Preparation for Childbirth & Parenting
advertisement

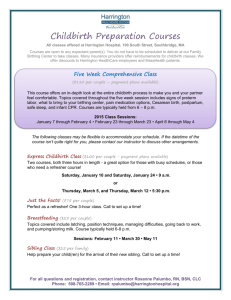
Preparation for Childbirth & Parenting Preparation for Childbirth Expectant families are faced with many choices about a childbirth experience and preparation for parenting. Birth attendant Setting Expectant parents need to be prepared for childbirth or cesarean birth. Physical Emotional Childbirth Education Prepare expectant mother and support person for the childbirth experience. Create knowledgeable consumers of OB care. Help clients reduce and manage pain. Help increase couples’ overall enjoyment with the childbirth experience. Childbirth Educators and Teaching: Group format with interaction with peers Videotapes, slides, lecture, demonstrations Efficacy of Childbirth Education Courses: Increase satisfaction, reduce amount of pain, and increase feelings of control. Cultural and Socioeconomic Factors: Sometimes the advice of family or friends carry more weight than a professionals. Avoid stereotyping Consider financial needs Perineal and Abdominal Exercises: Encourage woman to maintain an active exercise program during pregnancy. Classes teach exercises to strengthen their pelvic and abdominal muscles and make them more supple. This allows for stretching during birth, reducing discomfort, strengthened muscles return to normal quickly. Lamaze begins the last 8 to 10 weeks of pregnancy. Tailor Sitting: Stretches perineal muscles without occluding blood supply to the lower legs. Do not put one ankle on top of the other. 15 minutes per day. Squatting: Also stretches perineal muscles Useful position for 2nd stage of labor 15 minutes per day Keep feet flat on floor to be effective. Kegel Exercises (Pelvic Floor Contractions): Tighten muscles of perineum Helpful in postpartum period, perineal healing, increased sexual responsiveness, and stress incontinence in later life. Abdominal Muscle Contractions: Strengthen abdominal muscles. Prevents constipation and restores abdominal tone after pregnancy. Contracts abdominal muscles while standing or lying or hold fingers 6 inches in front of herself as if blowing out a candle. Pelvic Rocking: Helps relieve backache by making lumbar spine more flexible. Arch back, trying to lengthen or stretch the spine for 1 minute, then hollows her back. 5 times Methods for Pain Management 1. Discomfort can be minimized if woman is informed about what is happening and prepared with breathing exercises. 2. If abdomen is relaxed and uterus is allowed to rise freely against abdominal wall with contractions. 3. Pain perception can be altered by distraction techniques or gate control theory of pain perception. Bradley (Partner-Coached) Method: Muscle-toning exercises Limits foods with preservatives, animal fat, or high salt content. Abdominal breathing to relieve pain. Walk during labor and use an internal focus point as a disassociation technique. Psychosexual Method: A program of conscientious relaxation and levels of progressive breathing that encourages the woman to “flow with” the contraction. Dick-Read Method: Based on fear leads to tension Abdominal breathing during contractions. Lamaze Method Most often taught in the US today. Developed in Russia. Based on theory that thought stimulus-response conditioning, women can learn to use controlled breathing and reduce pain during labor. Gate control method of pain relief: Teaches A&P,labor and birth process. Sensation(contractions) can be inhibited from reaching the brain cortex and registering pain. Concentrate on breathing patterns Use imagery or focusing (concentrating) on a specific object to block incoming pain sensations. Conditioned reflexes-reflexes that automatically occur in response to stimulus. Displace pain during labor. Woman is conditioned to relax automatically on hearing a command. Pavlov Conscious Relaxation: Learn to relax body portions deliberately, relaxing one set of muscles then another. Support person notices symptoms of tension, wrinkled brow, clenched fists … Cleansing Breath: To begin and end all breathing exercises: woman breaths in deeply and exhales deeply. Limits hyperventilation. Consciously Controlled Breathing: Set breathing patterns at specific rates. Prevents diaphragm from descending fully which prevents pressure on uterus. Exhalation little stronger then inhalation. Level 1- slow chest breathing, full respirations, 6 to 12 /min. (early contractions). Level 2 – breathing lighter, rib cage expands but diaphragm barely moves. Rate 40/min. Use when cervix is 4 to 6 cm. Level 3- breathing more shallow at sternum. Rate 50 to 70/min. exhalation little stronger than inhalation saying “out” keeping tip of tongue against the roof of the mouth. Transition contractions. Level 4- “pant-blow”pattern. Take 3to 4 quick deep breaths in and out then forced exhalation. Breath-breath-breath-huff or hee-hee-hee-hoo. Level 5- Chest panting is continuous very shallow 60/min. used in 2nd stage to prevent pushing before full dilatation. Identify contraction by hand on abdomen or observe monitor. Cleansing breath Level 1- 3 breaths Level 2 - 4 to 6 breaths Level 3 - 10 breaths Level 2 - 4 to 6 breaths Level 1 - 3 or 4 breaths Cleansing breath Effleurage: Light abdominal massage with fingertips at constant pressure and rate. Distraction technique and decreases sensory stimuli transmission from abdominal wall. Can be done on thighs. Support person may do. Focusing or Imagery: Focusing intently on an object (sensate focus). Keeps sensory input from reaching the cortex of the brain. Do not break their concentration. Second Stage Breathing: Breath out while pushing. Avoid holding their breath. Do not practice pushing because they could rupture membranes. Expectant Parenting Classes Cover 4 to 8 hours of content spaced over a 4 to 8 week period. Tour of maternity unit, nutrition, birth, supplies, childcare and other plans. Sibling Education Classes: Acquaint siblings with what happens during birth at age appropriate levels. Childbirth Plan: Choice of setting and birth attendant. Meds, family, complications, visitation. Birth Setting Setting: Depends on woman’s health and fetus. Preferences, economics, hospital, birthing settings, or home. Physician, Nurse-midwife. Birth Attendant and Support Person: Obstetrician, physician, midwife. Father, doula or person to assist. Hospital Birth: Come to hospital when contractions are 5 min. apart and regular. Birthing room: LDR-labor-delivery-recovery rooms LDRP-labor-delivery-recovery-postpartum rooms. Bed converts to birthing bed. Home like setting, family present. Birthing chairs: Reclining chair with a slide away seat to allow perineal exposure. Gravity. Postpartal Care: May breast-feed immediately, infant remains with parents, “rooming in”, siblings visit. Alternative Birthing Centers: (ABCs) Wellness oriented childbirth facilities. Within or near a hospital. Screened for complications. Minimal analgesics or anesthesia. Remain 4 to 24 hours after birth. Home Birth: 1% in US Nurse midwife. No complications. Allows for family integrity: not separated. Children Attending the Birth: Need supervision. A pets birth may help prepare. Alternative Methods of Birth Leboyer Method: Based on decreasing the shock to the newborn. Moving from a warm, fluid filled intrauterine environment. Birthing room is darkened, warm, soft music playing or no harsh noises, handle the infant gently, cord is cut late, infant is placed immediately into a warm-water bath. Late cutting of cord may lead to excess blood viscosity in the newborn. Hydrotherapy and Water Birth: Soothing and relaxing. Baby is born under water and immediately brought to the surface for a first breath. Difficulties- feces, aspiration by fetus, and maternal chilling when she leaves the water.