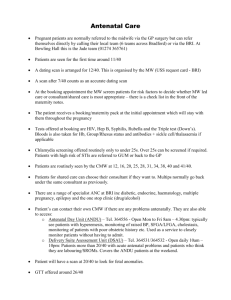
Antenatal Care Booking & Missed Appointment Guidelines
advertisement
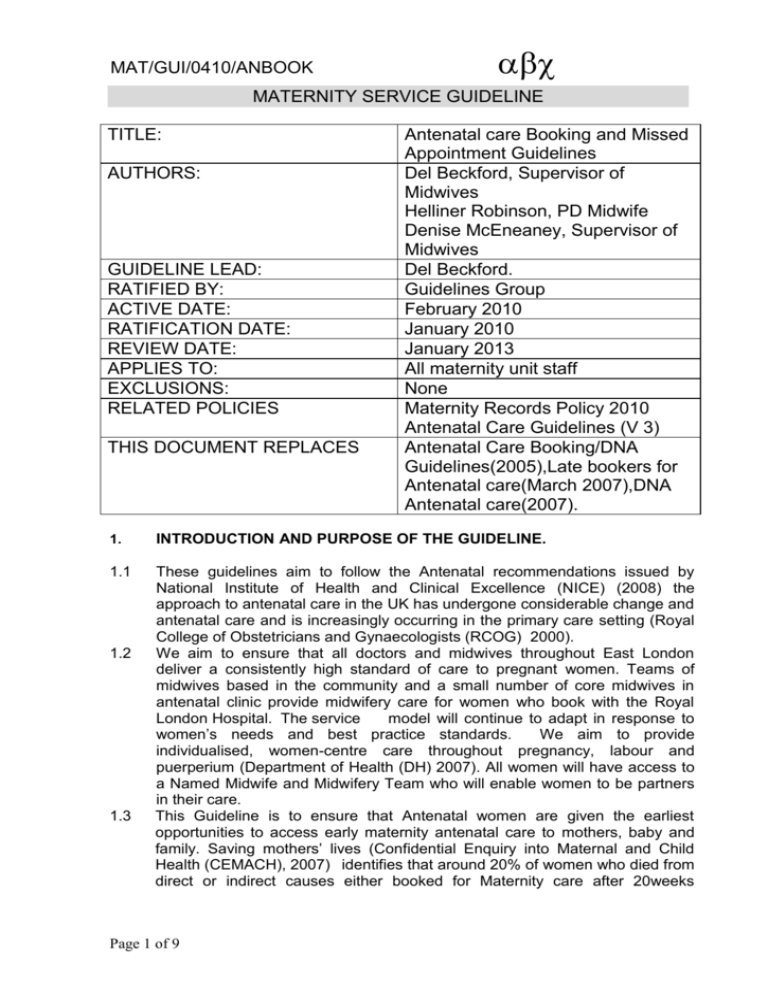
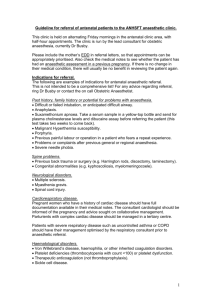
MAT/GUI/0410/ANBOOK MATERNITY SERVICE GUIDELINE TITLE: AUTHORS: GUIDELINE LEAD: RATIFIED BY: ACTIVE DATE: RATIFICATION DATE: REVIEW DATE: APPLIES TO: EXCLUSIONS: RELATED POLICIES THIS DOCUMENT REPLACES Antenatal care Booking and Missed Appointment Guidelines Del Beckford, Supervisor of Midwives Helliner Robinson, PD Midwife Denise McEneaney, Supervisor of Midwives Del Beckford. Guidelines Group February 2010 January 2010 January 2013 All maternity unit staff None Maternity Records Policy 2010 Antenatal Care Guidelines (V 3) Antenatal Care Booking/DNA Guidelines(2005),Late bookers for Antenatal care(March 2007),DNA Antenatal care(2007). 1. INTRODUCTION AND PURPOSE OF THE GUIDELINE. 1.1 These guidelines aim to follow the Antenatal recommendations issued by National Institute of Health and Clinical Excellence (NICE) (2008) the approach to antenatal care in the UK has undergone considerable change and antenatal care and is increasingly occurring in the primary care setting (Royal College of Obstetricians and Gynaecologists (RCOG) 2000). We aim to ensure that all doctors and midwives throughout East London deliver a consistently high standard of care to pregnant women. Teams of midwives based in the community and a small number of core midwives in antenatal clinic provide midwifery care for women who book with the Royal London Hospital. The service model will continue to adapt in response to women’s needs and best practice standards. We aim to provide individualised, women-centre care throughout pregnancy, labour and puerperium (Department of Health (DH) 2007). All women will have access to a Named Midwife and Midwifery Team who will enable women to be partners in their care. This Guideline is to ensure that Antenatal women are given the earliest opportunities to access early maternity antenatal care to mothers, baby and family. Saving mothers’ lives (Confidential Enquiry into Maternal and Child Health (CEMACH), 2007) identifies that around 20% of women who died from direct or indirect causes either booked for Maternity care after 20weeks 1.2 1.3 Page 1 of 9 MAT/GUI/0410/ANBOOK 1.4 1.5 gestation, missed over four routine appointments, did not seek care at all or actively concealed their pregnancies. All women should expect a standardised approach to accessing antenatal care which includes the booking referral pathway once pregnancy is confirmed; the booking interview enabling a detailed medical, social and obstetric history to be taken, the expected schedule of antenatal appointments in an uncomplicated pregnancy and recommendations for antenatal missed appointments whether this be midwifery clinic or consultant clinic. This Guideline will provide a care pathway for: Booking women for Antenatal care Late Bookers for Antenatal Care Missed antenatal appointments 2. IMPLEMENTATION 2.1 The updated paper copy will be attached to guideline notice board, in each clinical area for four weeks. Electronic copies will be distributed to the lead Midwives in each clinical area. The guideline will be available via the trust intranet and circulated to guidelines folders in all care settings. 2.2 2.3 ROLES AND RESPONSIBILITIES 3. 3.1 It is the responsibility of all maternity unit staff to carry out clinical care as described in the guideline unless there is justification for variation and the reason is documented. Further detail is in section 4. 4. GUIDELINE 4.1 BOOKING APPOINTMENT STANDARDS AND PROCESS FOR ENSURING WOMEN HAVE THEIR FIRST FULL BOOKING VISIT BY 12WEEKS 6 DAYS Women will be offered an appointment to be booked by 12+6 weeks. The Barts and the London ‘Your Antenatal Care’ leaflet is available from GP surgeries, children’s centres and clinics and advises all women to refer for first booking ideally before 9 weeks. This is to enable 2 visits in the first trimester of pregnancy. Women referred after 12 completed weeks will be booked within 10 working days. In an attempt to achieve the 12+6 weeks booking a fast track to the ‘Baby and me’ one Stop Clinic is available where needed for women to have their first full booking at the time of their first offered scan. Fast track Obstetric Consultant appointments can also be made for high risk Obstetric referrals within 5 working days or sooner if needed by contacting Antenatal Clinic Page 2 of 9 MAT/GUI/0410/ANBOOK (ANC) on 0207 377 3448. Alternatively Fax referral can be sent on 0207 377 7460 requesting urgent appointment and this will be organised as soon as possible by the Antenatal Clinic Manager. 4.1.1 Women from Tower Hamlets will be allocated to a midwifery team depending on the location of their GP. The teams are currently GP attached and are divided into localities. 4.1.2 Women who are known Type 1 or 2 Diabetics will be referred to the Diabetes Specialist Midwife for early antenatal booking. Women who live outside Tower Hamlets will be referred to City Team Midwives 4.1.3 4.2 REFERRAL PROCESS 4.2.1 Self or Direct referral: Women may self refer directly to a midwife by contacting the Community Midwives on 020 7377 7658. The Community Administration Manager will identify the appropriate midwifery team to contact the woman within 5 days of the referral to arrange a booking appointment 4.2.2 GP/Midwife Referral This is the most common referral route. A standardised booking referral form is completed by the GP/Midwife and faxed to Antenatal Clinic using agreed proforma. Address Antenatal Clinic 1st Floor, Outpatient's Department The Royal London Hospital Whitechapel Road London E1 1BB Fax number 020 7377 7460 4.2.3 The majority of GP surgeries have a regular midwifery clinic and the GP reception staff will arrange the midwifery booking appointment. This information will be recorded on the GP referral form. 4.3 4.3.1 4.3.2 REFERRAL ADMINISTRATION PROCESS Hospital based Antenatal Clinic Maternity Staff: GP Pregnancy Referral letters to be date stamped on receipt by maternity staff in ANC. All referral letters are logged in the “referral book” kept in ANC Antenatal clinic midwifery team to review and triage all referrals within 2 working days of receipt, and identify those with high-risk pregnancies, ensuring woman is booked under care of appropriate obstetric consultant team. Ensure the referrer had documented the woman’s last menstrual period date (LMP) and confirm the expected date of delivery (EDD). 4.3.3 Page 3 of 9 MAT/GUI/0410/ANBOOK 4.3.4 Send copy of GP referral form plus 2 scan request forms (one for dating and/or combined screening and one for anomaly scan) to the Obstetric Ultrasound Department (Basement, Holland Wing). Ultrasound clerk will post appointment and information leaflet to woman. 4.3.5 Outpatient Clerks (allocated to Hospital Based Antenatal Clinic) Identify existing hospital number or allocate hospital record number for new women to the hospital. 4.3.6 Print set of patient Identification (ID) labels. 4.3.7 Request main hospital notes and file these in Maternity Library (located in Antenatal Clinic). This ensures that health records from previous pregnancies and main hospital records are available for review by clinicians. 4.3.8 Book appointment by telephoning the woman with a choice of appointment date/s and time/s with appropriate consultant for high risk women (ANC midwife will provide guidance for admin staff on this). 4.3.9 All low risk women to be booked under allocated community midwifery team or consultant midwife as ‘lead professional.’ The lead professional must be documented on the front of the woman’s notes and CRS 4.3.10 ANC clerk to contact woman with a choice of appointment date/s and time/s for booking history 4.3.11 Community Administration Manager Daily collection (Monday – Friday) of GP referral letters from designated area in the antenatal clinic and distribute to the appropriate community teams to arrange booking appointments within agreed timeframe if not already done. Enter women’s details on ‘GP Referrals’ database. 4.3.12 Community Based Midwives Arrange a booking appointment for women within agreed timeframe if not already done. If there are no available booking appointments in the GP clinic, midwife to discuss with the woman and offer a home booking. 4.4 4.4.1 4.4.2 4.4.3 BOOKING APPOINTMENT DOCUMENTATION All women will be seen by a midwife for the booking appointment. During this appointment, a thorough health and social needs assessment will take place following the guidance in the Antenatal Care Guidelines. This information should be recorded in the maternity handheld records as identify in the Maternity Records Guideline. Clinical assessment for migrant women who have not had a full medical examination in the United Kingdom. Migrant women should have a full medical assessment including a heart and lung check. This will usually be completed on the GP referral form but if this is missing, or the woman has self referred, the midwife will arrange an appointment at the GP surgery (or hospital antenatal clinic if the woman is not registered with a GP) to have this examination carried out. This will be documented in the pregnancy notes as completed on page 3 medical history under physical examination All low risk women to be booked under allocated community midwifery team or consultant midwife as ‘lead professional.’ The lead professional must be documented on the front of the woman’s notes and CRS If the lead professional is changed from midwife to consultant during the antenatal Page 4 of 9 MAT/GUI/0410/ANBOOK 4.4.4 4.4.5 4.4.6 4.4.7 period, the consultant confirming this change must complete a proforma titled ‘Change to Consultant Led Care’. This needs to be sent to the community team or consultant midwife (whoever was previous lead professional) and GP. ANC clerks will change lead professional on CRS Community Midwives to complete Antenatal clinic diaries or clinic log sheets (bookings and follow up's) and forward to Community Administrative manager to update GP Referral database (this database monitors gestation at booking). Hospital based midwives to complete Antenatal Clinic Booking information to monitor gestation at booking. The booking Midwife to complete PAS form following all bookings and return to the hospital Antenatal Clinic. ANC clerk will enter social details on CRS and add to ‘Booked List (EDD must be confirmed.) The booking midwife to enter maternal booking assessment details on CRS such as Medical, Family & Obstetric history. 4.5 BABY AND ME - ONE STOP CLINIC 4.5.1 This is a new service in the maternal and Fetal assessment Clinic has been developed to support the booking process, assist risk assessment for the woman and agreement of appropriate care pathway. This contact also offers the woman the opportunity to discuss early pregnancy information, maternal screening results and to discus and questions regarding combined screening tests. This contact is being implemented in 2010, and by July 2010 will be offered to all women. Access to this clinic will be linked to the dating/combined screening appointment. 4.5.2 4.6 LATE BOOKINGS 4.6.1 Ascertain the reason for late referral and stress the importance of regular antenatal care. Ensure the appointment is arranged within 2 weeks of receipt of the referral (or fast track as required) see 4.1. If a woman has booked too late to make use of screening tests, explain and document this. Highlight late booking as risk factor on page 11 of the Pregnancy Notes. The blood pressure in the 2nd trimester may not reflect the true blood pressure of the woman due to the physiological drop in the 2 nd trimester. Note BMI may not be as accurate depending on gestation. If the woman knows her early pregnancy weight, calculate Body Mass Index according to this. Discuss with named Supervisor of Midwives/Community Midwifery Manager if you have concerns and require support to plan future care. 4.6.2 4.6.3 4.6.4 4.7 MISSED BOOKING OR FOLLOW UP APPOINTMENT GUIDEANCE (OFTEN CALLED DNA’S). PLEASE SEE FLOW CHART Appendix 1. 4.7.1 Non attendance has a strong correlation with poor maternal and neonatal outcomes. It is essential that a proactive and innovative approach is taken by all maternity staff to support early and regular contact with maternity services. Page 5 of 9 MAT/GUI/0410/ANBOOK 4.7.2 4.7.3 4.7.4 Women will usually attend if they understand the reason for the appointment, is at a time that is manageable for them. Where possible, antenatal contacts should be offered in community locations, close to the woman’s home and at a time that is convenient to the woman. Midwives must update CRS if a woman fails to attend her booking of follow up appointment and offer subsequent appointment. Medical staff will liaise with midwifery staff to support attendance if the woman did not attend (DNA) and initiate the guidance in Appendix 1 as necessary. Administrative staff must support the maternity team in organising appointments and generating appointment letters. 5 PROCESS FOR ARRANGING AVAILABILITY OF HEALTH RECORDS 5.1. Initialising Maternity Records The referral letter will be completed by the first professional that the woman refers herself to. This may be her Midwife or General practitioner. The referral letter should be completed using the clinical risk assessment (antenatal) guideline which will classify that the women will be booked for Team Care (High Risk) or Midwife Led Care (low risk). This box MUST be ticked to enable direct referral to the appropriate pathway of care. The woman’s maternity record will be ordered on receipt of the referral form and will be filed in the ‘mini maternity library’, for access at any time that the woman is admitted to the hospital. 5.2 Mini Maternity Library The clerk will file all of the women’s main hospital records received from medical records into the mini maternity library. They will remain in the library for the remainder of the pregnancy and retrieved as required for all CONSULTANT LED CLINICS, ALL JOINT CLINICS and ANY HOSPITAL ADMISSION. The main hospital record will not be required for LOW RISK MIDWIFE LED CLINICS. On a daily basis records received will be checked off on the list prior to filing. Any records that are not received in a reasonable time frame must be reordered. The clerk in the mini maternity library is responsible for retrieving the hospital notes for the clinics as required and refilling them on their return. 5.3 Process for requesting notes from previous pregnancies (not at Barts and the London NHS Trust) but a copy required based on high risk condition or other concerns If following obstetric review it is important that copies of notes are retrieved from another maternity unit a letter will be sent from the Consultant or lead midwife for Antenatal Clinic and a copy of the letter kept in the woman’s handheld record. When notes arrive at the antenatal clinic they will be filed in Page 6 of 9 MAT/GUI/0410/ANBOOK the Main Maternity record for review at subsequent appointments as required. 6. 6.1 BREACH OF GUIDELINES The incident will be reviewed within the risk management framework. The impact of this incident will be reviewed by the appropriate lead clinician and feedback/ training given to staff as required. 7. 7.1 MONITORING COMPLIANCE See Appendix 2 REFERENCES: 1. Department of Health, Welsh Office, Scottish Office Department & Department of Health and Social Services, Northern Ireland. (1998) Why mothers die: report on confidential enquiries into maternal Deaths in the UK 1994-1996.London: Statutory Office 2. Confidential Enquiry into Maternity and Child Health (2007) Saving Mothers’ Lives. Reviewing maternal deaths to make motherhood safer-2003-2005. London: CEMACH 3. Confidential Enquiries into Maternal Deaths in the United Kingdom (2001) Why mothers die 1997-1999: the fifth report of the confidential enquiry into maternal deaths in the U.K. London: CEMD. Available at: www.cmace.org.uk 4. Department of Health (2007) Maternity Matters: Choice, access and continuity of care in a safe service. London: DH. 5. National Institute of Health and Clinical Excellence (NICE) (2008) Antenatal care: Routine care for the healthy pregnant woman. London: NICE 6. Petrou, S. Kupek, E. Vause, S. Maresh, M. (2003) Antenatal visits and adverse perinatal outcomes: results from a British population – based study. European Journal of Obstetrics and Gynecology and Reporductive Biology. 106(1), pp40-49. Page 7 of 9 MAT/GUI/0410/ANBOOK Appendix 1 Woman does not attend appointment (DNA) Check EDD – has she given birth/miscarried? TOP Yes – No further action required Hospital Clinic 1st DNA, another appt is sent out to woman by ANC clerk Woman attends appointment. Record previous DNA and reason in Pregnancy Notes. Stress importance of regular attendance. Community Midwives 1st DNA, call woman to arrange next appointment or send letter if not available 2nd non attendance Midwife to contact woman, and/or speak to GP to ascertain if she has been seen by GP (or CMW’s if she has DNA’d hospital ANC). Ask if the woman has booked elsewhere. Confirm known address and contact details with GP. Arrange home visit by Community Midwife to do an ANC check, booking and/or arrange follow up appointments. If referred to City Team, follow as above and refer to CMW in the area where woman lives. Request home visit and encourage woman to attend next appt. Request feedback from CMW following home visit. Woman attends appointment. Record previous DNA and reason in Pregnancy Notes. Stress importance of regular attendance. If in any doubt at any stage, liaise with either the Band 7 Midwife Area/Team Manager or Community Manager/Matron or your named Supervisor of Midwives Document in pregnancy record all discussions and plans for care – page 11 pregnancy notes Page 8 of 9 Recording non attendance: Record on CRS Ensure next appointment booked Woman did not attend appt., process above repeated. If unable to contact woman (no known address or has left last known address and no contact Tel number), inform SOM. Consider Child Protection alert to London hospitals. Inform GP. Liaise with Social Worker if applicable. Take off booked list if woman has moved to another area MAT/GUI/0410/ANBOOK Monitoring lead Monitoring tool Monitoring time frame. Elements to be monitored Responsibilities of different staff groups related to giving and documenting pt information at different stages of pregnancy Audit and Quality midwife and community manager Community GP Referral database Monitor timeframes on database Community admin manager Community GP Referral database Continuous – reported monthly on maternity dashboard APPENDIX 2 Timeframe of receipt of referral in ANC, receipt by CMW’s and date of booking Continuous audit of gestation at booking Process for ensuring that women who refer > 12 weeks are booked within 2 weeks Process for clinical assessment of migrant women including completion of heart and lung check Audit and Quality audit lead Availability of health records Lead ANC midwife Missed appointments DNA recorded on CRS Next appointment booked Referral to CMW’s if DNA’d twice. Audit and Quality Audit midwife Lead ANC midwife Page 9 of 9 Notes audit Audit tool to monitor number of health records available Audit tool to monitor booking and follow up DNA’s Dashboard reported externally to the trust monthly Monthly – 10 sets of notes (incorporate in documentation audit) Community midwifery audit for high risk women (Gateway team) Quarterly audit for 1 week period of hospital based antenatal clinic sessions. Completed every 3 months Quarterly audit for 1 week period of hospital based clinic sessions Committee to receive the report. Action plan lead committee Implementing and sharing best practice The Maternity and Gynaecology Audit Committee will receive completed reports. Audit feedback and resultant action plans will be fed back to the maternity and Gynaecology governance Board Acting on recommendation s and Lead(s) The Maternity and Gynaecology Audit Committee will lead on the action plan. Change in practice and lessons to be shared The leads of the Maternity and Gynaecology Audit Committee will be expected to read and interrogate the report to identify deficiencies in the record keeping system. Minutes will be clearly documented. Any deficiencies will be addressed through multiprofessional action planning. Actions will be taken through teaching where necessary. Recommendations will be allocated to key areas of practice with identified leads. Required actions will be identified and completed in a specified timeframe and monitored by the Maternity and Gynaecology audit committee. Required changes to practice will be identified and actioned within a specific time frame documented in the agreed action plan. A lead member of the team will be identified to take each change forward where appropriate. Lessons will be shared with all the relevant stakeholders.