Short Notes on Headache
advertisement

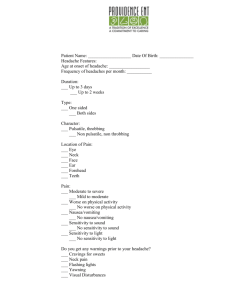
Short Notes on Headache Number Seven Cluster Headache In contrast to migraine and the other primary headache disorders, the intensity of a cluster headache is best described as excruciating. Cluster headaches have been called suicidal headaches because patients with cluster have often committed suicide. If the duration of the individual cluster headache were much longer than the usual 30–45 minutes, probably most of the patients with cluster would resort to suicide. I have been called to see a patient with cluster who was admitted to the psychiatric ward after an unsuccessful suicide attempt. When you are asked to see a patient with suspected cluster, it is an emergency and treatment should be given immediately. Fortunately most patients with cluster can be helped. Cluster headaches occur in 0.3 % of the young adult population, and are thus much less common than migraine. There is on a minimal increased occurrence in families. Cluster occur 3–4 time more frequently in males than females, the reason for this sex difference being unknown since there is no apparent relation to hormonal dysfunction. The onset is usually in the third or fourth decade, but recurrent cluster may continue in subsequent years. In the literature there are reports of the age of onset ranging from 1– 80 years of age. In one study the incidence in 18 year olds was 0.09%. The onset is rare in children and younger teenager. Kunkle and Pfieffer at Duke in 1952 first used the term “cluster” to describe the headaches as occurring in bunches followed by weeks, months or even as long as 20 years before the next series of daily headaches might occur. Between these clusters the patient might experience very infrequent, less intense, but otherwise typical cluster pain lasting only a single day, leading them to fear that another full blown cluster is starting. In 80-90% of cluster patients the headaches are episodic, occurring as bouts or “clusters” of daily headaches usually lasting 6–14 weeks which spontaneously cease. At the onset or near the termination of one of these clusters the intensity of pain might be less and the headaches might occur only once a day. The severity and frequency rapidly increases after the cluster begins to become 3-4 excruciating headaches each day, the individual headaches lasting 15-180 minutes. In the other 10-20% of patients with cluster, the condition is chronic. The classification committee of the International Headache Society defined chronic cluster as lasting for longer than one year without remission or with remissions lasting less than one month. The diagnosis of cluster is quite simple and does not require imaging or any laboratory studies. It is based on the history. When the patient is seen, he usually is not having an attack. The patient should have a complete history, review of systems and neurological examination to exclude other conditions. Careful inquiry should be made into previous medications taken for the headaches and possible medications that are being used daily for other conditions. The headaches are unilateral and localized to the eye and temple. Occasionally the pain is described as spreading up from the neck or down into the neck. Often the pain is circadian, occurring at or near the same time each day. A frequent time of onset is 2- 3 AM and another peak occurs at 9AM. The reason for this is unknown, but points to the suprachiasmatic nucleus, the site of the biologic clock. In contrast to a severe migraine headache which often causes the patient to remain motionless in a darkened room, the patient having a cluster headache feels the urge to get up and move about, even strike their head on the bedroom wall and breaking the drywall in their bedroom. Fifty percent of patients describe their pain as pulsating and up to 70% note mild photophobia or phonophobia. There is no nausea or vomiting, no aura or other migrainosus features. The pain reaches maximum intensity after 5-10 minutes, too fast to allow for relief with an oral medication. The individual headache pain rapidly subsides and between the daily clusters the patient has no symptoms other than fear of the next attack. Predominately unilateral changes of function of the autonomic nervous system on the same side as the pain occur in 97% of the headaches. In the other 3% autonomic changes might have been present but were not noted by the patient or those around them. Increased lacrimation is the most frequent (90%), with conjunctival injection, ptosis, miosis and rhinorrhea each noted in 75% of the patients. Facial flushing, sweating and nasal congestion are less frequent. These represent unilateral loss of sympathetic nervous system function and increases parasympathetic nervous system activity. The reason for this variation in autonomic changes and the site where the dysfunction occurs is not known. The underlying etiology of cluster is unknown. When headache free, the neurological examination is normal. During an attack there are changes reported on PET scans of the suprachiasmatic nucleus. This is not surprising since there often is a circadian pattern, indicating something is occurring in the body’s biological clock. Occasionally imaging studies on patients with cluster reveal asymptomatic brain tumors or AV malformations at various sites in the brain, either on the same side or the opposite side from the headaches. As will be discussed later, a subsequent series of cluster headaches might occur on the side opposite from the original site. Brain tumors and other structural lesions do not jump from side to side. Cluster headaches might be precipitated by alcohol, nitroglycerine and intravenous histamine, but these observations do not point to a specific chemical etiology. Intravenous sumatriptan, the 5HT1B/1D agonist used for stopping a migraine, will terminate a cluster headache, but this does not reveal the chemical basis and does not prevent the next headache which might start a few hours later. Unusual and unexplained presentations of cluster are seen. The patient’s spouse might note the onset of ptosis and myosis 30 minutes before the onset of headache. There are a few reports of a visual or sensory aura prior to the headache. After recurrent clusters on one side, 14% of patients experience a subsequent cluster on the opposite side. Infrequently the headaches might shift sides during a single cluster. The pain might start in the neck and spread up to the eye. As mentioned there may be absence of the ipsilateral autonomic dysfunction in up to 3% of cases, thought this may be due to lack of proper observation. There are a few reports of patients with the typical autonomic changes who deny a headache. A patient might describe minimal pain in the opposite eye. There may be low grade pain between the clusters of excruciating pain. There are two other headache patterns with the same unilateral changes of function of the autonomic nervous system but these are easy to distinguish from cluster. The first is paroxysmal hemicrania, a condition which occurs in both an episodic and chronic form but is three times more frequent in females than males. The pain is not as intense as cluster. It is unilateral, but might spread beyond the eye and temple. The individual headaches are shorter, 2-30 minutes in duration, and occur once every other day to as often as eight times a day. The patient with paroxysmal hemicrania does not have the urge to be up and move about. In contrast with cluster headaches, the patients with paroxysmal hemicrania have an immediate response to indomethacin 25-100 mg t.i.d. After the patient is headache free for a few weeks following indomethacin, attempts should be made to reduce or discontinue the drug. The other headache condition with unilateral changes of the autonomic nervous system is the extremely rare SUNCT syndrome (Short-lasting Unilateral Neuralgiform headache attacks with Conjunctival injection and Tearing). The pains last 5 seconds to 2 minutes and are orbital, supraorbital or temporal and may occur 3-200 times per day. These may be a manifestation of lesions in the posterior fossa or around the pituitary gland. Often they do not respond to drug therapy. Throughout the years physicians have tried almost every medication in the hope of providing relief. There is no therapy for cluster headaches which has been proven by adequate studies with comparison to placebo. The rapid increase to peak intensity excludes the use of oral medications to stop a headache. As mentioned previously intravenous sumatriptan will terminate a headache, but does not prevent the next headache that will occur later in the day. There is a limit on the number of injections of sumatriptan which can be administered in a single day and the drug is expensive. Therefore therapy must be selected to prevent the next attack. This author has found the following regimen will stop 70+% of clusters. First the patient should immediately be given prednisone 50 mg every 12 hours for 5 days, following which the drug is abruptly stopped. If the pharmacy does not have the 50 mg tablets, then the patient can alternate 60 mg and 40 mg doses. The onset of action is rapid. Patients have reported that if a headache starts 3-4 hours after the initial dose, the pain will be only brief and minimal and thereafter they are headache free for the following 5 days. Using a brief course of high dose prednisone without subsequent tapering does not cause Addison’s disease or other complications. On the same day that prednisone was started, the patient should be started on oral verapamil, using 40 mg t.i.d. the first day, 80 mg t.i.d. the second day, 120 mg t.i.d. the third day and 160 mg t.i.d. thereafter. This is about twice the dose of this calcium channel blocker than that which is used to treat hypertension. The use of 80 mg tablets provides a higher blood level than the once a day 240mg capsules. By the sixth and seventh day the patient is off prednisone and usually headache-free. If cluster headaches return on the sixth, seventh or eighth day, the verapamil should be increased to 640 mg per day or even 720 mg per day. Goadsby and his coauthors have recently stated that there is no need for a baseline EKG unless the daily dose exceeds 700 mg. His group had given 960 mg daily without complications and there was one report from Sweden of a patient using 1300 mg without ill effects. After the patient has remained headache free on verapamil and he is beyond the duration of his previous clusters, the verapamil can be progressively reduced and terminated by the fourth or fifth day. If the patent begins another series of daily cluster headaches in later months or years, the prednisone/ verapamil regimen can be repeated. Prior to the development of prednisone the standard treatment was the inhalation of 100% oxygen at 7-10 liters per minute flow. This provided partial or complete termination of a headache in about 70% of the subjects who used it. It can be used if the prednisone/verapamil approach fails. The patient would have to keep a small portable tank of 100% oxygen with him at all times. Lithium carbonate starting at 300 mg bid is reported to help patients with episodic cluster and chronic cluster. The onset of action is noted in about one week and the drug needs to be adjusted by following blood levels. There are multiple side effects from using lithium, so it would be advisable to have the assistance of someone who has previous experience with the drug. Methysergide is still mentioned in some books as a treatment of both migraine and cluster but fortunately has been taken off the marked. It caused major side effects including retroperitoneal and pericardial fibrosis. In the May 2011 issue of HEADACHE there was an article describing 50% successful treatment of chronic cluster using daily warfarin sufficient to obtain an INR of 1.5 - 1.9, slightly less than the dose used for atrial fibrillation and other problems. Since it often is impossible to find a satisfactory drug treatment for chronic cluster, various neurosurgical and radiation techniques have been used. These have included radiofrequency thermocoagulation of the trigeminal nerve, injections of glycerol into the gasserian ganglion, cutting (lesioning) the trigeminal nerve at the root entry zone, microvascular decompression of the trigeminal and gamma knife radiation. Apparently none of these procedures have yielded perfect results, complications vary and reoccurrence of the cluster headaches on the same side have often been reported. In the 14% of patients who might develop subsequent cluster headache on the opposite side, these procedures would not be beneficial. In summary cluster headaches are a medical emergency and most often can be helped, the first treatment to try is the combination or prednisone and verapamil. revised October 26, 2012