both primary care and YAS to the service model since their introduction in August 2013 has been very positive. Equity of Access The service model will would improve access to unscheduled care in the Whitby area, where ambulance travel times to their nearest A&E department in Middlesbrough are considerable. Based on current evidence the extended skills role is one that is expanding rather than declining with operational and strategic support from both the ambulance service and commissioners. Confidence in market The Northallerton model should reduce A&E attendances at the Friarage Hospital site thereby improving access and reducing waiting times for patients requiring A&E care at the Friarage. Sustainability / Corporate Social Responsibility The model should result in a reduction in conveyance rates to A&E departments for both the ambulance and self transporters thereby reducing the local carbon footprint as YAS are fully supportive of further developing the model in partnership with HRW CCG as a key strategic and operational aim in delivering improved unplanned care service and response in a highly rural area. Competition between NHS ambulance services for contracts has not included A&E services (employer of Paramedic Practitioners) to date. There is currently no indication that this is likely to change in the foreseeable future. Private sector competition is currently restricted to non-emergency PTS and some providers are now showing an interest in the delivery of some Urgent Care transport. Information Availability Early evidence (3 months) from GPs/YAS working with the existing schemes in Catterick and Sleights/Sandsend is very more unplanned care is delivered in local communities. positive. The only sustainability risks with the model are the recruitment and retention by YAS of Paramedic Practitioners local the Whitby and Northallerton areas. Evidence from similar (ECP) schemes in other localities across North Yorkshire reports excellent outcomes for patients in terms of numbers treated locally and not referred onto A&E and also in 999 Red call responses in the local area. Risks Risks identified (including unintended consequences) Based on identical existing models there are no foreseeable intended (or un-intended) risks with this model. Mitigating actions Timescale N/A N/A Method of Identifying (including KPIs) Where are savings released? Benefits/Outcomes Benefits/Outcomes Adding two additional PPs across HRW (Northallerton and Whitby) would result in more patients with urgent, (but not life-threatening), conditions from those towns being treated at home rather than being taken to hospital. This would benefit, for example, older people who have had a fall and suffered cuts, bruises or other minor injuries and would prefer not to leave their home for treatment. Evidence of existing Paramedic Practitioner schemes working to a Standard Operating Procedure shows more patients are treated in their own community, reducing 999 ambulance call outs (hence leaving more ambulance resource in the local community more often) and subsequent ambulance conveyance rates to A&E, which in turn reduces pressure on the 4hr A&E target and associated ambulance turnaround times from A&E. The Paramedic Practitioners would have the use of a YAS rapid Response Vehicle (RRV) allowing them to respond to 999 Red emergency calls in the local area. Quantity & Volume of the Service Number of referrals received by the Paramedic Practitioners from practice staff. Number of these referrals treated or referred onto alternative or further care (other than hospital) by the PP. Number of 999 Red calls responded to in the local area. Number of 999 Red calls responded to within 8 minutes. Quality of the Service Compliments received Complaints received Practice assessment of service quality delivered to their patients Paramedic Practitioner’s assessment of the quality of referrals made by practice staff Whether the service has made a difference Once fully established within the community a cost reduction (through A&E tariff savings) against the total overall cost of the PP investment would be the most likely scenario from the schemes in Northallerton, Whitby, Catterick and Sleights/Sandsend. Evidence from other schemes reports a high response percentage within 8 minutes. Stakeholder group and purpose Yorkshire Ambulance Service NHS Trust GP Practices in Northallerton and Whitby HRW CCG £’000 Expenditure FY14/15 6mths effect = £78.5k Reduction in A&E attendances – based on patient numbers seen and treated/referred (away from A&E) by the PPs Hospital admissions avoided (based on A&E attendance conversion rates). Method of engagement and frequency Engagement with GP Practices involved and local YAS operational leads to establish and introduce the new model locally and planned “go live” dates. FY15/16 FY16/17 Exit plan 6mths notice given to YAS to allow integration of PP staff members back into YAS core establishment as part of normal staff turnover and recruitment in HRW area. FY17/18 FY18/19 12 mths effect = £157k 12 mths effect = £157k 12 mths effect = £157k 12 mths effect = £157k £30k £30k £30k £30k 3.5 WTE PPs (based on 100hrs per week including relief) – top AfC Band 6 (plus 30% on costs) = £45000 x 3.5 WTE = £157k Saving 6mths effect = £15k 1 patient attendance at A&E per PP per day are avoided = 10 patients per week across the two new schemes = 520 patient attendances avoided per year. 520 A&E attendances @ £57 per attendance = £30k FYE Total Total net cost (savings) 63.5 127 127 127 127