1. general information - Wellington Intensive Care Unit
advertisement

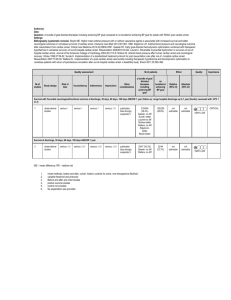
HOT or NOT CLINICAL TRIAL PROTOCOL The HyperOxia Therapy OR NormOxic Therapy cardiac arrest study (HOT OR NOT) A multi-centred phase 2b randomised, parallel groups, single blind, clinical trial investigating the safety, efficacy and feasibility of a strategy of avoidance of hyperoxia versus standard care in patients resuscitated from out-of-hospital VF and VT cardiac arrest CLINICAL TRIAL PROTOCOL PROTOCOL NAME: HOT OR NOT PROTOCOL VERSION: version 2 PROTOCOL DATE: 21/02/12 - ANZCTRN: TBA Ethics Approval: MEC 12/01/003 Funding: TBA HOT OR NOT clinical trial protocol: v2,21/02/2012 1 HOT or NOT TABLE OF CONTENTS LIST OF DEFINITIONS AND ABBREVIATIONS ................................................ 4 1. GENERAL INFORMATION ................................................................................. 5 1.1 Title ............................................................................................................................. 5 1.2 Chief investigator ....................................................................................................... 5 1.3 Coordinating and data management centre ............................................................ 5 2. BACKGROUND INFORMATION ...................................................................... 6 2.1 Background.................................................................................................................... 6 2.2 Animal Studies............................................................................................................... 6 2.3 Human Data................................................................................................................... 8 2.4 Rationale for the HOT OR NOT trial ......................................................................... 9 2.5 Trial feasibility .............................................................................................................. 9 3.1 Primary aim ................................................................................................................. 10 3.2 Secondary aims ............................................................................................................ 10 3.3 Tertiary aims ............................................................................................................... 10 5 ASSESSMENT OF EFFICACY ............................................................................ 10 5.1 Specification of the efficacy parameters.................................................................... 10 5.1.1 Primary outcome .................................................................................................................. 10 5.1.2 Secondary outcomes ............................................................................................................ 11 5.1.3 Tertiary outcomes ................................................................................................................ 12 6 SELECTION OF PARTICIPANTS ...................................................................... 12 6.1 Inclusion criteria ......................................................................................................... 12 6.2 Exclusion criteria ........................................................................................................ 12 8 TREATMENT OF PARTICIPANTS ................................................................... 13 8.1 Overview of Study Design .......................................................................................... 13 8.3 Concomitant treatment during trial period .............................................................. 13 8.4 Withdrawal of study treatment.................................................................................. 13 8.4.1 Withdrawal of study treatment criteria................................................................................. 13 8.4.2 Management of patients for whom study treatment has been withdrawn ............................ 14 10 STUDY TERMINATION .................................................................................... 14 11 STUDY PROCEDURES ...................................................................................... 14 11.1 Data collection ........................................................................................................... 14 11.2 Screening Log ............................................................................................................ 14 11.3 Data management of patients for whom study treatment has been withdrawn .. 14 11.4 Method of data collection ......................................................................................... 15 11.5 Case Report Forms ................................................................................................... 15 12 ASSESSMENT OF SAFETY ............................................................................... 15 12.1 Adverse Event and Serious Adverse Event Reporting .......................................... 15 12.1.1 Definitions.......................................................................................................................... 15 HOT OR NOT clinical trial protocol: v2,21/02/2012 2 HOT or NOT 12.2 Study safety reporting............................................................................................... 15 14 STATISTICS ......................................................................................................... 16 14.1 Sample size and justification .................................................................................... 16 14.1.1 Sample size ........................................................................................................................ 16 14.1.2 Justification ........................................................................................................................ 16 14.2 Statistical methods .................................................................................................... 16 14.2.1 Patient Characteristics ........................................................................................................ 17 14.2.2 Efficacy, Safety and Feasibility Analysis .......................................................................... 17 14.2.3 Efficacy, Safety and Feasibility Analysis .......................................................................... 17 14.2.4 Efficacy, Safety and Feasibility Analysis .......................................................................... 17 15 DIRECT ACCESS TO DATA & DOCUMENTS .............................................. 18 16 QUALITY CONTROL AND QUALITY ASSURANCE MONITORING ..... 18 16.1 Responsibilities of the principal investigator at each site ...................................... 18 16.2 Responsibilities of the co-coordinating centre ........................................................ 18 16.3 Source document requirements ............................................................................... 19 16.4 Management of protocol deviations ........................................................................ 19 17 ETHICAL CONSIDERATIONS ......................................................................... 19 17.1 Ethical Principles ...................................................................................................... 19 17.2 Independent Ethics Committee ................................................................................ 20 17.3 Informed Consent ..................................................................................................... 20 18 DATA HANDLING AND RECORD KEEPING ............................................... 21 19 FINANCING AND INSURANCE ....................................................................... 21 19.1 Funding ...................................................................................................................... 21 19.2 Participating Centres agreement ............................................................................. 21 20 PUBLICATION POLICY .................................................................................... 22 23 REFERENCES ...................................................................................................... 23 HOT OR NOT clinical trial protocol: v2,21/02/2012 3 HOT or NOT LIST OF DEFINITIONS AND ABBREVIATIONS ABG Arterial Blood Gas AE Adverse Event ANZICS-CTG Australian and New Zealand Intensive Care Society- Clinical Trials Group CI Chief Investigator CPR Cardiopulmonary Resuscitation eCRF Electronic Case Report Form FiO2 Inspired Oxygen Concentration NSE Neuron specific enolase NZ New Zealand PI Principal Investigator ROSC Return of spontaneous circulation S-100B Protein soluble in 100% ammonium sulphate SAE Serious adverse event VF Ventricular Fibrillation VT Ventricular Tachycardia HOT OR NOT clinical trial protocol: v2,21/02/2012 4 HOT or NOT 1. GENERAL INFORMATION 1.1 Title The HyperOxia Therapy OR NormOxic Therapy Cardiac Arrest Study (The HOT OR NOT Cardiac Arrest Study) 1.2 Chief investigator Name: Title: Address: Contact Number: Fax number: Email: Dr Paul Young Staff Specialist in Intensive Care, Wellington Regional Hospital, Private Bag 7902, Wellington South (027) 455 2269 (04) 806 0430 paul.young@ccdhb.org.nz 1.3 Coordinating and data management centre Medical Research Institute of New Zealand Private Bag 7902 Wellington 6242 New Zealand HOT OR NOT clinical trial protocol: v2,21/02/2012 5 HOT or NOT 2. BACKGROUND INFORMATION 2.1 Background Cardiovascular disease is the leading cause of death in New Zealand (NZ), accounting for 40% of deaths annually.1 It is responsible for 4200 and 2200 hospitalisations per 100,000 people in Maori and Non-Maori respectively.2 Using recent Wellington Free Ambulance data,3,4 there are an estimated 1,545 cases of out-of-hospital cardiac arrest attended by paramedics per year in NZ. The survival of these patients is poor, with only 36% surviving to hospital admission, and 12% surviving to discharge from hospital.3 The most common form of out-of-hospital cardiac arrest is a primary cardiac arrhythmia, either ventricular fibrillation (VF) or ventricular tachycardia (VT), and in this group the prognosis is relatively better, but still poor with 21% of patients who suffer a VF or VT arrest surviving to hospital discharge.3 Although, ischaemic heart disease is the most common cause of such cardiac arrests, in patients who suffer out-of-hospital cardiac arrest and survive to reach hospital, much of the morbidity and mortality that occurs is attributable to neurological injury. When this neurological injury occurs, it is typically devastating and leads to the patient dying in hospital or being discharged to nursing home care. Investigating novel management strategies that might improve survival is an important priority if the considerable public health burden of mortality and significant morbidity from out-of-hospital cardiac arrest can be reduced in NZ. 2.2 Animal Studies We have recently completed a systemic review and meta-analysis of animal data demonstrating that exposure to hyperoxia around the time of cardiac arrest worsens neurological injury in animal models.5 As summarised in Figure 1, treatment with 100% oxygen results in a significantly worse neurological deficit scores than oxygen administered at lower concentrations.5 Figure 1: Summary of standardised mean differences in studies comparing hyperoxic and normoxic regimes in animal cardiac arrest models HOT OR NOT clinical trial protocol: v2,21/02/2012 6 HOT or NOT Lipinski15 Brűken11 Zwemer10 Yeh14 Liu8 Balan12 Pooled -4 Favors normoxia -3 -2 -0.64 (-1.06 to -0.22) -1 0 1 2 3 4 Published animal studies generally involve inducing cardiac arrest by electrical 6-12, or chemical13,14 means; however, the one study15 in our meta-analysis that did not demonstrate a trend favouring normoxia induced cardiac arrest through asphyxia. Most animal studies involve the comparison of 100% oxygen during and after resuscitation (hyperoxia arm) with a regime that involves administration of room air during cardiopulmonary resuscitation followed by administration of inspired oxygen between 21 and 30% after return of spontaneous circulation (normoxia group). Such normoxic regimes are potentially problematic in the setting of human cardiac arrest given that hypoxia is harmful and some patients do have severe hypoxaemia despite administration of high concentration of oxygen due to aspiration. The animal study, which has the most relevance to our proposed study, was performed in dogs and compared a pulse oximetry-guided strategy (oximetry group) with administration of 100% oxygen (hyperoxic group).12 This study involved electrically-induced cardiac arrest followed by 10 minutes without CPR, then 3 minutes of CPR and then, finally, internal defibrillation along with administration of adrenaline. The hyperoxic group received 100% oxygen during and for 1 hour after resuscitation after which time arterial blood gas (ABG) guided adjustments were used to achieve physiological PaO2 levels. In the oximetry group, animals received 100% oxygen during resuscitation. Immediately upon return of spontaneous circulation (ROSC), oxygen was reduced to 50%. Thereafter, 5% reductions in FiO 2 were performed every 2 minutes until desaturation to less than 96% on pulse oximeter occurred. Once this occurred, ABG guided adjustments were used to achieve physiological PaO2 levels. Effectively, this meant an FiO2 of 21% to 30% was achieved within 12 minutes of ROSC. In this study, histological staining techniques were used to compare the extent of the neuronal damage in the two groups and neurological outcomes at 24 hours post ROSC were assessed using a previously validated neurological deficit score16 comparing 18 parameters in the following five categories: (i) level of consciousness, (ii) respiration, (iii) cranial nerve function, (iv) sensory function, (v) behaviour. The possible neurological deficit scored ranged from 0 (normal) to 100 (brain dead). An oximetry-guided strategy resulted in better neurological function and reduced hippocampal neuronal injury as HOT OR NOT clinical trial protocol: v2,21/02/2012 7 HOT or NOT shown in Figure 2. Figure 2: Individual variation of neuronal injury in the dorsal CA1 region of the hippocampus based on cresyl violet-staining and neurological deficit score 24 hours after return of spontaneous circulation 2.3 Human Data There is evidence that resuscitation with 100% oxygen has the potential to cause harm from studies of resuscitation of newborn babies. Until recently, routine clinical practice was to use 100% oxygen for resuscitation at birth; however, RCTs have shown that neonatal mortality is reduced by a third with room air compared with 100% oxygen treatment.17 Relevant to our proposal, there is evidence that 40% oxygen may result in earlier recovery than 100% oxygen in neonatal resuscitation.18 In adult cardiac arrest, existing evidence on oxygen administration is essentially limited to three large retrospective studies.19-21 The first retrospective study reported that hyperoxia, determined on the first ABG measurement after ICU admission, was associated with an increased risk of inhospital mortality, compared to patients with either normoxia or hypoxia.19 Unusually, this study classed all patients with a PaO2/FiO2 ratio of <300 as hypoxic irrespective of their PaO2. A second retrospective study, based on the same database, but excluding all patients with a PaO2/FiO2 ratio of <200, found a strong association between increasing supra-normal levels of PaO2 and mortality.20 In contrast to these studies, data from the Australian and New Zealand Intensive Care Society Adult Patient Database, which used data from the ‘worst ABG’ in patients admitted to ICUs in Australia and New Zealand after cardiac arrest, did not find an association between elevated PaO2 and mortality after adjustment for illness severity and inspired oxygen concentration.21 However, the Australasian data did confirm that hypoxia is associated with worse outcome than normoxia and hyperoxia in patients admitted to ICU following cardiac arrest. In addition to the large retrospective studies a small pilot randomised controlled trial has demonstrated that the delivery of lower concentrations than the standard of FiO2 100% by the ambulance is feasible.22 This trial was not powered to determine whether avoidance of hyperoxia affected outcome. HOT OR NOT clinical trial protocol: v2,21/02/2012 8 HOT or NOT The existing literature does not answer the question as to whether avoidance of hyperoxia might improve neurological outcome after cardiac arrest. Although the existing retrospective studies were large, all are limited as they used databases that were not designed to examine the question of whether avoidance of hyperoxia improves outcome. Additionally, the two North American studies failed to appropriately adjust for inspired oxygen concentration or illness severity. 2.4 Rationale for the HOT OR NOT trial Despite oxygen being a ubiquitous therapy in patients resuscitated from cardiac arrest, there is very little high quality evidence to guide clinicians and, with the exception of one small pilot trial,22 no previous prospective study of different oxygen regimes in patients resuscitated from cardiac arrest has been performed. A randomised trial of strategy of avoidance of hyperoxia versus standard care in patients resuscitated from out-of-hospital VF and VT cardiac arrest is being conducted for several reasons. There is a sound scientific basis for the hypothesis that avoidance of hyperoxia might reduce neurological injury after resuscitation from cardiac arrest. However, existing human data from retrospective trials are inconclusive and highlight the risks associated with hypoxia. Despite these risks, high profile retrospective studies19,20 have indicated the possibility that hyperoxia is harmful and, in the absence of prospective data, may lead to practice change which potentially exposes patients to the harms of hypoxia. This aim of this trial is to determine whether avoidance of hyperoxia improves neurological outcome and reduces levels of NSE (neurone specific enolase), and S100B (protein soluble in 100% ammonium sulphate) compared to standard care. These validated markers of neuronal injury predict outcome of resuscitation from cardiac arrest.23-27 Data from this study will determine whether a strategy of hyperoxia avoidance is feasible and safe. It will also determine how readily patients can be recruited into the trial and will provide efficacy data in relation to important clinical end points. Such data are necessary to establish whether a pivotal phase III trial is needed. 2.5 Trial feasibility The investigators have an established track record of excellence in the conduct of both small- and large-scale randomised-controlled trials in intensive care in Australia and New Zealand. The Saline and Albumin Fluid Evaluation study28 and the Normoglycaemia in Intensive Care study,29 conducted by the Australian and New Zealand Intensive Care Society Clinical Trials Group (ANZICS CTG) are regarded as a benchmark for trials in Critical Care Medicine. Together these trials randomised 13,000 patients. Our team includes established pre-hospital and intensive care researchers. Detailed data collected from Wellington Free Ambulance have been used to determine feasibility.3 The Wellington Free Ambulance services a population of 473,700. Over a two and a half year period between July 2007 and December 2009, the Wellington free ambulance attended 362 cardiac arrests in which resuscitation was attempted. Of these, 161 had a presenting rhythm of VF or VT. Of these, 83/161 (48%) survived to hospital. Of those surviving until hospital admission, 9/83 (11%) were admitted directly to a coronary care unit rather than an ICU (and hence were likely conscious) and 10/83 (12%) died in the emergency department. The remaining 64 patients would likely fulfil eligibility criteria and survive to reach assessment of the primary end point at 24 hours post ROSC. Assuming that the Auckland region (population 1,303,068) had three times as many patients as HOT OR NOT clinical trial protocol: v2,21/02/2012 9 HOT or NOT Wellington and the remaining centres (Christchurch, Dunedin and Hawkes Bay) were able to recruit the same number between them, a total of 320 patients could be recruited over a two and half year period and expected to survive until 24 hours post ROSC for assessment of the primary end point. 3 TRIAL AIM & HYPOTHESIS 3.1 Primary aim The primary aim of this study is to determine whether a strategy that limits exposure to hyperoxia after out-of-hospital VF/VT cardiac arrest, improves neurological outcomes and reduces levels of NSE levels measured 24-hour post ROSC. The study will establish whether a definitive phase III trial is safe, feasible and justifiable, and will provide essential information on the cost and likely sample size for such a trial. 3.2 Secondary aims Secondary aims are to determine whether a strategy that limits exposure to hyperoxia after out-of-hospital VF/VT cardiac arrest: 1. Reduces S-100B levels measured at hospital admission,12, 24, 48, and 72 hours post-ROSC 2. Reduces NSE levels measured at hospital admission, 12, 48, and 72 hours postROSC 3. Reduces the duration of ICU and hospital stay 4. Reduces mean PaO2 5. Alters mean PaCO2 6. Alters the number of documented episodes of desaturation 7. Alters the number of documented episodes of hyperoxia 8. Alters the number of episodes of cardiac arrest 9. Reduces high sensitivity troponin levels measured at hospital discharge, 12, 24, 48 and 72 hours post-ROSC 3.3 Tertiary aims To determine the recruitment rate and incidence of protocol violation with a view to the feasibility of using this design for a larger phase 3 trial. 4 TRIAL DESIGN The HOT OR NOT trial is a prospective, phase 2b, multi-centre, single-blinded, parallel-groups randomised placebo-controlled trial, designed to determine the safety, efficacy and feasibility of a strategy of avoidance of hyperoxia versus standard care in patients resuscitated from out-of-hospital VF and VT cardiac arrest. 5 ASSESSMENT OF EFFICACY 5.1 Specification of the efficacy parameters 5.1.1 Main outcomes Neuron specific enolase NSE is a glycolytic enzyme that is localised primarily in the neuronal cytoplasm. The enzyme is released into the cerebrospinal fluid and plasma with neural tissue injury HOT OR NOT clinical trial protocol: v2,21/02/2012 10 HOT or NOT and is elevated after a variety of types of neurological injury. In patients who have suffered out-of-hospital cardiac arrest, numerous studies have demonstrated a correlation between NSE and poor outcome.23-27 NSE levels are significantly lower in comatose cardiac arrest survivors who undergo therapeutic hypothermia than those who do not, indicating that this measurement can potentially guide response to therapy.26 Therapeutic hypothermia has been conclusively shown to improve neurological outcome after cardiac arrest.30,31 Assessment of neurological outcome: The method for assessing neurological outcome will be by assessment of the proportion of patients who survive to hospital discharge with sufficiently good neurological function to be discharged home or to a rehabilitation facility. This method has been used previously in interventional studies of patients post cardiac arrest.31,33 5.1.2 Secondary outcomes NSE and S-100B: In addition to the measurement for primary end point determination at 24 hours, NSE and S-100B will be measured at hospital admission, 12, 48 and 72 hours post ROSC. These additional measurements will be used to determine the levels of NSE and S-100B by ANOVA for repeated measurements. It will also be used to determine the proportion of patients who have a decrease in NSE and S-100B between 24 and 48 hours both of which have been shown to predict favourable neurological outcome.26,32 S-100B is a calcium binding protein located primarily in astroglial cells. It has been shown to be elevated after a variety of types of neurological injury including anoxic brain injury following cardiac arrest.26 Duration of ICU and Hospital stay: These measurements of clinical response to treatment and health service requirements are important in their own right. In order to deal with the issue of competing risk of death, we will analyse survivors and non-survivors separately. Mean PaO2: Mean PaO2 will be measured 6 hourly in ICU up until extubation or 72 hours (whichever is first). The purpose of measuring PaO2 is to determine that a strategy of hyperoxia avoidance in ICU does, in fact, reduce PaO2 levels compared to standard care. Mean PaCO2: Mean PaCO2 will be measured 6 hourly in ICU up until extubation or 72 hours (whichever is first). PaCO2 has important effects on cerebral blood flow.34 The purpose of determining PaCO2 is to determine that a strategy of hyperoxia avoidance in ICU does not have confounding effects on PaCO2. Episodes of hypoxia Previous studies have shown that hypoxia is associated with worse outcomes in patients admitted to ICU after cardiac arrest.19-21 We will record all documented episodes in which desaturation to below 88% is recorded by pulse oximetry. The purpose of measuring episodes of desaturation is to determine whether a strategy of hyperoxia avoidance increases the incidence of desaturation episodes. Episodes of hyperoxia: HOT OR NOT clinical trial protocol: v2,21/02/2012 11 HOT or NOT Previous studies have shown that hypoxia is associated with worse outcomes in patients admitted to ICU after cardiac arrest. We will record all episodes in which a PaO2 of > 120mmHg is documented on arterial blood gas. The purpose of measuring episodes of hyperoxia is to determine whether a strategy of oxygen titration increases the incidence of hyperoxic episodes. Episodes of cardiac arrest: We will record the number of cardiac arrest events after initial ROSC. The purpose of measuring this is to determine whether a strategy of oxygen titration alters the risk of further episodes of cardiac arrest. hsTNT levels: hsTNT will be measured at hospital admission,12, 24, 48 and 72 hours post ROSC. These measurements will be used to determine whether the oxygen strategies affect myocardial injury post resuscitation from cardiac arrest 5.1.3 Tertiary outcomes Recruitment To determine the number of patients recruited into the study as a proportion of total eligible patients. 6 SELECTION OF PARTICIPANTS Patients who fulfil all of the inclusion criteria and none of the exclusion criteria will be eligible for enrolment. 6.1 Inclusion criteria 1. 2. 3. 4. Cardiac arrest due to a primary cardiac cause with an initial rhythm of VF or VT Aged 16-90 years Ventilated via endotracheal tube or laryngeal mask airway Working pulse oximetry obtained within 15 minutes of ROSC 6.2 Exclusion criteria 1. obvious pregnancy 2. dependant on others for activities of daily living (i.e. in supported care or nursing home residents), 3. terminal disease 7 RANDOMISATION AND ALLOCATION OF TREATMENT Randomisation will be achieved by sequential numbered sealed envelopes, which will be prepared by a third party, who will receive a randomisation schedule generated by a statistician. There will be block randomisation with a block size of 6, stratified by study centre. Patients will be randomly assigned to either the ‘avoidance of hyperoxia’ or ‘standard care’ in a 1:1 ratio by the paramedics when they fulfil eligibility criteria. Note: where the ‘first responder’ to the cardiac arrest is the Fire Service,3 paramedics may still randomise patients provided that randomisation can be achieved within 15 minutes of return of spontaneous circulation Patients will be blinded as to the treatment allocation; however, due to the nature of the intervention, blinding of investigators will not be possible. HOT OR NOT clinical trial protocol: v2,21/02/2012 12 HOT or NOT 8 TREATMENT OF PARTICIPANTS 8.1 Overview of Study Design This study is a multicentre, randomised, single-blind, parallel, phase 2b study investigating the safety, efficacy and feasibility of a strategy of avoidance of hyperoxia versus standard care in patients resuscitated from out-of-hospital VF and VT cardiac arrest. 8.2 Study treatment and dosage regimen Patients assigned to the ‘standard care’ arm will receive usual care. This will involve administration of 100% oxygen by the ambulance officers and in the initial period in the emergency department. Subsequently, the oxygen target will be determined by the treating clinician in accordance with usual clinical practice. Data from our multicentre retrospective cohort study indicate that this standard care arm will lead to significant exposure to hyperoxia during ICU phase of management.35 It is anticipated that usual care will involve targeting oxygen saturation of >95% on a pulse oximeter. The use of such a ‘standard care’ arm is important because it will increase the generalisability of results and help to lay the ground work for a large pragmatic phase III trial (if our results indicate that such a trial is justified) Patients assigned to the ‘avoidance of hyperoxia’ arm will receive titrated oxygen from the time of ROSC aiming to achieve oxygen saturation of 90-94% via pulse oximeter. After randomisation patients in the ‘avoidance of hyperoxia’ arm will continue to receive titrated oxygen in the ambulance with delivery adjusted by adjustment of the oxygen flow meter. Titrated oxygen therapy will be maintained throughout the period of treatment in the emergency department and ICU up until extubation or 72 hours post ROSC (whichever is sooner). 8.3 Concomitant treatment during trial period Apart from the randomised oxygen interventions, patients will receive standard care (including therapeutic hypothermia if clinically appropriate). If a patient has further cardiac arrest after their initial return of spontaneous circulation, oxygen may be increased irrespective of which group the patient is assigned to at the discretion of the treating paramedic or doctor. If the patient is successfully resuscitated, oxygen should again be titrated according to the treatment to which the patient has been assigned. 8.4 Withdrawal of study treatment The patient (or the person responsible for the patient) may withdraw from study treatment at any time, irrespective of the reason. The treating clinician may also withdraw the patient from study treatment if it is felt that withdrawal from study treatment is in the patient’s best interests. The reason for withdrawal of treatment will be recorded in the electronic case report form (eCRF). All treatment discontinuation should also be recorded by the investigator in the source notes. 8.4.1 Withdrawal of study treatment criteria There are no pre-specified criteria for mandatory treatment withdrawal HOT OR NOT clinical trial protocol: v2,21/02/2012 13 HOT or NOT 8.4.2 Management of patients for whom study treatment has been withdrawn Patients withdrawn from the randomised treatment for any reason will be followed up according to the study follow up schedule and analysed according to the intention-totreat-principle unless the patient or their legal surrogate has specifically withdrawn consent to follow up data being used. A withdrawal form will be completed if a patient or their legal surrogate withdraws consent for data collection. Where a patient or their legal surrogate withdraws consent, the patient will be considered as lost to follow-up. 9 DURATION OF PARTICIPATION All patients will be followed until the earliest of any of the following: Discharge from acute hospital Withdrawal of consent, by subject or legal surrogate Patient death 10 STUDY TERMINATION The study may be terminated at any time at the request of the study management committee, the Investigator, or a regulatory authority, with proper and timely notification of all parties concerned. The Ethics Committee will be informed promptly and the co-ordinating centre or the investigator will supply reason(s) for the termination or suspension, as specified by the applicable regulatory requirements. Otherwise, the study is considered terminated upon completion of all patient treatments and evaluations. 11 STUDY PROCEDURES 11.1 Data collection Data collection will be collected by ICU research co-ordinators at each participating hospital and entered electronically via a secure web-based data entry system. The coordinating centre will take responsibility for the data management of the study. This includes programming and data management support of the database during the study. 11.2 Screening Log The screening log is designed to monitor patient recruitment and will allow the construction of a CONSORT diagram.36 A screening log of cardiac arrest patients will be maintained by ambulance services in respective regions with data entry into an online screening log performed by ambulance service representatives. 11.3 Data management of patients for whom study treatment has been withdrawn In patients in whom allocated study treatment is been discontinued for any reason, the follow-up schedule must continue unchanged for all randomised participants unless the patient or their representative has specifically withdrawn consent to follow up. Efforts will be made to follow all study participants, irrespective of their adherence to the randomised therapy. All losses to follow-up with reason will be reported to the coordinating centre and reviewed by the Study Management Committee. HOT OR NOT clinical trial protocol: v2,21/02/2012 14 HOT or NOT Patients withdrawn from randomised study treatment will be categorised as lost to follow-up and, where possible, will be included in the final analysis on an intention to treat basis. 11.4 Method of data collection Data collected while the patient is in the ICU will be from the ambulance record and the patient medical record and will be performed by trained ICU research coordinator. 11.5 Case Report Forms The electronic case report form (eCRF) will be developed by the management committee. Research co-coordinators will enter all required data described in the protocol onto eCRF. Information recorded in the CRF should accurately reflect the subject’s medical/hospital notes. Information must be completed in the eCRF as soon as it is available for recording. The intent of this process is to improve the quality of the clinical study by providing prompt feedback to the investigators on the progress of the data submitted and to enhance the ability to collect early safety information in a more timely fashion. 12 ASSESSMENT OF SAFETY 12.1 Adverse Event and Serious Adverse Event Reporting 12.1.1 Definitions 12.1.1.1 Adverse events (AEs) AEs are defined as any untoward medical occurrence in a patient administered an investigational intervention and which does not necessarily have to have a causal relationship with that intervention. 12.1.1.2 Serious adverse events (SAEs) SAEs are defined as any untoward medical occurrence that meets one of more of the following criteria: Results in death Is life threatening Requires inpatient hospitalisation or prolongation of existing hospitalisation Results in persistent or significant disability or incapacity Is a congenital anomaly or birth defect Is an important medical event, other than listed above, that the clinician believes may jeopardise the patient or require intervention to prevent one of the above outcomes 12.2 Study safety reporting It is recognised that the patient population post cardiac arrest will experience a number of aberrations in laboratory values, signs and symptoms due to the severity of the underlying disease and the impact of standard therapies. In this study, only those AEs and SAEs which are thought to have a causal relationship with study treatment should be reported. HOT OR NOT clinical trial protocol: v2,21/02/2012 15 HOT or NOT All SAEs should be reported by telephone to the coordinating centre within 24 hours of the awareness of the event. All non-serious AEs, that are not already captured on the eCRF should be reported to the coordinating centre within 48 hours of the awareness of the event. The co-ordinating centre staff will be responsible for following-up adverse events to ensure all details are available. The co-ordinating centre is also responsible for alerting other participating centres of the report of an AE and reporting AEs to the Multi-region Ethics Committee for New Zealand. 13 DATA MONITORING COMMITTEE A Data Monitoring Committee (DMC), independent from the investigators, will perform an ongoing review of predefined safety parameters and overall study conduct. The DMC will be comprised of experts in clinical trials and methodology. The DMC’s primary function is to ensure the safety and welfare of the patients. The DMC will review data on patient characteristics, specified outcomes and reportable adverse events at predetermined intervals during the study or as deemed appropriate by the DMC. Independent monitoring of data collected at participating centres in this study will be undertaken by the Medical Research Institute of New Zealand. 14 STATISTICS 14.1 Sample size and justification 14.1.1 Sample size The planned sample size is 150 patients. 14.1.2 Justification We have chosen a sample size of 150 participants with ROSC in each group to account for both the NSE measure and the categorical clinical outcome variable. If 64 participants in each group survive to reach assessment of NSE this sample size will provide 80% power with a type I error rate of 5%, to detect a decrease in NSE levels at 24 hours after ROSC from a mean (standard deviation) 13.0 +/- 7.3 µg/L based on reference22 9.35 +/- 7.3 µg/L. This difference represents 0.5 of a standard deviation and is less than the 0.6 standard deviation difference in neurological deficit score observed in our meta-analysis of animal models of cardiac arrest and oxygen use5. For the categorical outcome variable, survival to hospital discharge with a sufficiently good neurological outcome to be discharged home or to a rehabilitation facility, we plan to detect an increase in the proportion of patients with a good outcome from 49% based on reference31 to 71%, again with 80% power and an alpha of 0.05. This sample size provides greater power than the New England Journal of Medicine paper which used this outcome variable and studied a total of 77 subjects demonstrating that therapeutic hypothermia following cardiac arrest increases the number of patients with good neurological outcome31. 14.2 Statistical methods A detailed statistical analysis plan will be developed before completion of recruitment and published in a public domain before commencement of analysis. HOT OR NOT clinical trial protocol: v2,21/02/2012 16 HOT or NOT 14.2.1 Patient Characteristics The distribution of participant characteristics will be explored. These variables will be: age sex ethnicity whether the cardiac arrest was witnessed whether bystander CPR was performed time from pick up of ambulance call until first ambulance arrival time from first ambulance arrival until ROSC time from pick up of call until ROSC time from pick up of call until defibrillation number of defibrillations number of doses of adrenaline prior to ROSC systolic blood pressure immediately post ROSC heart rate immediately post ROSC oxygen saturation post ROSC end tidal CO2 post ROSC 14.2.2 Efficacy, Safety and Feasibility Analysis The main analysis of NSE at 24 hours after ROSC, will be a t-test as long as statistical assumptions are met. If normality assumptions are not met then we plan to try first a simple data transformation, such as a logarithm transformation, and if this fails to proceed to a Mann-Whitney rank based test. The proportion of patients achieving a good neurological outcome in each group will be compared using Fisher’s Exact test. Because this study has feasibility and planning aims secondary analyses of the main outcome variables will be multivariate regressions to determine if there are important co-variates that contribute to the outcomes. These might form the basis of stratified randomisation in a larger study. These will be explored using simple plots, tables, and univariate linear regressions, followed by model building to find a single or small set of models that provide a good fit to the data. We plan to use best sub-sets analysis although this model building will necessarily be iterative. For the secondary outcome variables which can be treated as continuous a similar analysis strategy will be used. For categorical outcome variables logistic regression will be used after simple tabulations and measures of association with a similar model building strategy. Some variables are measured repeatedly and for these variables plots supplemented by linear mixed models will be used to determine if there is a different pattern of change with time by randomised group. 14.2.3 Subgroup Analysis There are no pre-specified subgroup analyses 14.2.4 Data Monitoring Committee The Data Monitoring Committee will perform one interim analyses when 50% of participants have had assessment of the primary end point. For the main outcome variable and analysis a P-value of 0.047 will be used. For the planned interim analysis after half the data collection, a P-value of 0.00305 will be used with a group sequential alpha spending function calculated by the method of O’Brien and Fleming HOT OR NOT clinical trial protocol: v2,21/02/2012 17 HOT or NOT using two sided symmetric bounds.37 This will preserve an overall P-value for the study of 0.05. Additional reviews of the data may be performed at the discretion of the Data Monitoring Committee and will require recalculation of the interim P-values. The Data Monitoring Committee will also review summaries of all SAEs that occur during the study. 15 DIRECT ACCESS TO DATA & DOCUMENTS The study may be audited by government regulatory authorities, representatives of the management committee, or, the Medical Research Institute of New Zealand. Therefore access to medical records, other source documents such as ICU charts and other study related files must be made available at all study sites for monitoring and audit purposes during the course of the study and after its completion. Participants will not be identified by name, and confidentiality of information in medical records will be preserved. The confidentiality of the participant will be maintained unless disclosure is required by regulations. 16 QUALITY CONTROL AND QUALITY ASSURANCE MONITORING 16.1 Responsibilities of the principal investigator at each site The principal investigator (PI) is required to ensure compliance with all procedures required by the clinical trial protocol and with all study procedures provided by the cocoordinating centre. The PI agrees to provide reliable data and all information requested by the clinical trial protocol in an accurate and legible manner according to the instructions provided. The investigator agrees to allow representatives of the co-coordinating centre to have direct access to source documents. 16.2 Responsibilities of the co-coordinating centre The co-coordinating centre is responsible for taking all reasonable steps to ensure the proper conduct of the clinical trial protocol. Prior to initiation of the study at each participating site, the co-ordinating centre will be responsible for providing adequate training to the PI and study personnel. The training will cover all aspects of the study protocol and procedures and will include practical training in completing the eCRF and the study materials. All study materials will be provided at or before the training sessions. During the trial, the sites will be contacted, through monitoring visits, letters or telephone calls, by the study monitor to review study progress, investigator and patient compliance with study protocol requirements and any emergent problems. The main duty of the study monitor is to help the investigator and the coordinating centre maintain a high level of ethical, scientific, technical and regulatory quality in all aspects of the trial. HOT OR NOT clinical trial protocol: v2,21/02/2012 18 HOT or NOT Site monitoring visits will be performed periodically and in accordance with the Monitoring Plan. The investigator and study personnel will assist the study monitor by providing all appropriate documentation, and being available to discuss the study. These monitoring visits will include but not be limited to review of the following aspects: Adherence to the protocol including consistency with inclusion and exclusion criteria; The completeness and accuracy of the eCRFs and source documentation, patient informed consent; Patient recruitment and follow-up; AE and SAE documentation and reporting; Study treatment allocation; Patient compliance with the study treatment regimen; Study treatment accountability; Compliance with regulations. At completion of the trial, a final monitoring and close out visit will be conducted by the study monitor in accordance with the Monitoring Plan. Secure facilities for the storage of study data for 15 years will also be re-checked at this visit. 16.3 Source document requirements The monitoring team will check the eCRF entries against the source documents. The purpose of source documents is to document the existence of the participant and substantiate the integrity of the study data collected. Source documents include the original documents related to the trial, to medical treatment, and to the history of the subject. Adequate and accurate source documents allow the investigator and the site monitor to verify the reliability and authenticity of data recorded on the eCRFs and ultimately to validate that the clinical study was carried out in accordance with the protocol. 16.4 Management of protocol deviations A protocol deviation is an unanticipated or unintentional departure from the expected conduct of an approved study that is not consistent with the current research protocol or consent document. A protocol deviation may be an omission, addition or change in any procedure described in the protocol. The investigator should not implement any deviation from or changes of the protocol without agreement by the study management committee and documented approval from the Independent Ethics Committee of the amendment, except where necessary to eliminate an immediate hazard(s) to trial participants. In the event of an emergency intended to eliminate an apparent immediate hazard to participants the Investigator may implement any medical procedure deemed appropriate. Deviations from the protocol must be documented and promptly reported to the study management committee. The report should summarise the event and action taken. 17 ETHICAL CONSIDERATIONS 17.1 Ethical Principles This trial will be conducted in accordance with the principles laid down by Health Research Council of New Zealand and other Local Ethics Committees. HOT OR NOT clinical trial protocol: v2,21/02/2012 19 HOT or NOT 17.2 Independent Ethics Committee The CI is responsible for submitting this protocol to the Independent Ethics Committee. An application for Ethics Approval will be lodged with the Multi-region Ethics Committee of the Health Research Council of New Zealand. The content and format of the patient and next-of-kin information statements and consent forms will be approved by the Ethics Committee(s) and produced in line with their own guidelines and requirements. During the trial, any amendment or modification to the study protocol will be notified to the Ethics Committee by the CI and approved by the Ethics Committee before implementation, unless the change is necessary to eliminate an immediate hazard to the patients, in which case the Ethics Committee should be informed as soon as possible. The CI will be responsible for informing the Ethics Committee of any event likely to affect the safety of patients or the continued conduct of the clinical trial, in particular any change in safety. The CI will produce progress reports, adverse event reports, and any other documentation required by the Multi-region Ethics Committee in accordance with their guidelines. The CI will keep an up to date record of all correspondence with the Ethics Committee. A clean copy of the consent forms and information statements that are to be used at each hospital, together with a copy of all signed consent forms and any other consent related correspondence must also be kept in a separate file for this study, in case of any future requirement for audit purposes. 17.3 Informed Consent The Health Research Council Statement on Research Involving Unconscious Participants acknowledges that research involving patients who are heavily dependent on medical care, such as the patients in this study, is necessary to assess and improve the efficacy and safety of interventions used in their treatment. Obtaining written and informed consent from patients who are highly dependent on medical care, such as patients in ICU is difficult because Intensive Care patients are often unconscious, sedated, intubated and too ill to understand information relating to clinical trial participation. It is anticipated that all patients in this trial will be critically unwell and unable to give consent at the time that they are enrolled into the trial. Patients who are eligible for this trial will be in an emergency situation where decisions about their treatment will have to be made too quickly to consult with families and/or legal representatives. As a consequence, we plan that the paramedics will randomise patients into the clinical trial with a plan to obtain ‘delayed consent’. Patients, their families and/or legal representatives will be provided with pertinent information when, and if, it becomes possible and appropriate to do so after the patient arrives in hospital. Irrespective of the consent of surrogates, the patients themselves will be given the opportunity to provide informed consent as soon as it is possible for them to do so. HOT OR NOT clinical trial protocol: v2,21/02/2012 20 HOT or NOT 18 DATA HANDLING AND RECORD KEEPING Folders will be provided for the research co-ordinator to file any paper documents used for any form of data collection for each patient and to store the signed and dated consent forms. A comprehensive guide to the data collection with definitions and rationale will be provided together with a paper version of the data collection forms. Paper documents will be stored in secure locked cabinets with access limited to authorized persons. All of the documents will be available in PDF format for printing. The aim is to assist the research co-ordinator to ensure high-quality data collection and data entry. Data management will be provided by the co-ordinating centre. The principle means of data collection and data processing will be via online data entry performed by research co-ordinators at each site. All forms will be signed and dated by the authorised study staff and all changes made following data submission will be recorded. When archiving or processing data pertaining to the investigator and/or to the patients, the co-ordinating centre shall take all appropriate measures to safeguard and prevent access to this data by any unauthorized third party. The PI must maintain confidential all study documentation, and take measures to prevent accidental or premature destruction of these documents. It is recommended that the Investigator retain the study documents at least fifteen years after the completion or discontinuation of the study. The PI must notify the Study Management Committee prior to destroying any study essential documents following the study completion or discontinuation. If the PI's personal situation is such that archiving can no longer be ensured by him/her, the PI shall inform the Study Management Committee and the relevant records shall be transferred to a mutually agreed upon designee. If any PI retires, relocates, or otherwise withdraws from conducting the study, the responsibility for maintaining records may be transferred to the another designated PI at the study centre. All associated documentation must also be updated. 19 FINANCING AND INSURANCE 19.1 Funding Funding is being sought from the Health Research Council of New Zealand. 19.2 Participating Centres agreement Participating centre agreements will be signed between the participating sites and the Medical Research Institute of New Zealand and cover: Trial work and duration Obligations of the CI Confidentiality Intellectual property Indemnity The Co-ordinating Centre will complete Form A ‘Declaration of Eligibility of a Clinical Trial for Consideration of Coverage under Accident Compensation Legislation’ and anticipate that participants in the clinical trial will be insured under accident compensation legislation for injury caused as a result of their participation in the HOT OR NOT clinical trial protocol: v2,21/02/2012 21 HOT or NOT research. Indemnity for clinical trial staff will be provided by individual participating hospitals. 20 PUBLICATION POLICY The study will be conducted in the name of the HOT OR NOT investigators. The central project coordination and data management will be by the CI at the Medical Research Institute of New Zealand. The principal publication from the study will be in the name of the HOT OR NOT Investigators with full credit assigned to all collaborating investigators, research coordinators and institutions. Where an individuals’ name is required for publication it will be that of the writing committee, with the chair of the writing committee listed first and subsequent authors listed alphabetically. 21 PROJECT TIMELINE To be confirmed. HOT OR NOT clinical trial protocol: v2,21/02/2012 22 HOT or NOT 23 REFERENCES 1. Cardiovascular Disease in New Zealand. A Summary of Recent Statistical Information 2004. (Accessed at http://www.maorihealth.govt.nz/moh.nsf/indexma/cardiovascular-disease cardiovascular ) 2. Robinson S, Swain AH, Hoyle SR, Larsen PD. Survival from out-of-hospital cardiac arrest in New Zealand following the 2005 resuscitation guideline changes. Resuscitation 2010;81:1648-51. 3. Swain A BT, Hoyle S, Haywood G, Cameron H, Larsen P. Outcomes from out-of-hospital cardiac arrest in the Wellington Region: does the use of the fire service make a difference. . New Zealand Medical Journal 2011;124. 4. Robson B HRe. Hauora: Māori Standards of Health IV. A study of the years 2000-2005. . Wellington: Te Rōpū Rangahau Hauora a Eru Pōmare. . 5. Pilcher J, Weatherall, M, Shirtcliffe P, Beasley R, Bellomo R, Young P. The Impact of Hyperoxia Following Cardiac Arrest - A Systematic Review and Meta Analysis of Preclinical Trials (manuscript submitted). 6. Richards EM, Fiskum G, Rosenthal RE, Hopkins I, McKenna MC. Hyperoxic reperfusion after global ischemia decreases hippocampal energy metabolism. Stroke; a journal of cerebral circulation 2007;38:1578-84. 7. Richards EM, Rosenthal RE, Kristian T, Fiskum G. Postischemic hyperoxia reduces hippocampal pyruvate dehydrogenase activity. Free radical biology & medicine 2006;40:1960-70. 8. Liu Y, Rosenthal RE, Haywood Y, Miljkovic-Lolic M, Vanderhoek JY, Fiskum G. Normoxic ventilation after cardiac arrest reduces oxidation of brain lipids and improves neurological outcome. Stroke; a journal of cerebral circulation 1998;29:1679-86. 9. Vereczki V, Martin E, Rosenthal RE, Hof PR, Hoffman GE, Fiskum G. Normoxic resuscitation after cardiac arrest protects against hippocampal oxidative stress, metabolic dysfunction, and neuronal death. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism 2006;26:821-35. 10. Zwemer CF, Whitesall SE, D'Alecy LG. Cardiopulmonary-cerebral resuscitation with 100% oxygen exacerbates neurological dysfunction following nine minutes of normothermic cardiac arrest in dogs. Resuscitation 1994;27:159-70. 11. Brucken A, Kaab AB, Kottmann K, et al. Reducing the duration of 100% oxygen ventilation in the early reperfusion period after cardiopulmonary resuscitation decreases striatal brain damage. Resuscitation 2010;81:1698-703. 12. Balan IS, Fiskum G, Hazelton J, Cotto-Cumba C, Rosenthal RE. Oximetryguided reoxygenation improves neurological outcome after experimental cardiac arrest. Stroke; a journal of cerebral circulation 2006;37:3008-13. 13. Marsala J, Marsala M, Vanicky I, Galik J, Orendacova J. Post cardiac arrest hyperoxic resuscitation enhances neuronal vulnerability of the respiratory rhythm generator and some brainstem and spinal cord neuronal pools in the dog. Neuroscience letters 1992;146:121-4. 14. Yeh ST, Cawley RJ, Aune SE, Angelos MG. Oxygen requirement during cardiopulmonary resuscitation (CPR) to effect return of spontaneous circulation. Resuscitation 2009;80:951-5. 15. Lipinski CA, Hicks SD, Callaway CW. Normoxic ventilation during resuscitation and outcome from asphyxial cardiac arrest in rats. Resuscitation 1999;42:221-9. 16. Bircher N, Safar P. Cerebral preservation during cardiopulmonary resuscitation. Critical care medicine 1985;13:185-90. HOT OR NOT clinical trial protocol: v2,21/02/2012 23 HOT or NOT 17. Saugstad OD. Resuscitation of newborn infants: from oxygen to room air. Lancet 2010;376:1970-1. 18. Hellstrom-Westas L, Forsblad K, Sjors G, et al. Earlier Apgar score increase in severely depressed term infants cared for in Swedish level III units with 40% oxygen versus 100% oxygen resuscitation strategies: a population-based register study. Pediatrics 2006;118:e1798-804. 19. Kilgannon JH, Jones AE, Shapiro NI, et al. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA : the journal of the American Medical Association 2010;303:2165-71. 20. Kilgannon JH, Jones AE, Parrillo JE, et al. Relationship between supranormal oxygen tension and outcome after resuscitation from cardiac arrest. Circulation 2011;123:2717-22. 21. Bellomo R, Bailey M, Eastwood GM, et al. Arterial hyperoxia and in-hospital mortality after resuscitation from cardiac arrest. Crit Care 2011;15:R90. 22. Kuisma M, Boyd J, Voipio V, Alaspaa A, Roine RO, Rosenberg P. Comparison of 30 and the 100% inspired oxygen concentrations during early postresuscitation period: a randomised controlled pilot study. Resuscitation 2006;69:199206. 23. Steffen IG, Hasper D, Ploner CJ, et al. Mild therapeutic hypothermia alters neuron specific enolase as an outcome predictor after resuscitation: 97 prospective hypothermia patients compared to 133 historical non-hypothermia patients. Crit Care 2010;14:R69. 24. Cronberg T, Rundgren M, Westhall E, et al. Neuron-specific enolase correlates with other prognostic markers after cardiac arrest. Neurology 2011;77:62330. 25. Shinozaki K, Oda S, Sadahiro T, et al. S-100B and neuron-specific enolase as predictors of neurological outcome in patients after cardiac arrest and return of spontaneous circulation: a systematic review. Crit Care 2009;13:R121. 26. Tiainen M, Roine RO, Pettila V, Takkunen O. Serum neuron-specific enolase and S-100B protein in cardiac arrest patients treated with hypothermia. Stroke; a journal of cerebral circulation 2003;34:2881-6. 27. Ekmektzoglou KA, Xanthos T, Papadimitriou L. Biochemical markers (NSE, S-100, IL-8) as predictors of neurological outcome in patients after cardiac arrest and return of spontaneous circulation. Resuscitation 2007;75:219-28. 28. Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. The New England journal of medicine 2004;350:2247-56. 29. Finfer S, Chittock DR, Su SY, et al. Intensive versus conventional glucose control in critically ill patients. The New England journal of medicine 2009;360:128397. 30. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. The New England journal of medicine 2002;346:549-56. 31. Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. The New England journal of medicine 2002;346:557-63. 32. Prohl J, Rother J, Kluge S, et al. Prediction of short-term and long-term outcomes after cardiac arrest: a prospective multivariate approach combining biochemical, clinical, electrophysiological, and neuropsychological investigations. Critical care medicine 2007;35:1230-7. 33. Bernard SA, Smith K, Cameron P, et al. Induction of therapeutic hypothermia by paramedics after resuscitation from out-of-hospital ventricular fibrillation cardiac arrest: a randomized controlled trial. Circulation 2010;122:737-42. HOT OR NOT clinical trial protocol: v2,21/02/2012 24 HOT or NOT 34. Rostrup E, Law I, Blinkenberg M, et al. Regional differences in the CBF and BOLD responses to hypercapnia: a combined PET and fMRI study. NeuroImage 2000;11:87-97. 35. Pilcher J, Weatherall, M, Shirtcliffe P, Beasley R, Bellomo R, Young P. A multi-centred retrospective trial investigating the association between arterial oxygen levels and outcome in patients resuscitated from out-of-hospital cardiac arrest (manuscript in preparation). 36. Altman DG, Schulz KF, Moher D, et al. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Annals of internal medicine 2001;134:663-94. 37. Emerson SS, Fleming TR. Symmetric group sequential test designs. Biometrics 1989;45:905-23. HOT OR NOT clinical trial protocol: v2,21/02/2012 25