- D

RESERVOIR-TARGETED STRATEGIES TO CONTROL ZOONOTIC
DISEASES IN THE U.S.
by
Ali Bashir Na-Shatal
M.B.Ch.B, Tripoli University, Libya, 2003
Submitted to the Graduate Faculty of
Graduate School of Public Health in partial fulfillment of the requirements for the degree of
Master of Public Health
University of Pittsburgh
2015
UNIVERSITY OF PITTSBURGH
GRADUATE SCHOOL OF PUBLIC HEALTH
This essay is submitted by
Ali Bashir Na-Shatal on
May 4, 2015
Essay Advisor:
David Finegold, MD ______________________________________
Director, Multidisciplinary MPH Program
Professor, Department of Human Genetics
Graduate School of Public Health
University of Pittsburgh
Essay Reader:
Ronald Voorhees, MD, MPH ______________________________________
Professor of Public Health Practice, Epidemiology
Associate Dean for Public Health Practice, Office of the Dean
Graduate School of Public Health
University of Pittsburgh ii
Copyright © by Ali Bashir Na-Shatal
2015 iii
David Finegold, MD
RESERVOIR-TARGETED STRATEGIES TO CONTROL ZOONOTIC DISEASES IN
THE U.S
.
Ali Bashir Na-Shatal, MPH
University of Pittsburgh, 2015
ABSTRACT
The causative agents of zoonotic diseases are maintained in nature in an ongoing enzootic cycle between wildlife reservoirs and vectors. Over the past decade, zoonotic diseases in the U.S. have become a significant public health threat and a financial burden indicating that the current preventive measures against zoonotic diseases are not sufficient, therefore; further measures must be considered to reduce human risk. Recently, vaccines, acaricides, antibiotics, and contraceptives distributed in the landscape targeting wildlife reservoirs have been proven to be safe and effective in controlling rabies and Lyme disease in wildlife reservoirs. Furthermore, similar efforts are under research to control West Nile Virus in birds. This review is intended to explore the recent efforts to control the three major zoonotic diseases in the U.S., Rabies, Lyme disease and West Nile Virus, and present past, present and future reservoir-targeted strategies to control zoonotic diseases in the United States. iv
TABLE OF CONTENTS
1.0 INTRODUCTION ...............................................................................................................1
2.0 RABIES .................................................................................................................................2
2.1 EPIDEMIOLOGY OF RABIES IN THE U.S. ..……………………….…………..2
2.2 ORAL RABIES VACCINATION ..…………………………….…………………..4
2.3 NATONAL RABIES MANAGEMANT PROGRAM ..…….……………………..6
2.4 ORAL RABIES VACCINES………………………………………………………...8
2.4.1 Raboral ..........…………………………………………………..…………….8
2.4.2 Ontario Rabies Vaccine Bait ( ORNAB) ....…………………………………8
3.0 LYME DISEASE .................................................................................................................9
3.1 EPIDEMIOLOGY OF LYME DISEASE IN THE U.S. .........................................9
3.2 ACARICIDES ...........................................................................................................11
3.2.1 Four-poster delivery systems (Deer self treatment devices) .....................11
3.2.2 Bait Box Study ...............................................................................................12
3.3 ANTIBIOTICS ..........................................................................................................13
3.4 ORAL LYME DISEASE VACCINE.......................................................................13
4.0 WEST NILE VIRUS ..........................................................................................................14
4.1 EPIDEMIOLOGY OF WEST NILE VIRUS IN THE U.S. .................................14
4.2 WEST NILE VIRUS RESERVIOR TARGETED VACCINES .............................1
6 v
5.0 DISSCUSION .....................................................................................................................17
6.0 FUTURE RESEARCH ......................................................................................................18
6.1 GonaCon ....................................................................................................................18
6.2 Bait Distribution .......................................................................................................18
7.0 SUMMARY ....................................................................................................................... 19
BIBLIOGRAPHY .......................................................................................................................20 vi
LIST OF FIGURES
Figure 1: CDC annual reports of rabid animals and human rabies in the U.S. (2010-2013) ........3
Figure 2: Map of terrestrial rabies reservoirs in the U.S ...............................................................3
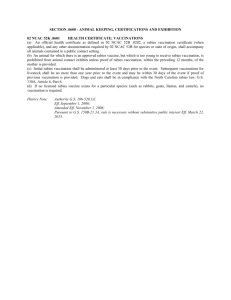
Figure 3: States involved in the ORV national program ...............................................................7
Figure 4: Distribution of Lyme disease in the U.S ........................................................................9
Figure 5: Reported cases of Lyme disease in the U.S 1995-2013 ...............................................10
Figure 6: West Nile Virus cases and deaths reported to CDC .....................................................15 vii
1.0 INTRODUCTION
Nearly 75% of recently emerging infectious diseases affecting humans are diseases of animal origin, and almost 60% of all human pathogens are zoonotic [1]. In the United States, zoonotic diseases have become a major public health issue and a significant financial burden over the past decade . Preventive measures to control zoonotic diseases represent a collaborative effort between sectors responsible for public health, animal health, and environmental safety.
The current efforts to control zoonotic diseases mostly rely on public education, pet vaccination, and vector control. While effective, theses preventive measures are insufficient, therefore; an additional strategy seems imperative to reduce public health risks from zoonoses. Although human prophylaxis and treatment for zoonotic diseases are effective in some cases, they are costly and often overprescribed. Furthermore, human vaccines have no effect on preventing potential spread of zoonotic disease into new geographical locations.
Reservoir-targeted strategies, on the other hand, are designed to target main reservoirs of zoonoses in wildlife animals and break the enzonotic cycle of such disease. Furthermore, reservoir-targeted strategies halt potential spread of infectious diseases into new locations and spillover into newer species.
Over the past 20 years, a growing interest in targeting wildlife reservoirs had led to the development of new strategies that could compliment the current preventive measures to control zoonotic diseases . Most of these strategies rely on the use oral baits that contain vaccines, antibiotics, acaricides or contraceptives that target specific pathogens in specific species.
Furthermore, reservoir-targeted strategies have been considered more effective and practical than lethal control of wildlife reservoirs [2]. Since rabies, Lyme disease, and West Nile Virus represent the major zoonotic diseases in the U.S., reservoir-targeted strategies in the U.S. have
1
focused primarily on developing medicinal baits that could be distributed in the landscape and reduce the population of infected reservoirs for such diseases.
Oral rabies vaccination (ORV) programs represent the most well established reservoirtargeted strategies to control zoonotic diseases in the United States. Since the late 1990s, ORV programs have expanded from few states in the U.S. to cover 16 states in 2015. Reservoirtargeted strategies to control Lyme disease and West Nile Virus, on the other hand, are still in their early phase of research and development and do not rely primarily on oral vaccines.
2.0 RABIES
2.1 EPIDEMIOLOGY OF RABIES
Human rabies is caused by lyssaviruses, usually as a result of an infected animal bite, and is associated with a high case fatality rate. However, rabies is 100% preventable when rabies post-exposure prophylaxis (PEP) is administered soon after exposure. Initial symptoms include fever, fatigue, and hydrophobia. Late complications range from neurological symptoms to death.
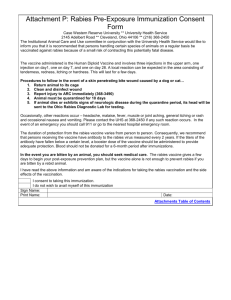
Globally, it is estimated that 50,000 to 70, 000 deaths per year are attributed to rabies infection. Because of an extensive surveillance system, pet vaccination programs, and PEPs in the U.S., human rabies is extremely rare, 2-3 cases per year, where most cases are due to overseas exposure. Although there has been a slight decline in the annual numbers of rabid animals reported to the Centers for Disease Control and Prevention (CDC), the current numbers being reported are still significant and represent a public health risk (Figure 1). This indicates that the virus is maintained in nature and the current preventive measures are insufficient in eliminating rabies in wildlife animals.
2
Figure (1) CDC annual reports of rabid animals and human rabies in the U.S. (2010-2013)
In the U.S., raccoons represent the most reported rabid animal (36.5%), followed by skunks (23.5%), bats (23.2%), and foxes (7%) [3]. Rabies variant’s geographical distribution is a key element in targeting reservoirs. Raccoon rabies variant exists in eastern United States, while the fox variant is confined in Texas, Arizona, and Alaska. Skunk rabies is distributed over a larger geographical area in central United States and California, which makes efforts to control skunks rabies challenging (figure 2).
Figure (2) Map of terrestrial rabies reservoirs in the U.S
(adapted from CDC website)
3
PEP represents the last line of defense in preventing human rabies, and with more rabid animals being reported; more PEPs are being prescribed, especially during epizotics.
Furthermore, PEPs are considered to be overprescribed and costly, therefore; represent a major financial burden on the public health sector. The annual costs of rabies PEPs are estimated to range from $25 million to $65 million per year.
As long as the rabies virus is maintained in wildlife animals, it will remain a threat to the public, therefore; reservoir-targeted strategies to control rabies represent the ultimate method to reduce human risks and lower financial burdens caused by rabies prophylaxis.
2.2 ORAL RABIES VACCINATION
Over the past 30 years, wildlife vaccination campaigns to control rabies have gained more acceptance by the public health sector, and proven to be more practical and cost effective than lethal control strategies [4]. The goal of wildlife vaccination is to generate herd immunity among wildlife animals in an effort to reduce the population of infected animals, halt the spread of infection to new geographical locations, and prevent spillover to other competent species.
Efforts to develop an oral rabies vaccine for wildlife vaccinations began as early as in
1971, when researchers examined the effectiveness and safety of using a live attenuated virus vaccine in foxes [5]. Subsequently, researchers examined the feasibility of incorporating such vaccines into sausage baits to develop an edible vaccine for field distribution [6].
In 1978, researchers in Switzerland conducted the first field study using live attenuated rabies vaccines by catching and vaccinating red foxes [7]. Although the study was time consuming, laborious, and unsuccessful, the Switzerland rabies program is considered a milestone in the history of wide-scale vaccination of wildlife against rabies.
4
Following the Switzerland field study, researchers began to develop edible vaccines that could be deployed on a larger scale without having to catch, vaccinate, and release animals.
However, live rabies vaccines were proven to be pathogenic to skunks [8] and ineffective in some raccoon species such as the Procyon lotor , most commonly found in North America [8].
Therefore, safety and efficacy concerns urged researchers to develop recombinant vaccines instead of live rabies vaccines.
In 1986, Rupprecht et al . demonstrated the safety and efficacy of oral immunization of raccoons using a vaccinia-rabies glycoprotein (V-RG) recombinant virus vaccine [9]. In laboratory settings, the team demonstrated that the oral recombinant vaccine produced a longterm protection against rabies virus challenge tests, and they suggested that further field-testing could demonstrate the cost-benefits of wide-scale distribution of such vaccine.
During 1989-1990 in Belgium, Brocheir et al . conducted the first field study to evaluate the effectiveness of oral recombinant vaccines against rabies in foxes [10]. The vaccine used was a recombinant vaccinia virus expressing rabies glycoprotein (G), the same vaccine that is used in the U.S. today (Raboral
TM
). The results from this study indicated complete eradication of rabies in southern Belgium after 2 years of vaccine distribution.
Even though the concept of wildlife vaccination was introduced to the CDC during the
1960s, the first field trial in the U.S., using a recombinant vaccine, was carried out in 1990 on
Parramore Island, Virginia, USA [11]. The raccoon population were exposed to a high density
(10 baits/ha) of vaccine-laden baits distributed on a 300 ha vaccination area. The results reinforced safety data from previous laboratory studies and facilitated the licensing of V-RG, the only licensed oral vaccine for use in wildlife in the U.S.
5
2.3 NATONAL RABIES MANAGEMANT PROGRAM
Commercial availability of an oral vaccine in the mid-1990s, and safety results from initial field trails had lead to more oral rabies vaccination initiatives by local health departments and universities to control the raccoon variant of rabies in Ohio, New York, Vermont, Maryland,
Massachusetts, Florida, and Texas [12], however; resources were limited at that time mainly from the CDC.
Wildlife Services initial involvement in (ORV) programs began in 1995 in south Texas to prevent canine rabies in coyotes. However, over the subsequent 2 years the WS became more involved with several other states. To ensure effectiveness and long term planning, the WS formed a multidisciplinary National Rabies Management Program in 1997.
The program consisted of WS research personnel (National Wildlife Research Center), expertise from CDC, cooperating states, and universities. In 1998, WS’s national rabies management program
(NRMP) received its first federal funds designated for rabies control [13, 14].
In 1999, three index cases of raccoon rabies were confirmed in Ontario, Canada [15], an issue that urged the WS to seek increased federal funding as well as additional funding from other resources such as the Commodity Credit Corporation (CCC) and the APHIS Contingency
Fund to extend ORV zones and stop raccoon rabies from moving south into Ohio.
In 2000, the WS proposed the following; an expansion of vaccination zones along the
Canadian border, an extension of the current Ohio vaccination zone south into West Virginia to tie the Appalachian Mountains and prevent raccoon variant form spreading west, and provide additional federal funding to assist Texas with its ORV gray fox project.
The ultimate goal of the ORV zone expansion was to create a barrier from lake Erie south to the high mountains of eastern Tennessee that will prevent raccoon-variant rabies from
6
spreading westward, also known as the Appalachian Ridge project. Additionally, the national
ORV program was set to include eastern Pennsylvania, where raccoon-variant rabies was considered enzootic, and for the first time to operate in a major U.S. metropolitan city, the city of
Pittsburgh.
While the initial funds received by the WS for rabies control were estimated at 1.3 million dollars to cover New York, Ohio, Texas, and Vermont, the 2014 funds reached 28 million and the WS’s National Rabies Management Program is currently operating in 16 states
(Fig 3). Although the costs of rabies control in the U.S. are variable, CDC estimates suggest that over 300 million dollars annually are spent on rabies control. These costs include pet vaccination, animal control, rabies laboratories maintenance, and medical costs. Furthermore,
CDC estimates suggest that about 40,000 PEPs are administered annually in the U.S. resulting in over 150 million dollars spent on health care costs [16] [17]. Recent cost benefit studies by WS suggest that stopping the westward spread of raccoon rabies alone could reduce PEP costs by as much as $50 million dollars each year [17].
Figure (3) States involved in the ORV national program, adapted from Wildlife Services
7
2.4 ORAL RABIES VACCINES
2.4.1 Raboral
SAG
2
and VR-G vaccines are currently the only rabies vaccines that fulfill the World
Health Organization’s requirements for anti-rabies guidelines. While SAG
2
, a live rabies vaccine, is used in countries other than the U.S., Raboral V-RG is the only licensed oral rabies vaccine for field distribution. The vaccine, which is a recombinant vaccinia virus derived from the
Copenhagen strain of vaccinia virus, expresses the genetic sequence of rabies glycoprotein
(VVTGgRAB). The rabies glycoprotein (G) is an envelope protein, which is the major antigen responsible for eliciting humoral response [18] .
Raboral V-RG is distributed in the form of a fishmeal sachet containing a vaccine and a tetracycline biomarker that is used to trace uptake.
2.4.2 Ontario Rabies Vaccine Bait ( ORNAB)
Although skunks represent a major host for rabies virus in the U.S., the current efforts are mostly intended for raccoons, coyotes, and foxes. The National Rabies Management Program only uses Raboral V-RG, which although effective in raccoons, coyotes, and foxes, it has been proven to be ineffective in skunks [19]. ONRAB on the other hand , an oral live human adenovirus-rabies glycoprotein recombinant vaccine, which has been used extensively in
Canada, is equally effective against rabies in raccoons and skunks.
In 2014, Brown et al.
demonstrated that ONRAB is safe and effective in captive striped skunks (Mephitis mephitis). Furthermore, some studies suggest that ONRAB is even more effective than Raboral V-RG in controlling raccoon rabies [20].
The WS has recently conducted its first field trial using ONRAB in West Virginia to evaluate the safety and efficacy of ONRAB. Although the results affirmed safety of ONRAB, the
8
results were inconclusive, which has led to second field trials in Vermont, New Hampshire, New
York, and Ohio. To date, no current data have been published.
3. LYME DISEASE
3.1 EPIDEMIOLOGY OF LYME DISEASE IN THE U.S.
Lyme disease is caused by Borrelia burgdorferi , a spirochete that is transmitted among rodents via ticks such as Ixodes scapularis. Humans are an accidental and dead end host, acquiring infection as a result of an infected tick bite. Since the identification of the causative agent of
Lyme disease by W. Burgdorferi in 1982 [21], the number of Lyme disease cases has increased dramatically in the U.S., mostly in the northeastern states (Figures 4 and 5). In 1991, Lyme disease was listed as a nationally reportable disease by the CDC. Lyme disease represents more than 90% of the reportable vector-borne diseases and is the fifth most reportable diseases with approximately 30,000 confirmed cases per year [22]. However, the CDC recently updated its estimated yearly Lyme disease incidences to 300,000 probable cases to account for underreporting and misdiagnosis.
Figure (4) Distribution of Lyme disease in the U.S, adapted from CDC website
9
JHSV
Figure (5) Reported cases of Lyme disease in the U.S 1995-2013 (adapted from CDC website)
Lyme disease commonly presents with fatigue and headache with or without a febrile illness. A characteristic sign is a skin rash referred to as erythema migrans. The most common demographic are male children. A history of a tick bite in an endemic area is highly significant during diagnosis. If untreated, Lyme disease could lead to serious complications involving the joints, heart, and central nervous system (facial palsy or cranial neuritis). On the other hand,
Lyme disease could be successfully treated with the proper course of antibiotics soon after exposure.
Human risk for acquiring B. burgdorferi infection in any given geographic location is directly proportional to the infected tick density [23, 24, 25]. Meanwhile, the current measures to control Lyme disease such as public education, tick avoidance, pest control, and implementation of surveillance systems have proven to be insufficient since Lyme disease incidences have
10
dramatically increased over the past decade and spread into new geographical locations in the
U.S. such as Minnesota, Pennsylvania, and Wisconsin [26]. Such data underscore the importance of reservoir-targeted stratigies to reduce human risk from Lyme disease.
Although human vaccines for Lyme disease have been developed, none are available for distribution today, mostly due to commercial reasons. Furthermore, a human vaccine would not reduce infected tick density in endemic areas, therefore; a human vaccine cannot stop the spread of B. burgdorferi into new geographic locations.
In order to reduce the financial burden and human risk that Lyme disease poses, and to stop the spread of infected ticks and reservoirs into new geographical locations, reservoirtargeted strategies represent the ultimate strategy to break the enzootic cycle and reduce Lyme disease in the U.S..
Over the past decade, public health officials and researchers have explored new and effective strategies to quell the current rise in Lyme disease incidence in the U.S. The success of oral rabies vaccination campaigns have influenced researchers to approach Lyme disease using similar strategies, targeting the main reservoir through a wide comprehensive campaign.
In northeastern U.S., white-footed mice, Peromyscus leucopus , are considered the critical reservoir of B. burgdorferi [27, 28, 29], and other less significant hosts, such as deer, squirrels and raccoons are considered not competent [30]. Therefore white-footed mice have been the main targets for research and field studies to reduce infected tick density in the U.S..
3.2 ACARICIDES
3.2.1 Four-poster delivery systems (Deer self treatment devices)
In Maryland, New Jersey, Connecticut, and New York [31-34] several field studies, supported by the CDC, examined the efficacy and feasibility of a passive topical treatment of
11
white-tallied deer using an acaricide 2% (amitraz). Four-poster feeders, harboring acaricides, were used to attract white-tailed deer while topical amitraz was passively applied to deer. The results were promising as most studies presented data that suggest a dramatic reduction in tick population compared to control areas. However, all studies seemed to have insufficient data in terms of follow up.
3.2.2 Bait Box Study
Bait boxes have been used as a remote method of reservoir-targeted acaricide delivery to reduce tick infestation on white-footed mice. Such boxes contain an acaricide, fipronil, that has been proven to be effective in reducing tick infestation on white-footed mice and reduce B. burgdorferi [35].
Dolan et al. conducted a 3-yr community-based study on Mason's Island, Mystic, CT, to evaluate the effectiveness of fipronil bait boxes in controling immature Ixodes scapularis on
Peromyscus leucopus.
Results showed that bait boxes were effective in reducing nymphal and larval tick infestations on white-footed mice by 68 and 84%, respectively. The study also indicated that B. Burgdorferi infection among white-footed mice were decreased significantly
[36].
In 2013, the Center for Disease Control and Prevention conducted a similar Bait Box study on a larger scale in Connecticut by collaborating with local health departments and universities. The aim of the study was to evaluate the effectives of rodent-targeted tick control using the commercially available SELECT TCS™ TICK CONTROL SYSTEM bait boxes. Two types of boxes were being used; bait boxes with an acaricide fipronil and placebo bait boxes. The bait boxes were randomly distributed to 500 households. No official results have been published yet, however; the study is expected to be concluded in 2015.
12
3.3 ANTIBIOTICS
The use of antibiotics to target wildlife reservoirs is a highly debatable issue, mostly due to resistance and efficacy concerns. However, in the laboratory setting Donlan et al. demonstrated 100% prevention in tick-transmitted infection among C3H/HeJ mice by feeding mice doxycycline hyclate baits. Furthermore, doxycycline baits were effective in achieving clearance of spirochete infection in infected mice [37]. Because of these promising laboratory results, the same group conducted a field trial in New Jersey using a novel reservoir-targeted method that involves the distribution of doxycycline-laden baits. The aim was to reproduce the laboratory results in a field setting. After 2 years, results indicated a reduction in B. burgdorferi infection rates in reservoir rodents by approximately 87% and a reduction in B. burgdorferi infection rates in ticks by approximately 94%.
3.4 ORAL LYME DISEASE VACCINE
Although there are no licensed reservoir-targeted vaccines for Lyme disease, there are several studies testing the efficacy and safety of reservoir-targeted Lyme disease vaccines. The goal of these studies is to develop oral vaccines that can be distributed remotely in Lyme endemic areas and generate herd immunity among reservoirs against B. burgdorferi.
Reservoir-targeted Lyme disease vaccines are under extensive research; these vaccines are based on B. burgdorferi outer surface antigen (OspA), which has been proven to be an efficient immunogen in eliciting immunity against B. burgdorferi [38, 39].
In laboratory setting, either vaccinia based or E. coli based vaccines expressing the OspA have been tested in mice to evaluate their efficacy in producing immunity. Results indicate that vaccines expressing OpsA could provide complete protection against B. burgdorferi infection in mice, and reduce carriage in infected ticks that fed on vaccinated mice [40, 41].
13
Although laboratory results were promising, the use of vaccinia based vaccines has not been field tested due to safety concerns. In 1998, Tsao et al. carried out the first field trial in the
U.S. using a recombinant B. burgdorferi OspA vaccine . The vaccine was administered to trapped mice, which were evaluated two years later to test the efficacy of OspA vaccines in providing immunity in white-footed mice, and whether or not OspA vaccines can reduce B. burgdorferi infection in ticks. The results indicated that immunizing whited-footed with OspA vaccines reduced B. burgdorferi infection among nymphal ticks by approximately 24% [42].
Direct vaccination of reservoirs remains impractical, especially for large-scale vaccination campaigns. Oral baits, on the other hand, serve as a better alternative for mass distribution and achieving a wider range of Lyme disease control. To overcome such limitations, an OspA-based, oral vaccines have been developed and field-tested over the last 5 years. To test the hypothesis that transmission of B. burgdorferi to humans can be disrupted by targeting 2 key elements in its enzootic cycle: the reservoir host and the tick vector, Richer et al. conducted a prospective 5-year field trial in New York, using an oral reservoir-targeted bait. The bait consisted of an E.coli
expressing OspA, water, and an oatmeal bait. Their results showed an
OpsA specific seropositivity, which has lead to a significant reduction in nypmphal infection prevalence [43].
4.0 WEST NILE VIRUS
4.1 EPIDEMIOLOGY OF WEST NILE VIRUS IN THE U.S.
West Nile virus (WNV) is an arbovirus that belongs to the family Flaviviridae. Like all arboviruses, WNV cause fever, headaches and malaise. If untreated, the virus can lead to neurological complications (neuro-invasive disease)
14
The virus is maintained in nature by mosquito-bird-mosquito transmission. There are more than 60 mosquito species and 350 bird species that have been identified as vectors and competent hosts respectively for WNV. Horses and humans are considered accidental and dead end hosts.
The virus first appeared in the U.S in 1999 in New York City [44] and spread to the East coast in 2003 [45, 46]. In 2014, WNV cases have been reported to the CDC by 47 states and the
District of Columbia. Currently, WNV infections are the most arboviral diseases reported to
CDC and the main causes of neuroinvasive arboviral disease in the U.S. [47, 48]. Although the number of WNV cases has declined slightly over the last three years, more than 2100 cases and
80 deaths occurred annually since 2012 (Figure 5). Such data highlight the importance of reservoir-targeted strategies to control WNV in the U.S.
Figure (6) West Nile Virus cases and deaths reported to CDC (2010-2014)
15
4.2 WEST NILE VIRUS RESERVIOR TARGETED VACCINES
A human or horse vaccine would limit the number of West Nile Virus infection in humans and horses only since they are dead end hosts. In other words, horse or human vaccines cannot control WNV cycle in nature. A reservoir-targeted strategy, on the other hand, could reduce the amount of infected reservoirs and reduce human risk. Birds are the main reservoir for
WNV, and are also considered an amplifying reservoir . There are no evidences that animals other than birds can develop enough virus load to transmit infection to mosquitos.
Even though birds are considered the main reservoir in maintaining the life cycle of
WNV, to date there is no WNV vaccine approved for avian use. Currently, there are few studies evaluating the efficacy of vaccines approved for horses in birds, however; these efforts are intended to protect certain species from extinction, not to control the risk of human infection with WNV.
Wheeler et al. evaluated the efficacy of several vaccines in Western Scrub-Jays
( Aphelocoma californica ). They used the commercially available WNV vaccine for horses West
Nile-Innovator (killed virus), an experimental DNA plasmid vaccine pCBWN, and a recombinant WNV vaccine Merial Recombitek WNV equine vaccine, which has been recently approved by USDA for horse use. Overall, results suggested a significant reduction in viremia in vaccinated birds following a WNV challenge [49]
To date, the only laboratory study that has been conducted to test the efficacy of WNV vaccine in birds to protect extinction and consider the possible effect on human risk was carried out by Young et al (50). They tested a recombinant WNV vaccine consisting of a non-replicating recombinant adenoviruse expressing WNV envelope genes in Japanese Quail ( Coturnix japonica ). Results suggested that vaccination of Japanese quail increased humoral and cellular
16
immune responses against WNV, and vaccination of birds may protect against extinction of an endangered avian species and minimizes the amount of reservoirs that pose a threat to humans .
Such strategies will not only reduce the risk of WNV infections among humans, but will enhance our preparedness for all vector-born pathogens.
5.0 DISSCUSION
Reservoir-targeted strategies to control zoonotic diseases in the U.S. are expensive, however; they have been considered an effective strategy to stop spread of infected reservoirs into new locations, reduce human risk, and reduce costs for treatments and prophylaxis.
For example, because of the national ORV program a potential westward spread of raccoon rabies from eastern states was prevented, grey fox rabies is only reported in west central
Texas, and no rabid coyotes have been reported since 2004 [51]. Furthermore, most economic assessments and modeling studies indicate that ORV programs can yield cost savings mostly as a result of fewer PEPs during epizotics [52, 53, 54]. A recent benefit-cost analysis of the results of the domestic dog and coyote oral rabies vaccine (ORV) program in Texas from 1995 through
2006 was carried out to determine potential savings (avoided costs) yielded by the program. Data indicate that the total estimated benefits of the program ranged from $89 million to $346 million, with total program costs of $26,358,221 for the study period [55].
To date, data for cost benefits of reservoir-targeted strategies to control Lyme disease or
WNV infection are unavailable, partly because such strategies are still in their trial phase.
However, the CDC is currently conducting a Cost of Lyme Disease study (COLD study) to estimate the cost of Lyme disease and is expected to be concluded in 2016.
17
6.0 FUTURE RESEARCH
6. 1 GonaCon
The National Wildlife Research Center has been investigating the use of contraceptives similar to GonaCon as means for wildlife population control. Currently, efforts are intended to develop an oral contraceptive that could help control wildlife reservoirs of zoonotic diseases.
GonaCon is registered with the Environmental Protection Agency (EPA) for restricted use in white-tailed deer in urban/suburban areas and is considered to have no significant ecological impact since it is only licensed for parental administration (56). An oral GonaCon would have to be designed to be target specific because of the potential ecological effects on non-target species.
6.2 Bait Distribution.
Most baits that have been used in ORV are distributed aerially. Such methods of distribution are not suitable in suburban areas and could be replaced with less costly and more effective methods. In 2015, Smyser et al. developed an automated fishmeal bait dispensers designed to target raccoon’s dexterity and limit non-target species. The team monitored dispensers placed in three different forest patches in northwest Indiana. Results showed that more than 70% of the baits were removed by raccoons, and 11% were removed by white-footed mice (52). These results favor the use of automated dispensers in suburban areas rather than aerial distribution. Furthermore, dispensers could be modified and used to distribute Lyme disease vaccines to target white-footed mice. Telford et al. have investigated another method for bait distribution. They concluded that wooden nest boxes could effectively deliver peanut butter scented baits to white-footed mice as a mean for an oral Lyme disease vaccine (57)
18
7.0 SUMMARY
In conclusion, zoonotic diseases are a significant public health and a financial burden in the U.S. The current preventive measures to control zoonotic diseases are not sufficient and reservoir-targeted strategies represent an additional effective mean to control zoonotic disease and reduce human risk.
Although effective and cost beneficial, reservoir-targeted strategies require further research and improvement. For example, ORV programs should consider adding another type of vaccines such as ORNAB to target skunks or add contraceptives to their campaigns to further reduce human risk. ORV programs should also consider incorporating Lyme disease vaccines or acaricides baits into their programs that operates in areas where both diseases poses public health risks. Nest boxes can be used for ORV and Lyme disease vaccines in suburban areas where aerial distribution is not feasible. Additionally, Reservoir-targeted strategies to control Lyme disease should consider other important hosts such as chipmunks, squirrels, and birds.
Furthermore, Lyme disease vaccines would be more effective if they include outer surface antigens other than OspA such as OspC to cover a wider range of B. burgdorferi serotypes.
Although WNV incidences do not represent a significant threat to the public as rabies and Lyme disease do, establishing a well-developed WNV vaccination programs for birds could become useful in controlling other arboviruses diseases. The infrastructure of reservoir-targeted strategies could involve more than one type of baits and provide an effective platform to control major zoonotic diseases in the U.S
19
BIBLIOGRAPHY
1.
The control of neglected zoonotic diseases. (n.d.). Retrieved February 16, 2015, from http://www.who.int/zoonoses/control_neglected_zoonoses/en/
2.
The potential of oral vaccines for disease control in wildlife species. Cross ML, Buddle BM,
Aldwell FE. Vet J.
2007 Nov;174(3):472-80.
3.
Rabies Surveillance Data in the United States. (2011, November 15). Retrieved February 16,
2015, from http://www.cdc.gov/rabies/location/usa/surveillance/index.html
4.
Aubert, M.F., 1999. Cost and benefits of rabies control in wildlife in France. Rev Sci Tech
18, 533-543.
5.
Baer GM, Abelseth MK, Debbie JG. Oral vaccination of foxes against rabies.
Am J
Epidemiol .
1971 Jun;93(6):487-90.
6.
Baer GM, 1976. The oral rabies immunization of foxes and dogs with sausage baits. Dev Biol
Stand 33:417-23.
7.
Steck F, Wandeler A, Bichsel P, Capt S, Schneider L.Oral immunisation of foxes against rabies. A field study.
Zentralbl Veterinarmed B .
1982 Jun;29(5):372-96.
8.
Rupprecht CE, Charlton KM, Artois M, Casey GA, Webster WA, Campbell JB, Lawson KF,
Schneider LG.1990 Ineffectiveness and comparative pathogenicity of attenuated rabies virus vaccines for the striped skunk (Mephitis mephitis). J Wildl Dis 26(1):99-102.
9.
Rupprecht CE, Wiktor TJ, Johnston DH, Hamir AN, Dietzschold B, Wunner WH, Glickman
LT, Koprowski H. Oral immunization and protection of raccoons (Procyon lotor) with a vaccinia-rabies glycoprotein recombinant virus vaccine.
Proc Natl Acad Sci U S A.
1986
Oct;83(20):7947-50.
10.
Brochier B, Kieny MP, Costy F, Coppens P, Bauduin B, Lecocq JP, Languet B, Chappuis G,
Desmettre P, Afiademanyo K, et al. Large-scale eradication of rabies using recombinant vaccinia-rabies vaccine.
Nature .
1991 Dec 19-26;354(6354):520-2.
20
11.
Hanlon CA, Niezgoda M, Hamir AN, Schumacher C, Koprowski H, Rupprecht CE, 1998
First North American field release of a vaccinia-rabies glycoprotein recombinant virus. J
Wildl Dis 34(2):228-39.
12.
Wildlife Damage. http://www.aphis.usda.gov/wps/portal/aphis/ourfocus/wildlifedamage?1dmy&urile=wcm:pat h:/aphis_content_library/sa_our_focus/sa_wildlife_damage/sa_programs/sa_nrmp/ct_rabies
13.
Slate D, Rupprecht CE, Rooney JA, Donovan D, Lein DH, Chipman RB. Status of oral rabies vaccination in wild carnivores in the United States. Virus Res. 2005 Jul;111(1):68-76.
Epub 2005 Apr 21.
14.
D. Slate, R.B. Chipman, C.E. Rupprecht, T. DeLibertoOral rabies vaccination: a national perspective on program development and implementationR.M. Timm, R.H. Schmidt (Eds.),
Proceedings of the 20th Vertebrates Pest Conference, University of California, Davis (2002), pp. 232–240.
15.
Rosatte R, Donovan D, Allan M, Howes LA, Silver A, Bennett K, MacInnes C, Davies C,
Wandeler A, Radford B. Emergency response to raccoon rabies introduction into Ontario. J
Wildl Dis . 2001 Apr;37(2):265-79.
16.
Cost of Rabies Prevention. (2011, April 22). Retrieved April 29, 2015, from http://www.cdc.gov/rabies/location/usa/cost.html
17.
Oral Rabies Vaccination. (n.d.). Retrieved April 30, 2015, from http://www.aphis.usda.gov/wps/portal/aphis/ourfocus/wildlifedamage/sa_programs/sa_nwrc/ sa_research/sa_rabies/ct_orv_vaccination/!ut/p/a0/04_Sj9CPykssy0xPLMnMz0vMAfGjzOK
9_D2MDJ0MjDzd3V2dDDz93HwCzL29jAwMTfQLsh0VAXWczqE!/
18.
Wunner WH, Dietzschold B, Curtis PJ, Wiktor TJ. Rabies subunit vaccines. J Gen Virol .
1983 Aug;64 (Pt 8):1649-56.
19.
Grosenbaugh DA, Maki JL, Rupprecht CE, Wall DK. Rabies challenge of captive striped skunks (Mephitis mephitis) following oral administration of a live vaccinia-vectored rabies vaccine. J Wildl Dis.
2007 Jan;43(1):124-8.
20.
Brown LJ, Rosatte RC, Fehlner-Gardiner C, Ellison JA, Jackson FR, Bachmann P, Taylor JS,
Franka R, Donovan D. Oral vaccination and protection of striped skunks (Mephitis mephitis) against rabies using ONRAB®.
Vaccine . 2014 Jun 17;32(29):3675-9.
21.
W. Burgdorfer, A.G. Barbour, S.F. Hayes, J.L. Benach, E. Grunwaldt, J.P. Davis. Lyme disease – a tick-borne spirochetosis? Science, 216 (1982), pp. 1317–1319.
22.
Bacon RM, Kugeler KJ, Mead PS; Centers for Disease Control and Prevention (CDC)
Surveillance for Lyme disease--United States, 1992-2006. MMWR Surveill Summ. 2008 Oct
3;57(10):1-9.
21
23.
Diuk-Wasser MA1, Hoen AG, Cislo P, Brinkerhoff R, Hamer SA, Rowland M, Cortinas R,
Vourc'h G, Melton F, Hickling GJ, Tsao JI, Bunikis J, Barbour AG, Kitron U, Piesman J,
Fish D. Human risk of infection with Borrelia burgdorferi, the Lyme disease agent, in eastern
United States. Am J Trop Med Hyg .
2012 Feb;86(2):320-7. doi: 10.4269/ajtmh.2012.11-
0395.
24.
Stafford KC III, Cartter ML, Magnarelli LA, Ertel SH, Mshar PA. Temporal correlations between tick abundance and prevalence of ticks infected with Borrelia burgdorferi and increasing incidence of Lyme disease. J Clin Microbiol 1998; 36:1240–4.
25.
Ginsberg HS. Transmission risk of Lyme disease and implications for tick management. Am
J Epidemiol . 1993 Jul 1;138(1):65-73.
26.
Bacon RM, Kugeler KJ, Mead PS. Surveillance for Lyme disease--United States, 1992-2006.
MMWR Surveill Summ. 2008 Oct 3;57(10):1-9.
27.
Anderson JF. Ecology of Lyme disease. Conn Med . 1989 Jun;53(6):343-6.
28.
LoGiudice K, Ostfeld RS, Schmidt KA, Keesing F.The ecology of infectious disease: effects of host diversity and community composition on Lyme disease risk. Proc Natl Acad Sci U S
A. 2003 Jan 21;100(2):567-71.
29.
Levine JF, Wilson ML, Spielman A. Mice as reservoirs of the Lyme disease spirochete. Am.
J. Trop. Med. Hyg . 1985;34:355–360.
30.
Matuschka FR, Heiler M, Eiffert H, Fischer P, Lotter H, Spielman A. Diversionary role of hoofed game in the transmission of Lyme disease spirochetes. Am J Trop Med Hyg . 1993
May;48(5):693-9.
31.
Carroll JF, Allen PC, Hill DE, Pound JM, Miller JA, George JE.Control of Ixodes scapularis and Amblyomma americanum through use of the '4-poster' treatment device on deer in
Maryland. Exp Appl Acarol.
2002;28(1-4):289-96.
32.
Schulze TL, Jordan RA, Hung RW, Schulze CJ. Effectiveness of the 4-Poster passive topical treatment device in the control of Ixodes scapularis and Amblyomma americanum (Acari:
Ixodidae) in New Jersey. Vector Borne Zoonotic Dis . 2009 Aug;9(4):389-400. doi:
10.1089/vbz.2008.0160.
33.
Stafford KC 3rd, Denicola AJ, Pound JM, Miller JA, George JE. Topical treatment of whitetailed deer with an acaricide for the control of Ixodes scapularis (Acari: Ixodidae) in a
Connecticut Lyme borreliosis hyperendemic Community. Vector Borne Zoonotic Dis.
2009
Aug;9(4):371-9. doi: 10.1089/vbz.2008.0161.
34.
Stafford KC 3rd, Denicola AJ, Pound JM, Miller JA, George JE. Topical treatment of whitetailed deer with an acaricide for the control of Ixodes scapularis (Acari: Ixodidae) in a
22
Connecticut Lyme borreliosis hyperendemic Community. Vector Borne Zoonotic Dis. 2009
Aug;9(4):371-9.
35.
CDC, Bait Box Study (Connecticut) (2013, June 5). Retrieved April 10, 2015, from http://www.cdc.gov/ticknet/ltdps/ltdps_bait.html
36.
Dolan MC, Maupin GO, Schneider BS, Denatale C, Hamon N, Cole C, Zeidner NS, Stafford
KC 3rd. Control of immature Ixodes scapularis (Acari: Ixodidae) on rodent reservoirs of
Borrelia burgdorferi in a residential community of southeastern Connecticut. J Med Entomol.
2004 Nov;41(6):1043-54.
37.
Dolan MC, Zeidner NS, Gabitzsch E, Dietrich G, Borchert JN, Poché RM, Piesman J. A doxycycline hyclate rodent bait formulation for prophylaxis and treatment of tick-transmitted
Borrelia burgdorferi. Am J Trop Med Hyg . 2008 May;78(5):803-5.
38.
Fikrig E, Barthold SW, Kantor FS, Flavell RA Long-term protection of mice from Lyme disease by vaccination with OspA.. Infect Immun . 1992 Mar;60(3):773-7.
39.
de Silva AM, Telford SR 3rd, Brunet LR, Barthold SW, Fikrig E Borrelia burgdorferi OspA is an arthropod-specific transmission-blocking Lyme disease vaccine . J Exp Med.
1996 Jan
1;183(1):271-5.
40.
Scheckelhoff MR, Telford SR, Hu LT. Protective efficacy of an oral vaccine to reduce carriage of Borrelia burgdorferi (strain N40) in mouse and tick reservoirs. Vaccine . 2006 Mar
10;24(11):1949-57.
41.
Gomes-Solecki MJ, Brisson DR, Dattwyler RJ. Oral vaccine that breaks the transmission cycle of the Lyme disease spirochete can be delivered via bait.
Vaccine .
2006 May
15;24(20):4440-9.
42.
Tsao JI,Wootton JT, Bunikis J, Luna MG, Fish D, Barbour AG. An ecological approach to preventing human infection: vaccinating wild mouse reservoirs intervenes in the
Lyme disease cycle. Proc Natl Acad Sci U S A 2004; 101:18159-64
43.
Richer LM, Brisson D, Melo R, Ostfeld RS, Zeidner N, Gomes-Solecki M. Reservoir targeted vaccine against Borrelia burgdorferi: a new strategy to prevent Lyme disease transmission. J Infect Dis. 2014 Jun 15;209(12):1972-80. doi: 10.1093/infdis/jiu005. Epub
2014 Feb 11.
44.
Nash D, Mostashari F, Fine A, et al. The outbreak of West Nile virus infection in the New
York City area in 1999. N Engl J Med . 2001;344(24): 1807-1814.
45.
Lindsey NP, Staples JE, Lehman JA, Fischer M. Surveillance for human West Nile disease,
MMWR Surveill Summ. 2010;59(2):1-17.
23
46.
Petersen LR, Hayes EB.West Nile virus in the Americas. Med Clin North Am . 2008;92(6):
1307-1322; ix.
47.
Reimann CA, Hayes EB, DiGuiseppi C, et al. Epidemiology of neuroinvasive arboviral disease in the United States, 1999–2007. Am J Trop Med Hyg 2008;79:974–9.
48.
Nicole P. Lindsey, MS, Jennifer A. Lehman, J. Erin Staples, MD, Marc Fischer, MD. West
Nile Virus and Other Arboviral Diseases — United States, 2013. June 20, 2014 / 63(24);521-
526.
49.
Sarah S. Wheeler, Stanley Langevin, Leslie Woods, Brian D. Carroll, Winston Vickers, Scott
A. Morrison, Gwong-Jen J. Chang, William K. Reisen, and Walter M. Boyce. Efficacy of
Three Vaccines in Protecting Western Scrub-Jays ( Aphelocoma californica ) from
Experimental Infection with West Nile Virus: Implications for Vaccination of Island Scrub-
Jays ( Aphelocoma insularis ) Vector Borne Zoonotic Dis. 2011 Aug; 11(8): 1069–1080.
50.
Young JA, Jefferies W. Towards the Conservation of Endangered Avian Species: A
Recombinant West Nile Virus Vaccine Results in Increased Humoral and Cellular Immune
Responses in Japanese Quail. PLoS One. 2013 Jun 25;8(6):e67137. doi:
10.1371/journal.pone.0067137. Print 2013.
51.
Sterner RT, Meltzer MI, Shwiff SA, Slate D. Tactics and economics of wildlife oral rabies vaccination, Canada and the United States. Emerg Infect Dis [serial on the Internet]. 2009
Aug [ date cited ]. Available from http://wwwnc.cdc.gov/eid/article/15/8/08-1061 DOI:
10.3201/eid1508.081061.
52.
Uhaa IJ, Data VM, Sorhage FE, Beckley JW, Roscoe DE, Gorsky RD, Benefits and costs of using an orally absorbed vaccine to control rabies in raccoons. J Am Vet Med Assoc.
1992;201:1873–82. NJ PEP
53.
Kreindel SM, McGill M, Meltzer MI, Rupprecht CE, DeMaria A. The cost of rabies postexposure prophylaxis: one state’s experience.
Public Health Rep.
1998;113:247–51.
54.
Shwiff SA, Kirkpatrick KA, Sterner RT. Economic evaluation of a Texas oral rabies vaccination program for control of a domestic dog–coyote rabies epizootic: 1995–2006. J Am
Vet Med Assoc . 2008;233:1736–41.
55.
National Service Center for Environmental Publications. Retrieved April 30, 2015, from http://nepis.epa.gov/Exe/ZyNET.exe/P1008DPF.txt?ZyActionD=ZyDocument&Client=EPA
&Index=2006Thru2010&Docs=&Query=&Time=&EndTime=&SearchMethod=1&TocRestr ict=n&Toc=&TocEntry=&QField=&QFieldYear=&QFieldMonth=&QFieldDay=&UseQFiel d=&IntQFieldOp=0&ExtQField
56.
Smyser TJ, Redding JV Jr, Bevis CM, Page LK, Swihart RK. Development of an Automated
Dispenser for the Delivery of Medicinal or Vaccine-Laden Baits to Raccoons (Procyon lotor). J Wildl Dis . 2015 Apr;51(2):513-8. doi: 10.7589/2014-08-211. Epub 2015 Feb 3.
24
57.
Telford SR 3rd, Cunningham JA, Waltari E, Hu L. Nest box-deployed bait for delivering oral vaccines to white-footed mice. Ticks Tick Borne Dis . 2011 Sep;2(3):151-5.
25