SONOGRAPHY OF THE HAND AND WRIST - e
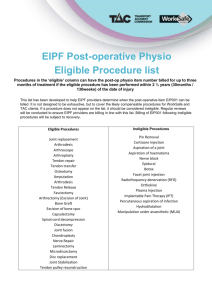
advertisement

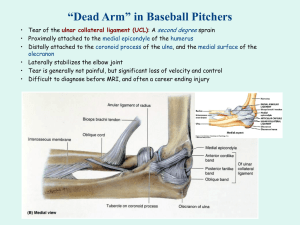
HAND AND WRIST SONOGRAPHY UPDATED – PART II Author: Sharlene A. Teefey, M.D. Objectives: Upon the completion of this CME article, the reader will be able to 1. Identify the sonographic appearance of the pertinent musculoskeletal anatomy of the normal hand and wrist. 2. Describe the sonographic appearance of the various forms of tenosynovitis and injuries to the hand. 3. Identify Dupuytren’s contracture and foreign bodies sonographically. Tenosynovitis: Tenosynovitis is a common problem of the hand and is due to inflammation of the synovial lining of a tendon sheath. Whereas this condition is usually idiopathic, other etiologies may include inflammatory arthritis (rheumatoid arthritis), crystalline tendonopathy (calcific tenosynovitis or gout), deposition diseases (amyloidosis), and infectious tenosynovitis (bacterial, mycobacterial, viral). Although controversial, work-related microtrauma has also been implicated as a cause for tenosynovitis. In general, sonographic findings include tendon sheath fluid and or debris, nodularity, and sheath thickening. Hypervascular changes may be observed in the tendon or a thickened synovium with color Doppler sonography. In advanced cases of tenosynovitis, the tendon may also become involved, which predisposes it to tendon rupture (figures 1 and 2). Rheumatoid arthritis is a common cause of inflammatory tenosynovitis. The hand and or wrist may be involved in up to 64% to 95% of patients with this condition. Patients usually present with painless swelling at the site of involvement. The third, fourth, fifth and sixth extensor compartments, or the flexor tendons, are typically involved. Gout and calcific tendonitis are two of the more common causes of crystalline tendonopathy, but gouty tenosynovitis of the hand is uncommon in patients whose disease has been well managed. This condition can involve the flexor or extensor tendons of the hand. Patients typically present with pain, erythema and swelling. Although the cause of calcific tenosynovitis is unclear, it has been suggested that repetitive microtrauma is a prerequisite for intratendinous calcium deposits. These deposits are usually asymptomatic until they are released into the synovial space, where they incite an inflammatory response. Symptoms are similar to those reported with gout. Tenosynovitis of the hand is common in patients with amyloidosis. Plaque like deposits along the flexor tendons, either within the carpal tunnel or digits, can lead to median nerve compression or trigger finger and flexion contracture, respectively. Patients typically present with painless swelling along the affected tendon. Acute suppurative tenosynovitis is often caused by a penetrating injury but may also be hematogenous in origin. It frequently occurs in immunologically compromised patients or individuals with diabetes. The infectious process usually begins in the distal flexor tendon sheath but may extend proximally. The most common infecting organism is Staphylococcus aureus. Historically, Kanavel described four classic signs and symptoms of a flexor tendon sheath infection: a flexed finger position, diffuse swelling of the finger, extreme tenderness over the course of the flexor tendon sheath, and pain with passive finger extension. The differential diagnosis includes cellulitis or a local abscess. At sonography, tendon sheath fluid (consisting of purulent material), subcutaneous edema, and tendon enlargement may be evident. Surrounding hyperemic changes can also be seen with color Doppler sonography. If the clinical diagnosis is uncertain, aspiration of tendon sheath fluid can be performed under sterile conditions using sonographic guidance. If a focal fluid collection suggestive of an abscess is detected at sonography, it must be drained surgically. Chronic tenosynovitis as the result of mycobacterial or fungal infections can also cause synovial thickening that can be demonstrated by sonography. However, tendon sheath fluid is usually absent in chronic tenosynovitis related to infection. Tenosynovitis may be caused by work-related, repetitive microtrauma; however, this etiology is controversial. Patients with rheumatoid arthritis, diabetes mellitus, calcium pyrophosphate deposition disease, gout, hypothyroidism, tuberculosis, fungal infections, or collagen vascular disease are at increased risk for the development of work-related tenosynovitis. Any of the six-extensor compartments may be involved. In the flexor compartment, the flexor carpi ulnaris or radialis or the digital flexor tendons are most commonly involved. Patients usually present with pain on motion, tenderness, swelling, and crepitus. At sonography, synovial sheath fluid and thickening are seen. Two specific syndromes, De Quervain’s disease and trigger digit, represent the more common types of idiopathic tenosynovitis. De Quervain's disease involves the first extensor compartment (abductor pollicis longus and extensor pollicis brevis tendon sheaths) at the level of and proximal to the radial styloid process. This condition is more common in women than in men (a ratio of 6 to 1) and usually occurs between 30 and 50 years of age. Patients will present with pain along the radial side of the wrist (that increases with movement of the thumb) and tenderness and swelling approximately 1 to 2 cm proximal to the radial styloid. At sonography, tendon sheath fluid is observed, as well as a thickened, hypoechoic sheath. The tendon itself is usually normal in echotexture. Trigger digit is another idiopathic tenosynovitis. Pathological changes include fibrocartilaginous metaplasia at the level of the A1 pulley (metacarpophalangeal joint) and the flexor tendon surface. It occurs more commonly in women than in men (a ratio of about 4 to 1) and has a peak incidence between 40 and 60 years of age. The thumb is most commonly affected followed by the ring, long, little, and index fingers. Most patients will present with pain and with triggering and or locking of the digit. Sonographic findings include tendon thickening, a hypoechoic nodule on the flexor tendon surface proximal to the A1 pulley, synovial sheath thickening and fluid, and small peritendinous cysts. Treatment of idiopathic tenosynovitis, including De Quervain’s syndrome and trigger finger, is usually conservative using splinting, non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, warm soaks and possibly steroid injections. Surgery is reserved for patients with persistent symptoms who fail conservative therapy. Tendinous and Ligamentous Injuries of the Hand: Two of the more common injuries to the hand, flexor tendon avulsion and ulnar collateral ligament injury not only can be diagnosed by sonography, but the findings can also be used to direct management and surgical approach. Traumatic avulsion of the flexor digitorum profundus tendon, usually in the ring finger, occurs commonly in young male athletes when there is forced extension of the digit during maximum contraction of the profundus muscle. This results in an inability to flex the distal interphalangeal joint. Early surgical repair is important for a good outcome. At sonography, it is important to identify the location of the avulsed tendon end. It typically is retracted back into the palm, or to the level of the proximal phalanx (A2 pulley), or to the middle phalanx (A4 pulley). Tendon rupture is diagnosed on ultrasound when the normal tendon cannot be identified in its expected location (figures 3 and 4). Sonography is extremely useful for identifying the location of the proximal torn tendon end, which can help to minimize the length of the initial surgical incision. The simplest method for locating the proximal tendon is to initiate imaging in a transverse plane at the distal aspect of the finger and then scan proximally until a mass is encountered. That mass will represent the blunt tip of the proximal tendon. The ulnar collateral ligament (UCL) of the metacarpophalangeal joint of the thumb is most commonly injured during skiing. The mechanism of injury is a sudden, forceful abduction (the thumb moving out from the hand or away from the other fingers) of the already abducted thumb, usually from falling with a ski pole in the hand. The tear typically occurs near the proximal phalangeal insertion of the tendon. Two types of UCL tears may occur: 1) the nondisplaced type in which the torn UCL remains beneath the adductor aponeurosis; or 2) the displaced type in which the torn UCL lies superficial and at the proximal margin of the adductor aponeurosis. The displaced type of UCL tear is referred to as a Stener lesion. This distinction is important because non-displaced or incomplete tears may be treated conservatively with a cast for four to six weeks, whereas displaced tears require surgical repair. The anatomy of the metacarpophalangeal region of the thumb is complex, but it is essential to have an understanding of the relationship of the UCL to the adductor aponeurosis. The UCL arises from the ulnar side of the metacarpal head and inserts on the proximal phalanx. The adductor aponeurosis, which is the tendinous portion of the adductor pollicis muscle of the thumb, inserts on the base of the proximal phalanx of the thumb and the UCL lies underneath the adductor aponeurosis. Its distal two-thirds is covered by the first interosseous dorsalis muscle. Thus, the longitudinal axis of the aponeurosis is perpendicular to the long axis of the ligament. Sonography has been reported to be accurate not only in differentiating nondisplaced from displaced UCL tears, but also partial tears from complete tears. Dupuytren's Contracture: Dupuytren's contracture is an idiopathic, benign proliferative disorder that results in fibrous tissue deposition in the palmar aponeurosis of the hand. It occurs in the fibrofatty layer between the skin and deep palmar structures, resulting in the formation of nodules, that over time, develop into longitudinal cords. Whereas advanced stages of the disease are easily diagnosed clinically, in the early stage, these nodules may be indistinguishable from other pathologic processes of the hand, such as a Giant Cell Tumor. At sonography, these subcutaneous nodules are hypoechoic and oriented longitudinally to the digit. Foreign Bodies: Foreign bodies in the hand are usually caused by penetrating injuries and, if radiopaque (glass, metal, stone) are readily diagnosed on plain radiographs. However, radiolucent foreign bodies such as wood may not be visible radiographically, but are easily detected with ultrasound. Sonography is quite sensitive and specific in detecting all types of foreign bodies. It is important to orient the transducer perpendicular to the long axis of the foreign body to optimally visualize it. Glass and metal are often echogenic and produce a comet-tail artifact whereas wood is usually hyperechoic with posterior acoustic shadowing. If the foreign body has been present for a few days or weeks, a surrounding hypoechoic inflammatory reaction will often occur and may help to localize the foreign body. However, chronically embedded wood fragments may not be visible within a fluid collection, perhaps because of fluid absorption by the wood itself that alters the sonographic appearance (figures 5 and 6). Figures: 1 and 2 Tenosynovitis of the extensor compartment of the extensor digitorum and indices. 3 and 4 Rupture of the flexor digitorum profundus. 5 and 6 Foreign body (sliver of wood) in the palm of the hand. References or Suggested Reading: 1. Teefey SA, Middleton Wd, pateel V, et al. The accuracy of high-resolution ultrasound for evaluating focal lesions of the hand and wrist. J Hand Surg 2004;29:393-399. 2. De Maeseneer M, Marcelis S, kOsteaux M, et al. Sonography of a rupture of the tendon of the extensor pollicis longus muscle: initial clinical experience and correlation with findings at cadaveric dissection. AM J Roentgenol 2005;184:175-179. 3. Ozgocmen S, Kiris A, Kocakoc E, et al. Evaluation of metacarpophalangeal joint synovitis in rheumatoid arthritis by power Doppler technique: relation between synovial vascularization and periarticular bone mineral density. Joint Bone Spine 2004;7:384-348. 4. Netter FH: The Ciba Collection of Medical Illustrations, Vol 8, Musculoskeletal system, Summit, NJ, Ciba-Geigy Corporation, 1987; pp 55-74. 5. Strickland JW: Flexor tendons-acute injuries, in Green DP (ed): Green’s Operative Hand Surgery (ed 4). Philadelphia, PA, Churchill Livingstone, 1999; pp 1851-1883. 6. Shapiro RS, Wagreich J, Parsons RB, et al: Tissue harmonic imaging sonography: Evaluation of image quality compared with conventional sonography. AJR 1998;171:1203-1206. 7. Martinoli C, Derchi LE, Pastorino C, et al: Analysis of echotexture of tendons with US. Radiology 1993;186:839-843. 8. Erickson SJ: High-resolution imaging of the musculoskeletal system. Radiology 1997;205:593-618. 9. Wolfe SW: Tenosynovitis, in Green DP (ed): Green’s Operative Hand Surgery (ed 4). Philadelphia, PA, Churchill Livingstone, 1999; pp 2171-2183. 10. Neviaser RJ: Acute Infections, in Green DP (ed): Green’s Operative Hand Surgery (ed 4). Philadelphia, PA, Churchill Livingstone, 1999; pp 1033-1047. 11. Bureau NJ, Chhem RK, Cardinal E: Musculoskeletal infections: US manifestations. Radiographics 1999;19:1585-1592. 12. Verdon ME. Overuse syndromes of the habd and wrist. Prim Care 1996;23:305-319. 13. Thorson E, Szabo RM: Common tendinitis problems in the hand and forearm. Ortho clin North Am 1992;23:65-74. 14. Giovagnorio F, Andreoli C, DeCicco ML: Ultrasonographic evaluation of de Quervain disease. J Ultrasound Med 1997;16:685-689. 15. Serafini G, Derchi LE, Quadri P, et al: High resolution sonography of the flexor tendons in trigger fingers. J Ultrasound Med 1996;213-219. 16. Noszian IM, Dinkhauser LM, Orthner E, et al: Ulnar collateral ligament: differentiation of displaced and nondisplaced tears with US. Radiology 1995;194:6163. 17. Glickel SZ, Barron OA, Eaton RG: Dislocations and ligament injuries in the digits, in Green DP (ed): Green’s Operative Hand Surgery (ed 4). Philadelphia, PA, Churchill Livingstone, 1999; pp 772-794. 18. Murphey SL, Hashimoto BE, Buckmiller J, et al: Ultrasonographic stress testing of ulnar collateral ligament injuries of the thumb. J Ultrasound Med 1997;16: 201-207. 19. O’Callaghan BI, Kohut G, Hoogewoud HM. Gamekeeper thumb: identification of the Stener lesion with US. Radiology 1994;192: 477-480. 20. Hergan K, Mittler C, Oser W: Ulnar collateral ligament: differentiation of displaced and nondisplaced tears with US and MR imaging. Radiology 1995;194: 65-71. 21. McGrouther D.A.: Dupuytren’s contracture, in Green DP (ed): Green’s Operative Hand Surgery (ed 4). Philadelphia, PA, Churchill Livingstone, 1999; pp 563-569. 22. Jacobson JA, Powell A, Craig JG, et al: Wooden foreign bodies in soft tissue: detection at US. Radiology 1998;206:45-48. 23. Bray PW, Mahoney JL, Campbell JP: Sensitivity and specificity of ultrasound in the diagnosis of foreign bodies in the hand. J Hand Surg 1995;20A:661-666. About the Author: Sharlene A. Teefey, M.D. is currently an Associate Professor of Radiology at the Mallinckrodt Institute of Radiology at Washington University School of Medicine in St. Louis Missouri. She is a member of numerous societies and organizations including the American College of Radiology, the Society of Radiologists in Ultrasound, and the American Institute of Ultrasound in Medicine. She is a reviewer of manuscripts for Radiology, the American Journal of Roentgenology, and Radiographics. She has more than 45 publications in peer review medical journals and has been a speaker at numerous institutions and conferences across the country. Examination of the Hand / Wrist Part II: 1. Tenosynovitis is a common problem of the hand and is due to inflammation of the synovial lining of a tendon sheath. The etiology that is considered controversial is A. work-related microtrauma B. a crystalline tendonopathy such as gout C. deposition diseases such as amyloidosis D. infectious causes E. inflammatory causes such as rheumatoid arthritis 2. The sonographic findings of tenosynovitis in general, include all of the following except A. tendon sheath fluid B. tendon sheath debris C. nodularity D. E. sheath thinning hypervascular changes may be observed with color Doppler sonography 3. Rheumatoid arthritis is a common cause of inflammatory tenosynovitis. The hand and or wrist may be involved in up to __________ of patients. A. 13% to 25% B. 26% to 33% C. 34% to 52% D. 53% to 63% E. 64% to 95% 4. Which of the following statements is true? A. Unfortunately, gouty tenosynovitis of the hand is still common in patients whose disease has been well managed. B. Gout is one of the more common causes of crystalline tendonopathy. C. Patients with gouty tenosynovitis typically have no symptoms. D. Calcific tendonitis is an uncommon cause of crystalline tendonopathy. E. With calcific tenosynovitis, the intratendinous calcium deposits are painful but become asymptomatic once they are released into the synovial space. 5. In tenosynovitis of the hand due to amyloidosis, the plaque like deposits along the flexor tendons, either within the carpal tunnel or digits, can lead to _______ nerve compression. A. median B. radial C. ulnar D. axillary E. musculo-cutaneous 6. Acute suppurative tenosynovitis is often caused by a penetrating injury but may also be hematogenous in origin. Which of the following statements is true? A. It is uncommon in immunologically compromised patients. B. The infectious process usually begins in the proximal flexor tendon sheath but may extend distally. C. The differential diagnosis includes cellulitis or a local abscess. D. The most common infecting organism is Streptococcus. E. It is uncommon in individuals with diabetes. 7. At sonography for acute suppurative tenosynovitis, all of the following statements are true EXCEPT A. tendon sheath fluid (consisting of purulent material) may be evident. B. surrounding hyperemic changes may be seen with color Doppler sonography. C. subcutaneous edema may be evident. D. a decrease in tendon size may be evident. E. if a focal fluid collection suggestive of an abscess is detected at sonography, it must be drained surgically. 8. Even though the etiology is controversial, all of the following statements regarding tenosynovitis caused by work-related, repetitive microtrauma are true EXCEPT A. Patients with calcium pyrophosphate deposition disease, hypothyroidism, or collagen vascular disease are at increased risk for its development. B. Any of the three-extensor compartments may be involved. C. In the flexor compartment, the flexor carpi ulnaris or radialis or the digital flexor tendons are most commonly involved. D. Patients usually present with pain on motion, tenderness, swelling, and crepitus. E. At sonography, synovial sheath fluid and thickening are seen. 9. Regarding De Quervain's disease, which of the following statements is true? A. This condition is more common in men than in men (6 to1 ratio). B. It usually occurs between 50 and 70 years of age C. Patients present with tenderness and swelling approximately 1 to 2 cm proximal to the radial styloid. D. Patients present with pain along the ulnar side of the wrist that increases with movement of the little finger. E. At sonography, tendon sheath fluid is rarely observed and the sheath appears thinner and hyperechoic. 10. Regarding trigger digit, which of the following statements is true? A. It occurs more commonly in men than in women. B. It has a peak incidence between 10 and 30 years of age. C. Sonographic findings include tendon thinning and large peritendinous cysts. D. Most patients have no pain. E. The etiology of this tenosynovitis is idiopathic. 11. Regarding trigger digit, the digit that is most commonly affected is the A. thumb B. index finger C. middle finger D. ring finger E. little finger 12. Traumatic avulsion of the flexor digitorum profundus tendon, usually in the _____, occurs commonly in young male athletes when there is forced extension of the digit during maximum contraction of the profundus muscle. A. little finger B. ring finger C. middle finger D. index finger E. thumb 13. Regarding tendon rupture, the simplest method for locating the proximal tendon is to initiate imaging in a A. longitudinal plane and look for a mass. B. longitudinal plane and look for a gap in the tendon itself. C. D. E. transverse plane at the proximal aspect of the finger and then scan distally until a gap is encountered. transverse plane at the proximal aspect of the finger and then scan distally until a mass is encountered. transverse plane at the distal aspect of the finger and then scan proximally until a mass is encountered. 14. The ulnar collateral ligament (UCL) of the metacarpophalangeal joint of the thumb is most commonly injured during A. skiing B. walking C. running D. swimming E. cycling 15. The displaced type of ulnar collateral ligament (UCL) tear is referred to as a _______ lesion. A. Kanavel B. Lee C. Stener D. Wolfe E. Strickland 16. The distinction between a displaced torn UCL and a non-displaced torn UCL is important because a non-displaced or incomplete tear may be treated A. conservatively with steroid injections. B. conservatively with a cast for four to six weeks. C. conservatively with acetaminophen. D. conservatively with non-steroidal anti-inflammatory drugs. E. surgically. 17. An idiopathic, benign proliferative disorder that results in fibrous tissue deposition in the palmar aponeurosis of the hand is called A. Gout B. Amyloidosis C. Calcific tendonitis D. De Quervain's disease E. Dupuytren's contracture 18. The nodules seen with Dupuytren's contracture may be indistinguishable from other pathologic processes of the hand, such as a A. foreign body of wood B. Stener lesion C. Giant Cell Tumor D. Kanavel lesion E. foreign body of glass 19. At sonography in Dupuytren's contracture, the subcutaneous nodules appear A. B. C. D. E. 20. hyperechoic and are oriented transversely to the digit. hyperechoic and are oriented longitudinally to the digit. hyperechoic and are not oriented to the digit. hypoechoic and are oriented longitudinally to the digit. hypoechoic and are oriented transversely to the digit. Foreign bodies in the hand are usually caused by penetrating injuries. Which of the following statements is true? A. If the foreign body is glass, metal, or stone, it can be difficult to diagnose on plain radiographs. B. It is important to orient the transducer parallel to the long axis of the foreign body to optimally visualize it. C. Glass and metal are hyperechoic with posterior acoustic shadowing. D. If the foreign body is wood, it may not be visible radiographically, but is easily detected with ultrasound. E. Wood is echogenic and produces a comet-tail artifact.