Polnick, Nikki 1
advertisement

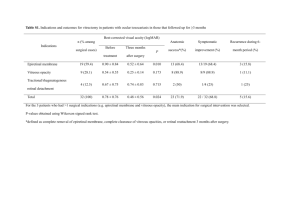
Nikki Polnick, OD and Mahnia Madan, OD Eye Center of Texas Residents, Bellaire, Texas Valsalva Retinopathy: Heart-shaped Pre-retinal Hemorrhage Attributed to Fainting during Blood Donation I. Abstract Valsalva retinopathy occurs when increased pressure transmitted to the eye causes a sharp rise in the intra-ocular venous pressure and rupture of superficial retinal capillaries. Due to its good prognosis, the mainstay treatment is observation. II. Case History a. 33 year old healthy Indian male b. Felt he was looking through a ‘red film’ in his right eye immediately after losing consciousness while donating blood c. Unremarkable ocular history with last eye exam being 3 years prior d. Noncontributory medical history with no evidence of diabetes mellitus, hypertension, anemia, leukemia, or clotting disorders e. Patient denied any recent vomiting, coughing, sneezing, heavy lifting, constipation, or straining f. Reported using a daily multivitamin and denied the use of aspirin or ibuprofen products III. Pertinent Findings a. BCVA: OD: 20/40, OS: 20/20 b. Extra-ocular motilities and confrontation fields were within normal limits c. Pupils were not assessed secondary to dilation from referring doctor d. Intra-ocular pressure measured 16 and 18mmHg in the right and left eye, respectively e. Unremarkable anterior segment in each eye f. Well perfused optic nerve heads with a cup to disk ratio of 0.1 in each eye g. Normal vitreous with no evidence of hemorrhage or posterior vitreous detachment in either eye h. Normal posterior segment in the left eye i. 5DD pre-retinal hemorrhage encompassing the macula in the right eye. No evidence of hard exudates, microaneurysms, dot-blot hemorrhages, flame shaped hemorrhages, venous dilation, vessel tortuosity, cotton wool spots, retinal hole, or retinal tear. Nikki Polnick, OD and Mahnia Madan, OD Eye Center of Texas Residents, Bellaire, Texas IV. Differential Diagnosis a. Posterior vitreous detachment b. Retinal arterial macroaneurysm c. Diabetic retinopathy d. CRVO/BRVO e. Anemia f. Leukemia g. Retinal tear V. Diagnosis and Discussion a. Diagnosis: Pre-retinal hemorrhage in the right eye secondary to probable valsalva retinopathy b. Valsalva retinopathy, a unilateral or bilateral condition, occurs when increased intra-thoracic or intra-abdominal pressure transmitted to the eye causes a sharp rise in the intra-ocular venous pressure and rupture of superficial retinal capillaries. c. Patients can present asymptomatic or with complaints of sudden decreased vision. Most commonly, a history of a recent strenuous act can be elicited. These range in nature from heavy lifting, coughing, sneezing, vomiting, constipation, and straining. Literature reports a higher incidence during pregnancy possibly due to hematological changes such as thrombocytopenia. d. The retinal will reveal single or multiple hemorrhages under the internal limiting membrane in the area of the macula in one or both eyes. On occasion, the pre-retinal hemorrhage can be accompanied by vitreous, subretinal, or subconjunctival hemorrhages. e. Diagnosis is one based on exclusion. All systemic etiologies, including diabetes, hypertension, sickle cell disease, anemia, coagulopathy, blood dyscrasias, and previous ocular vein occlusions must be ruled out. VI. Treatment and Management a. Due to its good prognosis, the mainstay treatment of valsalva retinopathy is observation. On average, the pre-retinal hemorrhage resolves in a few weeks to a several months depending on the size. Recommended followup ranges from every 2 weeks to monthly until resolution. Patients are instructed to avoid aspirin, ibuprofen, and strenuous activity. b. Few patients may have decreased visual acuity after resolution of the hemorrhage secondary to retinal pigmentary changes in the macula or epiretinal membrane formation. c. Literature has reported the use of laser (Nd-YAG-laser hyaloidotomy) to permit blood to drain into the vitreous cavity thereby uncovering the macula and preventing any retinal pigmentary changes in the macular Nikki Polnick, OD and Mahnia Madan, OD Eye Center of Texas Residents, Bellaire, Texas from occurring. With treatment, 100% of patients had resolution at 1 month.2 This treatment is not without risks, which include macular hole formation, macular tear, and retinal detachment. d. Vitrectomy is rarely performed and only when non-clearing vitreous hemorrhages are present. VII. Conclusion a. Valsalva retinopathy, a self-limiting condition, is a diagnosis of exclusion. All causes of retinal hemorrhages need to be ruled out. b. Due to the good prognosis of this retinopathy, one must weigh the risks and benefits of treatment versus observation. VIII. References a. Al-Mujaini A, Montana C. Valsalva retinopathy in pregnancy: a case report. Journal of Medical Case Reports 2008; 2:101. b. Khan M, Shehzad M. Nd:YAG laser treatment for Valsalva premacular hemorrhages: 6 month follow up. Int Ophthalmol 2008; 28:325-327. c. Perez-Rico C, Montes-Mollon A, Castro-Rebollo M, Pareja-Esteban J, Benitez-Herreros J. Optical coherence tomography features of sub-internal limiting membrane hemorrhage and temporary premacular cavity following Nd-YAG laser membranotomy in valsalva retinopathy. Jpn J Ophthalmol 2008; 52:513-515. d. Kirwan RP, Cahill MT. Nd:YAG laser hyaloidotomy for valsalva premacular hemorrhage. Ir J Med Sci 2009; online.