Personal Protective Equipment (PPE)
advertisement

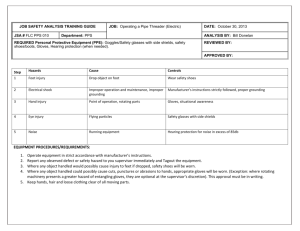
Personal Protective Equipment (PPE) Personal Protective Equipment (PPE) Introduction Personal protective equipment (PPE) involves use of protective barriers such as gloves, gowns, aprons, masks, or protective eyewear, which can reduce the risk of exposure of health care personnel (HCP) skin, mucous membranes, and respiratory tract to potentially infective materials and certain airborne agents. PPE also provides protection against other hazards in the health care facility such as chemicals and physical injury. Employers and personnel share in the responsibility for ensuring use of PPE. Employers need to provide PPE and assure that it is accessible to all personnel. Personnel need to consistently use PPE for their own protection. Some components of PPE, e.g. gloves and gowns, are also used for protection of patients during invasive procedures such as insertion of a central venous catheter or surgical operations where a sterile field and aseptic technique are required. 46 The selection of PPE should be based on assessment of the risk of contamination of HCP’s clothing and skin by blood, body fluids, secretions and excretions and – if applicable- to minimize risk of exposure to splashes or sprays of blood and body fluids or certain airborne microorganisms, e.g., Mycobacterium tuberculosis. Use of PPE also should include assessment of the risk of transmission of microorganisms from HCP or the environment to the patient. Gloves Types of Gloves There are three main types of gloves used in the health care setting 1. Sterile gloves: Mostly used for surgery. They are disposable, sterile, and individually wrapped items. They are used whenever there will be a percutaneous or permucosal contact with tissues (e.g. surgical procedures, insertion of central venous catheter and urinary catheter). 46 Fig. 16: Sterile Gloves 50 Personal Protective Equipment (PPE) 2. Non-sterile gloves: Non-sterile disposable, single use gloves (e.g. latex gloves) are usually not individually wrapped. They are used to protect against direct skin exposure to blood or other body fluids or for anticipated contact with mucous membranes and prior to contact with contaminated equipment or surfaces. Examples of application include putting on gloves prior to insertion of a Fig. 17: Nonperipheral IV catheter (except in high risk areas). These sterile Gloves types of gloves should be discarded after one use followed by hand hygiene. 3. Utility or heavy-duty household gloves: Utility gloves are used for handling contaminated items and waste and for performing environmental cleaning activities. They can be reused after decontamination, but they should be discarded when punctured or torn. General Indications for Gloves Fig. 18: Utility Gloves Staff should wear gloves when they anticipate their hands will come into contact with blood, body fluids, nonintact skin or tissue or equipment and surfaces that are visibly contaminated with body fluids. Indications for Sterile Gloves Before surgery Before any invasive procedure that require aseptic technique (e.g. insertion of urinary catheter, insertion of central venous catheter, insertion of canulas in immunocompromised patients and newborns). Before wound dressing. Mixing I.V. fluids and using multidose vials. Indications for Disposable Non-sterile gloves When starting intravenous (I.V.) lines or performing phlebotomy. When changing dressings or handling soiled dressings. When cleaning or handling soiled equipment, instruments, or other items that may be contaminated with blood, urine, feces, or drainage. When handling specimens and their containers. 51 Personal Protective Equipment (PPE) When suctioning the respiratory tract of a patient or performing oral care in which fingers need to be placed inside the patient’s mouth. Indications for Utility gloves: When handling medical waste (red bag trash). When cleaning up spills of blood or body fluids (As they are difficult to be cleaned, it is preferable to use double non-sterile disposable gloves). When using chemicals such as cleaning products and disinfectants. 42 For most chemical disinfectants latex exam gloves that protect hands and forearms are sufficient. Other glove materials such as nitrile offer additional protection against certain chemicals if prolonged contact with the chemical is anticipated. Gloving tips Washing utility gloves: Always wash utility gloves before you take the gloves off your hands. Washing hands: Hand hygiene is always recommended after removing gloves because gloves may become perforated during use and bacteria can multiply rapidly on gloved hands. Reusing disposable gloves: Never reuse any type of disposable gloves (e.g., latex gloves, surgical gloves) as they are difficult to reprocess properly and the protective integrity of the glove is usually compromised when attempting to clean and reuse. Latex allergy: If you or your patient has a latex allergy, wear nonlatex gloves, e.g., vinyl or nitrile. Changing gloves: Gloves must be changed: Between patients. Before each procedure if more than one procedure is done for the same patient. If they become soiled, contaminated or perforated while caring for a single patient. Removing gloves: When removing gloves, you should not allow the outside surface of the gloves to come into contact with your skin. Avoid letting the gloves snap, as this may cause contaminates to splash into your eyes or mouth or onto your skin or other people in the area. It is important to remove used gloves before touching anything that can become contaminated through contact, such as surfaces, faucets, or pens. 52 Personal Protective Equipment (PPE) Aprons and Gowns Single use plastic aprons or gowns should be used during procedures that are likely to generate splashes of blood or body fluids or during activities that may contaminate clothing or uniforms with microorganisms or infectious material. Most often, aprons can be used to minimize potential for contamination of HCP uniforms or personal clothing. The neck strap and the waist tie should be torn and the apron should be discarded into a clinical waste bag before it is carried out of the room.11 More extensive coverage, such as a gown covering arms, trunk, and upper thighs are only needed if the patient care might involve splashes or sprays of blood or body fluids. Ideally gowns worn for such purposes should be fluid resistant. Note: Cotton gowns are permeable to water and are no longer recommended. Disinfection of heavy duty aprons Heavier duty plastic aprons can be reused provided that they can be disinfected by a wash with warm water and detergent and dried; followed by wiping the apron with 70% isopropyl alcohol. Another option would be immersing the heavy duty plastic aprons in water and chlorine. Cleaning and disinfection should be done between each patient. 9 Headgear Disposable caps, balaclavas, or scarves should be worn to confine and contain hair during certain procedures such as surgical procedures performed in the operating theater. They should be well-fitting and sealed. Note: Well fitting cotton caps and scarves may be recycled (by laundering at a high temperature) if disposable ones are not available. Recycled caps must be changed frequently (at least after every shift; in hot climates they should be changed more frequently). 9 Face, Eye and Respiratory Protection Face masks and eye protection should be worn when there is risk of splashes or sprays of blood or body fluids into the face and eyes of HCP. Options for this type of PPE include separate mask and eye protection or combination products wherein an eye shield is bonded to a standard mask. Most masks are designed to be used one time and then discarded. Another option however is a full-face shield that protects the eyes and mouth. This can be disposable or reusable. If reusable it should be cleaned and disinfected after contamination. Splashes of 53 Personal Protective Equipment (PPE) chemicals are additional examples of the need for face and eye protection of HCP. 9 Respiratory Protection Use a standard mask alone when there is risk of exposure to droplets that might contain infectious agents. Examples of microorganisms that are transmitted by exposure to droplets from patients with infection include Neisseria meningitidis, Bordetella pertussis, and influenza virus. 9 Both disposable paper and cotton masks offer less protection once they become moist; however, if resources are limited these do provide some protection against large droplets. If available, disposable paper masks with synthetic material for filtration are ideal for most patient care needs. Most masks should be used once and then discarded; reusable, cotton masks must be laundered. Cotton masks offer less protection against airborne infectious agents such as M. tuberculosis but are better than no respiratory protection if no alternative is available. Airborne disease and respiratory protection For airborne infectious agents such as M. tuberculosis a high filtration respiratory protective device is ideal, and if available, should be used to care for patients with suspected or proven active pulmonary tuberculosis. Such devices may be labeled as high efficiency masks or respirators and are designed to capture high percentages (>95%) of particles that are less than 1 micron in size. Instructions for use of these devices are usually supplied by the manufacturer and are designed to assure a good seal around the nose and mouth of the wearer. If such devices are not available, a standard mask still offers some protection of personnel and therefore should be worn. Other measures to prevent exposure to airborne disease such as tuberculosis should be employed. These include asking the patient to cough into a disposable tissue and, if tolerable, to have the patient wear a mask when in corridors or in areas that do not have negative pressure airflow and exhaust. Overshoes and Footwear Overshoes worn over the ordinary shoes are not recommended, as it is an ideal way of transferring microorganisms from floor and shoes to hands. Closed footwears replacing the ordinary shoes are not generally needed with the exception of some special areas such as the Operating Theatre (OT). The intent is to confine contaminants on footwear prior to entering an OT. In addition, certain surgical procedures, such as hip replacement, may result in spills of blood around the patient table and onto the floor. Fluid resistant shoe covers or boots are recommended for this situation to protect operative personnel from skin exposure to blood. 9 Fig. 19: Commonly used protective Barrier 54 Personal Protective Equipment (PPE) 55