Chapter 32
advertisement

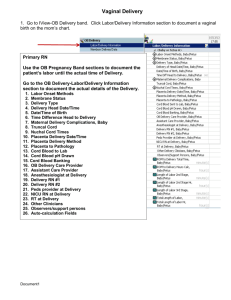
Ready for Review Most births are uneventful and do not require significant medical intervention. When ovulation occurs and a mature egg is released, it travels down the fallopian tubes toward the uterus. If sperm are present, fertilization may occur. The zygote should implant into the lining of the uterus. The umbilical cord connects woman and fetus through the placenta. The placenta acts as a barrier and a filter. As the fetus grows, the different structures that are recognizable begin to form. All fetal organs have formed by the eighth week of development. Full term is considered 40 weeks after conception. During pregnancy, the woman’s body undergoes many changes to support and protect the developing fetus. Menstruation ceases, the total blood volume increases, the heart rate elevates, blood pressure changes, the respiratory minute volume increases, and gastrointestinal complaints such as morning sickness and heartburn can occur. Emergencies can occur prior to delivery. The most common cause of vaginal bleeding during the first and second trimesters of pregnancy is spontaneous abortion (miscarriage). Abortion does not imply any cause but means that the fetus is released from the uterus before 20 weeks of gestation. Spontaneous abortion occurs when the fetus is released as the result of natural causes (miscarriage). In the field, keep the pregnant woman calm during a predelivery emergency; the hospital will determine the best course of action. Ectopic pregnancy occurs when the embryo implants in the fallopian tube, ovary, in the abdominal cavity, or the cervix. This is the most life-threatening emergency for the pregnant woman during the first trimester. Hypertension may occur during pregnancy. The most common disorder is preeclampsia, an increase in blood pressure after the 20th week of gestation. Preeclampsia can lead to cerebral hemorrhage or seizures. When a fetus has a different Rh factor than his or her mother, the antibody may attack fetal red blood cells and create complications such as hemolytic disease. Placenta previa is a condition where the placenta develops over and covers the cervix partially or completely. Abruptio placenta is the premature separation of the placenta from the wall of the uterus. This condition is dangerous for the woman and the fetus. Uterine rupture can occur after the mother experiences trauma. Uterine rupture causes significant bleeding that may be internal, external, or both. Knowing key obstetric terms such as gravida and para will create easier communication between health care providers. Gravida refers to the number of times a woman has been pregnant. Para refers to the number of times a woman has delivered a viable newborn. Ask an obstetric patient about any prior pregnancies as well as her current condition. You will have to determine whether you have time to provide transport to the hospital or attempt delivery in the field. You will assist with the delivery of the newborn at the scene when delivery can be expected within a few minutes. There are three stages of labor. The first stage of labor begins with the onset of contractions and ends when the cervix is fully effaced and dilated. The second stage of labor is from the point of full dilation and effacement (crowning [in the field]) until the newborn is delivered. The third stage of labor is from the delivery of the newborn until the delivery of the placenta. The only times you should place a finger or hand into the vagina are to keep the walls of the vagina from compressing the newborn’s airway during a face-down breech presentation or to push the newborn’s head away from the umbilical cord if it is prolapsed. If you deliver a newborn in the field, remember that your job is to help, guide, and support the newborn during delivery. Always contact medical control for guidance if you have concerns. To deliver a newborn, prepare a sterile delivery field. Support the newborn’s head as it emerges and feel to see if the cord is wrapped around the newborn’s neck. Guide the head and upper body to help deliver the shoulders. Keep the airway open, clamp and cut the cord, and allow the woman to deliver the placenta. Dry the newborn off and wrap the newborn to maintain body heat. The AEMT should be prepared to assess and manage postdelivery complications such as postpartum hemorrhage, pulmonary embolism, and prolapsed uterus. Abnormal or complicated deliveries include breech deliveries (buttocks first), limb presentations (arm, leg, or foot first), and prolapsed umbilical cord (umbilical cord first). Quickly transport the patient with a limb presentation or prolapsed umbilical cord or uterus to the hospital. Multiple gestations do not pose any special problems, although breech deliveries and premature newborns are more common with multiple gestations. Preterm labor may occur and result in the delivery of a premature newborn. These newborns need special care and resuscitation to survive. AEMTs should be prepared to address other complications during delivery such as stillborn babies, unruptured amniotic sac, meconium staining, and nuchal cords. After birth, the newborn makes a transition from receiving oxygen through the umbilical cord to breathing on its own. Most newborns breathe spontaneously without any advanced interventions. In a small percentage of births, fetal distress occurs. Newborn resuscitation refers to the series of interventions used to stimulate spontaneous breathing. Initial steps of neonatal resuscitation include drying and warming, positioning, suctioning, and stimulating the newborn. Three criteria are used to assess the need for further resuscitation in newborns: heart rate, color, and respiratory effort. The Apgar score is designed to measure the success of resuscitation, and should be taken at 1 and 5 minutes following birth. Venous access is not usually needed for newborns, but if required, IV access sites include the peripheral veins in the antecubital fossa and the saphenous vein just anterior to the medial malleolus of the ankle. Umbilical vein catheterization may be allowed in some EMS systems. A newborn who is not breathing or whose heart rate is less than 100 beats/min requires immediate positive-pressure ventilation and 100% oxygen. After 30 seconds of adequate ventilation, if the heart rate is at least 100 beats/min and the infant is breathing adequately, you may stop ventilations and assess the newborn’s color. If a newborn’s heart rate is less than 60 beats/min, provide ventilation and begin chest compressions. If a newborn has central cyanosis, apply free-flow oxygen. A newborn with hypovolemia may be given an isotonic crystalloid.