Chapter 19
advertisement

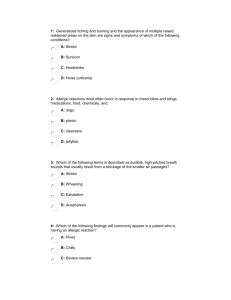
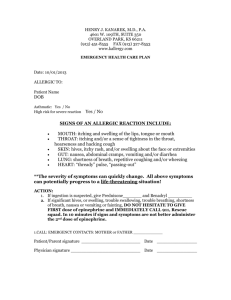
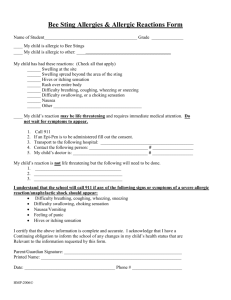
Ready for Review An allergic reaction is a response to chemicals the body releases to combat certain stimuli, called allergens. Almost any substance can trigger the body’s immune system and cause an allergic reaction. Allergic reactions occur most often in response to five categories of stimuli: insect bites and stings, medications, foods, plants, and chemicals. An allergic reaction may range from mild and local, involving itching, redness, and tenderness, to severe and systemic, including shock and respiratory failure. Anaphylaxis is a life-threatening allergic reaction mounted by multiple organ systems that must be treated with epinephrine. Wheezing and skin wheals can be signs of anaphylaxis. The immune system protects the human body from substances and organisms that are considered foreign to the body. Allergens enter the body through oral ingestion, injection or envenomation, inhalation, or topical absorption. Injected or inhaled allergens tend to cause the most severe reactions. When a foreign substance first invades the body, the primary response begins. If the body is unable to identify the substance, immune cells record the features of the outside substance and produce antibodies to inactivate the foreign substance. This process is called development of sensitivity. Basophils and mast cells contain antibodies and can recognize the foreign substance should it enter the body again. Basophils are stationed in specific sites within the tissues. Mast cells are on patrol throughout the body. Chemical mediators are essentially the body’s weapons against foreign substances. They release substances when an antigen invades the body and combines with one of the antibodies. If this response spreads throughout the body (becoming systemic), it causes the signs and symptoms of an anaphylactic reaction. Allergic reactions are more localized. Histamines are some of the primary chemical mediators. They cause the blood vessels in the local area to dilate and the capillaries to leak; this translates into flushed skin, hypotension, tissue swelling, and fluid secretion. Leukotrienes are another chemical mediator and cause additional dilation and leaking of fluid into the tissues. Signs and symptoms of an allergic reaction are varied but can include hives, pruritis (itching), flushed skin, swelling, respiratory symptoms (wheezing, stridor, dyspnea, and angioedema), cardiovascular symptoms, gastrointestinal symptoms, neurologic symptoms, and even shock if the reaction is severe. In assessing a person who may be having an allergic reaction, check for flushing, itching, and swelling skin; hives; wheezing and stridor; a persistent cough; a decrease in blood pressure; a weak pulse; dizziness; abdominal cramps; and headache. The patient history will help to identify problems specific to the allergic reaction. When assessing a patient with an allergic reaction, ask if the patient has a history of allergies, what the patient was exposed to, when the exposure occurred, and how the patient was exposed. Determine the onset of symptoms, what the effects of the exposure have been, and how they have progressed. All patients with suspected anaphylaxis require oxygen. Management of anaphylaxis also includes removing the offending agent, providing fluid resuscitation as needed, administering epinephrine, and transporting promptly. People who know that they are allergic to bee, hornet, yellow jacket, or wasp venom often carry a bee sting kit that contains epinephrine in an auto-injector. You may help to administer this medication in this form with authorization from medical control. Always provide prompt transport to the hospital for any patient who is having an allergic reaction or has been bitten by a poisonous insect. Remember that the patient’s condition can deteriorate rapidly. Carefully monitor the patient’s vital signs en route, especially for airway compromise.