Diagnostic Laboratory Tests
advertisement

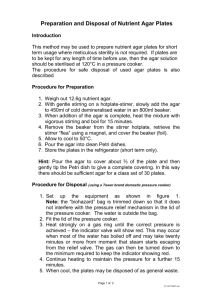
Diagnostic Laboratory Tests Students should be familiar with the following diagnostic laboratory tests, media, and procedures that were discussed in lecture and/or demonstrated in the laboratory and how they are used in the identification of bacteria. Consult the Laboratory Manual and textbook for further information Gram stain – includes heat fixation, crystal violet, iodine, decolorizer, and safranin. Gram + stain purple, contain thick peptidoglycan layer, Gram – stain red, contain thin peptidoglycan layer and outer membrane. Kinyoun acidfast stain – stained with carbolfuchsin, decolorized with acid-alcohol solution, counterstained; positive acid-fast stain reacton corresponds to higher infectivity, confirms mycobacterial infection. Auramine-Rhodamine Stain - also known as the Truant fluorochrom stain, used to visualizee acid-fast bacilli using fluorescence microscopy, notably species in the Mycobacterium genus. Acid-fast organisms display a reddish-yellow fluorescence. AR stain is a mixture of Auramine O and Rhodamine B. Alpha, beta, gamma hemolysis – alpha: colony surrounded by zone of intact, but discolored erythrocytes that have a green or brownish-green color; beta: colonies surrounded by clear zone in which few or no intact erythrocytes are visible; gamma: colonies produce no change in blood surrounding the colony. Catalase test – place drop of 3% H2O2 on slide containing colony, oxygen bubbles indicate a positive test. Coagulase test – coagulase clots plasma; use kit with latex particles coated with fribrinogen to detect bound coagulase (“clumping factor”) and IgG which detects protein A, which binds the Fc region. Positive = white clumps. Also can be performed by adding organisms to rabbit plasma. Optochin test – ethylhydrocupreine hydrochloride; pure culture of organism form lawn on blood agar, filter disk paper placed on plate, incubated overnight in a CO2 incubator. Zone of inhibition >/= 14mm indicates susceptibility. Alpha and non-hemolytic streptococci are not susceptible. Bacitracin test – antibiotic that impairs cell wall synthesis in some gram + bacteria, any degree of inhibitory zone surrounding a filter paper disk indicates susceptibility. Novobiocin test – a narrow spectrum toxic antimicrobial agent that inhibits bacterial DNA gyrase, zone of inhibition of </= 12mm around disk on sheep blood agar indicates resistance. Nitrocefin (Cefinase) test – Beta lactamase production detection, disks contain chromogenic cephalosporin, nitrocefin, place drop of water on disk on slide, smear colony on disk, beta lactamase producing strains hydrolyze nitrocefin changing it from yellow to red as amide bond in beta-lactam ring is hydrolyzed. Oxidase test – used to aid in identification of gram – rods and Neisseria. Neisseria are oxidase positive, all members of Enterobacteriacae are oxidase negative. Other gram – rods, such as Pseudomonas aeruginosa, camplybacter and vibrio are oxidase +. The oxidase reagent, 1% tetramethyl-p-phenylenediamine dihydrochloride, detects cytochrome oxidase enzyme system. Drop of reagent on swab, use swab to collect colonies from blood or chocolate agar plate; positive = dark purple color within a few seconds. PYR test – based on hydrolysis of pyrrolidonyl-α-napthylamide by organisms that contain enzyme pyrrolidonyl arylamidase. Identifies group A strep from Enterococcus, which are PYR-positive. PYR substrate on disk on slide, scrape unknown organism onto disk, incubate at room temp 1 min; red color = positive. Indole test – tryptophanase catalyzes the reaction to metabolize the amino acid trypophan to produce indole, pyruvic acid and ammonia; this test identifies oxidase negative, lactose fermenting gram – rod (like E.coli). Add drop or two of indole reagent to swab, collect colonies from blood agar plate on swab, observe for blue color within seconds. Bile esculin test – growth in presence of bile and hydrolysis of esculin to produce a black color in nutrient agar; distinguishes Enterococcus from streptococci, except groupD and O organisms; use 6.5% NaCl to distinguish enterococci from group D. 6.5% NaCl test – separates enterococci from streptococci, especially bile-esculine positive S. bovis, S. equines. Todd-hewitt broth (used to grow strep) with NaCl added to final conc of 6.5%; bile-esculin + gram +, catalase – cocci that grow are enterococci, bile esculin + gram + catalase – cocci that do not grow are in bovis-equinus group. CAMP test – distinguishes group A streptococci from group B, which secrete CAMP factor that enhances the hemolytic action of beta lysin on blood agar. Unknown organism streaked perpendicular to S. aureus, “arrow head” of hemolysis indicates group B strep. Motility test – semisolid agar inoculated by “stabbing”, motile organisms will spread out form the point of inoculation; Listeria monocytogenes forms “umbrella” pattern, nonmotile orgs grow only at the site of inoculation. Sheep blood agar – nutrient agar + 5% sheep blood, supports the growth of most pathogens; almost always used when initially plating out bacteriologic specimen. MacConkey agar – contains lactose, peptone; bile salts and crystal violet to inhibit Gram + bacteria. Indicator dye, neutral red is taken up by colonies fermenting lactose (usually non-pathogenic), non-colored colonies are formed by important stool pathogens such as Salmonella and Shigella. Also used to control swarming of Proteus sp. Xylose-lysine-desoxycholate agar – contains sucrose, lactose and xylose as carb sources, lysine added to detect lysine decarboxylase rxn, bile salts (desoxycholate) selectively inhibits gram + but not coliforms. Sodium thiosulfate and ferric ammonium citrate added to permit detection of hydrogen sulfide gas production. Phenol red is pH indicator. Salmonella colonies appear red due to elevation of pH (lys decarboxylation) and contain black centers (hydrogen sulfide production in presence of ferric ammonium citrate). Shigella appear colorless or red, E. coli and Enterobacter appear yellow due to carb utilization. Chocolate agar – blood agar heated to 80 degrees C for 15 min until color chocolate brown; lyses RBC releasing hemoglobin and growth factors needed by fastidious bacteria, heat also coagulates proteins, helping absorb fatty acids and amino acids that inhibit some bacteria. N. gonorrhoeae, H. influenzae cultivable on chocolate but not ordinary blood agar. Mannitol salt agar – pink agar, yellow zone indicates acid production. Mueller-Hinton agar – contains starch and casamino acids, fastigioius pathogen Neisseria grow well on it, starch binds traces of free fatty acid that would otherwise inhibit growth; also widely used for antibiotic and sulfonamide sensitivity tests of staph, enteric gram – rods, and strep when supplemented with 5% blood. Thayer Martin agar – selective for meningococci and gonococci; nutrient rich agar supplemented with hemoglobin, vitamins and other known growth factors for Neisseria, contains antibiotic vancomysin, colistin and nystatin, which inhibit practically all normal flora Sabouraud dextrose agar – used for isolation, identification and maintenance of pathogenic and non-pathogenic fungi. Contains dextrose, a nitrogen source, agar and acid pH of 5.6, which inhibits many bacteria present in mycological specimens. Various inhibitory agens may be incorporated to restrict growth of other fungi/bacteria. Lowenstein-Jensen agar – used to culture Mycobacterium Selective media – basic or enriched medium to which antibiotics, growth inhibitory dyes or other chemicals such as bile salts have been added to select for growth of organisms that are resistant to these factors. MacConkey agar contains crystal violet that inhibits gram positive bacteria and selects for gram negative. Differential media – can be nutritive or enriched and additional substrates such as carbohydrates have been added to detect specific metabolic characteristics of organisms that set them apart from similar organisms. Mannitol salt agar allows differentiation of staphylococci that can ferment mannitol and those that cannot because there is a pH indicator incorporated that shows color change when the sugar is converted to acid. Mannitol salt agar also has a high NaCl content, which discourages growth of organisms found on skin. Enriched media – general medium to which additional growth supplements have been added, such as blood or serum products, eggs, and/or vitamins and minerals essential for fastidious organisms; e.g. sheep blood agar Nutritive media – basic medium with simple nutrients such as protein extracts (peptone, tryptone) derived enzymatically from meat, milk or soybean; supports growth of nonfastidious organisms; e.g. trypiticase soy agar (TSA), nutrient agar, brain heart infusion agar, Mueller-Hinton agar Oxidation reaction – obligate aerobes and facultative anaerobes generate energy by oxidation. Reaction is performed in a test tube containing semisolid glucose medium with a pH indicator. Each strain is placed in 2 tubes with one overlaid with mineral oil to create an anaerobic environment. Fermentative organisms will utilize carbohydrates and produce acid in both aerobic and anaerobic environments; oxidative organisms will only use carbohydrates in the aerobic environment. Asaccharolytic organisms do not use carbs for energy and will not grow in either tube. Fermentation reaction – fermentation is anaerobic and is done by obligate and facultative anaerobes. See above. Discussion on p. 34 of lab manual API Biochemical strip – identify gram-negative bacteria based on the differential abilities of species to utilize carbohydrates or to react with certain enzymatic substrates. Agar disk diffusion test – test antibiotic susceptibility; procedure: apply paper antibiotic discs of variable known concentration to colonized plate and measure zone of inhibition (include disc diameter); zone diameter is inversely proportional to the activity of the drug against the bacterium; this method does NOT measure MIC (minimum inhibitory concentration) Agar gradient diffusion test – set up is the same as for agar disk diffusion except that instead of a filter paper disk with antimicrobial, a plastic strip called the E-test is used. The E-test has the antimicrobial incorporated in a continuous gradient. Determine MIC by looking at the intersection of the zone of growth inhibition with the numerical reading on the E-test strip. Agar dilution test – antibiotic concentrations are diluted in agar plates that are then inoculated with bacteria; determines MIC Microbroth dilution test – antibiotics are diluted in broth, usually in well of a microtiter plate, bacteria are added and determine the lowest concentration of antibiotic needed to prevent bacterial growth; determines MIC Minimum inhibitory concentration – lowest concentration of antimicrobial agent that inhibits growth of a bacterium Satellitism – Haemophilus needs NAD (V factor) to grow, so if S. aureus is plated on blood agar and releases NAD from hemolysis, the Haemophilus will grow around it. Method can also be done with strips containing X and V factor and seeing which Haemophilus species will grow around them X and V Factor test – Haemophilus species can be determined by their requirements for exogenous hemin (X factor) and/or NAD (V factor), both of which are in chocolate agar. H. influenzae will grow on blood agar by cross streaking with S. aureus or on unsupplemented agar with added X and V factors. Sterility test with biological indicator – following incomplete sterilization (autoclaving), the purple media turns yellow upon incubation, due to organism growth Enzyme immunoassay – detect the presence of an antibody or an antigen in a sample; unknown amount of antigen is affixed to a surface, and then a specific antibody is washed over the surface so that it can bind to the antigen. This antibody is linked to an enzyme, and in the final step a substance is added that the enzyme can convert to some detectable signal Complement fixation –patient’s serum is reacted with antigen and excess complement. Ag-Ab complexes bind, activate and fix complement. Residual complement is assayed through lysis of rbc’s coated with antibody Latex agglutination – detect antibody or soluble antigen. Virus-specific antibody causes latex particles coated with viral antigens to clump. Antibody-coated latex particles can also be used to detect viral antigen. Like hemagglutination. Darkfield microscopy – like a regular light microscope, except a condenser is used that prevents transmitted light from directly illuminating the specimen. Only oblique light hits the specimen, which allows it to be brightly lit against a dark background. Resolving power is better that with brightfield (light) microscopy, which makes it possible to see thin bacteria, like Treponema and Borrelia. Disadvantage: cannot view internal structures because light does not pass through the organism.