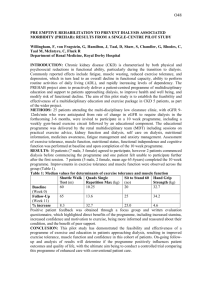
Dialysis
advertisement

Dialysis Dialysis Introduction Dialysis is a procedure that replaces the normal functions of the kidney by removing metabolic waste products through diffusion and hydraulic pressure gradients. Use of an artificial semipermeable membrane (hemodialyzer) or a natural semipermeable membrane (peritoneum) allows passage of some molecules while passage of other molecules is restricted. Molecules that can move through membrane move from the area of higher concentration to the area of lower concentration. 6 The dialysate is a combination of treated water and electrolyte concentrates used with the dialysis machine and system. 6 Dialysis is hazardous for the patient and for the staff that take care of the patient. Dialysis treatment is accomplished by two primary mechanisms, hemodialysis (HD) and peritoneal dialysis (PD). HD utilizes an artificial dialyzer for removal of metabolic waste products and PD uses the patient’s peritoneal cavity and membranes. Dialysis can be hazardous for the patient as venous access and insertion of foreign bodies can increase risk of infection. Also the patient might be exposed to exogenous microorganisms or to endotoxin from contaminants in the water used to prepare dialysis. Personnel that care for the patient are at risk of occupational exposure to blood-borne pathogens as patients requiring dialysis can have a high prevalence of blood-borne diseases. 7 Reuse of syringes and other breakdowns in infection control resulted in transmission of HIV to 39 patients at two dialysis centers in Egypt. 8 Infection Control in the Dialysis Setting Dialysis is used as a life sustaining treatment for patients with renal failure. Patients undergoing dialysis are already at risk of certain types of infections resulting from underlying diseases or conditions such as: Diabetes Hypertension Cardiovascular disease Immunosuppressive therapy Other critical diseases6 Furthermore, dialysis increases the patient’s risk of infection because direct access into normally sterile areas, including the circulatory system or peritoneal 24 Dialysis cavity, is required. Infection can be caused by contamination occurring at various steps in the dialysis procedure or because of intrinsic contamination of any of the components of the dialysis system. The most common types of dialysis-associated infections: Access site infections Bacteremias Peritonitis Pyrogenic reactions Infections with blood-borne pathogens6 Reducing Dialysis-Associated Infection Risk Infections and adverse reactions may be the result of inadequate infection control measures. 6 Risk of infection or of adverse reactions in the dialysis unit can be reduced by strictly adhering to aseptic technique and to procedures for disinfection, by maintenance of equipment, and by carefully monitoring all procedures in which bacterial or chemical contamination can occur. 6 Contact transmission is the most important route by which pathogens are transmitted in health care settings including dialysis units. Transmission can occur when microorganisms from a patient are transferred to the hands of health care personnel who do not use infection control precautions and who then touch another patient. Less often the environment around the patient, bedside tables, countertops, etc., become contaminated and serve as a reservoir of pathogens that can be picked up on hands of health care personnel and transferred subsequently to a patient. For example, if health care personnel hands are contaminated with blood-borne virus-infected blood from one patient, they can transfer the virus to another patient’s skin or blood line access port when the skin or port is accessed with a needle. Hemodialysis (HD) Hemodialysis removes toxins, electrolytes, and fluid by circulating the patients’ blood through a hemodialyzer (artificial kidney). Patients are usually scheduled to receive hemodialysis for two to six hours three times per week. The basic components of hemodialysis include circulatory access, water treatment system, water distribution system, dialysate (components), dialysis machines, blood tubing and the hemodialyzer.6 25 Dialysis Circulatory Access Access to the patients’ circulatory system is gained through the establishment of several different types of devices including external arteriovenous shunts, internal arteriovenous fistula, graft arteriovenous fistula, and temporary vascular access devices (e.g., dual lumen catheter in subclavian, jugular vein).6 Standard Precautions Hand hygiene and Protective Barriers Indications of routine handwashing in Dialysis unit Before and after dealing with dialysis machines Before and after performing non-invasive techniques After removal of gloves If hands are visibly dirty After leaving a particular patient dialysis station and before dealing with another patient’s stations Indications for aseptic handwashing Before performing any invasive procedure such as inserting circulatory access, CV lines and peritoneal catheters. Before and after connecting the patient to the dialysis machine through the AV fistulae Alcohol based hand rub can substitute handwashing in emergency cases or if water source is lacking, provided that hands are visibly clean. Gloves: Use non-sterile disposable gloves when performing non-invasive procedures, cleaning or disinfecting instruments or environment including the dialysis machine. Use sterile gloves when performing invasive procedures or connecting the patient to the dialysis machine Water-proof aprons or gowns should be worn if the nurse is located within the patient station producing any service. Note: Personnel should always have protective equipment (fluid resistant gown, mask, and eyewear) readily available to prevent their exposure to blood in the event that there is rupture of hemodialyzer membrane and/or a disconnection or rupture of tubing. These events can happen if there is increased pressure in the blood compartment of the hemodializer caused by an obstruction between the blood outlet of the hemodialyzer and the patient.6 26 Dialysis Aseptic technique Healthcare personnel can reduce the risk of infection by practicing the following procedures: Hands should be washed or waterless alcohol-based handrub should be applied before and after each patient contact. Any item taken to a patient's dialysis station could become contaminated with blood and other body fluids and therefore could serve as a vehicle of transmission to other patients either directly or by contamination of the hands of personnel. Therefore, items taken to a patient's dialysis station, including those placed on top of dialysis machines, should either be disposed of, dedicated for use only on a single patient, or cleaned and disinfected before being returned to a common clean area or being used for other patients. HCP should prepare a sterile set of materials for each patient for insertion of central venous catheters. Heparin should be prepared just prior to use for each patient. Vials should not be shared between patients. Aseptic technique of the skin over the fistula site (creation of a sterile field, use of sterile barriers and gloves) is effective in preventing infection. Before fistula cannulation, the patient should clean the arm with soap, if possible. Then any antiseptic solution (e.g. alcohol, betadine) should be applied in an outward circular motion to the selected needle insertion site and allowed to dry. If betadine (povidone-iodine) is used, permit it to dry for > 2 minutes prior to catheter insertion. Meticulous attention to aseptic technique should be used and the insertion site should not be palpated once the site has been prepared. A sterile gauze should be saturated with an antiseptic solution and applied to the ports of the central venous catheter for 5 minutes before opening the catheter when initiating hemodialysis and before disconnecting the blood lines at the termination of hemodialysis. Clean, non-sterile exam gloves and clean technique should be used during dressing changes. When shunts or central venous catheters are used for vascular access, a new sterile dressing should be applied after each dialysis treatment. Adhesive tape should not be applied directily to the catheter. Patients should be instructed in the proper way to care for the site. 6 27 Dialysis Equipment Dialysis machines Blood pump A blood pump consists of two or more rollers and is usually necessary to pump the patient’s blood through tubing and the hemodialyzer at stable and accurate blood flow rates. Fluid pathways There are three types of hemodialysis machines: Recirculating machines. Recirculating machines recirculate dialysate repeatedly through the hemodialyzer during dialysis.6 Recirculating single pass machines. Recirculating single pass machines recirculate dialysate repeatedly through the hemodialyzer during dialysis; however, dialysate in the recirculating reservoir is partially displaced by a constant flow of fresh dialysate.6 Single pass machines. Single pass machines provide a constant flow of dialysate, which passes through the dialysate compartment and is discarded.6 Recommendations Single-pass delivery machines are preferred. Recirculating systems permit nutrient-rich waste products from the patient to be used as nutrients for microorganisms and therefore may result in increased levels of bacteria during the dialysis treatment. In contrast, contamination of single pass machines is usually related to the quality of treated water or other dialysate components going into the machine and the adequacy of cleaning and disinfection procedures. 6 In a single pass machine Pipes and tubing of incoming water (batch system) or dialysate (proportioning system) as well as the internal dialysate and dialysate pathways must be disinfected at the end of the day In a single-pass machine the internal fluid pathways that supply dialysis fluid to the dialyzer are not subject to contamination with blood. If a blood leak occurs in a single-pass machine, it is not necessary to disinfect the internal fluid pathways because even if the fluid pathways that exhaust the dialysate became contaminated with blood, it would be unlikely that this blood contamination could reach the patient. 28 Dialysis External surfaces of the machine should be cleaned and disinfected between patients using low level disinfectant (according to manufacturers’ instructions).6 In a recirculating or recirculating single pass dialysis machine All fluid pathways should be disinfected immediately prior to first use and after each patient use. If a blood leak occurs, then the disinfection procedures used to control bacterial infection in the machines are considered sufficient to reduce blood contamination below infectious levels. Waste from the dialysis machine must not be allowed to back flow into the machine. This is often accomplished by allowing an air gap between the drain hose and the drain.6 Blood tubing To avoid bacteremia from contaminated blood tubing (e.g. gram-negative bacilli infecting the blood from ultrafiltration waste) the following control measures should be followed: Do not attach the venous tubing directly to the waste container during hemodialyzer priming. Always follow gloving and handwashing guidelines after contact with ultrafiltration waste. Decontaminate ultrafiltration waste containers daily.6 Cleaning of dialysis machines. For single-pass machines perform rinsing and disinfection procedures at the beginning or end of the day. For batch recirculating machines, drain, rinse, and disinfect after each use. Follow the same methods for cleaning and disinfection if a blood leak has occurred, regardless of the type of dialysis machine used. Venous pressure transducer protectors should be used to cover pressure monitors and should be changed between patients and should not be reused. Environmental Issues Establish written protocols for cleaning and disinfecting surfaces and equipment in the dialysis unit, including careful mechanical cleaning before any disinfection process. 29 Dialysis If the manufacturer has provided instructions on sterilization or disinfection of the item, these instructions should be followed. After each patient treatment, clean and perform low level disinfection of the environmental surfaces at the dialysis station, including the dialysis bed or chair, countertops, and external surfaces of the dialysis machine. Ideally, all linens should be changed between patients. Between uses of medical equipment (e.g., scissors, hemostats, clamps, stethoscopes, blood pressure cuffs), clean and apply a hospital disinfectant (i.e., low-level disinfection). If the item is visibly contaminated with blood, use an intermediate-level disinfection. For a blood spill, Clean up blood spills immediately. Besides preventing the spread of infection, prompt removal also prevents accidents. When cleaning up spills, always wear gloves, such as disposable or heavy duty gloves. If the spill is small, wipe it with a disposable cloth and then disinfect the surface area of the spill with another disposable cloth that has been saturated with a disinfectant (200-500 PPM chlorine solution). If the spill is large, place a disposable paper or cloth towel ove the spill to soak up the fluid. Still wearing gloves, pick up the towel, dispose into a container and then soak the area with non-diluted chlorine ). Leave it for considerable time then dry the surface. Do not simply place a cloth over the spill for cleaning up later; someone could easily slip and fall on it and be injured. Housekeeping staff members in the dialysis facility should promptly remove soil and potentially infectious waste and should maintain an environment that enhances patient care. Monitoring Water Used for Dialysis There should be a designated staff member who is responsible for the initial and routine monitoring of water and dialysate. This staff member should be knowledgeable of all aspects of the water treatment and distribution systems and have the authority to investigate and act on problems related to the quality of water used for hemodialysis. Water used to prepare dialysate and dilute germicides and reprocess hemodializers should meet Ministry of Health standards as defined in Ministerial Decree #63 for the year 1996. Microbiologic and chemical monitoring should be performed at least monthly in accordance with this decree.6 30 Dialysis Microbiologic monitoring The microbiologic monitoring of treated water should be performed at least monthly and more frequently if problems are identified. Water used to prepare dialysate should be collected at the point where it enters the proportioner or the dialysis machine. Water used to clean hemodialyzers during reprocessing or to dilute germicides should also be sampled. Dialysate samples should be collected during or at the end of dialysis or beyond the point where the dialysate leaves the hemodialyzer. Microbiologic testing of samples 1. Total viable counts should be obtained using either spread plates or the membrane filter technique. A calibrated loop should not be used because the small amount of water sampled makes this test insensitive. 2. The sample should be inoculated onto tryptic soy agar within 30 minutes of collection or the sample should be refrigerated at 5 degrees Celsius and processed within 24 hours. 3. Culture plates should be incubated at 35 to 37 C for 48 hours before colonies are counted. 4. Identification of organisms may be necessary to link high counts to cases of bacteremia. Total viable bacterial counts in water used to prepare dialysate or to reprocess hemodialyzers should not exceed 50 colony forming units (cfu) per milliliter. Total viable count for dialysate should not exceed 2000 cfu/ml. 6 If the count is greater than 2000 cfu/ml, dialysate equipment should be disinfected and culture repeated. Water treatment Municipal or potable water used to prepare dialysate or reprocess hemodialyzers must be treated to remove chemical, bacterial, or endotoxin contaminants that could be harmful to patients. When chlorine is removed from the water, as occurs during the treatment of water for hemodialysis, there is little to impede bacterial growth. Therefore, care must be taken at each step in the water treatment process to minimize the risk of introducing bacteria into the system or of allowing treated water to remain stagnant. 6 31 Dialysis Note: No system should be considered 100% effective at removing bacteria and/or endotoxin. This means that there is always a need to monitor product water for bacterial and endotoxin contamination.6 Most hemodialysis water treatment systems consist of the following components: Carbon filters: Carbon filters remove chlorine, chloramines, and organic material from the potable water. Carbon filters are prone to bacterial contamination. Consider placing at least two carbon filters in series to increase their effectiveness and to provide redundancy in the system. Because of the risk of cross-contamination and inadequate disinfection, carbon filters should be replaced, not regenerated, when exhausted.6 Particulate filters: Particulate filters are used to remove sediment from water. Bacterial growth can occur on the filter and lead to subsequent bacteremia and/or pyrogenic reactions. Note: These filters should be replaced and disinfected according to the manufacturer’s recommendations.6 Reverse Osmosis (RO): RO uses osmotic and hydrostatic pressure over a semi-permeable membrane to remove ions and organic compounds. In theory RO is capable of removing 90% to 99% of electrolytes and all bacteria, viruses and endotoxins. 6 Note: Cleaning and restoration of semipermeable membranes should be done according to the manufacturer’s recommendations.6 Deionizers: Deionizers contain resin beds, which remove cations and anions by binding them to the resin and releasing hydrogen and hydroxyl ions. Deionizers do not remove bacteria and endotoxin and resin beds may contribute to significant bacterial growth. Note: Deinonizers should be suspected of producing water that may contain high numbers of bacteria and/or endotoxin, even if proceeded by RO. 6 32 Dialysis Filters, ultrafilters, and ultraviolet germicidal irradiation (UVGI): Some dialysis centers use filters, ultrafilters, and/or UVGI to further reduce microbial and/or endotoxin contamination. UVGI may be ineffective in killing some bacteria and does not remove endotoxin. Only ultrafiltration is capable of removing bacteria and endotoxin. Water distribution and storage Water distribution systems should be constructed of plastic pipes because metal pipes could contaminate the treated water with chemicals such as copper, lead, or zinc. The minimal number of elbows and T joints should be used and outlets should be at the highest point of the system to allow adequate contact of all parts of the system with germicide. When possible, storage tanks should not be used because they increase the amount of water and surface area available for bacterial contamination. If a storage tank is used, it should be: 1. The smallest tank possible. 2. Designed to have a constant flow with no stagnant areas. 3. Airtight using an airtight lid. 4. Able to be cleaned, disinfected, and rinsed. All piping (including water lines to the dialysis machines) and storage tanks must be disinfected at intervals adequate to prevent bacterial growth in excess of 200 cfu/ml. The interval will depend on the quality of water entering the system and on the system’s design.6 Waste management All disposable items should be placed in bags thick enough to prevent leakage. Wastes generated by the hemodialysis facility might be contaminated with blood and should be considered infectious and handled accordingly. Solid medical wastes should be disposed of properly.6 Sharps should be disposed separetly in a safety sharp disposal box immediately after use. Safety box should be available for each patient station. Peritoneal Dialysis (PD) Peritoneal dialysis removes toxins, electrolytes, and fluid by diffusion through the peritoneal membrane. Peritoneal dialysis requires placement of a catheter into 33 Dialysis the abdomen for access and repeated infusion and drainage of dialysate. Basic components for peritoneal dialysis include: Abdominal access with a peritoneal catheter that can be placed either surgically or medically. Dialysate: a solution that is commercially available in glass bottles, polyvinyl bags, and plastic bottles. In Egypt plastic bottles are available in high and low concentrations. A schedule and system for dialysate infusion and removal. Note: There are three types of infections related to site of insertion for peritoneal dialysis: exit site infection, subcutaneous tunnel infections, and peritonitis. Sources of pathogens include the patient’s skin or nares, the dialysate, migration from the gastrointestinal tract, and vaginal leaks. Catheter related infections are due primarily to catheter placement and maintenance. Aseptic Technique Strict use of aseptic technique in the care of the operative wound and catheter exit site should be observed. Exit site care should be performed daily and when exit site becomes wet or soiled. Soap and water may be as effective as povidone-iodine for exit site care. Powders, lotions, ointments, and other skin irritating compounds should not be used. Patients and personnel should recognize early manifestations of infectious complications. Equipment Intermittent peritoneal dialysis (IPD) is performed several times a week (usually overnight), lasts to up to 48 hours. Continuous ambulatory peritoneal dialysis (CAPD) involves exchanges every 4 to 6 hours during the day. Prevention of infection Sterile technique and sterile field should be maintained during insertion of peritoneal catheter. Aseptic techniques should always be used during exchange procedures. The use of a mask during connect and disconnect procedures may reduce risk of infection with nasally carried S. aureus. The catheter exit site should be kept clean and dry. 34 Dialysis The catheter should be immobilized in a way that minimizes the chances of accidental pulling or trauma to the surrounding skin. Patients should be educated on proper catheter exit site care. Use of a disconnect system should be considered for each patient as they have been demonstrated to decrease the incidence of peritonitis. Dialysis Personnel Training and education for all personnel at risk for occupational exposure should be provided on a regular basis (e.g. annually) and for all new employees before beginning work in the dialysis unit. Hepatitis B vaccine should be provided to all dialysis personnel. Personnel should use of protective barriers in order to protect themselves and in order to prevent soiling of clothing when performing procedures during which spurting or spattering of blood might occur (e.g., during initiation and termination of dialysis, cleaning of dialyzers, and centrifugation of blood). Protective clothing or gear should be changed if it becomes soiled with blood, body fluids, secretions, or excretions. Staff members should not eat, drink, or smoke in the dialysis treatment area or in the laboratory. No work restrictions for staff infected with HVC, HBV or HIV/Aids, however they should strictly follow dialysis specific precautions. Environmental Factors and Design Issues for the Dialysis Facility Key Principles of Design Adequate provision of storage of clean and sterile supplies. At least one separate room for dialysis of patients who are HbsAg positive. Separate area of adequate size for all the water treatment equipment and filters. Separate room for disinfection of portable dialysis equipment. Separate area for disposable of soiled supplies and large volumes of body fluids. 35 Dialysis Patient Care Issues Devices used in dialysis units create an access site, which requires patient education to help minimize the risk of infection-related morbidity and mortality. Patient education steps that should be taken include: Patients should be instructed to keep the access site clean and dry at all times. The importance of personal hygiene and its possible relation to access site infections should be emphasized. Patients should be instructed in the proper way to care for the access site and to recognize and report any signs and symptoms of infection immediately. These signs include fever, chills, pain, and redness or drainage around the access site.6 Patients can be served meals or can eat food brought from home at their dialysis station. The glasses, dishes, and other utensils should be cleaned in the usual manner. No special care of these items is needed.6 Notes: HBsAg +ve patients should use be isolated in special rooms and use specific machines. Staff should be dedicated to these patients. Prevention of Transmission of Blood-borne Pathogens General recommendations: Staff members must follow Standard Precautions when exposure to blood or other potentially infectious materials (including peritoneal fluid) is likely. Dialysis clinics and centers should perform a hazard assessment to determine what personal protective equipment is necessary. Protective clothing might include fluid resistant gowns, gloves, masks, and/or protective eyewear. Times when exposure is likely to occur include initiation of dialysis, termination of dialysis, and during cleaning and disinfection procedures. Personal protective equipment should be available to dialysis personnel and visitors in the appropriate sizes. Use of protective equipment should be monitored and enforced. Prompt thorough cleaning and disinfection of surfaces and equipment that are contaminated with blood or other potentially infectious materials should be done with chlorine solution or with other disinfectants. 36 Dialysis Disposable items contaminated with blood, peritoneal fluid, or other potentially infectious materials should be disposed of according to the waste management guidelines found in Part I “Waste Management II: Safe Sharps Disposal.” All soiled linen should be considered potentially infectious and handled according to procedures outlined in Part I: “Enviromental Cleaning”. When multiple dose medication vials are used, prepare individual patient doses in a clean (centralized) area away from dialysis stations and deliver separately to each patient. Do not carry multiple dose vials from dialysis station to station. Personnel who experience an exposure incident should follow the procedures outlined in their facility’s infection control plan.6, 9, 10 Prevention and management of hepatitis B virus infection Preventing HBV transmission among chronic hemodialysis patients requires: Infection control precaution recommended for all hemodialysis patients. Regular testing for HbsAg every 3 months and prompt review of results. Isolation of HBsAg-positive patients with a dedicated room, machine, other equipment, supplies, and staff members. Vaccination of all patients pending availability of resources.10 When a HBsAg-positive seroconversion occurs: Review all patients’ routine laboratory test results to identify additional cases. Investigate potential sources for infection to determine if transmission might have occurred within the dialysis unit. Include a review of the newly infected patient’s recent medical history (e.g. blood transfusion, hospitalization), of high-risk behaviors (e.g. injecting drug use, sexual activity), and of unit practices and procedures. 10 Repeat HBsAg testing. Three months later repeat HBsAg testing and test for HBsAb to determine clinical outcome and need for counseling, medical evaluation, and vaccination of contacts. Patients who become HBsAg negative are no longer infectious and can be moved from isolation. 10 37 Dialysis Isolation of HBV-infected patients In order to isolate HBsAg-positive patients, designate a separate room for their treatment. Dedicate machines, equipment, instruments, supplies, medications that will not be used by HBV susceptible patients. and Staff members who are caring for HBsAg-positive patients should not care for susceptible patients at the same time. This includes the period when dialysis is terminated on one patient and initiated on another. In facilities in which a separate room is not possible, HBsAg positive patients should be separated from HBV-susceptible patients in an area removed from mainstream activity and should undergo dialysis on dedicated machines. If a machine that has been used on an HBsAg-positive patient is needed for an HBV-susceptible patient, internal pathways of the machine can be disinfected using conventional protocols and external surfaces can be cleaned using water and detergent and germicide. Dialyzers should not be reused on HBsAg-positive patients. Because HBV is efficiently transmitted through occupational exposure to blood, reprocessing dialyzers from HBsAg-positive patients might place HBVsusceptible staff members at increased risk for infection. Chronically infected patients (i.e., those who are HBsAg positive, total anti-HBc positive, and IgM anti-HBc negative) are infectious to others and are at risk for chronic liver disease. They should be counseled regarding preventing transmission to others and their household and sexual partners should receive hepatitis B vaccine. They should be evaluated (by consultation or referral, if appropriate) for the presence or development of chronic liver disease according to current medical practice guidelines. Persons with chronic liver disease should be vaccinated against hepatitis A, if susceptible. Chronically infected patients do not require any routine follow-up testing for purposes of infection control. However, annual testing for HBsAg is reasonable to detect the small percentage of HBV-infected patients who might lose their HBsAg. 10 Vaccination Ideally, Hepatitis B vaccine should be administered for all susceptible hemodialysis patients and staff. Vaccination is recommended for all pre-end-stage renal disease patients before they become dialysisdependent. The hepatitis B vaccine should administered through the 38 Dialysis intramuscular route and only in the deltoid muscle for both adults and children. Because antibody response is poorer in hemodialysis patients than in healthy controls, larger vaccine doses or an increased number of doses are required. In addition, vaccine induced protection is less complete in dialysis patients and necessitates administration of booster doses if antibody levels decline below 10 miu by enzyme immunoassay. If an adult patient begins the vaccine series with a standard dose before beginning hemodialysis treatment and then moves to hemodialysis treatment before completing the series, complete the series using the higher dose recommended for hemodialysis patients. 10 Post-vaccination testing and revaccination of nonresponders Test all vaccinated patients for antibody to surface antigen (anti-HBs) one to two months after the last primary vaccine dose to determine if the response to the vaccine is adequate (an adequate response is defined as > 10 mIU/ml). Patients and staff who do not respond to the primary vaccine series should be revaccinated with three additional doses and retested for response. No additional doses of vaccine are warranted for those who do not respond to the second series. Evaluate personnel who do not respond to revaccination to determine if they are HBsAg positive. Persons who are HBsAg positive should be counseled accordingly (e.g. the need for medical evaluation, vaccination of sexual and household contacts). Primary nonresponders who are HBsAg negative should be considered susceptible to HBV infection and counseled regarding precautions to prevent HBV infection and the need to obtain postexposure prophylaxis with hepatitis B immune globulin for any know or probable percutaneous or mucosal exposure to HBsAg-positive blood.10 Prevention and management of hepatitis C virus infection HCV transmission within the dialysis environment can be prevented by strict adherence to infection control precautions recommended for all hemodialysis patients. Although isolation of HCV-infected patients is not recommended, routine testing for ALT and anti-HCV is important for monitoring transmission within centers and for ensuring that appropriate precautions are being properly and consistently used.10 39 Dialysis HCV-negative patients Testing for anti-HCV every 3 months should be sufficient to monitor the occurrence of new HCV infections. Monthly ALT testing will facilitate timely detection of new infections and will provide a pattern from which to determine when exposure or infection might have occurred. If unexplained ALT elevations are observed in patients who are antiHCV negative, repeat anti-HCV testing is warranted. If unexplained ALT elevations persist in patients who repeatedly test anti-HCV negative, testing for HCV RNA should be considered.10 Anti-HCV seroconversions When a seroconversion occurs: Review all other patients' routine laboratory test results to identify additional cases. Perform additional testing as indicated later in this section. Investigate potential sources for infection to determine if transmission might have occurred within the dialysis unit. Include a review of the newly infected patient’s recent medical history (e.g., blood transfusion, hospitalization), of the patient’s high-risk behaviors (e.g., injecting-drug use, sexual activity), and of unit practices and procedures. If ongoing HCV transmission among patients is identified, implement control measures based on results of investigation of potential sources for transmission and monitor their effectiveness. HCV-positive patients Patients who are anti-HCV positive (or HCV RNA positive) have to be isolated from other patients or dialyzed separately on dedicated machines. Unlike HBV, HCV is not transmitted efficiently through occupational exposures. HCV-positive persons should be evaluated (by consultation or referral, if appropriate) for the presence or development of chronic liver disease according to current medical practice guidelines. They also should receive information concerning how they can prevent further harm to their liver and prevent transmitting HCV to others. Persons with chronic liver disease should be vaccinated against hepatitis A, and B if susceptible.10 40 Dialysis Prevention and management of hepatitis D infection transmission Because of the low prevalence of HDV infection, routine testing of hemodialysis patients is not necessary or recommended. However, if a patient is known to be infected with HDV or if evidence exists of transmission of HDV in a dialysis center, screening for delta antibody is warranted. Because HDV depends on an HBV-infected host for replication, prevention of HBV infection will prevent HDV infection in a person susceptible to HBV. Patients who are known to be infected with HDV should be isolated from all other dialysis patients, especially those who are HBsAg-positive.10 Prevention and management of HIV infection Routine testing of hemodialysis patients for HIV infection every 3 months for infection control purposes is recommended. If infected, they can receive proper medical care and counseling regarding preventing transmission of the virus. Infection control precautions recommended for all hemodialysis patients are sufficient to prevent HIV transmission between patients. HIV-infected patients do not have to be isolated from other patients or dialyzed separately on dedicated machines. Prevention and management of bacterial Infection Follow published guidelines for judicious use of antimicrobials, particularly vancomycin, to reduce selection for antimicrobial-resistant pathogens. Infection control precautions recommended for all hemodialysis patients are adequate to prevent transmission for most patients infected or colonized with pathogenic bacteria, including antimicrobialresistant strains. However, additional infection control precautions should be considered for treatment of patients who might be at increased risk for transmitting pathogenic bacteria. Such patients include those with either: 1. An infected skin wound with drainage that is not contained by dressings (the drainage does not have to be culture positive for VRE, MRSA, or any specific pathogen). 2. Fecal incontinence or diarrhea uncontrolled with personal hygiene measures. For these patients, consider using the following additional precautions: 41 Dialysis 1. Staff members treating the patient should wear a separate gown over their usual clothing and should remove the gown when finished caring for the patient. 2. Dialyze the patient at a station with as few adjacent stations as possible. (e.g., at the end or corner of the unit).10 42