Rabies Suspect Patient Protocol
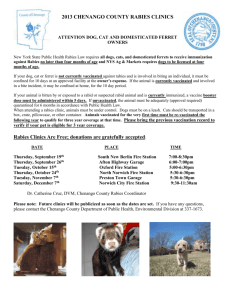
advertisement

Rabies Suspect Patient Protocol – Large Animal Rabies is a zoonotic disease that can cause a variety of clinical signs in affected animals. Clinical signs that should be considered suspicious of possible rabies infection in large animals include dysphagia (inability to swallow), dysphonia (alteration in voice), changes in behavior or demeanor, weakness, and unusual aggression. Large ruminants may be initially suspected of having an obstructed esophagus with salivation a prominent sign. Animals that present with clinical signs consistent with possible rabies infection should be treated as rabies suspects. The following protocol should be enforced for patients considered rabies suspects. 1. Only vaccinated personnel may come into direct contact with rabies suspects or positive animals. 2. A list of personnel that have come into contact with the suspect animal should be recorded and kept outside of the stall. 3. Suspect patients should be confined to their stalls and signage on stall entrances must clearly indicate each animal’s rabies status. 4. Personnel handling products associated with rabies suspect animals (e.g. bedding, linens, feed pans, water buckets, etc.) must be made aware of the patient’s status. 5. Affected animals may be handled only by operators wearing gloves, surgical masks, and protective glasses. After handling, operators should wash hands thoroughly. 6. Laboratory samples should be presented to the veterinary diagnostic laboratory with clear (written and verbal) indication that the samples are from a rabies suspect animal. Diagnostic specimens must be transported in leak-proof containers within leak proof plastic bags. The bags must be clearly marked as containing samples from suspect animals. 7. Animals that die or are euthanized while in rabies suspect status must have a mandatory necropsy examination that incorporates rabies testing. The VDL must be informed of the patient’s status in advance of receiving the carcass. Necropsy results should be reported to relevant parties as soon as they are released. 8. Products, such as fabric and porous items, should be presented to the RVP garage washer for initial laundering in a leak-proof bag clearly marked, Potential Rabies Case. 9. Linens and fabric items should be prewashed in the RVP garage washer before being presented to Central Sterile (CS) for further processing. Linens need only be washed in the RVP garage washer and may be delivered to CS bagged and wet. 10. The clinician in charge of the case must inform the Hospital Director and the LA Patient Services Manager that a suspect patient has been hospitalized. 1 Pre-Exposure Vaccination: Pre-exposure vaccination simplifies post-exposure prophylaxis by eliminating the need for rabies immune globulin (RIG) and may provide protection in the event that an exposure is not recognized. Veterinarians, veterinary technicians, and veterinary students in the College of Veterinary Medicine who come into contact with reservoir animals (dogs, cats [especially feral dogs and cats], skunks, raccoons, foxes, coyotes and bats), and workers in the Veterinary Diagnostic Laboratory who may come into contact with diagnostic specimens submitted for rabies evaluation are strongly encouraged to receive the rabies vaccine or these employees must sign a declination waiver. Since OSU faculty and students may travel internationally to perform their duties, faculty and staff fulfilling the following criteria should also be vaccinated: 1. Those going to countries where rabies is present and who intend to have regular contact with animals. 2. Those going to countries where rabies is endemic and who will be more than 24 hours away from a reliable source of post-exposure vaccine and care. Please note: Persons who are taking chloroquine derivatives as anti-malarial drugs should only receive the IM rabies vaccination, as these drugs suppress the immune response to ID rabies vaccine. Exposure Protocol: Pre-exposure vaccination does not eliminate the necessity to cleanse and treat bite wounds. Therefore hospital staff, students, and faculty exposed to possible rabies infections via splash or bite wounds should: 1. Thoroughly and promptly cleanse bite wounds with soap and water or flush eyes. Once bleeding has stopped or slowed sufficiently, providone-iodine or other virucidal antiseptic should be used liberally to irrigate the wounded area. 2. Where appropriate, post-exposure prophylaxis advice should be sought from a qualified medical professional. If injury occurs on or near the OSU main campus, students may go to the Student Health Services (SHS) during daytime hours; exposed employees and students after SHS closes should go to or be transported to the Samaritan Medical Center Emergency Department. 3. Bite victims should be treated promptly by medical professionals. Initial antirabies post-exposure prophylaxis needs to be administered within 24 hours of exposure. Post-Exposure prophylaxis is more intensive in non-vaccinated individuals but in both cases must be sought on the day of the incident for maximum efficacy. All possible rabies exposures must be reported to the employee’s supervisor, who is responsible for collecting appropriate documentation and reporting the incident in a timely manner. Bite/Accident and SAIF forms are in the LA Patient Services Manager’s office and LA Reception. Proper documentation consists of the following: 1. An Accident / Illness Report (form SAIF 801) must be filled out and forwarded to OSU Human Resources, following any exposure. 2. Oregon State Law requires that all animal bites be reported to the local health department within one (1) working day after the bite. In Benton County, 2 animal bites must be reported to the Benton County Health Department (BCHD). An animal bite reporting form is available on the BCHD, Environmental Health Division website, http://www.co.benton.or.us/health. 3. All animal bites that involve animals under the responsibility of the OSU Attending Veterinarian (i.e. all animals used for research or teaching) need to be reported to the campus Attending Veterinarian. More information regarding human rabies exposure can be found at http://oregonstate.edu/ehs/bio/HRPP.php. If you want to speak to someone about rabies exposure or have further questions contact OSU Environmental Health and Safety 541737-4557. Approved by the CVM-VTH Infectious Disease Committee, Date: September 24, 2009 Signature of Chair: ______________________________________________________ Date: ________________________________________________________________ 3