Breast cancer survival paper
advertisement

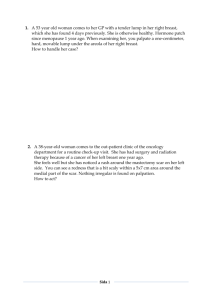
12 February 2008 Improvements in breast cancer survival over time, related to adjuvant treatment and node status. AK Imkampe*a, T Bates Breast Unit, William Harvey Hospital, Ashford, Kent TN24 0LZ, UK *Corresponding author. Breast Unit, William Harvey Hospital, Ashford, Kent TN24 0LZ, UK. Tel: 0044-1233-633331 Fax: 0044-1233-616019 e-mail address: a.imkampe@gmx.de a present address: 89 Hunter Road, Ashford, Kent, TN24 0RT, UK Summary Background: There has been an increase in the use and effectiveness of adjuvant treatment for operable breast cancer and the aim of this study was to examine whether this has resulted in improved survival for all prognostic groups. Methods: A retrospective study of 1517 patients with invasive breast cancer treated between 1980 and 2002 was carried out. The use of adjuvant treatment was compared between two time periods in patients divided by nodal status and survival was calculated by Kaplan-Meier Life Table Analysis. Independent predictors for Recurrence Free Survival (RFS) were determined by Cox regression analysis. Results: The use of adjuvant therapy increased for all prognostic groups. On multivariate analysis the use of radiotherapy and endocrine therapy was positively associated with RFS which was significant in the second time period. Outcome in node positive patients improved: Five-year RFS from 59% to 76%, p < 0.01 and Breast Cancer Specific Survival (BCSS) from 70% to 83%, p < 0.01. However, there was no survival improvement in the larger group of node negative patients; BCSS 93% versus 95%, p = 0.99. Within the node negative group, patients with tumours ≥ 2cm had an improved RFS from 80% to 88%, p < 0.02. Conclusion: The increased use of adjuvant therapy was associated with an improved outcome in node positive patients. For node negative patients with good prognostic features the evidence of benefit was marginal. Keywords: Breast cancer survival, lymph node status, adjuvant treatment 2 Introduction Breast cancer survival is improving [1] and studies have shown that use of adjuvant treatment is one of the main reasons. Chemotherapeutic drugs have become increasingly effective over the past decades and have produced a significant reduction in breast cancer mortality rates [2, 3]. This, in turn, has led to a general rise in the use of systemic adjuvant therapies [4]. But, depending on stage of the disease and tumour characteristics, there has been debate about the indications for and absolute benefit from adjuvant treatment in different prognostic groups. The present study examined two groups of patients, those who were node negative and those who were node positive at the time of diagnosis. The aim was to compare the use of adjuvant therapy between two time periods and to relate changes to differences in breast cancer recurrence and survival. 3 Methods Patient selection The study was a review of breast cancer patients diagnosed between 1980 and 2002. Patient details were collected prospectively on an actively managed database and the follow-up is near-complete. Only patients with operable breast cancer were included in the study and those who had no node status recorded, solely in situ carcinoma or bilateral disease were excluded. Tumour characteristics and adjuvant treatment The remaining 1517 patients were divided into two groups according to the nodal status at the time of diagnosis. The following data were compared for those with positive or negative nodes, between two time periods (1980 – 1995 and 1996 – 2002): median age, tumour type, tumour size, tumour grade, type of operation and the use of adjuvant chemotherapy, endocrine therapy and radiotherapy. The adjuvant chemotherapy regime in patients diagnosed during the first time period consisted of combination therapy with cyclophosphamide, methotrexate and 5fluorouracil (CMF). During the year of 1996 this was switched to the routine use of doxorubicin and cyclophosphamide (AC) when studies had confirmed the superiority of anthracycline combinations. Statistical analysis The results were analysed using the chi-square and Mann-Whitney U test. Time to first recurrence and length of survival were determined from the date of diagnosis until the date of recurrence or death or the last clinic date if no event had occurred. Data were included until July 2007. Median follow up time was 140 months 4 for patients diagnosed between 1980 and 1995 and 71 months for patients diagnosed between 1996 and 2002. The Kaplan-Meier method was used to calculate Recurrence Free Survival (RFS), Breast Cancer Specific Survival (BCSS) and Overall Survival (OS) and survival curves were compared using the log-rank test. Independent predictors for RFS were determined with Cox regression analysis. Differences were considered to be statistically significant at p < 0.05. 5 Results Overall survival improvement There was a significant improvement in RFS and BCSS when comparing the two time periods 1980 – 1995 and 1996 – 2002. RFS increased from 76% to 85% (HR 1.63, 95% CI 1.32 – 2.01, p < 0.01), and BCSS from 84% to 90% (HR 1.4, 95% CI 1.1 – 1.82, p < 0.01). Use of adjuvant therapy was significantly increased during the latter period, in both node positive and node negative patients including prognostic subgroups (Table 1). In Cox regression analysis the use of adjuvant radiotherapy and endocrine therapy were independent predictors for RFS irrespective of time period. In separate analyses use of radio- and endocrine treatment were significant in the second but not in the earlier time period (Table 2). Survival in node positive disease There was a higher proportion of infiltrating ductal carcinomas diagnosed during the earlier time period (88% versus 78%, p < 0.01, Table 3) but in general tumour characteristics for node positive patients were comparable between the two groups. Five-year RFS improved form 59% in the first to 76% in the second period (HR 1.92, 95% CI 1.46 – 2.53, p < 0.01), Figure 1. Local RFS alone increased from 84% to 95% (HR 2.97, 95% CI 1.74 – 5.25, p < 0.01). BCSS improved from 70% to 83% (HR 1.67, 95% CI 1.23 – 2.28, p < 0.01) and OS from 68% to 79% (HR 1.39, 95% CI 1.06 – 1.83, p = 0.02). Survival in node negative disease Node negative patients diagnosed during the second time period had on average smaller sized tumours (Table 3). BCSS and OS were similar in both time periods, 6 BCSS 93% versus 95% (HR 1.0, 95% CI 0.65 – 1.53, p = 0.99) and OS 89% in both time periods (HR 0.85, 95% CI 0.64 – 1.15, p = 0.3). Subgroup analysis of node negative patients by tumour size showed a significant difference in RFS for patients with tumours ≥ 2cm. Five-year RFS was 80% for patients diagnosed during the first compared to 88% for patients diagnosed during the second time period (HR 1.72, 95% CI 1.11 – 2.7, p = 0.02), Figure 2. There was no difference in RFS for patients with tumours < 2cm in size (93% versus 91%, HR 0.82, 95% CI 0.47 – 1.41, p = 0.46), Figure 3, and no difference in local RFS for this group (97% in both time periods, HR 1.07, 95% CI 0.44 – 2.63, p = 0.88). Subgroup analysis by tumour grade did not show any statistical difference in RFS for patients with Grade I tumours (95% in both periods, HR 1.29, 95% CI 0.58 – 2.98, p = 0.53) Grade II tumours (86% versus 91%, HR 1.23, 95% CI 0.73 – 2.07, p = 0.44) or Grade III tumours (82% versus 87%, HR 1.29, 95% CI 0.88 – 1.91, p = 0.19). 7 Discussion Adjuvant treatment and survival in node positive patients The present study shows that breast cancer recurrence rates and survival have significantly improved over time, correlating with a general increase in the use of adjuvant treatment in all prognostic groups and a switch from CMF to AC chemotherapy regimens. The importance of the increasing use of adjuvant radiotherapy and endocrine therapy on RFS in the second time period was confirmed in a multivariate analysis. The increased use of adjuvant chemotherapy did not show a significant improvement in outcome although there was a switch from CMF to anthracycline based therapy in 1966. This may explained by the limited number of patients in the present study but there may also have been unknown confounding factors not adjusted for in the Cox analysis. Hormone receptor status for example was not routinely determined during the first time period. The assessment of oestrogen-receptor (ER) status during the second time period would have enabled more targeted treatment with hormone medication thus explaining the survival advantage for patients diagnosed during this period. Subgroup analysis showed that survival advantages were maximal for node positive breast cancer patients and the beneficial effect of adjuvant treatment on this patient group has been reported in many studies [5-8]. Controversy in node negative patients However, the majority of patients who are diagnosed with breast cancer are node negative (62%) and these patients generally have a good prognosis. Within the node negative group there were more patients with small sized invasive cancers in the 8 second time period and this may be a reflection of the increasing number of patients diagnosed in screening programmes. There has been controversy about the appropriateness of adjuvant therapy in node negative patients and a number of studies have looked at the effectiveness of adjuvant radio-, chemo- or hormonal therapy in patients with good prognostic features. Some authors suggest that there may be subgroups of patients for whom adjuvant treatment is of no additional benefit [9-11] but Fisher et al [12] looked at survival in node negative patients with small tumours of 1cm or less and found that hormonal therapy and chemotherapy significantly improved RFS and BCSS in ER positive patients. A later report from the same study group showed that the addition of adjuvant chemotherapy to tamoxifen in ER positive patients significantly benefited pre- and postmenopausal node negative breast cancer patients, although the response to additional chemotherapy decreased in older women [13]. In the present study documentation of ER status in the earlier time period was insufficient for analysis but it is unlikely that the overall levels and distribution of hormone receptors was substantially different in the two periods. The EBCTC group [2] confirmed in a meta-analysis that endocrine treatment improves survival in ER positive disease and that chemotherapy is effective in all patients regardless of their nodal status or ER status and substantially reduces breast cancer mortality at 15 years. Radiotherapy has similarly been shown to reduce local recurrences in both node positive and node negative patients and to potentially produce improved overall survival at 15 years [3]. In the present study patients who had radiotherapy or a mastectomy had an improved (?local) RFS, as expected (Table 2). 9 Adjuvant treatment and survival in node negative patients by subgroups The length of follow up is known to be important in breast cancer and in patients with good prognostic features recurrences may occur many years after the initial diagnosis [14, 15]. Although studies have shown improved outcome for node negative patients in relation to adjuvant treatment, the absolute benefits are small and improved recurrence rates may only become apparent after 10 or more. The results of the current study correlate with these reports in the literature and there was no significant difference in survival of node negative patients between the two time periods after a median follow up of over 6 years in spite of the increased use of adjuvant treatment. Subgroup analysis by tumour size showed that RFS had improved partially in patients with large tumours at diagnosis but not in patients with small sized tumours of less than 2cm. There was a possible trend towards improved prognosis in patients with higher grade tumours but this did not reach statistical significance. In patients with good prognostic features (Grade I, ≤ 1cm), who have disease free survival rates reported between 88 - 95% after 9 - 10 years without systemic adjuvant treatment [16-18], the decision for appropriate adjuvant management may be challenging and the potential side effects have to be weighed against the expected benefit in the individual patient. Conclusion: Adjuvant treatment is effective in reducing recurrence and mortality in node positive breast cancer patients and in node negative patients with larger tumours. The outcome in node negative patients with low grade and small sized tumours is very good and it is difficult to improve on an already good prognosis in this patient group. 10 Literature 1 Peto R., Boreham J, Clarke M, Davies C, Beral V. UK and USA breast cancer deaths down 25% in year 2000 at ages 20 - 69 years. Lancet 2000; 355(9217):1822 2 Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;365(9472):1687-717 3 Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;366(9503):2087-106 4 Mariotto A, Feuer EJ, Harlan LC, Wun LM, Johnson KA, Abrams J. Trends in Use of Adjuvant Multi-Agent Chemotherapy and Tamoxifen for Breast Cancer in the United States: 1975-1999. J Natl Cancer Inst 2002;94:1626-34 5 Bonadonna G, Valagussa P, Moliterni A, Zambetti M, Brambilla C. Adjuvant cyclophosphamide, methotrexate, and fluorouracil in nodepositive breast cancer: the results of 20 years of follow-up. N Engl J Med 1995;332(14):901-6 6 Hartman AR, Fleming GF, Dillon JJ. Meta-analysis of adjuvant cyclophosphamide/methotrexate/5-fluorouracil chemotherapy in postmenopausal women with estrogen receptor-positive, node-positive breast cancer. Clin Breast Cancer 2001;2(2):138-43 11 7 Castiglione-Gertsch M, Johnsen C, Goldhirsch A, Gelber RD, Rudenstam CM, Collins J, Lindtner J, Hacking A, Cortes-Funes H, Forbes J, et al. The International (Ludwig) Breast Cancer Study Group Trials I-IV: 15 years follow-up. Ann Oncol. 1994;5(8):717-24 8 Berry DA, Cirrincione C, Henderson IC, Citron ML, Budman DR, Goldstein LJ, Martino S, Perez EA, Muss HB, Norton L, Hudis C, Winer EP. Estrogen-receptor status and outcomes of modern chemotherapy for patients with node-positive breast cancer. JAMA. 2006;295(14):1658-67 9 Boyages J, Taylor R, Chua B, Ung O, Bilous M, Salisbury E, Wilcken N. A risk index for early node-negative breast cancer. Br J Surg. 2006;93(5):564-71 10 Arnesson LG, Smeds S, Fagerberg G. Recurrence-free survival in patients with small breast cancer. An analysis of cancers 10mm or less detected clinically and by screening. Eur J Surg. 1994;160(5):271-6 11 Wood WC, Anderson M, Lyles RH, Styblo TM, Murray D, Staley C, Yang L, Carlson G. Ann Surg. 2002;235(6):859-62 12 Fisher B, Dignam J, Tan-Chiu E, Anderson S, Fisher ER, Wittliff JL, Wolmark N. Prognosis and treatment of patients with breast tumors of one centimeter or less and negative axillary lymph nodes. J Natl Cancer Inst. 2001;93(2):112-20 13 Fisher B, Jeong JH, Bryant J, Anderson S, Dignam J, Fisher ER, Wolmark N. Treatment of lymph-node-negative, oestrogen-receptor-positive breast cancer: long-term findings from National Surgical Adjuvant Breast and Bowel Project randomised clinical trials. Lancet. 2004;364(9437):858-68 12 14 Rosen PR, Groshen S, Saigo PE, Kinne DW, Hellman S. A long-term follow-up study of survival in stage I (T1N0M0) and stage II (T1N1M0) breast carcinoma. J Clin Oncol. 1989;7(3):355-66 15 Quiet CA, Ferguson DJ, Weichselbaum RR, Hellman S. Natural history of node-negative breast cancer: a study of 826 patients with long-term follow-up. J Clin Oncol. 1995;13(5):1144-51 16 Chia SK, Speers CH, Bryce CJ, Hayes MM and Olivotto IA. Ten-Year Outcomes in a Population-Based Cohort of Node-Negative, Lymphatic, and Vascular Invasion-Negative Early Breast Cancers Without Adjuvant Systemic Therapies. J Clin Oncol. 2004; 22(9):1630-7 17 Joensuu H, Isola J, Lundin M, Salminen T, Holli K, Kataja V, Pylkkanen L, Turpeenniemi-Hujanen T, von Smitten K, Lundin J. Amplification of erbB2 and erbB2 expression are superior to estrogen receptor status as risk factors for distant recurrence in pT1N0M0 breast cancer: a nationwide population-based study. Clin Cancer Res. 2003;9(3):923-30 18 Rosen PP, Groshen S, Kinne DW, Norton L. Factors influencing prognosis in node-negative breast carcinoma: analysis of 767 T1N0M0/T2N0M0 patients with long-term follow-up. J Clin Oncol. 1993;11(11):2090-100 13