Chapter 21
advertisement

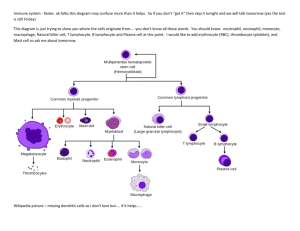
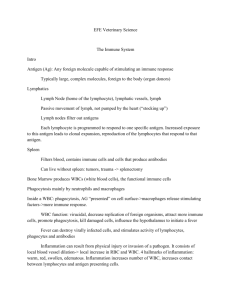
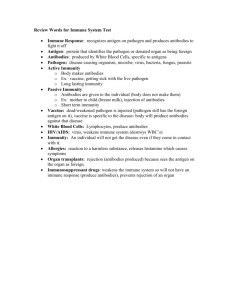
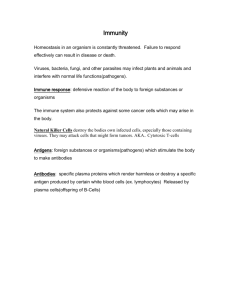
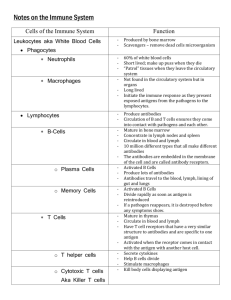
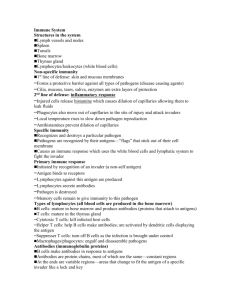
BIOLOGY 206 I. II. CHAPTER 21: NONSPECIFIC BODY DEFENSESS & IMMUNITY: LAUREL, SPRING 2007 2 types of defense systems A. Nonspecific defense system 1. Response is the same each time the body is exposed to a substance. 2. No memory. 3. Categorized as innate immunity. B. Specific or adaptive defense system: the immune system 1. Second response to the same substance is faster and stronger. 2. May be so fast that no symptoms develop. 3. Has memory 4. Categorized as adaptive immunity (the immune system). 5. Immunity is highly specific resistance to disease. Nonspecific Body Defenses A. Surface membrane barriers (skin and mucosa) 1. First line of defense against pathogens (organisms that cause disease). 2. Both form physical barriers to entry of microorganisms. 3. Epithelial membranes produce numerous protective chemicals: a. Acids which inhibits bacteria are found on skin in stomach and vagina. b. Digestive enzymes such as lysozyme in tears and saliva. c. Cilia and mucous traps bacteria that are swallowed or expelled by coughing or sneezing. B. Phagocytosis 1. One of most important nonspecific defenses. 2. Macrophages derived from monocytes are the chief phgocytes of the body. 3. Neutrophils are also extremely important phagocytes. 4. Eosinophils are more weakly phagocytic but important against parasites. C. Natural Killer Cells (NK) 1. Cells that lyse and kill cancer cells and virus-infected body cells before the immune system is activated. 2. They are a type of large granular lymphocytes. 3. Other lymphocytes are specific, but NK cells are non-specific. 4. First lyse plasma membrane and then nuclear membrane, plus enchance inflammatory response. D. Inflammation response 1. Second line of defense and is triggered whenever body tissues are injured. 2. Involves interaction of cells, chemicals and tissue fluid to: a. Prevent spread of damaging agents. b. Dispose of cell debris and pathogens. 1 III. c. Set stage for tissue repair. 3. Indicated by redness, heat, swelling, and pain. 4. See flow chart 5. Pus is a mix of dead or dying WBCs, broken-down tissue cells and living and dead pathogens. Forms in severely infected areas. E. 2 important antimicrobial proteins 1. Complement: complex of plasma proteins that circulate in the blood in an inactive state. 2. Compliment is activated by: a. Interacting with an antigen-antibody complex or b. Interacting with chemicals on cell walls of pathogens. 3. Once activated compliment works by : (OIL) a. Lysing pathogens . b. Intensifying all aspects of the inflammation response via chemotaxis, increased permeability etc. and c. Opsonization.This is a process that provides “handles” on the pathogen so phagocytes can more easily grab them. 4. Note: Complement functions both as nonspecific and specific defense mechanism. 5. Interferons are the second important antimicrobial protein a. IFNs are proteins secreted by cells infected with a virus that then stimulate other cell membranes to produce proteins that prevent viruses from reproducing in these uninfected cells . b. IFNs are not virus-specific. c. IFNs also activate macrophages and mobilize NK cells. F. Fever 1. Macrophages and other leukocytes that are exposed to bacteria and other foreign material release pyrogens. These are chemicals that cause the hypothalamus to reset its thermostat. 2. Liver and spleen store and hide iron in response to pyrogens. These nutrients are needed by bacteria to reproduce. 3. Fever also increases metabolic rate which speeds up defense and repair. Specific Body defenses (Third line of defense) A. Overview 1. Immune system is a functional system rather than an organ-system with trillions of lymphocytes that circulate throughout the body. 2. Immune response: Antigen-specific defenses mounted by activated lymphocytes (T and B cells). It: a. is antigen-specific b. is systemic, not limited to site of infection c. has memory 3. Foreign Antigen: a substance that is recognized as foreign by the immune system, activates the immune system, and reacts with immune cells or its products. 2 4. ***** ***** IV. V. Antibody is a protein molecule released by a plasma cell (daughter cell of an activated B lymphocyte) in response to a specific antigen that binds specifically to an antigen. 5. Humoral immunity is immunity conferred by antibodies present in blood plasma and other body fluids. a. Antibodies bind primarily to bacteria, bacterial toxins and to free viruses. b. Antibodies inactivate pathogens and mark them for destruction by phagocytes or complement. 6. Cell-mediated immunity occurs when lymphocytes themselves (activated T cells) defend the body. a. These lymphocytes directly lyse infected or cancerous body cells or cells of foreign grafts, or b. Indirectly by the release of chemicals that enhance inflammation or activate other lymphocytes and macrophages. *** Attack invading cell directly. Cells of the Immune System: an Overview A. 3 critical cell types of the immune system 1. B lymphocytes or B cells 2. T lymphocytes or T cells 3. Antigen presenting cells or APCs B. Lymphocytes 1. Originate in red bone marrow. 2. B cells probably remain in red bone marrow for their maturation, then move to blood and lymphoid tissues. 3. T-cells migrate to thymus gland for maturation then move out to blood and lymphoid tissues. 4. Immunocompetence (maturity) for both T and B cells occurs with the development of a single unique cell-surface receptor protein (receptor). a. Each cell can bind to 1 and only 1 kind of antigen. b. Acquired before it meets a foreign antigen. c. Body has millions of immunocompetent cells which will never meet its antigen, and never be involved in immune response. C. Antigen-Presenting Cells (APC) 1. Ingest cell or antigen and then present foreign antigens on their surfaces for recognition by immunocompetent lymphocytes. 2. Secrete proteins to activate T cells which in turn release chemicals that mobilize macrophages into super killer phagocytes. 3. We’ll consider the macrophage as our example of an APC. Antibody-mediated immunity (humoral) Ex. of bacteria. invasion. A. Antigen challenge, clonal selection and differentiation of B cells. 3 1. B. C. Antigen challenge, the first encounter between an immunocompetent B cell and its antigen, usually occurs in spleen or lymph node (where B cells are). a. Antigen binds to receptor on B cell. 2. This activates the B cell and it divides rapidly to produce a family of identical cells, clones (all with same antigen-receptors on surface.). 3. Most cells are plasma cells which produce huge quantities of antibodies (2,000/sec!) for 4-5 days. a. This is the is primary response. 4. Other cells of the clone become long-lived memory B cells capable of mounting an immediate humoral response if the same antigen is encountered again. a. Responses generated by membory cells are called secondary responses. Immunological memory 1. Primary response: stimulated by first exposure to a foreign antigen. Characterized by : a. lag period of 3-6 days before antibodies are produced (process of activation and clone formation). b. Logarithmic (log) phase where number of antibodies increases for several days. Peaks around 10 days. c. Decline phase: concentration decreases to low level. 2. Secondary response:stimulated by subsequent exposure to the same foreign antigen. a. Because of memory cells, response is very fast (short latent period and peaks in 2 days), more antibodies are produced, and decline is slower. b. High levels can be maintained for weeks or months. 3. Memory cells retain memory for a lifetime. Active vs passive humoral immunity 1. Active humoral immunity: immunity acquired when body is exposed to a foreign antigen and it produces its own antibodies and own memory cells. a. Natural immunity: occurs through natural exposure to the antigen. b. Artificially acquired immunity: when we receive vaccines. This involves exposure to an antigen that has been killed or weakened (attenuated) . Examples: chicken pox, polio, diptheria, tetanus 2. Passive humoral immunity: antibodies are received from a donor, and memory is NOT established. a. Transfusion of gamma globulin after exposure to rabies or snake bites. 4 VII. b. Occurs naturally from mother to fetus. D. Antibody targets and functions 1. Antibodies do not destroy antigen-bearing substances directly, but they inactivate them or mark them for destruction. 2. All interactions involve the formation of an antigen-antibody complex (lock/key). One of several possible actions follows that eventually leads to phagocytosis, inflammation or cell lysis: 3. Complement fixation: a. When antigen binds to antibody the shape of antibody changes and its complement-binding sites become exposed such that first chemical in complement cascade binds to this site. b. This triggers complement fixation (cascade reaction to activate complement). c. Activated Complement lyses foreign cell etc. See page 2. 4. Neutralization: a. Antibodies block specific sites on viruses or bacterial exotoxins such that they cannot bind to receptor sites on tissue cells to cause injury. b. Antigen-antibody complexes are eventually destroyed by phagocytes. 5. Agglutination and precipitation: a. Antibodies have more than 1 antigen-binding site so can bind to more than 1 antigen. b. A-A complexes can form lattices (interlocking networks). c. If cell-bound antigens = agglutination; d. If soluble molecules = precipitation e. Both makes them more susceptible to phagocytosis. Cell-mediated immunity A. Overview 1. Recall antibodies are only effective against extracellular antigens 2. Cell-mediated immunity primarily defends against virus-infected cells, grafts and cancer cells 3. T cells function in cell-mediated immunity 4. 2 primary populations of T cells are CD4 or T helper cells and CD8 or Cytotoxic T cells B. 2 types of MHC proteins important to T cell activation 1 Class I MHC proteins 2. Class II MHC proteins C. Class 1 MHC proteins 1. are found on all body cells except RBCs which lack nuclei 2. Class 1 MHC proteins protrude from the cell’s plasma membrane 3. Attached to Class 1 MHC proteins are fragments of cells being made within the cell (either normal or abnormal 5 If normal cellular proteins are being synthesized they’ll be displayed and serve as a sign that says: “I BELONG! DON’T KILL ME” 5. If viral or cancer cell proteins are being synthesized, they’ll be displayed and serve as a sign that says: “HEY! LOOK AT ME! I’VE BEEN INFECTED, COME AND KILL ME! Class II MHC proteins 1. Found primarily on antigen-presenting cells; i.e., phagocytes. They display fragments of foreign antigens that have been pahgocytosed and chopped up within the cell 2. These foreing chopped up proteins are displayed on the Class II MHC protein a. These phagocytes also have Class 1 MHC proteins 3. The displayed antigen and MHC II complex serves as a sign that says: “ EXCUSE ME! I JUST SAW THIS PATHOGEN AND ATE HIM. HE’S IN THE ECF! THIS IS WHAT HE LOOKS LIKE. GO FIND HIM AND KILL HIM!!! T cell Activation 1. Activation is a 2-step process: a. antigen binding b. Costimulation 2. Cytotoxic T cells (CD8) bind to antigens complexed with MHC proteins 3. Helper T cells bind to antigens complexed with MHC proteins 4. Once a T cell has bound to the combination of its specific antigen and the appropriate MHC protein, co-stimulation must occur. a. Think of co-stimulation as a double check that the bound cell is really one that is infected or alien. b. One way this works is that the T cell looks for a second virus protein on the cell membrane c. In response to this double binding, the T cell will be activated and perform functions based on its T cell class. Cytotoxic T cell Functions 1. Activated Cytotoxic T cells will undergo clonal selection and form mature cytoxic T cells and memory cells 2. Mature Cytotoxic T cells will set about to kill those body cells displaying the specific antigen by secreting lethal chemicals. One of these is perforin which pokes holes in the infected cell Helper T cell Functions 1. Activated helper T cells undergo clonal selections and form mature helper T cells and memory helper T cells 2. Mature helper T cells “direct” the immune response by releasing chemical signals known as cytokines 3. Cytokines: 4. D. E. F. G. 6 a. H. Stimulate the production, mobilization and activation of all phagocytes b. Assist B cells in undergoing clonal selection c. Stimulate inflammation d. Activate Natural Killer Cells Supressor T cells 1. Supressor T cells are also stimulated by antigens which depress B and T cells. However, they reproduce more slowly that cytotoxic T cells, so they don’t begin to depress the immune response until at least 1 week after it is well underway. a. Vital to wind down the immune response after the antigen has been destroyed. Antibody-mediated Immunity Cell-mediated Immunity 1. Attack bacteria, bacterial toxins and free 1. Attack foreign antigens on surface of viruses our own body cells, cancer and grafts 2. B cells activated to become plasma cells 2. Produces activated Tc 3. Produces antibodies that go to the site of 3. Tc go site of infection the infection. 4. Antibodies neutralize, agglutinate, 4. Tc produce perforans which lyse target precipitate and/or activate complement for cells directly. lysis, phagocytosis and enhanced inflammatiion. 5. Both have direct and costimulation, require T helper cells 6. Both undergo the antigen challenge, clonal selection and the production of memory cells. 7