What Can Medical Students Learn From Anthropology?
advertisement

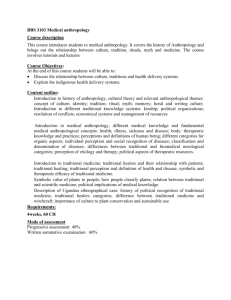
Eddie Rooke 1 What Can Medical Students Learn From Anthropology? Most medical practitioners would find it difficult to give a definition of anthropology and may not be acquainted with information on how factors such as ecology, culture, and politics influence the health of a society. To many Western-style medical practitioners (biomedical physicians), culture is something linked to noncompliance and misunderstanding and has no place in hospitals and clinics. It is hard to dispute the massive benefits that the world has gained from biomedical progress, but increasingly more people are growing disenfranchised with biomedicine, both in Canada and around the world. As a medical student with an appreciation for anthropology, I have always felt that biomedicine has much to gain from the social sciences. This paper is my attempt to provide an introduction to medical anthropology for medical students by discussing three main theories regarding health and sickness: medical ecology, health systems theory, and critical medical anthropology. I will also comment on an emerging theory, anthropological medicine, and on research that might be of particular interest to medical students. Following this, I will comment on the theory that seems most relevant and applicable to medical students. Medical Ecology The holistic and interdisciplinary approach to looking at health and disease is known as medical ecology. This approach tries to account for the many variables in the environment that affect health: “medical ecologists view health and disease as Eddie Rooke 2 reflections of relationships within a population, between neighboring populations, and among the life forms and physical components of a habitat.” (McElroy and Townsend, 2004: 2) Ann McElroy and Patricia Townsend are major contributors to the ecological model of medicine and favor it because it can incorporate the efforts of many disciplines, such anthropology, as: physical medicine, traditional anthropology, healing, environmental archaeology, studies, and cultural applied anthropology. Their theory of medical ecology relies on three central premises. The first is that disease is caused by a “chain of factors related to ecosystem imbalances,” (2004: 30) in addition to the clinical reasons for disease. The second premise is that culture, biology, and physical environment are in constant interaction with each other and health and disease arise out of this relationship (2004: 30). Thirdly, environment is not solely the physical environment, but also the culturally created environment that all human being live in (2004: 30). This includes buildings, farms, slums, villages, and also social stratification, values systems, and worldviews. McElroy and Townsend also utilize adaptation as part of health and medical anthropology. They describe adaptation as “changes, modifications, and variation enabling a person or group to survive in a given environment.” (2004:14) They go on to say that “health is one measure of environmental adaptation, and that health can be studied through ecological models.” (2004:14) There are many studies that illustrate the role of adaptation between health, culture, and environment, but few are more famous than the rising prevalence of sickle cell anemia in conjunction with malaria in West Africa. Sickle cell anemia is a genetic variation that offers some Eddie Rooke 3 innate protection from the illness caused by malaria. It was found that, as agriculture became more common in West Africa, there was an increased risk of contracting malaria because the environment had changed to one that fostered the growth of the mosquito that carries malaria (Livingstone 1958 in Hanh, 1995: 60). Livingstone (1958) concluded that, “the shift to agriculture thus fosters the introduction of malaria, which in turn increases the likelihood that populations with high frequencies of heterozygous sickle cell trait will survive.” (in Hanh, 1995: 60) Finally, medical ecology theorists note the effect of politics and economics on societal health. McElroy and Townsend believe that politics and economics play a major role in the health of a community or society and state these as entities that “must be considered in any model of ecology and health.” (2004: 31) Health Care Systems The health care systems theory is a widely recognized “cultural” theory of health devised by psychiatrist-anthropologist, Arthur Kleinman. Kleinman believes that health practices are part of a larger system of beliefs and values present in each culture. Through cross-cultural analysis, Kleinman has discovered trends and universals that he believes are crucial to understanding and comparing health care systems. He theorizes on the components, factors, and influences that shape the dynamics of a health care system. Kleinman describes internal and external forces that determine the structure of a health care system; the universal clinical functions of a health care system; how explanatory models affect health, outcomes, and Eddie Rooke 4 relationships; the dynamics of therapeutic relationships; and how health care systems are socially and culturally constructed. A health care system contains all “health related components of society” and therefore, “must be studied in a holistic manner as socially organized responses to disease” (Kleinman, 1980: 24). Kleinman believes that in order to understand universals such as patients, healers, illness, and healing we must view actions in the context of cultural environment. By studying health care systems this way, we can begin to make cross-cultural comparisons, which will eventually lead to generalizations (Kleinman, 1980: 8). The social reality of a group of people is created and perpetuated by the community’s institutions, beliefs, values, ideologies, history, and worldview. Likewise, clinical reality is created and influenced by these same forces. This means that realities can vary, sometimes to great degrees, between societies, social groups, professions, communities, families, and individuals (Kleinman, 1980: 36). The structure of a health care system is heavily influenced by external factors such as environment, economy, politics, history, and co-existing institutions. Although these forces greatly affect health care systems, this theory is primarily concerned with factors influencing the inner structure of health care systems. The inner structure of a local health care system is broken down into 3 sectors: the popular sector, the professional sector, and the folk sector. The popular sector is usually the most robust in a given society: “In the United States and Taiwan, roughly 70 to 90 percent of all illness episodes are managed within the popular sector.” (Kleinman, 1980: 50) This level contains the beliefs and actions of individuals, Eddie Rooke 5 families, social networks, and communities and regulates the entrance into the professional and folk sectors (Kleinman, 1980: 50). The professional sector is comprised of groups of organized professionals, which may include western style medicine, Ayurvedic medicine, or traditional Chinese medicine (Kleinman, 1980: 54). When professional health care is brought to a new society, it undergoes a process called indigenization, which is the change and modification made to it so that it suits the local clinical realities. The third sector of a health care system is the folk sector, which includes any non-professional group, or specialist group. Folk practices are often classified as either sacred or secular. Health systems theory identifies 5 main (clinical) functions that can be used for comparison and analysis purposes (Kleinman, 1980: 71). These functions are: 1. The cultural construction of illness as psychosocial experience. 2. The establishment of general criteria to guide the health care seeking process and to evaluate treatment approaches that exist prior to and independent of individual episodes of sickness. 3. The management of particular illness episodes through communicative operations such as labeling and explaining. 4. Healing activities per se, which include all types of therapeutic interventions, from drugs and surgery to psychotherapy, supportive care, and healing rituals. 5. The management of therapeutic outcomes, including cure, treatment failure, recurrence, chronic illness, impairment, and death. (Kleinman, 1980: 71-72) Eddie Rooke 6 Kleinman writes about the difference in explanatory models, which are “the notions about an episode of sickness and its treatment that are employed by all those engaged in the clinical process.” (1980: 105) Explanatory models are found in every health system in the world, and like clinical reality, they differ between societies, communities, families, and individuals. Even more importantly they can differ significantly between patient and healer in all the different sectors of a health care system (Kleinman, 1980: 105). Explanatory models attempt to answer 5 questions: “(1) etiology; (2) time and mode of onset of symptoms; (3) pathophysiology; (4) course of sickness (including both degree of severity and type of sick role – acute, chronic, impaired etc.); and (5) treatment.” (Kleinman, 1980: 105) One last important aspect of Kleinman’s health systems theory is his description of the variables in “practitioner-patient interaction.” (1980: 207) Important variables that can be determined are: institutional setting (specific location among the different sectors and subsectors); characteristics of the interpersonal interaction (number of participants, amount of visits and length of consult, formal or informal, attitudes and views); idiom of communication (method of communicating, explanatory model compatibility); clinical reality (sacred or secular, disease oriented or illness oriented, symbolic or instrumental interventions, therapeutic expectations, and locus of responsibility); and therapeutic stages and mechanisms (structures involved, mechanism of change, adherence, termination, and evaluation of outcome) (Kleinman, 1980: 207-208). Eddie Rooke 7 Critical Medical Anthropology Critical medical anthropology (CMA), which is closely associated with the approach of political economy, is a major theory with many contributors. This theory tends to focus on biomedicine (western, biologically based). Although there are differences in beliefs and emphases, there are a few main and ubiquitous ideas that are unique to CMA. CMA states that it is not sufficient to look at illness and its causes without a thorough analysis of its relationship to the overarching political and economical forces: Critical medical anthropology understands biomedicine not solely as a socially constructed system embedded in a wider cultural pattern, nor only a as mechanistic and depersonalizing structure with important social controls functions in contemporary society, but more broadly in terms of its relationship with the truly global capitalist world economic system (Singer and Baer, 1995: 33). To critical medical anthropologists, power structures at the macro-social level, intermediate-social level, micro-social level, and individual level, all influence the health of a society (Singer and Baer, 1995: 63). Adherents of critical medical anthropology do not ignore the impact of socially constructed realities, environment, and ecology, but are weary of these factors distracting from the larger more ominous factors (Baer, 1996 in Schnurr, 1998: 5). Critical medical anthropologists have been know to criticize ecological/adaptive theories of health for ignoring the ways power regulates access to health resources and determines who is at risk for illness (Hanh, 1995). Eddie Rooke 8 The roots to CMA rest in Marxism, but not all critical medical anthropology theorists and practitioners are strict followers of Marx. Singer and Baer believe that the class struggle is an essential aspect to CMA: Pivotal to the worldview of critical medical anthropology is recognition of class and related race and gender antagonism as the defining characteristics of capitalist society and the reigning world-system. Classes have inherently conflicted social interests, in that, at its heart, capitalism is a system designed to promote the ability of one class to control and expropriate the labor of other classes (1995: 61). Scheper-Hughes has contributed a significant amount of work towards the maturation of CMA and is credited with bringing the theory in touch with the lived experiences of suffers (Singer and Baer, 1995: 44-45). A central premise of CMA is that the capitalist mode of production and consumption, as well as its current hegemony, have led to great inequalities and power differentials. It also sees biomedicine as a structure that helps to perpetuate this capitalist system through both its unquestioned authority and for-profit agenda (Singer and Baer, 1995: 62). Besides commenting on the structures and forces that contribute to sickness and disease, CMA attempts to confront the medicalization of social issues. Medicalization is the transformation of sickness due to social inequality, into a medical diagnosis. This process diverts the blame of the illness from society onto the individual or at least covers up the social and avoidable causes of the illness such as poverty, racism, and exploitation (Schnurr, 1999: 8) Although controversial among academics, many CMA practitioners believe that a crucial role of CMA is to stand up Eddie Rooke 9 against the institutions that contribute to inequality and oppression and therefore bad health. Singer and Baer write in their book, Critical Medical Anthropology that “CMA asserts that its mission is consciously emancipatory and partisan: it aims not simply to understand but to change culturally inappropriate, oppressive and exploitive patterns in the health arena and beyond” and believe that this approach is preferential to the “folly of so-called value-free social science.” (Singer and Baer, 1995: 61) Anthropological Medicine Robert Hanh has his own approach to medical anthropological theory. Hanh makes it clear that theories, which do not account for the constant interaction of different levels of society, are problematic. He analyzes the three major schools of thought in medical anthropology (environmental/ecological/adaptation, cultural, and political economy/CMA) and comes to the conclusion that many of their elements are useful and can be used in conjunction to fully understand sickness and health in a society. Hanh, however, gives priority to critical medical anthropology: “while I believe that a comprehensive theory of sickness and healing must consider adaptation and culture, my own theory would begin with the position of critical medical anthropology.” (1995: 75) Hanh lists four reasons why CMA is an important theoretical starting point. First, he believes that it is essential to take note of how interactions in social settings are highly influenced by forces far removed from local interactions. Second, Hanh believes that critical anthropology is right in addressing the uneven distribution of sickness and power in the world, which is vital to Eddie Rooke 10 understanding a society’s health. Third, CMA acknowledges that theory is a product of culture and is open to this criticism. Finally, Hanh believes that theory and research must be used as tools to correct injustices and inequalities and not to justify them. Hanh believes there is a crisis in health care around the world including in the biomedical strongholds: North America and Europe. There are nearly 50 million Americans without any health insurance (Miller, 2008), the expectations of physicians and patients are often worlds apart (Hanh, 1995: 262), and patients do not feel involved in their treatment plan and are bitter about their physician’s income (Hanh, 1995: 263). Meanwhile, physicians are dissatisfied with practice, do not feel they are respected by their patients, are frustrated with bureaucratization, and are annoyed by insurers scrutinizing their work (Hanh, 1995: 263-264). Hanh’s theory is founded in the principle that medicine does not need to function this way and could work much better for patients and physicians: In brief, anthropological medicine is a theory and practice that gives primacy to sickness – conditions of patients as conceived and unwanted by themselves – that accepts the social and cultural roots of both professional and lay ideas and attitudes about sickness; that fully recognizes the etiology of sickness in social and cultural as well as physiological and environmental conditions; that also acknowledges sociocultural effects in therapy and healing processes and respects the social context of healing; and that addresses the well-being of healers and their patients alike. It integrates a sociocultural perspective with a Eddie Rooke 11 biological one at the core of medical education, medical practice, research, and institutional arrangements (1995: 264-265). Anthropological medicine offers 6 principles that can help remedy the illnesses found in clinical medicine, public health, and international health. One of the core beliefs in anthropology is the importance of listening. By hearing and understanding a patient’s beliefs about sickness and health, life and death, and bodily functions the likelihood of developing a treatment plan and mutual understanding is greatly increased (Hanh, 1995: 275). The past shows that listening has led to successful health programs such as the Polela Health Center in South Africa (Trostle, 1986 in Hanh, 1995: 277). Anthropological medicine recognizes the importance of understanding the context in which people live, such as their social environment, economic status, access to resources, and their exposure to sickness. Medical practitioners may need to become ethonographers (Stein, 1982 in Hanh 1995: 280) in order to come up with a treatment plan that is appropriate to the patient. Otherwise, it may be overlooked that the patient does not have the money for medication, access to three meals a day to take medication with, or that they have other day-to-day hardships that take priority over managing their disease or illness. There is a tendency to lump people who appear to be of one ethnic group into a category of beliefs. This tendency can lead to many problems in healing, so anthropological medicine prescribes recognizing intraethnic variability. There is a long list of factors that can affect beliefs of people from a region: level of education, place of birth, age of immigration, rural life, urban life, degree of involvement in local Eddie Rooke 12 traditions, experience with the medical system, income, occupation, religion, and age (Harwood, 1981 in Hanh, 1995: 281). Studies have found that great variability in beliefs about illness exists within the ethnic categories of “Black”, “Hispanic”, and “Asian/Pacific Islanders” (CDC, 1993a, qtd. in Hanh, 1995: 282). A study by Brieger showed that even among communities in Western Nigeria that all identified as Yoruba, there were large differences in health priorities (1984 in Hanh, 1995: 282). Anthropological medicine addresses the need for “explaining, translating, and brokering” in health care systems (Hanh, 1995: 282). Tests, procedures, and prevention programs may not be understood by people within a health care system; therefore, bilingual and multicultural practitioners and aides are needed in order to reach an understanding between patients and practitioners (Hanh, 1995: 283). Patients often enter the medical system with their own beliefs, taboos, and practices regarding health; which should be respected. These differences in behavior need not be barriers, they simply require that the practitioners and patients accommodate for each other’s needs (Harwood, 1981 in Hanh, 1995: 285). One final principle of anthropological medicine is the need to care for medical practitioners. The needs of all those involved in health have traditionally been ignored, as Stein says in 1982, “For the most part we instruct future clinicians as though they as persons, are not really present. We hope that their years in professional training have effectively socialized out of them any and all subjectivity – the bane of scientific, objective medicine.” (qtd in Hanh, 1995: 287) The long hours, stressful environment, and emotionally challenging cases can be very trying on practitioners that do not have effective coping mechanisms. Unfortunately, “routine Eddie Rooke 13 ways of caring for physicians themselves, particularly as they are affected by the demands of their work, have not been widely established.” (Hanh, 1995: 287) The practice of anthropological medicine in clinical settings makes the experience of the patient’s illness central to treatment and acknowledges the social environment in which that person lives. Arthur Kleinman and his colleagues, Good and Eisenberg, stress the importance of disclosing the different explanatory models (1978 in Hanh, 1995:270) in clinic so that the patient and practitioner are able to create an understanding and a plan for treatment that is appropriate (Katon and Kleinman, 1981 in Hanh, 1995: 270). George Foster (1987) describes a fallacy that he calls the “silver platter model”, which is also known as the “empty vessel” fallacy (Hanh, 1995: 272): when information, technology, or expertise is offered to an individual or a group from the biomedical regime it is assumed to be needed to fill a void or to provide an explanation where one did not exist previously. In reality, there was likely an explanation already in place that was more culturally appropriate, which is why attempts to introduce biomedical concepts to people and groups often fails when adequate understanding has not been reached. Anthropological case studies and research have described ways of packaging, accommodating, and explaining that make information, technology, and expertise palatable not only to specific cultural groups, but to entire societies as well. Other Interesting Theory in Medical Anthropological This next section is devoted to highlighting any other provocative anthropological theory that is not necessarily a “grand theory”. The importance of Eddie Rooke 14 the placebo effect, the socialization of medical students, and knowledge and practice in biomedicine have been analyzed by anthropologists and have led to some very interesting theories. I will briefly outline them here as I feel they are relevant to the purpose of this paper. The Placebo Effect A placebo is a medical intervention that produces a desirable effect for the patient; however the mechanism of this effect is unknown or cannot be proven scientifically. Building on the work of scholars before him, Daniel Moerman has studied the placebo effect and how it affects healing in ethnomedicine and biomedicine. Moerman argues that biomedicine is guilty of ignoring the placebo effect and regard it as unscientific, when in reality, it is as much a part of Westerm medicine as ethnomedicine. His goal is not to discredit the efficacy of biomedicine but to demonstrate the validity of symbolic healing in western cultures and cultures around the globe. Moerman illustrates the placebo effect by examining angina pectoris and two procedures that have been devised by surgeons to deal with patients’ symptoms. The first technique was through indirect revascularization and was reported to have 68% symptomatic improvement (Moerman, 1997: 244). After a double blind study was conducted, it was found that the symptomatic reduction by this technique “could be accounted for by placebo effects, and therefore should be discontinued.” (Moerman, 1997: 244) The second technique is the infamous coronary bypass surgery. Studies have shown that this procedure is successful in reducing symptoms Eddie Rooke 15 “in 80 to 90 percent of patients with severe stable angina pectoris.” (Moerman, 1997: 245) However, a study by Gott and his colleagues in 1973 found a significant number of patients reported reduction of symptoms even when their arteriography showed that their bypass graphs were not functioning (in Moerman, 1997: 246). Moerman believes that this case and others like it are compelling evidence for symbolic healing and its legitimacy and that “the form of medical treatment as well as its content can be effective medical treatment.” (Moerman, 1997: 241. Emphasis in original) Knowledge and Practice in Biomedicine Some fascinating work has been done in anthropology regarding knowledge and practice in biomedicine. A central belief that is held about biomedicine is that its practices are based in scientific evidence, but there is a wealth of evidence to show that this is not the case (Hanh, 1995: 149). McKinlay has found that “many medical interventions are accepted, adopted, and widely used in practice without valid evidence, sometimes with detrimental effects and often at enormous expense.” (1981 qtd. in Hanh, 1995: 150) New procedures are often accepted by physicians after a promising report and eventually the procedure is accepted by the medical community and the public (McKinlay, 1981 from Hanh, 1995: 149). McKinlay found that randomized controlled trials are not done until after the procedure has become standard and argues that they should always be done before the procedure is adopted (1981 from Hanh, 1995: 150). After studying adoptions and scientific evidence behind many medical techniques and procedures, Thomas Chalmers estimated that only 5 % of current medical procedures had been validated with Eddie Rooke 16 controlled clinical trials (1974 from Hanh, 1995: 150). It has also been found that physicians use their personal experience as their primary source of knowledge and clinical reasoning, which many believe is contradictory to the scientific process (Hanh, 1995: 151). Socialization of Students Medical school is notorious for its heavy workload and extensive training. Anthropologists have asked the questions, “how do students deal with this workload?” and “what social transformations happen during those long years of training?” Becker and his colleagues found that students are forced to abandon their “idealistic goal of acquiring all there is to know” about treating patients (1961 from Hanh, 1995: 157). It becomes clear to them that there is too much for them to learn so they instead focus on what “they need for their exams and for later practice.” (Hanh, 1995: 157) During this time, it was found that students learn to deal with uncertainty and patients in an objective, detached manner to prevent getting emotionally involved (Fox, 1956 from Hanh, 1995: 158). Medical students were found to deal with the uncertainties of medical training, knowledge, skill, treatment, and diagnosis by specializing (effectively narrowing their knowledge base) and by adopting “a school of thought, its rationale and its practice, so that they need not repeatedly consider alternatives.” (Light, 1979 qtd. in Hanh, 1995: 159) Students were also believed to develop “a cloak of competence” in order to convince themselves, their patients, and their preceptors that they had the knowledge, and skills necessary to treat patients (Haas and Shaffir, 1987 from Hanh, 1995: 159). Eddie Rooke 17 What Can Medical Students Learn From All This? Medical students could learn a lot from seriously analyzing how medical anthropological theories relate to their field of study. There is such a wealth of theory and research in anthropology that can be considered useful and this is just a small sample. My goal now is to look at this research critically, through the eyes of a medical student/aspiring anthropologist, to discuss some very important questions: “What is most relevant to medical students?”, “What will make their future practice more satisfying and effective?”, and “What information will alter their views of health and illness?” I will begin with a sketch of a typical medical college class, based on my own college, and will then discuss what theories and insights from this sampling of medical anthropology will be “applicable” to medical students. I will start with the macro perspectives of CMA and medical ecology, and progress to cultural medical anthropology and anthropological medicine, which offer insight into micro-level medical issues. Furthermore, I will touch on some additional work that may be of particular interest to medical students that does not fit into any one of the above theories. In Canadian medical schools there is a fair amount of diversity in age, cultural backgrounds, socioeconomic status, and worldviews. This transformation from a predominantly white, male profession can likely be attributed to our multicultural society and the selection process for medical students. There is no direct entry into Canadian medical colleges from high school and all applicants are interviewed prior to offer of admission. As a result, there are a number of applicants who have had Eddie Rooke 18 previous careers or exposure to other health fields, business, music, athletics, social science, humanities, and research. That being said, there are often pre-requisite courses in the sciences required by the college and many applicants are from various fields in science who enter university intent on becoming physicians. Many students come from families with a strong academic emphasis and others from so called “blue collar” families. At the end of the day, the majority of medical students are young, of European descent (although there is a large minority of minorities), have a background in science, are from upper middle class families, and enjoy eating pizza. I begin with critical medical anthropology because it offers insight into the issue of “who gets sick and why”, which is a vital question to ask if we are ever to prevent illness effectively. CMA asserts that we cannot understand health and sickness within a society or on the global scene without understanding the processes that perpetuate inequality. As mentioned above, mode of production, consumption, and exploitation are characteristics of our capitalistic society. It is the values of the few that create the ideologies that perpetuate unequal access to resources vital for health. Privatization of health services has made access to care nearly impossible for the billions living in poverty and among poverty. It is vital that medical professionals have a full understanding of the consequences of health for-profit. By its very nature, privatized health care means that only the financially privileged have access to care. The effects of privatized medicine are not felt by the people living in the upper middle class, which is the background of many medical students, so it is essential in a time where our national organizations are lobbying for private clinics that our soonto-be professionals understand the consequences of privatization. Eddie Rooke 19 Our medical system perpetuates inequality among classes. Medical education is mostly accessible only to individuals who are wealthy or very educated, and so perpetuates the classism we currently have in society. Likewise, the power differentials are played out in clinical situations every single day. Students need to recognize that society’s perception of them as doctors can negatively affect treatment. Although there are practicing doctors who recognize the problems in our system, many students are passively taught to perpetuate the power differentials by the doctors they train under. They learn to objectify patients, to see them as a disease or pathology, and to believe that the answers to their medical problems lie in their biomedical knowledge rather than in the patient’s experience. The result is a quick, impersonal interview; a rushed physical exam; a treatment plan made with little or no patient involvement; and little mutual understanding or satisfaction. This style of medicine has been recognized to be problematic and medical schools now teach interviewing techniques that deal with the patient’s feeling, ideas about causation, how the illness affects the day-to-day functioning of the patient, and the expectations of the patient (know as FIFE: Feeling, Ideas, Functioning, Expectations). “FIFE-ing”, however, does not survive medical school as practicing doctors assure students that it is unrealistic and unnecessary to FIFE patients in “the real world”. Since the bulk of medical training happens in hospitals, with doctors, it seems that in order for initiatives to take root that are aimed at a more pleasant and egalitarian health care experience, practicing physicians must be educated too. This education could prevent those in health care from mistaking a seedling for a weed. Eddie Rooke 20 Medicalization is the process of turning issues that are social in nature into clinical issues. It is important for students to realize that in for-profit medicine it benefits pharmaceutical companies to make social issues into medical issues because it means that they can provide and create drugs to “treat” the condition. Medicalization can also act as an alibi for difficult social/societal problems such as obesity, atherosclerosis, smoking, armchair sports, and binge drinking. Medicalization takes blame, and therefore action, away from the societal level. Perhaps the most important aspect of CMA is its dedication to justice and equality. If medical colleges taught CMA’s knowledge about the great inequalities being perpetuated in the world and explained that health systems both cause and react to injustice and inequality in society, they could build many generations of enlightened and progressive medical professionals. It could, in fact, change the face of medicine. Medical ecology is another perspective that is capable of analysis at the macro and micro-level of health care. The value in medical ecology for the medical student is the idea of inter-connectedness of biotic structures, abiotic structures, and culture that make up the environment (McElroy and Townsend, 2004:29). A change in this environment may have implications at the human population level, all the way down to the tissue level. This is the only model that directly considers biology as an important factor to health. The medical ecology model states, “there is no single cause of disease”, which is an important notion for medical students to understand, as no one gets sick outside of an environmental context. Eddie Rooke 21 The idea of adaptation is an interesting academic concept and can help explain some current health phenomena, but it can also be problematic. The idea that health is a measure of adaptation can be misleading. It can have the effect of placing blame for poor health on a community that has “not adapted well” to its conditions, when it is through political and economic inequality that this change to the environment has occurred in the first place. The concept of adaptation also implies superiority of certain groups and is apolitical and ahistorical. I agree with the CMA’s criticisms of adaptation and believe that learning about adaptation and its problems would actually be an important exercise in critical thought for medical students. Things aren’t always as they appear. Arthur Kleinman is often cited for his many contributions to cultural medical theory by describing the socially constructed nature of health care systems, the three internal structures of health care systems, the universal clinical functions, explanatory models, and the therapeutic relationship. Kleinman’s health systems theory is focused on how culture affects health, especially in clinical circumstances, and that understanding social reality can greatly influence compliance, results, and satisfaction. The essential points for medical students to take away from Kleinman’s work is that a person’s values, ideologies, traditions, and beliefs about sickness influence clinical reality; including how patients present their illnesses, how they communicate, who they go to for healing, and how they view biomedicine. Each patient has his/her own explanatory model, which is their belief about why they are ill and what treatment is needed. It is vital that medical students understand that explanatory models differ greatly from person to person and that mutual disclosure Eddie Rooke 22 of explanatory models can be very effective in ensuring compliance, understanding, and attaining greater satisfaction, and better results. Medical students may also benefit from understanding the role of the popular health sector, the professional health sector, and the folk health sector. Understanding the local practices and lay understanding of disease can help a physician uncover issues of non-compliance or any misunderstandings about treatment. Medical students should learn to respect the popular and folk health sectors, as it is in these sectors that the majority of health issues are “treated”. Anthropological medicine echoes some aspects of the other theories mentioned above and also brings new ideas into the spotlight. The most valuable contribution of this theory to medical students is the practical solutions it brings to building a more satisfying biomedical paradigm in this period of crisis. Doctors need to listen to their patients and negotiate a treatment plan with them. Health, as we have seen, is culturally constructed and has different meaning for all of us. For this reason physicians must not assume that they know what is best for their patients and should be careful not to assume they know the values or beliefs of their patients. The practice of exchanging explanatory models is incredibly valuable for understanding and is a part of cultural brokering that must happen between patient and physician. Medical students must be aware of the different clinical beliefs, expectations, and taboos that people from different cultures possess especially in a multicultural country like Canada. Understanding the “empty vessel” fallacy can prevent misunderstanding and remind students that they must never assume that a patient Eddie Rooke 23 or a group does not have their own way of explaining and dealing with sickness and can help facilitate the transferring of knowledge. The well-being of physicians is severely overlooked in most medical systems and it is time we start thinking about the health of our healers. Our medical system is crowded, hectic, and hyper-focused on efficiency, and biological causes for disease. If we are to create a system that works for the people of Canada, we must become open-minded, patient-focused, and efficacy-oriented, not efficiency-oriented. This can be done in part by following the principles of anthropological medicine. We know that health and sickness are socially created, and so it follows that healing is symbolic by nature. The placebo effect is a powerful phenomenon that is testimony to the symbolic nature of healing. It is important for medical professionals to know that what they are taking part in each day carries great cultural importance to patients and can greatly impact their healing. This is motivation to develop a more humanistic health care experience for the ill and to learn to recognize the importance and validity of traditional healing. Reflecting on the practices in medicine and their experimental nature is an important exercise for health professionals. We say that biomedicine is scientific and conveniently forget the strong history of experimentation and trial and error that we continue to perpetuate. Direct, personal experience is perhaps the oldest and most effective way of learning, but we must also reflect on how our biases can affect our ability to treat in the face of new evidence or “promising reports”. Medical school is a period full of stress and anxiety for many students. They are in a socialization process like no other. If medical students understood, that what Eddie Rooke 24 they are going through is normal or expected, it could potentially alleviate some of this stress. Dealing with the information overload is particularly difficult for many and accepting that uncertainty is a part of being a physician may help students develop more effective coping mechanisms, rather than locking themselves away with their books. Understanding this process and the way physicians have learned to cope also allows us some insight into why the medical system seems slow to change. If it is a coping mechanism to not change one’s practice, then it makes sense why physicians and other professionals in health often seem unwilling to change their ways. Perhaps if there was less pressure on physicians and students to know everything and to have all the answers, it would be easier for them to change their practices and adopt new beliefs about illness and health. Researching this paper has been a thought-provoking and stimulating experience. The insight and knowledge that medical anthropologists offer to understanding and improvement of the healing process is remarkable and incredibly valuable. This paper is a humble attempt to illustrate the variety of applications and uses that medical anthropology offers, particularly to biomedical students who will soon be practicing in our multicultural medical system and our rapidly globalizing world. It is my hope that this paper will be of value to medical students by granting them insight into the ecological, cultural, and political nature of health care. Eddie Rooke 25 References Hanh, Robert. Sickness and Healing: An Anthropological Perspective. New Haven: Yale University Press, 1995. Kleinman, Arthur. Patients and Healers in the Context of Culture: An Exploration of the Boarderland between Anthropology, Medicine, and Psychiatry. Los Angeles, California: University of California Press, 1980. McElroy, Ann and Patricia Townsend. Medical Anthropology in Ecological Perspective. Fourth Ed. Oxford: Westview Press, 2004. Miller, Thomas. “What Do We Know About the Uninsured?”. The American. qtd. from Current Population Survey. U.S. Census Bureau. 2006. Accessed November 20, 2008. http://www.american.com/archive/2008/july-august-magazinecontents/what-do-we-know-about-the-uninsured. Moreman, Daniel. “Physiology and Symbols: The Anthropological Implications of the Placebo Effect”. The Anthropology of Medicine: From Culture to Method. Third Edition. Ed. Lola Romanucci-Ross, Daniel E. Moerman, and Laurence R. Tancredi. Westport, CT: Greenwood Publishing Group, Inc., 1997. 240-253 Schnurr, Joseph. “Critical Medical Anthropology and the Medicalization of Social Distress”. University of Saskatchewan Paper for Professor Alexander Ervin, 1999. Singer, Merril and Hans Baer. Critical Medical Anthropology. New York: Baywood Publishing Company, Inc., 1995.