here - Student Nurse Laura
advertisement
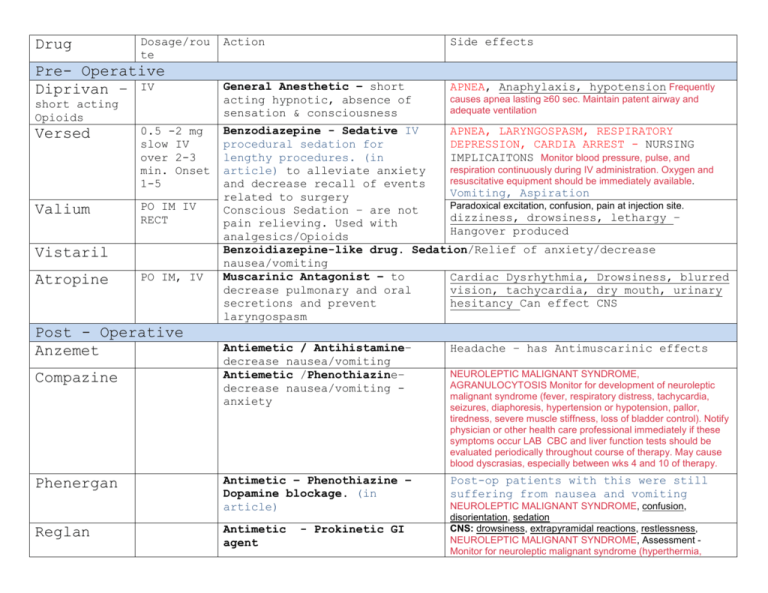
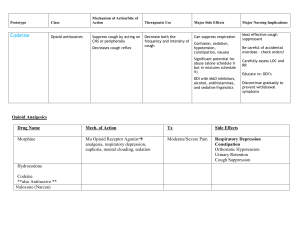
Drug Dosage/rou te Pre- Operative Diprivan – IV short acting Opioids Versed 0.5 -2 mg slow IV over 2-3 min. Onset 1-5 Valium PO IM IV RECT Vistaril Atropine PO IM, IV Post - Operative Anzemet Compazine Phenergan Reglan Action Side effects General Anesthetic – short acting hypnotic, absence of sensation & consciousness APNEA, Anaphylaxis, hypotension Frequently causes apnea lasting ≥60 sec. Maintain patent airway and adequate ventilation Benzodiazepine - Sedative IV APNEA, LARYNGOSPASM, RESPIRATORY procedural sedation for DEPRESSION, CARDIA ARREST - NURSING lengthy procedures. (in IMPLICAITONS Monitor blood pressure, pulse, and respiration continuously during IV administration. Oxygen and article) to alleviate anxiety resuscitative equipment should be immediately available. and decrease recall of events Vomiting, Aspiration related to surgery Paradoxical excitation, confusion, pain at injection site. Conscious Sedation – are not dizziness, drowsiness, lethargy – pain relieving. Used with Hangover produced analgesics/Opioids Benzoidiazepine-like drug. Sedation/Relief of anxiety/decrease nausea/vomiting Muscarinic Antagonist – to Cardiac Dysrhythmia, Drowsiness, blurred decrease pulmonary and oral vision, tachycardia, dry mouth, urinary secretions and prevent hesitancy Can effect CNS laryngospasm Antiemetic / Antihistamine– decrease nausea/vomiting Antiemetic /Phenothiazine– decrease nausea/vomiting anxiety Headache – has Antimuscarinic effects Antimetic – Phenothiazine – Dopamine blockage. (in article) Post-op patients with this were still suffering from nausea and vomiting Antimetic agent - Prokinetic GI NEUROLEPTIC MALIGNANT SYNDROME, AGRANULOCYTOSIS Monitor for development of neuroleptic malignant syndrome (fever, respiratory distress, tachycardia, seizures, diaphoresis, hypertension or hypotension, pallor, tiredness, severe muscle stiffness, loss of bladder control). Notify physician or other health care professional immediately if these symptoms occur LAB CBC and liver function tests should be evaluated periodically throughout course of therapy. May cause blood dyscrasias, especially between wks 4 and 10 of therapy. NEUROLEPTIC MALIGNANT SYNDROME, confusion, disorientation, sedation CNS: drowsiness, extrapyramidal reactions, restlessness, NEUROLEPTIC MALIGNANT SYNDROME, Assessment Monitor for neuroleptic malignant syndrome (hyperthermia, In addition, it is given to prevent nausea and vomiting caused by cancer chemotherapy and surgery. muscle rigidity, altered consciousness, irregular pulse or blood pressure, tachycardia, and diaphoresis. Opioid Antagonists – decrease severity of pain Phenanthrene – moderate to severe pain, pulmonary edema, MI Phenylpiperidine – IM, patch, wide variation in client response avoid with older adults Diphenylheptane – dosing for maintenance of opioid dependence 20120mg/daily-avoid older Adverse effects/Side effects Nursing Implications/Labs/Assessments Route/dose Drug Use with extreme caution in constipation RESPIRATORY DEPRESSION confusion, sedation, Moderate to Morphine patients receiving MAO hypotension, severe pain sulfate inhibitors (may result in For overdose – Narcan 0.4mg IV unpredictable, severe, and Constipation – increase water consumption 2000ml/daily, fiber in diet. Class: potentially fatal reactions-mobility decrease initial dose to Phenanthre 25% of usual dose). ne Nursing Implications High Narcotic Alert: Assess level of Tylenol analgesic – mild consciousness, blood w/codeine to severe pain. pressure, pulse, and respirations before and (#3, 4) Metabolizes to periodically during administration. If Phenanthre morphine respiratory rate is ne <10/min, assess level of Dizziness, weakness, nausea – Narcan for overdose sedation. Physical Darvocet-N stimulation may be Diphenylhe sufficient to prevent significant hypoventilation. ptane Subsequent doses may IV - Rate: High Alert: SEIZURES, confusion, sedation hypotension, bradycardia. need to be decreased by Demerol GI: constipation, nausea, vomiting RESPIRATORY DEPRESSION. Administer slowly over at 25-50%. Phenylpipe least 5 min. Rapid Hypertension, muscle rigidity, coma, seizures, hyperpyrexia, death. Implementation administration may lead to Avoid combinations ridine High Alert: Accidental increased respiratory Dilaudid Also a Antitussive depression, hypotension, and circulatory collapse Rate: Administer slowly, at a rate not to exceed 2 mg over 3-5 min. High Alert: Rapid administration may lead to increased over dosage of opioid analgesics has resulted in fatalities. Before administering, clarify all ambiguous orders; have second practitioner independently check discontinue MAO inhibitors 2 wk prior to hydromorphone). Assessment Assess blood pressure, pulse, and respirations before and periodically during administration. If respiratory rate is <10/min, assess level of sedation. Dose may need to be decreased by 25-50%. Initial drowsiness will diminish with continued use Phenanthre ne respiratory depression, hypotension, and circulatory collapse. Faster acting, but shorter lasting original order, dose calculations, and infusion pump settings. Vicodin Implementation Monitor daily High Alert: Accidental overdosage of opioid analgesics has resulted in fatalities. Before administering, clarify all ambiguous orders; have second practitioner independently check original order and dose calculations. RESPIRATORY DEPRESSION. Assess blood pressure, pulse, and respirations before and periodically during administration. If respiratory rate is <10/min, assess level of sedation. Physical stimulation may be sufficient to prevent significant hypoventilation. Dose may need to be decreased by 25-50%. Initial drowsiness will diminish with continued use Narcan for overdose Phenanthren e Percodan Phenanthren e Percocet Phenanthren e Fentanyl Patch, RESPIRATORY DEPRESSION, dizziness, drowsiness nausea Should not be used within 14 days of MAO inhibitors because of possible severe and unpredictable reactions Toxicity and Overdose: naloxone (Narcan) is the antidote. Phenylpiper idine Partial Opioids Agonist-Antagonists Nubain – less On set 1-3 minutes IV Opioid analgesics - decrease pain potent analgesics, lower dependency potential tan opiods. Use with extreme caution in patients receiving MAO inhibitors (may result in unpredictable, severe reactions--reduce initial dose of nalbuphine to 25% of usual dose). Naloxone (Narcan) antidote overdose Implementation High Alert: Accidental overdose of opioid analgesics has resulted in fatalities. Before administering, clarify all ambiguous orders; have second practitioner independently check original order, dose calculations, and infusion pump settings. Opioid Antagonist Narcan Direct IV: Diluent: Administer undiluted for suspected opioid overdose. For opioid-induced respiratory depression, dilute with sterile water for injection Antidote for opioids – reversal fo signs of opioid overdose/excess 0.4mg IV is usually ordered Opioid-like Drug Ultram Renal Impairment PO (Adults): CCr <30 ml/min--increase dosing to q 12 hr (not to exceed 200 mg/day). Analgesics (centrally acting) – inhibits reuptake SEIZURES, dizziness, headache, somnolence constipation, nausea Monitor patient for seizures. May occur within recommended dose range. Risk is increased with higher doses and in patients taking antidepressants (SSRIs, tricyclics, or MAO inhibitors), opioid analgesics, or other drugs that decrease the seizure threshold. Hepatic Impairment PO (Adults):50mg q 12hr. of serotonin and norepinephrine in cns. Decreased pain Narcan may reduce some, but not all symptoms of overdose Analgesics Tylenol Non opioid Analgesics, antipyretic – mild pain, fever HEPATIC FAILURE, HEPATOTOXICITY (OVERDOSE). Acetaminophen intake > 4 grams daily What is a MAO? Antidepressants - MAO Inhibitors: When other antidepressants don't work, some people find relief from an older class of medications - MAO inhibitors. Monoamine oxidase inhibitors (MAOIs) were the first type of antidepressant to be used, starting in the 1950s Opioid Antagonist– binds to Opioids receptors and competitively displace the Opioids analgesics from their receptor sites. Emergency Treatment. Guedel’s Stages of Anesthesia Stage Stage 1: Analgesia (administration to LOC) Stage 2: Excitement (Vary depending on: type/amount premedication. Anesthetic agent used. Degree of external stimuli) Stage 3: Surgical Anesthesia Stage 4: Medullary Paralysis Alternative Nomenclature Induction Plane 1 Plane 2 Plane 3 Plane 4 Toxicity Key Features Nursing Management Analgesia/numbness Loss of senses Auditory/visual hallucinations Exaggerated reflexes Client may struggle Periods of apnea Vomiting or incontinence may occur Reduced with use of balanced anesthesia Maintain tranquil environment Eye movement stops Partial intercostals paralysis Divergent pupil dilation Complete intercostals paralysis Diaphragmatic paralysis Respiratory arrest Vasomotor collapse Maintain airway Protect against aspiration (Most surgical procedures happen here) Maintain airway Protect against aspiration Resuscitation