CHAPTER 27 - Nursing Pharmacology
advertisement

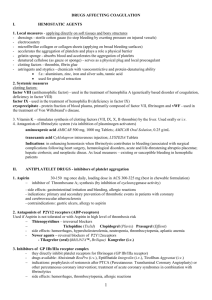
CHAPTER 27 DRUGS FOR COAGULATION DISORDERS LEARNING OUTCOME 1 Illustrate the major steps of hemostasis and fibrinolysis. Concepts 1. Hemostasis is a complex process involving a number of clotting factors that are activated in a series of sequential steps. The final product is a fibrin clot that stops blood loss. 2. The clotting process begins when blood-vessel injury causes vessel spasm (constriction); platelets are attracted to and adhere to the injured area. That aggregation of platelets forms a plug in which formation of insoluble fibrin strands and coagulation (coagulation cascade) occurs. Normal blood clotting occurs in about 6 minutes. The basic steps of hemostasis are shown in Figure 27.1. 3. The coagulation cascade includes intrinsic and extrinsic pathways that lead to formation of the fibrin clot. Near the end of the cascade, a chemical called prothrombin activator or prothrombinase is formed. Prothrombin activator converts the clotting factor prothrombin to an enzyme called thrombin. Thrombin then converts fibrinogen, a plasma protein, to long strands of fibrin. The fibrin strands provide a framework for the clot. Thus, two of the factors essential to clotting, thrombin and fibrin, are formed only after injury to the vessels. The fibrin strands form an insoluble web over the injured area to stop blood loss. The steps in each coagulation cascade are shown in Figure 27.2. 4. Fibrinolysis or clot removal involves several sequential steps. When the fibrin clot is formed, nearby blood vessel cells secrete the enzyme tissue plasminogen activator (TPA). TPA converts the inactive protein plasminogen, which is present in the fibrin clot, to its active enzymatic form, plasmin. Plasmin then digests the fibrin strands to remove the clot. The body normally regulates fibrinolysis such that unwanted fibrin clots are removed, whereas fibrin present in wounds is left to maintain hemostasis. The steps of fibrinolysis are shown in Figure 27.3. Figure 27.1 Basic Steps in Hemostasis Figure 27.2 Major Steps in the Coagulation Cascade: Common Pathway Figure 27.3 Primary Steps in Fibrinolysis LEARNING OUTCOME 2 Describe thromboembolic disorders that are indicators for coagulation modifiers. Concepts Diseases of hemostasis include thromboembolic disorders caused by thrombi and emboli, thrombocytopenia, and bleeding disorders such as hemophilia and von Willebrand’s disease. Adams_IRM Ch 27-1 LEARNING OUTCOME 3 Identify the primary mechanisms by which coagulation modifier drugs act. Concepts 1. Drugs can modify hemostasis by four basic mechanisms. The basic mechanisms of hemostasis are shown in Table 27.2. 2. Anticoagulants prevent the formation of clots by either inhibiting specific clotting factors in the coagulation cascade or diminishing the clotting action of platelets. All anticoagulant drugs will increase the normal clotting time. 3. Antiplatelets prevent clot formation by inhibiting platelet action. 4. Thrombolytics remove an existing clot by dissolving life-threatening clots. 5. Hemostatics promote clot formation by inhibiting fibrin destruction. Table 27.2 Mechanisms of Action of Coagulation Modifiers LEARNING OUTCOME 4 Explain how laboratory testing of coagulation parameters is used to monitor anticoagulant pharmacotherapy. Concepts Laboratory tests are an integral part of diagnosing bleeding disorders and monitoring anticoagulant pharmacotherapy. These tests include Activated clotting time, Activated partial thromboplastin time (aPTT), Bleeding time, Heparin anti-Xa, Platelet count, Prothrombin Time (PT), Thrombin time. Table 27.1 Laboratory Testing for Coagulation Disorders LEARNING OUTCOME 5 Describe the nurse’s role in the pharmacologic management of coagulation disorders. Concepts 1. The role of the nurse in the pharmacologic management of coagulation disorders involves careful monitoring of patient’s condition and providing education as it relates to the prescribed drug treatment. Obtain baseline medical, surgical, and drug history; lifestyle and dietary habits, including use of herbal or alternative therapies; and detailed description of symptomology and current therapies. 2. Anticoagulants: The most serious side effect is bleeding; monitor for signs and symptoms of excessive visible bleeding: bleeding at IV sites, wounds, excessive echhymosis, petechiae, hematuria, black/tarry stools, rectal bleeding, “coffee-ground” emesis, epistaxis, bleeding from gums, hemoptysis, prolonged and/or heavy menstrual flow; and for occult bleeding: pallor, dizziness, hypotension, tachycardia, abdominal pain, areas of abdominal wall swelling or firmness, lumbar pain, decreased level of consciousness. Risk for bleeding increases during the transition time from heparin to warfarin when both drugs are given at the same time. Do not give warfarin to pregnant patients; heparin and low-molecular-weight heparin can be given to pregnant patients. Take warfarin at the same time each day. Avoid vitamin K supplements, and protein Ch 27-2 Adams_IRM supplement drinks (e.g., Ensure™ or Boost™), which often have vitamin K added, and limit intake of garlic. Teach patient or caregiver in proper self-administration techniques. 3. Antiplatelets: Monitor for signs and symptoms of bleeding: oozing at IV sites or wounds, ecchymosis, petechiae, hematuria, black/tarry stools, rectal bleeding, “coffee-ground” emesis, epistaxis, bleeding from gums, prolonged and/or heavy menstrual flow; and for occult bleeding: pallor, dizziness, hypotension, tachycardia, abdominal pain, areas of abdominal wall swelling or firmness, lumbar pain, decreased level of consciousness. Risk for bleeding; increases if given concurrently with anticoagulants. Injection or venipuncture sites will need prolonged pressure to control bleeding. Continue to monitor peripheral pulses for quality and volume, complaints of angina or chest pain, especially if new or of sudden onset or accompanied by dyspnea. 4. Thrombolytics: Be aware of conditions that exclude patients from receiving thrombolytics. Monitor frequently for signs and symptoms of excessive visible bleeding: bleeding at IV sites, wounds, hematuria, rectal bleeding, “coffee-ground” emesis, bleeding from gums, hemoptysis, bleeding at previous recent incisional sites; and for occult bleeding: pallor, hypotension, tachycardia, dizziness, sudden severe headache, lumbar pain, and decreased level of consciousness. Monitor vital signs and ECG every 15 minutes during first hour of infusion, and then every 30 minutes during remainder of infusion and for first 8 hours. Report any dysrhythmias immediately. Monitor baseline coagulation studies. Monitor level of consciousness, as cerebral hemorrhage is a concern. Observe for reperfusion arrhythmias. Teach patient about the increased risk of bleeding. 5. Hemostatics: Monitor for clotting in the peripheral vascular system, pulmonary system, nervous system, and cardiac system. Administer intravenously; monitor site closely for thrombophlebitis and extravasation. Assess for presence of myopathy and myoglobinuria (reddish-brown urine). Teach patient to report symptoms of clotting or bleeding. Do not take aspirin. LEARNING OUTCOME 6 For each of the classes listed in Drugs at a Glance, know representative drug examples, and explain the mechanism of drug action, primary actions, and important adverse effects. Concepts 1. Parenteral Anticoagulants: prototype drug: heparin. The mechanism of action is to inhibit specific clotting factors, thereby interfering with the coagulation cascade and preventing formation or enlargement of clots. Within minutes after intravenous (IV) administration of heparin, the loss of activated clotting factors prevents the formation of fibrin clots. The primary use is to prevent formation of clots in veins and treat thromboembolic disorders. Adverse effects include abnormal bleeding. 2. The heparin molecule has been shortened and modified to create a newer class of drugs called lowmolecular-weight heparins (LMWHs). The mechanism of action of these agents is similar to that of heparin, except their inhibition is more specific to active factor X (see Figure 27.2). Their duration of action is two to four times longer than that of heparin. The LMWHs also produce a more stable response than heparin; thus, fewer follow-up lab tests are needed, and family members or the patient can be trained to give the necessary SC injections at home. These anticoagulants are less likely than heparin to cause thrombocytopenia. LMWHs have become the drugs of choice for a number of clotting disorders, including the prevention of DVT following surgery. 3. Other parenteral anticoagulants include the direct thrombin inhibitors argatroban (Acova, Novastan), bivalirudin (Angiomax), and lepirudin (Refludan). The mechanism of action is to bind to the active site of thrombin, preventing the formation of fibrin clots. The thrombin inhibitors have limited therapeutic uses. Adams_IRM Ch 27-3 4. Oral anticoagulants: prototype drug: warfarin (Coumadin). The mechanism of action is to inhibit the hepatic synthesis of coagulation factors II, VII, IX, and X. Often, patients begin anticoagulation therapy with heparin and are switched to warfarin when their condition stabilizes. When transitioning, the two drugs are administered concurrently for 2 to 3 days because warfarin takes several days to achieve optimum effect. Pentoxifylline (Trental) is another oral anticoagulant that works by a different mechanism than heparin. Pentoxifylline reduces the viscosity of red blood cells and increases their flexibility. It is given to increase the microcirculation in patients with intermittent claudication. The most frequent, and potentially serious, adverse effect of all the anticoagulant agents is bleeding. Specific antagonists may be administered to reverse the anticoagulant effects: protamine sulfate is used for heparin, and vitamin K is administered for warfarin (see the drug prototype features in this chapter). (See Table 27.3 for a list of anticoagulants.) 5. Antiplatelet drugs include aspirin, ADP blockers, glycoprotein 11b/111a receptor anatagonists, and miscellaneous agents for treating intermittent claudication. The prototype drug in the antiplatelet class is (ADP receptor blocker) clopidogrel (Plavix). The mechanism of action is to prolong bleeding time by inhibiting platelet aggregation directly inhibiting ADP binding to its receptor. The primary use is to prevent thromboembolic events in patients with a recent history of MI, CVA, or peripheral artery disease. It is also approved for thrombi prophylaxis in patients with unstable angina, including those who are receiving vascular bypass procedures or angioplasty. Adverse effects include abnormal bleeding. (See Table 27.4 for a list of antiplatelets.) 6. Thrombolytics are used to dissolve existing intravascular clots in patients with MI and CVA. The prototype drug in this class is altepase (Activase). The mechanism of action is to convert plasminogen to plasmin, which digests the fibrin and dissolves the clot. The primary uses are treatment of acute myocardial infarction (MI), deep vein thrombosis (DVT), cerebrovscular accident (CVA), pulmonary embolism, and arterial thrombosis and to clear intravenous (IV) catheters. Adverse effects include abnormal bleeding; it is contraindicated in patients with a bleeding disorder or who have had recent trauma or surgery. (See Table 27.5 for a list of thrombolytics.) 7. Hemostatics or antifibrinolytics are used to promote the formation of clots in patients with excessive bleeding from surgical sites. The prototype drug for this class is aminocaproic acid (Amicar). Its mechanism of action is to prevent fibrin from dissolving. The primary use is to prevent and treat excessive bleeding from surgical sites. Adverse effects include possible hypercoagulation with concurrent use of estrogens and oral contraceptives. Aminocaproic acid is contraindicated in patients with disseminated intravascular clotting or severe renal impairment. (See Table 27.5 for a list of hemostatics.) Table 27.3 Anticoagulants Table 27.4 Antiplatelet Agents Table 27.5 Thrombolytics Table 27.6 Hemostatics Prototype drugs heparin (parenteral) warfarin (oral) clopidogrel (Plavix) alteplase (Activase) aminocaproic acid (Amicar) Ch 27-4 Adams_IRM ANIMATIONS AND VIDEOS Mechanism in action: Warfarin (Coumadin) Mechanism in action: Heparin (Heplock) LEARNING OUTCOME 7 Use the nursing process to care for patients receiving drug therapy for coagulation disorders. Concepts 1. Patients receiving anticoagulant therapy—Assessment: Obtain a complete health history including any surgeries, drug therapy including herbal drugs, and dietary intake (especially note intake of vitamin K-rich foods and garlic). Assess coagulation studies initially and as therapy progresses. 2. Patients receiving anticoagulant therapy—Nursing Diagnoses: Pain (thrombosis and lessened perfusion); Ineffective Tissue Perfusion (decreased circulation); Impaired Skin Integrity (ineffective tissue perfusion); Anxiety; Deficient Knowledge (drug therapy); Risk for Injury (bleeding, related to adverse effects of anticoagulant therapy). 3. Patients receiving anticoagulant therapy—Planning: The patient will experience therapeutic effects dependent on the reason the drug is being given (e.g., prevention of thrombosis or limited extension of existing thrombosis); being free from, or experiencing minimal adverse effects, verbalizing an understanding of the drug’s use, adverse effects and required precautions and demonstrating proper selfadministration of the medication (e.g., dose, timing, when to notify provider). 4. Patients receiving anticoagulant therapy—Implementation: Monitor for adverse clotting reactions, skin necrosis, and cautious use in specific populations, monitoring for bleeding, monitoring of lab values, including prothrombin time (PT), international normalized ratio (INR), thrombin time, activated partial thromboplastin time (aPTT), and complete blood count (CBC). 5. Patients receiving anticoagulant therapy—Evaluation: The patient will experience a reduction in blood coagulation as noted in laboratory studies, be free from, or experience minimal adverse effects, demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider). Verbalize an understanding of the drug’s use, adverse effects, and required precautions, and verbalize an understanding of anticoagulant therapy. 6. Patients receiving thrombolytic therapy—Assessment: Obtain a complete health history, including trauma, allergies, drug history, and possible drug interactions. Obtain vital signs; assess in context of patient’s baseline values. Assess lab values: prothrombin time (PT), international normalized ratio (INR), thrombin time, activated partial thromboplastin time (aPTT), and complete blood count (CBC). 7. Patients receiving thrombolytic therapy—Nursing diagnoses: Pain (thrombosis and lessened perfusion); Ineffective Tissue Perfusion (decreased circulation); Impaired Gas Exchange (pulmonary emboli); Impaired Skin Integrity (ineffective tissue perfusion); Anxiety; Deficient Knowledge (drug therapy); Risk for Injury (bleeding and hemorrhage, related to adverse effects of thrombolytic therapy). 8. Patients receiving thrombolytic therapy—Planning: The patient will experience therapeutic effects dependent on the reason the drug is being given (e.g., reperfusion of coronary arteries, being free from or experiencing minimal adverse effects, verbalizing an understanding of the drug’s use, adverse effects and required precautions and demonstrating proper self-administration of the medication (e.g., dose, timing, when to notify provider). Adams_IRM Ch 27-5 9. Patients receiving thrombolytic therapy—Implementation: Monitor vital signs and ECG every 15 minutes during the first hour of infusion, and then every 30 minutes during the remainder of infusion and for the first 8 hours. Report any dysrhythmias immediately. Frequently check vital signs and assess for adverse effects of the drug including hypotension and tachycardia associated with bleeding and for dysrhythmias. Maintain the patient on bedrest and with limited activity during the infusion. (Limited physical activity and bedrest decrease the chance for bruising, injury and bleeding.) Monitor neurological status frequently, especially if thrombolytics are used for CVA. Avoid invasive procedures during infusion and up to 8 hours post-infusion when possible. (Any puncture site or site of invasive procedure will create an additional site for bleeding.) Whenever an invasive procedure must be used (e.g., ABGs), the site must be maintained under pressure for 30 minutes or longer to prevent hemorrhage. Monitor vital signs frequently; prevent injury; assess neurovascular and cardiovascular status frequently; monitor lab values including prothrombin time (PT); international normalized ratio (INR); thrombin time; activated partial thromboplastin time (aPTT); and complete blood count (CBC). 10. Patients receiving thrombolytic therapy—Evaluation: The patient experiences therapeutic effects dependent on the reason the drug is being given (e.g., reperfusion of coronary arteries). The patient is free from, or experiences minimal adverse effects; verbalizes an understanding of the drug’s use, adverse effects, and required precautions; and demonstrates proper self-administration of the medication (e.g., dose, timing, when to notify provider). Ch 27-6 Adams_IRM