Can you summarize briefly what you found? We have found that
advertisement
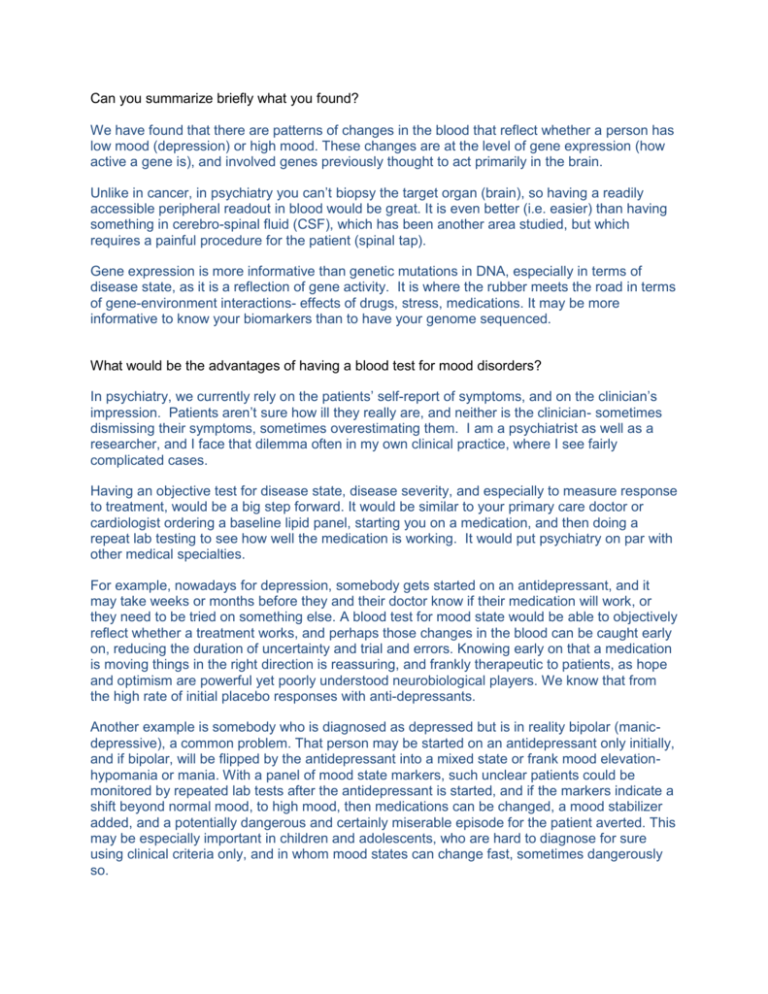
Can you summarize briefly what you found? We have found that there are patterns of changes in the blood that reflect whether a person has low mood (depression) or high mood. These changes are at the level of gene expression (how active a gene is), and involved genes previously thought to act primarily in the brain. Unlike in cancer, in psychiatry you can’t biopsy the target organ (brain), so having a readily accessible peripheral readout in blood would be great. It is even better (i.e. easier) than having something in cerebro-spinal fluid (CSF), which has been another area studied, but which requires a painful procedure for the patient (spinal tap). Gene expression is more informative than genetic mutations in DNA, especially in terms of disease state, as it is a reflection of gene activity. It is where the rubber meets the road in terms of gene-environment interactions- effects of drugs, stress, medications. It may be more informative to know your biomarkers than to have your genome sequenced. What would be the advantages of having a blood test for mood disorders? In psychiatry, we currently rely on the patients’ self-report of symptoms, and on the clinician’s impression. Patients aren’t sure how ill they really are, and neither is the clinician- sometimes dismissing their symptoms, sometimes overestimating them. I am a psychiatrist as well as a researcher, and I face that dilemma often in my own clinical practice, where I see fairly complicated cases. Having an objective test for disease state, disease severity, and especially to measure response to treatment, would be a big step forward. It would be similar to your primary care doctor or cardiologist ordering a baseline lipid panel, starting you on a medication, and then doing a repeat lab testing to see how well the medication is working. It would put psychiatry on par with other medical specialties. For example, nowadays for depression, somebody gets started on an antidepressant, and it may take weeks or months before they and their doctor know if their medication will work, or they need to be tried on something else. A blood test for mood state would be able to objectively reflect whether a treatment works, and perhaps those changes in the blood can be caught early on, reducing the duration of uncertainty and trial and errors. Knowing early on that a medication is moving things in the right direction is reassuring, and frankly therapeutic to patients, as hope and optimism are powerful yet poorly understood neurobiological players. We know that from the high rate of initial placebo responses with anti-depressants. Another example is somebody who is diagnosed as depressed but is in reality bipolar (manicdepressive), a common problem. That person may be started on an antidepressant only initially, and if bipolar, will be flipped by the antidepressant into a mixed state or frank mood elevationhypomania or mania. With a panel of mood state markers, such unclear patients could be monitored by repeated lab tests after the antidepressant is started, and if the markers indicate a shift beyond normal mood, to high mood, then medications can be changed, a mood stabilizer added, and a potentially dangerous and certainly miserable episode for the patient averted. This may be especially important in children and adolescents, who are hard to diagnose for sure using clinical criteria only, and in whom mood states can change fast, sometimes dangerously so. Last but not least, pharma companies may use such markers to help make the discovery of new medications be less of a hit-or-miss process. Currently, developing a new drug is like developing a Hollywood blockbuster- no guarantees that it will pan out, and sequels are a safer bet. We need to emphasize that we are at an early stage in this work, and that a lot more prospective work needs to be done to establish which markers work best, to look at different subpopulations, potential gender differences, age related differences, response to different medications. Psychiatry, like the rest of medicine, will likely end up being personalized and tailored to the individual, based on their biomarker profiles. The exciting thing is that we made a breakthrough that suggests such work is feasible and worth doing in the first place. Other than depression and bipolar, are there other diseases could these findings be used to diagnose? Mood state is important and sometimes overlooked in terms of severity in other complex disorders- postpartum depression (trivialized as “baby blues”), post-traumatic stress disorder, after myocardial infarction and cardiovascular procedures, in cancer, in fibromyalgia, etc. having an objective measure may speed up getting the appropriate attention and treatment. We are also doing similar work in schizophrenia, looking for blood markers for delusions and hallucinations. Schizophrenia is a tough disorder, where subjectivity and uncertainty about illness severity are even more of a factor. We are excited about our yet unpublished findings in that area, and hope to move that work forward fast. NIH funding being on the decline these days, I think philanthropy stepping in can play a major role for funding such early stage, unconventional research. Last but not least, we are doing some work on biomarkers for anxiety and stress, using a new animal model we have developed, as well as studies in human blood samples. This work, in addition to my collaborators at Indiana University (notably Helen Le-Niculescu, and John Nurnberger) is being done in collaboration with colleagues at The Scripps Research Institute in La Jolla, CA, my PhD alma mater (notably Dan Salomon, and more recently Nik Schork), and with advice from Ming Tsuang and others at UC San Diego, my clinical alma mater. We are looking at ways of collaborating with the military for expanding such studies of high relevance to combat stress. There is a role for industry, including biotech, in this area. We hope that the FDA will take an active role in evaluating, regulating and approving any such tests. I would predict that tests like these may hit the market in about five years, plus/minus two years. A lot more work needs to be done, and will be done. Two drugs were found to exert similar effects to high and low mood. Can you expound on the implications of this and also on how this data could aid drug development? It’s a bit of an esoteric point. In brief, looking at the patterns of things we see changed in the blood in relationship with mood state, and comparing that pattern with a database at the Broad Institute at MIT that has the signature patterns of a large number of known drugs, one can find which drugs exert a similar effect. It might suggest new drugs (or at least chemical structures to be tweaked and developed by pharma companies) to be tried in the treatment of mood disorders. Also, can you expound on the implications of the overlap between some of the genes identified in your study and those involved in cancer? It’s more of a surprise to us than anything, and we don’t want to over-interpret it. Other colleagues in the field (Husseini Manji at NIMH, Francine Benes at Harvard, Huda Akil and colleagues at Michigan, and others) have had results pointing in this direction, and now the full picture we report seems to make sense. Nature is a tinkerer, has a limited number of building blocks at its’ disposal, and seems to be re-using some of the same molecules used for “lower” functions such as cell proliferation and cell death, for higher mental functions such as mood regulation. Philosophically and evolutionarily one can speculate about the normal roles of this particular overlap- expansiveness of cells and of behavior (high mood) when the environment is favorable for expansion; shrinkage of cells, apoptosis (cell death), retraction into self (low mood) and suicide when the environment is not supportive or hostile. An interesting example of that may be athletes on illegal performance enhancing drugs such as steroids, who have an expansive behavior and sometimes boorish behavior in tandem with their expanding muscles, and are depressed when they get of these drugs, in tandem with their muscle shrinkage. We speculated about this “brain as a muscle “model in an article in the journal Genome Biology in 2005 Pragmatically, we don’t know yet for sure if mood drugs may help with treating cancer, or cancer drugs may help with treating mood, but there are interesting hints in both directions that this may turn out to be a very fruitful avenue to pursue. Also, are mood disorders associated with different types of cancer? A lot of empirical work needs to be done. *************************************************** Thank you for your interest in this early-stage, long-term effort. Please check periodically www.neurophenomics.info for scientific updates and study participation opportunities, as they become available. Together we can make a difference. In the meantime, seeing an expert and/or getting a second opinion, in your local geographic area, may be wise if the symptoms are not well controlled and/or the diagnosis is unclear. In this era of limited government funding for science due to other more urgent priorities, individuals can make a difference. If you would like to support this work, you can send a check made out to: “Laboratory of Neurophenomics- IU SOM”, putting “blood biomarkers project” in the memo line. For large donations or (named) endowment of the Laboratory, please contact myself or Liz Elkas: Elizabeth Elkas, Associate Dean for Development Indiana University School of Medicine eelkas@iupui.edu; 317-274-3270; 800-643-6975 Best wishes, Alexander B. Niculescu III, MD, PhD Assistant Professor of Psychiatry and Medical Neuroscience Indiana University School of Medicine Staff Psychiatrist, Indianapolis VA Medical Center Director, INBRAIN and Laboratory of Neurophenomics Institute of Psychiatric Research 791 Union Drive Indianapolis, IN 46202-4887 e-mail: anicules@iupui.edu