Dimensional Yale-Brown Obsessive
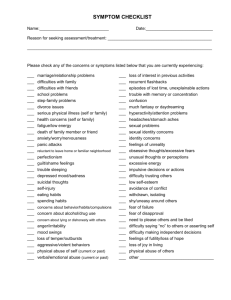
advertisement

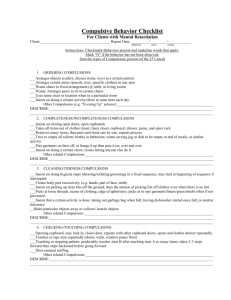
Patient's name________________________________ Today's Date: ___/___ /___ mm dd yy Clinician ____________________________________ Dimensional Yale-Brown Obsessive-Compulsive Severity Scale Clinician's Ratings of Current Severity by Symptom Dimension Aggressive Obsessions and Related Compulsions Sexual and Religious Obsessions and Related Compulsions Symmetry, Ordering, Counting, and Arranging Obsessions and Compulsions Contamination Obsessions and Cleaning Compulsions Hoarding and Collecting Obsessions and Compulsions Somatic Obsessions and Compulsions Miscellaneous Obsessions and Compulsions Clinician's Ratings of Current Global Symptom Severity June 2000 This scale is based in part on items from the Yale-Brown Obsessive Compulsive Sale (Goodman et al., 1989; Rosenfeld et al., 1993), the results of earlier factor analyses (Leckman et al., 1997; Mataix-Cols et al., 1999; Summerfeldt et al., 1999), and the DSM-IV field trial for OCD (Foa et al., 1995). Clinician Version 9.0 DIMENSIONAL YALE-BROWN OBSESSIVE-COMPULSIVE SCALE Rationale This rating scale is designed to evaluate the nature and current severity of obsessive-compulsive symptoms. It is an extension of the original Yale-Brown Obsessive-Compulsive Scale (Y-BOCS). The impetus for this new scale came from the results of factor analytic studies of the Y-BOCS symptom checklist in which four to five symptom dimensions have been consistently identified (Baer, J. Clin. Psychiatry 1994; 55:18–23; Leckman et al., Am. J. Psychiatry 1997; 154:911-917; Mataix-Cols et al., Am. J. Psychiatry 1999; 156:1409-16). These factors were: (1) aggressive obsessions and related compulsions, (2) sexual and religious obsessions and related compulsions; (3) symmetry, ordering, counting, and arranging obsessions and compulsions; (4) contamination obsessions and cleaning compulsions; and (5) hoarding and collecting obsessions and compulsions. Additional support for a dimensional approach has come from several sources. First, this factor structure has been confirmed by investigators in Canada (Summerfeldt et al., Behav Res Ther 1999; 37:297311). Second, based on family study data from Yale (Alsobrook et al., Neuropsychiatric Gene, 1999; 88:66975), two factors, were found to be associated with increased rates of OCD among first degree family members. The specific finding was that individuals with high scores on Factor 3 nearly were twice as likely to have first-degree family members with OCD compared to individuals with low scores. This suggests that some of the genetic determinants of OCD might be associated with particular symptom dimensions. Third, Scott Rauch and his colleagues at Massachusetts General Hospital have recently published a preliminary PET study (using an implicit learning activation technique) where they analyzed their results in light of this factor structure (Rauch et al., CNS Spectrums 1998; 3:37-43). They found that severity scores on factor (1) were positively associated with the blood flow (at each voxel) in the striatum but not with other brain regions. These results suggest the following: 1. It may be better to view OCD as a multidimensional disorder rather than a unitary condition; 2. A dimensional approach to OC symptoms may be useful in genetic and neurobiological studies; 3. Rating OC symptom severity within dimensions may be more sensible than making other distinctions, e.g., rating the severity of obsessions vs. compulsions as is presently done in the Y-BOCS; and 4. It is possible that using a multidimensional severity scale in treatment studies may reveal clinically relevant patterns of response (some treatments may do better in treating specific sets of symptoms, e.g., the Black et al. (J Clin Psychiatry 1998; 59:420-425) or the Mataix-Cols et al. studies that indicate that individuals with hoarding obsessions and related compulsions are less responsive to treatment). Consequently, this new instrument was developed - the Dimensional Yale-Brown Obsessivecompulsive Scale (DY-BOCS). Practically, by dividing symptoms by dimension, it is possible to inquire about symptom types that are inherently ambiguous. For example, checking compulsions are now asked about in several of the domains - checking related to sexual and religious obsessions vs. obsessions based on contamination worries. Other differences from the Y-BOCS include: inclusion of avoidance as an integral part of the severity ratings; expansion of ordinal severity scales (frequency, distress and interference) from 5 to 6 anchor points; and the absence of severity ratings based on the patient's effort to resist and control their symptoms. Acknowledgements The DY-BOCS is based on the Y-BOCS created by Wayne K. Goodman, Lawrence H. Price, Steven A. Rasmussen, and colleagues (Goodman et al., 1989; 1989). Many of the desirable elements of the Y-BOCS are retained in the DY-BOCS. The DY-BOCS is a product of a collaborative team of investigators from Yale University (James F. Leckman, Sheila Woody, Lawrence Scahill, and Sara Patrick), the Universidade de São Paulo (Maria C. Rosario-Campos and Euripedes C. Miguel), and Yukiko Kano (University of Tokyo). Many 2 other colleagues have contributed critiques and comments including Gail Steketee, Steven A. Rasmussen, Susanne Bejerot, David A. Clark, Dean McKay, David Rosenberg, Scott Rauch, John E. Calamari, Steven Taylor, Fugen Neziroglu, Neal Swerdlow, David L. Pauls, Bradley S. Peterson, Robert A. King, Diane Findley, C. Neill Epperson, John P. Alsobrook, and Donald J. Cohen. Their suggestions and encouragement are gratefully acknowledged. General Instructions Like the Y-BOCS, the DY-BOCS is intended for use as a semi-structured interview by qualified raters. Qualifications are based on training, experience and demonstrated reliability. Self-report questionnaire. In the interest of time, patients and families (if the patient is a child or adolescent) are asked to complete a self-report questionnaire that includes an extensive inventory of obsessive-compulsive symptoms prior to the DY-BOCS interview. The rater should review the completed questionnaire prior to beginning the DY-BOCS interview. DY-BOCS interview. We typically begin the interview by thanking the patient (and other informants) for the time they devoted to complete the questionnaire. In cases where the patient is a child or adolescent, it is important to establish who completed the questionnaire and how much participation the patient had in its completion. If the patient had a marginal role, it will be essential to establish the accuracy of the self-report. If the self-report data are judged inaccurate, indicate this on the clinician rating form (below). Next the interviewer should inquire if the patient had any difficulty in completing the questionnaire. It may be helpful to review the definitions of obsessions and compulsions provided at the beginning of the selfreport questionnaire and ask if the patient had any questions concerning what the definitions mean. Following this discussion, it is best to outline the rest of the interview - state that the interview will focus on five discrete groups of obsessive-compulsive symptoms. Then briefly describe the seven symptom categories: The first category concerns obsessions about harm (aggressive content) coming to oneself, to close family members or to other people because of some action (or lack of action) by the patient. The second category includes sexual, moral and religious obsessions. The compulsions in this category are mostly checking compulsions that relate directly to the obsessions. The third category includes obsessions about things needing to be perfect or exact. Other obsessions deal with a need for things to look or sound "just right" or to be symmetrical or properly aligned. Related compulsions include the need to count, order, arrange, or do certain things over and over again in hopes of getting it just right. The fourth category is simply contamination obsessions and cleaning and washing compulsions. The fifth category includes obsessions and compulsions that relate to hoarding or collecting. The sixth category includes obsessions and compulsions that relate to somatic concerns about health distinction from body dysmorphic and hypochondriacal symptoms. The seventh category includes miscellaneous obsessions and compulsions that relate to superstitions among other symptoms. Next, based on the information contained in the self-report the interviewer should identify symptoms in the first category present during the previous seven-day period. The interview should also indicate symptoms that have been present in the past but are not currently being experienced. Use the checklists for this purpose. As with the Y-BOCS, the rater must ascertain whether the reported symptoms are bona fide symptoms of OCD and not symptoms of another disorder, such as simple phobia, hypochondriasis, body dysmorphic disorder or paraphilia. Record this information on the clinician’s checklist provided below. Be sure to inquire about possible avoidance behaviors that may waste time, restrict or interfere with the patient's life, and that may cause distress. Rate only those symptoms present during the previous one-week period. 3 Once the group of symptoms has been identified (combining obsessions, related compulsions and avoidance behaviors), the three severity ratings for the first symptom category should be completed on the form provided. These ratings of duration, distress, and impairment should reflect the best judgment of the interviewer and be independent of the patient's self-ratings. The rater should assess the items in the listed order and use the questions provided. As with the Y-BOCS, the interviewer is free to ask additional questions for clarification. Having completed the first category checklist and ratings, the interviewer should repeat this process for each of the four remaining categories. If the patient is symptom-free in any category, check the appropriate box and move on to the next category. This version of the DY-BOCS also includes a “Other OC Spectrum Symptoms” category of obsessivecompulsive symptoms. us Obsessions and Compulsions,” and “Other OC Spectrum Symptoms” category of obsessive-compulsive symptoms. This is an assortment of symptoms - some are from the original Y-BOCS and others that have been included for research purposes. As before, the interviewer should document the presence of any of these symptoms during the previous week using the checklist provided. Finally, the interviewer should make a global, composite rating of symptom severity reflecting all obsessions and compulsions. In making these ratings the interviewer needs to review all of the major obsessions and compulsions mentioned in each category. If the patient has symptoms in only one dimension, then the global ratings can be taken directly from the ratings on that dimension - without the need for any additional interviewing in most cases. Practical Points In practice if difficulties are encountered in using this scale, it is often because the patient has difficulty in deciding in which dimension a particular symptom (or set of symptoms) belongs. In an effort to clarify how best to approach this issue a few practical points (with supporting examples) are discussed below. In general, however, we follow the patient’s lead, so if the patient rates a symptom on the DY-BOCS self report on a particular dimension and if the clinician determines that the symptom in question is bona fide, then the clinician should make a severity rating for that category. Selection of the most appropriate symptom dimension. Conceptually, some symptoms or constellations of symptoms may be included in more than one symptom dimension. It is commonplace for patients in completing the Self Report to check items in more than one dimension even though there is only a unitary set of symptoms. For example, obsessions about disease, related checking compulsions and an excessive need for reassurance conceivably might be under dimension (6) or (4). Our recommendation is for the clinician to rate them under dimension (6) unless there is a clear spontaneous report of contamination obsessions and cleaning rituals. If contamination obsessions and cleaning rituals are present (or have been present in the past) and that is the patient’s concern, the interviewer should make a rating for that dimension. In our experience, while it is best not to parse a unitary group of symptoms (as perceived by the patient) between two dimensions, sometimes it is necessary. Hybrid symptom combinations. Hybrid symptoms do occur (the combination of an obsession from one category with a compulsion from another). For example, cleaning compulsions performed because of "religious" or moral obsessions. Here a patient is obsessed with doing the "morally right thing" and is unable to leave a public bathroom unless he has compulsively cleaned the facilities used. In this instance, because of the patient's clarity that the cleaning compulsions were done in order to do the right thing, two ratings would need to be made – one for factor 2 and one for factor 4. Complex ensembles. It is not unusual for patients to describe discrete periods of time when symptoms from one dimension are interleaved with symptoms from another. For example, making sure things look symmetrical and "just right" as well as having worries about harm (aggressive content) befalling a close 4 family member and needing to check the burners on the stove. In these instances, it is often possible for the patient and interviewer to separate these symptoms into their respective dimensions and to rate them accordingly. 5 Checklist of Aggressive Obsessions and Related Compulsions (past week) Checklist check once () for any symptoms present during the past week. Here the emphasis is on aggressive thoughts and images. Care may be needed to distinguish between contamination and somatic obsessions. The term “harm” was used in the self-report. It is inherently ambiguous and some subjects may have checked some of the harm items when the symptoms are best understood in another context, i.e., contamination or somatic worries. Check only if clear that obsessions or compulsions are present and have aggressive content. Aggressive Obsessions Related compulsions _____ Might harm self (aggressive content) _____ Might be harmed (aggressive content) _____ Might harm loved ones unintentionally (close family members) _____ Might harm others unintentionally _____ Might harm loved ones intentionally (close family members) _____ Might harm others intentionally _____ Checking that no harm to self has occurred _____ Might be responsible for something else terrible happening _____ Violent or horrific images _____ Might blurt out obscenities or insults _____ Might do something embarrassing _____ Might be responsible for something terrible _____ Might act on other unwanted aggressive impulses _____ Might say harmful things (aggressive content) _____ Checking that no harm to others has occurred _____ Checking compulsions to prevent harm _____ Repeating to prevent harm _____ Mental rituals to prevent harm _____ Checking that nothing terrible has happened Avoidance – aggressive obsessions _____ Intentional avoidance of people, places or things because of any of the above obsessions or compulsions concerning aggressive obsessions Other obsessions or compulsions in this category (describe):___________________________ _______________________________________________________________________________ _______________________________________________________________________________ Symptoms in this category were present during the past week? Yes No If yes, complete the next page. If no, skip to next section. 6 Severity Ratings (past week) for Aggressive Obsessions and Related Compulsions 1. How much of your time is occupied by these obsessions and compulsions? Or how frequently do these obsessive thoughts and compulsions occur? Be sure to include the amount of time wasted by avoidance behaviors. 0 = No time at all 1 = Rarely, present during the past week, often not on a daily basis, typically less than 3 hours/week 2 = Occasionally, more than 3 hours/week, but less than 1 hour/day - occasional intrusion, need to perform compulsions, or avoidance (occurs no more than 5 times a day) 3 = Frequently, 1 to 3 hours/day - frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day, but most hours of the day are free of these obsessions, compulsions, and related avoidance) 4 = Almost always, more than 3 and up to 8 hours/day - very frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day and occurs during most hours of the day) 5 = Always, more than 8 hours/day - near constant intrusion of obsessions, need to perform compulsions, or avoidance (too numerous to count and an hour rarely passes without several obsessions, compulsions and/or avoidance) 2. How much distress do these obsessions and related compulsions cause? In most cases, distress is equated with anxiety, guilt, a sense of dread, or a feeling of exhaustion. It may be helpful to think about how distressed you would feel if you were prevented from performing your compulsions? Or how much distress you feel from needing to repeat your compulsions over and over again. Or how you would feel if you encountered something (person, place, or thing) you were planned to avoid? [Only rate distress or discomfort that seems triggered by these obsessions, the need to do the compulsions, or distress associated with avoidance]. 0 = No distress 1 = Minimal - when symptoms are present they are minimally distressing 2 = Mild - some clear distress present, but not too disturbing 3 = Moderate - disturbing - but still tolerable 4 = Severe - very disturbing 5 = Extreme - near constant and disabling distress 3. How much do these obsessions and related compulsions interfere with your family life, friendships, or ability to perform well at work or at school? Is there anything you can't do because of them? If you avoid things because of these thoughts, please include the interference that is the result of that avoidance. If you are not currently studying or working, how much would your performance be affected if you were a full time student or employee? 0 = No interference 1 = Minimal, slight interference with social or occupational activities, overall performance not impaired 2 = Mild, some interference with social or occupational activities, overall performance affected to a small degree 3 = Moderate, definite interference with social or occupational performance but still manageable 4 = Severe interference, causes substantial impairment in social or occupational performance 5 = Extreme, incapacitating interference 7 Sexual and Religious Obsessions and Related Compulsions Severity Ratings (past week) Checklist check once () for any symptoms present during the past week. Here the emphasis is on obsessions and compulsions based on sexual and religious concerns. Moral concerns that are not explicitly religious in character belong in this category as well. There may be some inherent overlap with the aggressive domain. However, check items in this category if the primary issue concerns sexual, moral or religious matters. Obsessions with sexual content Related compulsions _____ Forbidden or improper sexual thoughts _____ Content involves children or incest _____ Content involves homosexuality _____ Content involves violent sexual acts _____ Checking compulsions related to sexual obsessions _____ Repeating compulsions related to sexual obsessions _____ Mental rituals related to sexual obsessions Avoidance because of sexual obsessions _____ Intentional avoidance of people, places or things because of any of the above obsessions or compulsions concerning sex Obsessions with religious content* Related compulsions _____ Content involves sacrilege or blasphemy _____ Excessive concern with what is morally right or wrong _____ Checking or other compulsions related to religious obsessions _____Fear saying certain things _____ Need to tell, ask or confess things _____ Repeating compulsions related to religious obsessions _____ Mental rituals related to religious obsessions Avoidance - religious _____ Intentional avoidance of people, places or things because of any of the above obsessions or compulsions concerning religious topics Other obsessions or compulsions in this category (describe):___________________________ _______________________________________________________________________________ _______________________________________________________________________________ Symptoms in this category were present during the past week? Yes No If yes, complete the next page. If no, skip to next section. 8 Severity Ratings (past week) for Sexual and Religious Obsessions and Related Compulsions 1. How much of your time is occupied by these obsessions and compulsions? Or how frequently do these obsessive thoughts and compulsions occur? Be sure to include the amount of time wasted by avoidance behaviors. 0 = No time at all 1 = Rarely, present during the past week, often not on a daily basis, typically less than 3 hours/week 2 = Occasionally, more than 3 hours/week, but less than 1 hour/day - occasional intrusion, need to perform compulsions, or avoidance (occurs no more than 5 times a day) 3 = Frequently, 1 to 3 hours/day - frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day, but most hours of the day are free of these obsessions, compulsions, and related avoidance) 4 = Almost always, more than 3 and up to 8 hours/day - very frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day and occurs during most hours of the day) 5 = Always, more than 8 hours/day - near constant intrusion of obsessions, need to perform compulsions, or avoidance (too numerous to count and an hour rarely passes without several obsessions, compulsions and/or avoidance) 2. How much distress do these obsessions and related compulsions cause? In most cases, distress is equated with anxiety, guilt, a sense of dread, or a feeling of exhaustion. It may be helpful to think about how distressed you would feel if you were prevented from performing your compulsions? Or how much distress you feel from needing to repeat your compulsions over and over again. Or how you would feel if you encountered something (person, place, or thing) you were planned to avoid? [Only rate distress or discomfort that seems triggered by these obsessions, the need to do the compulsions, or distress associated with avoidance.] 0 = No distress 1 = Minimal - when symptoms are present they are minimally distressing 2 = Mild - some clear distress present, but not too disturbing 3 = Moderate - disturbing - but still tolerable 4 = Severe - very disturbing 5 = Extreme - near constant and disabling distress 3. How much do these obsessions and related compulsions interfere with your family life, friendships, or ability to perform well at work or at school? Is there anything you can't do because of them? How much do these symptoms bother other people and so affect your relationships with them? If you avoid things because of these thoughts, please include the interference that is the result of that avoidance. If you are not currently studying or working, how much would your performance be affected if you were a full time student or employed? 0 = No interference 1 = Minimal, slight interference with social or occupational activities, overall performance not impaired 2 = Mild, some interference with social or occupational activities, overall performance affected to a small degree 3 = Moderate, definite interference with social or occupational performance but still manageable 4 = Severe interference, causes substantial impairment in social or occupational performance 5 = Extreme, incapacitating interference 9 Checklist of Symmetry, Ordering, Counting, and Arranging Obsessions and Compulsions (past week) Checklist check once () for any symptoms present during the past week. This dimension is usually fairly distinctive when present. However, overlaps can occur with other dimensions, particularly when there are concerns about harm or illness. Check these items only if in your best judgement the symptoms are best accounted for under this category. Similarly, if you are uncertain about which category best covers the symptoms in question, please indicate your doubts with annotations and rate the symptoms accordingly in more than one dimension. Obsessions Compulsions _____ Content involves needing things to be perfect or exact or “just right” _____ Content involves needing things to be _____ Checking for own mistakes _____ Ordering and arranging compulsions _____ Compulsions involving touching, tapping or rubbing symmetrical or correctly aligned _____ Fear not saying “just the right thing” _____ Compulsions involving evening-up, or aligning _____ _____ _____ _____ Re-reading or re-writing compulsions Repeating routine activities Counting compulsions Other mental rituals Avoidance _____ Intentional avoidance of places or things because of these obsessions or compulsions Other symptoms in this category (describe):____________________________________ _____________________________________________________________________________ _____________________________________________________________________________ Symptoms in this category were present during the past week? Yes No If yes, complete the next page. If no, skip to next section. 10 Severity (past week) of Symmetry, Ordering, Counting, and Arranging Obsessions and Compulsions 1. How much of your time is occupied by these obsessions and compulsions? Or how frequently do these obsessive thoughts and compulsions occur? Be sure to include the amount of time wasted by avoidance behaviors. 0 = No time at all 1 = Rarely, present during the past week, often not on a daily basis, typically less than 3 hours/week 2 = Occassionally, more than 3 hours/week, but less than 1 hour/day - occasional intrusion, need to perform compulsions, or avoidance (occurs no more than 5 times a day) 3 = Frequently, 1 to 3 hours/day - frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day, but most hours of the day are free of these obsessions, compulsions, and related avoidance) 4 = Almost always, more than 3 and up to 8 hours/day - very frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day and occurs during most hours of the day) 5 = Always, more than 8 hours/day - near constant intrusion of obsessions, need to perform compulsions, or avoidance (too numerous to count and an hour rarely passes without several obsessions, compulsions and/or avoidance) 2. How much distress do these obsessions and related compulsions cause you? In most cases, distress is equated with anxiety, guilt, a sense of dread, or a feeling of exhaustion. It may be helpful to think about how distressed you would feel if you were prevented from performing your compulsions? Or how much distress you feel from needing to repeat your compulsions over and over again. Or how you would feel if you encountered something (person, place, or thing) you were planned to avoid? [Only rate distress or discomfort that seems triggered by these obsessions, the need to do the compulsions, or distress associated with avoidance.] 0 = No distress 1 = Minimal - when symptoms are present they are minimally distressing 2 = Mild - some clear distress present, but not too disturbing 3 = Moderate - disturbing - but still tolerable 4 = Severe - very disturbing 5 = Extreme - near constant and disabling distress 3. How much do these obsessions and related compulsions interfere with your family life, friendships, or ability to perform well at work or at school? Is there anything you can't do because of them? How much do these symptoms bother other people and so affect your relationships with them? If you avoid things because of these thoughts, please include the interference that is the result of that avoidance. If you are not currently studying or working, how much would your performance be affected if you were a full time student or employed? 0 = No interference 1 = Minimal, slight interference with social or occupational activities, overall performance not impaired 2 = Mild, some interference with social or occupational activities, overall performance affected to a small degree 3 = Moderate, definite interference with social or occupational performance but still manageable 4 = Severe interference, causes substantial impairment in social or occupational performance 5 = Extreme, incapacitating interference 11 Checklist of Contamination Obsessions and Cleaning Compulsions Checklist check once () for any symptoms present during the past week. Again, this category is usually quite distinctive when present and in some individuals it is the only dimension present. Care may be needed to distinguish between aggressive and somatic obsessions. Check only if clear obsessions or compulsions that include contamination content are present. Obsessions Compulsions _____ Content involves dirt and germs _____ Compulsive or ritualized hand washing _____ Repeated cleaning of household items or other inanimate objects _____ Ritualized showering, bathing, or toilet routines _____ Measures taken to prevent contact with household contaminants _____ Mental rituals associated with contamination _____ Concerns or disgust with bodily waste or secretions _____ Content involves environmental household contaminants _____ Content involves insects or animals _____ Bothered by sticky substances _____ Content involves worry about becoming ill because of contamination Avoidance _____ Intentional avoidance of places or things because of these obsessions or compulsions Other symptoms in this category (describe):____________________________________ _____________________________________________________________________________ _____________________________________________________________________________ Symptoms in this category were present during the past week? Yes No If yes, complete the next page. If no, skip to next section. 12 Severity (past week) of Contamination Obsessions and Cleaning Compulsions 1. How much of your time is occupied by these obsessions and compulsions? Or how frequently do these obsessive thoughts and compulsions occur? Be sure to include the amount of time wasted by avoidance behaviors. 0 = No time at all 1 = Rarely, present during the past week, often not on a daily basis, typically less than 3 hours/week 2 = Occasionally, more than 3 hours/week, but less than 1 hour/day - occasional intrusion, need to perform compulsions, or avoidance (occurs no more than 5 times a day) 3 = Frequently, 1 to 3 hours/day - frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day, but most hours of the day are free of these obsessions, compulsions, and related avoidance) 4 = Almost always, more than 3 and up to 8 hours/day - very frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day and occurs during most hours of the day) 5 = Always, more than 8 hours/day - near constant intrusion of obsessions, need to perform compulsions, or avoidance (too numerous to count and an hour rarely passes without several obsessions, compulsions and/or avoidance) 2. How much distress do these obsessions and related compulsions cause? In most cases, distress is equated with anxiety, guilt, a sense of dread, or a feeling of exhaustion. It may be helpful to think about how distressed you would feel if you were prevented from performing your compulsions? Or how much distress you feel from needing to repeat your compulsions over and over again. Or how you would feel if you encountered something (person, place, or thing) you were planned to avoid? [Only rate distress or discomfort that seems triggered by these obsessions, the need to do the compulsions, or distress associated with avoidance.] 0 = No distress 1 = Minimal - when symptoms are present they are minimally distressing 2 = Mild - some clear distress present, but not too disturbing 3 = Moderate - disturbing - but still tolerable 4 = Severe - very disturbing 5 = Extreme - near constant and disabling distress 3. How much do these obsessions and related compulsions interfere with your family life, friendships, or ability to perform well at work or at school? Is there anything you can't do because of them? How much do these symptoms bother other people and so affect your relationships with them? If you avoid things because of these thoughts, please include the interference that is the result of that avoidance. If you are not currently studying or working, how much would your performance be affected if you were a full time student or employed? 0 = No interference 1 = Minimal, slight interference with social or occupational activities, overall performance not impaired 2 = Mild, some interference with social or occupational activities, overall performance affected to a small degree 3 = Moderate, definite interference with social or occupational performance but still manageable 4 = Severe interference, causes substantial impairment in social or occupational performance 5 = Extreme, incapacitating interference 13 Checklist of Collecting and Hoarding Obsessions and Compulsions Checklist check once () for any symptoms present during the past week. This is a distinctive category that at times overlaps with concerns about doing harm. Check only if clear obsessions or compulsions that include collecting and hoarding are present. Obsessions Compulsions _____ _____ _____ _____ _____ Hoarding _____ Mental rituals that relate to hoarding Content involves needing to save things Content involves distress over discarding things Unable to decide to throw things away Obsessions about losing things Avoidance _____ Intentional avoidance of places or things because of these obsessions or compulsions Other symptoms in this category (describe):____________________________________ _____________________________________________________________________________ _____________________________________________________________________________ Symptoms in this category were present during the past week? Yes No If yes, complete the next page. If no, skip to next section. 14 Severity (past week) of Collecting and Hoarding 1. How much of your time is occupied by these obsessions and compulsions? Or how frequently do these obsessive thoughts and compulsions occur? Be sure to include the amount of time wasted by avoidance behaviors. 0 = No time at all 1 = Rarely, present during the past week, often not on a daily basis, typically less than 3 hours/week 2 = Occasionally, more than 3 hours/week, but less than 1 hour/day - occasional intrusion, need to perform compulsions, or avoidance (occurs no more than 5 times a day) 3 = Frequently, 1 to 3 hours/day - frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day, but most hours of the day are free of these obsessions, compulsions, and related avoidance) 4 = Almost always, more than 3 and up to 8 hours/day - very frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day and occurs during most hours of the day) 5 = Always, more than 8 hours/day - near constant intrusion of obsessions, need to perform compulsions, or avoidance (too numerous to count and an hour rarely passes without several obsessions, compulsions and/or avoidance) 2. How much distress do these obsessions and related compulsions cause? In most cases, distress is equated with anxiety, guilt, a sense of dread, or a feeling of exhaustion. It may be helpful to think about how distressed you would feel if you were prevented from performing your compulsions? Or how much distress you feel from needing to repeat your compulsions over and over again. Or how you would feel if you encountered something (person, place, or thing) you were planned to avoid? [Only rate distress or discomfort that seems triggered by these obsessions, the need to do the compulsions, or distress associated with avoidance.] 0 = No distress 1 = Minimal - when symptoms are present they are minimally distressing 2 = Mild - some clear distress present, but not too disturbing 3 = Moderate - disturbing - but still tolerable 4 = Severe - very disturbing 5 = Extreme - near constant and disabling distress 3. How much do these obsessions and related compulsions interfere with your family life, friendships, or ability to perform well at work or at school? Is there anything you can't do because of them? How much do these symptoms bother other people and so affect your relationships with them? If you avoid things because of these thoughts, please include the interference that is the result of that avoidance. If you are not currently studying or working, how much would your performance be affected if you were a full time student or employed? 0 = No interference 1 = Minimal, slight interference with social or occupational activities, overall performance not impaired 2 = Mild, some interference with social or occupational activities, overall performance affected to a small degree 3 = Moderate, definite interference with social or occupational performance but still manageable 4 = Severe interference, causes substantial impairment in social or occupational performance 5 = Extreme, incapacitating interference 15 Somatic Obsessions and Compulsions Symptoms Checklist check once () for any other symptoms present during the past week. Do not include symptoms related to body dysmorphic disorder or hypochondriasis. In hypochondriasis subjects believe that they have a serious illness or they are preoccupied with the idea that they do have a serious illness. Somatic obsessions _____ Content involves illness or disease Related compulsions _____ Checking or other compulsions related to somatic obsessions _____ Mental rituals other than checking related to somatic obsessions Avoidance – somatic obsessions _____ Intentional avoidance of people, places or things because of any of the above obsessions or compulsions concerning illness or disease Other symptoms in this category (describe):____________________________________ _____________________________________________________________________________ _____________________________________________________________________________ Symptoms in this category were present during the past week? Yes No If yes, complete the next page. If no, skip to next section. 16 Severity (past week) of Somatic Obsessions and Compulsions* 1. How much of your time is occupied by these obsessions and compulsions? Or how frequently do these obsessive thoughts and compulsions occur? Be sure to include the amount of time wasted by avoidance behaviors. 0 = No time at all 1 = Rarely, present during the past week, often not on a daily basis, typically less than 3 hours/week 2 = Occasionally, more than 3 hours/week, but less than 1 hour/day - occasional intrusion, need to perform compulsions, or avoidance (occurs no more than 5 times a day) 3 = Frequently, 1 to 3 hours/day - frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day, but most hours of the day are free of these obsessions, compulsions, and related avoidance) 4 = Almost always, more than 3 and up to 8 hours/day - very frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day and occurs during most hours of the day) 5 = Always, more than 8 hours/day - near constant intrusion of obsessions, need to perform compulsions, or avoidance (too numerous to count and an hour rarely passes without several obsessions, compulsions and/or avoidance) 2. How much distress do these obsessions and related compulsions cause? In most cases, distress is equated with anxiety, guilt, a sense of dread, or a feeling of exhaustion. It may be helpful to think about how distressed you would feel if you were prevented from performing your compulsions? Or how much distress you feel from needing to repeat your compulsions over and over again. Or how you would feel if you encountered something (person, place, or thing) you were planned to avoid? [Only rate distress or discomfort that seems triggered by these obsessions, the need to do the compulsions, or distress associated with avoidance.] 0 = No distress 1 = Minimal - when symptoms are present they are minimally distressing 2 = Mild - some clear distress present, but not too disturbing 3 = Moderate - disturbing - but still tolerable 4 = Severe - very disturbing 5 = Extreme - near constant and disabling distress 3. How much do these obsessions and related compulsions interfere with your family life, friendships, or ability to perform well at work or at school? Is there anything you can't do because of them? How much do these symptoms bother other people and so affect your relationships with them? If you avoid things because of these thoughts, please include the interference that is the result of that avoidance. If you are not currently studying or working, how much would your performance be affected if you were a full time student or employed? 0 = No interference 1 = Minimal, slight interference with social or occupational activities, overall performance not impaired 2 = Mild, some interference with social or occupational activities, overall performance affected to a small degree 3 = Moderate, definite interference with social or occupational performance but still manageable 4 = Severe interference, causes substantial impairment in social or occupational performance 5 = Extreme, incapacitating interference 17 Miscellaneous Symptoms Checklist check once () for any other symptoms present during the past week. Miscellaneous Obsessions Compulsions _____ Superstitious fears _____ Luck or unlucky numbers _____ Colors with special significance _____ Intrusive nonsense sounds, words or music _____ Intrusive (nonviolent) images _____ _____ _____ _____ _____ Need to know or remember certain things _____ Compulsions re: knowing, remembering Superstitious behavior Related compulsions Related compulsions Related compulsions _____ Related compulsions _____ Excessive list making ______ Obsessive slowness Avoidance associated with Miscellaneous Obsessions and Compulsions _____ Intentional avoidance of places or things because of these obsessions or compulsions Other symptoms in this category (describe):____________________________________ _____________________________________________________________________________ _____________________________________________________________________________ Symptoms in this category were present during the past week? Yes No If yes, complete the next page. If no, skip to next section. 18 Severity (past week) of Miscellaneous Obsessions and Compulsions* 1. How much of your time is occupied by these obsessions and compulsions? Or how frequently do these obsessive thoughts and compulsions occur? Be sure to include the amount of time wasted by avoidance behaviors. 0 = No time at all 1 = Rarely, present during the past week, often not on a daily basis, typically less than 3 hours/week 2 = Occasionally, more than 3 hours/week, but less than 1 hour/day - occasional intrusion, need to perform compulsions, or avoidance (occurs no more than 5 times a day) 3 = Frequently, 1 to 3 hours/day - frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day, but most hours of the day are free of these obsessions, compulsions, and related avoidance) 4 = Almost always, more than 3 and up to 8 hours/day - very frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day and occurs during most hours of the day) 5 = Always, more than 8 hours/day - near constant intrusion of obsessions, need to perform compulsions, or avoidance (too numerous to count and an hour rarely passes without several obsessions, compulsions and/or avoidance) 2. How much distress do these obsessions and related compulsions cause? In most cases, distress is equated with anxiety, guilt, a sense of dread, or a feeling of exhaustion. It may be helpful to think about how distressed you would feel if you were prevented from performing your compulsions? Or how much distress you feel from needing to repeat your compulsions over and over again. Or how you would feel if you encountered something (person, place, or thing) you were planned to avoid? [Only rate distress or discomfort that seems triggered by these obsessions, the need to do the compulsions, or distress associated with avoidance.] 0 = No distress 1 = Minimal - when symptoms are present they are minimally distressing 2 = Mild - some clear distress present, but not too disturbing 3 = Moderate - disturbing - but still tolerable 4 = Severe - very disturbing 5 = Extreme - near constant and disabling distress 3. How much do these obsessions and related compulsions interfere with your family life, friendships, or ability to perform well at work or at school? Is there anything you can't do because of them? How much do these symptoms bother other people and so affect your relationships with them? If you avoid things because of these thoughts, please include the interference that is the result of that avoidance. If you are not currently studying or working, how much would your performance be affected if you were a full time student or employed? 0 = No interference 1 = Minimal, slight interference with social or occupational activities, overall performance not impaired 2 = Mild, some interference with social or occupational activities, overall performance affected to a small degree 3 = Moderate, definite interference with social or occupational performance but still manageable 4 = Severe interference, causes substantial impairment in social or occupational performance 5 = Extreme, incapacitating interference *Just include the miscellaneous obsessions and compulsions listed on p.17 in making these severity ratings 19 Global Obsessive-compulsive Symptom Severity Indicate your best judgment concerning which symptom categories are present. Review with the patient how well their obsessions and compulsions fit within a given symptom category: 2 = Clearly present and symptoms are readily understood in terms of a given symptom dimension; 1 = might be present, but significant uncertainty exists such that their symptoms are not readily understood in terms of a given symptom dimension; 0 = symptoms within a given dimension were absent or “probably absent” during the past week. _____ Aggressive obsessions and related compulsions _____ Sexual and religious obsessions and related compulsions _____ Symmetry, ordering, counting, and arranging obsessions and compulsions _____ Contamination obsessions and cleaning compulsions _____ Collecting and hoarding _____ Somatic obsessions and compulsions _____ Miscellaneous obsessions and compulsions Rank order the symptom categories by severity for the past week. 1 = most severe, 2 = next most severe, and so on. Please mark each category. If symptoms were absent during the past week, place a "0" in the space provided. _____ Aggressive obsessions and related compulsions _____ Sexual and religious obsessions and related compulsions _____ Symmetry, ordering, counting, and arranging obsessions and compulsions _____ Contamination obsessions and cleaning compulsions _____ Collecting and hoarding obsessions and compulsions _____ Somatic obsessions and compulsions _____ Miscellaneous obsessions and compulsions List the patient's most prominent obsessive-compulsive symptoms: 1.___________________________________________________________________________ 2.___________________________________________________________________________ 3.___________________________________________________________________________ 20 What is the worst thing that the patient worries will happen if she/he did not respond to obsessive thoughts or urges to perform compulsions or rituals? Please describe: __________________________________________________________________________ __________________________________________________________________________ How certain is the patient that this feared consequence is reasonable and will actually occur? 0 = Certain that the feared consequence will not happen 1 = Mostly certain that the feared consequence will not happen 2 = Unsure whether or not the feared consequence will or won't happen 3 = Mostly certain that that the feared consequence will happen 4 = Certain that the feared consequence will happen Finally review all obsessive-compulsive symptoms endorsed as occurring during the past week (excluding "other" symptoms judged not be bona fide obsessive-compulsive symptoms) and make a global severity rating for the past week using the ordinal scales on the next page and complete the score sheet. Reliability of informant(s) Excellent = 0 Good = 1 Fair = 2 Poor = 3 21 Global Severity Obsessions and Compulsions (past week) 1. How much of your time is occupied by these obsessions and compulsions? Or how frequently do these obsessive thoughts and compulsions occur? Be sure to include the amount of time wasted by avoidance behaviors. 0 = No time at all 1 = Rarely, present during the past week, often not on a daily basis, typically less than 3 hours/week 2 = Occasionally, more than 3 hours/week, but less than 1 hour/day - occasional intrusion, need to perform compulsions, or avoidance (occurs no more than 5 times a day) 3 = Frequently, 1 to 3 hours/day - frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day, but most hours of the day are free of these obsessions, compulsions, and related avoidance) 4 = Almost always, more than 3 and up to 8 hours/day - very frequent intrusion, need to perform compulsions, or avoidance (occurs more than 8 times a day and occurs during most hours of the day) 5 = Always, more than 8 hours/day - near constant intrusion of obsessions, need to perform compulsions, or avoidance (too numerous to count and an hour rarely passes without several obsessions, compulsions and/or avoidance) 2. How much distress do these obsessions and related compulsions cause? In most cases, distress is equated with anxiety, guilt, a sense of dread, or a feeling of exhaustion. It may be helpful to think about how distressed you would feel if you were prevented from performing your compulsions? Or how much distress you feel from needing to repeat your compulsions over and over again. Or how you would feel if you encountered something (person, place, or thing) you were planned to avoid? [Only rate distress or discomfort that seems triggered by these obsessions, the need to do the compulsions, or distress associated with avoidance.] 0 = No distress 1 = Minimal - when symptoms are present they are minimally distressing 2 = Mild - some clear distress present, but not too disturbing 3 = Moderate - disturbing - but still tolerable 4 = Severe - very disturbing 5 = Extreme - near constant and disabling distress 3. How much do these obsessions and related compulsions interfere with your family life, friendships, or ability to perform well at work or at school? Is there anything you can't do because of them? How much do these symptoms bother other people and so affect your relationships with them? If you avoid things because of these thoughts, please include the interference that is the result of that avoidance. If you are not currently studying or working, how much would your performance be affected if you were a full time student or employed? 0 = No interference 1 = Minimal, slight interference with social or occupational activities, overall performance not impaired 2 = Mild, some interference with social or occupational activities, overall performance affected to a small degree 3 = Moderate, definite interference with social or occupational performance but still manageable 4 = Severe interference, causes substantial impairment in social or occupational performance 5 = Extreme, incapacitating interference 22 Clinician Rating of Impairment Finally, we would like you to think about how much impairment these symptoms have caused cumulatively (up until the present time) to the patient's self-esteem, social, family and job (or academic) functioning as well as her or his ability to cope with life’s difficulties. Please refer to the anchor points listed below. Choose the best value between 0-15, including the ones that are between the anchor points. 0 NONE 3 MINIMAL. Obsessions and compulsions associated with subtle difficulties in self-esteem, family life, social acceptance, or school or job functioning (infrequent upset or concern about obsessions and compulsions vis à vis the future, periodic, slight increase in family tensions because of obsessions and compulsions, friends or acquaintances may occasionally notice or comment about obsessions and/or compulsions in an upsetting way). 6 MILD Obsessions and compulsions associated with minor difficulties in self-esteem, family life, social acceptance, or school or job functioning. 9 MODERATE Obsessions and compulsions associated with some clear problems in self-esteem family life, social acceptance, or school or job functioning (episodes of dysphoria, periodic distress and upheaval in the family, frequent teasing by peers or episodic social avoidance, periodic interference in school or job performance because of obsessions and/or compulsions). 12 MARKED Obsessions and compulsions associated with major difficulties in self-esteem, family life, social acceptance, or school or job functioning, 15 SEVERE Obsessions and compulsions associated with extreme difficulties in self-esteem, family life, social acceptance, or school or job functioning (severe depression with suicidal ideation, disruption of the family (separation/divorce, residential placement), disruption of ties - severely restricted life because of social stigma and social avoidance, removal from school or loss of job). Reliability of informant(s) Excellent = 0 Good = 1 Fair = 2 Poor = 3 23 DY-BOCS Score Sheet Patient's name______________________________ Clinician ____________________ Today's Date: __ / _ _ / _ _ mm dd yy 1. DOCSSS Clinician Severity Ratings by Symptom Dimension for the Past Week Symptom Dimension Time (0-5) Distress (0-5) Interference (0-5) Total (0-15) Contamination & Cleaning Hoarding & Collecting Symmetry, Ordering, Counting & Arranging Harm due to Injury, Violence, Aggression, Natural Disasters and related compulsions Sexual & Religious Miscellaneous 2. DOCSSS Global Severity Ratings for the Past Week Time (0-5) Distress (0-5) Interference (0-5) Impairment (0-15) Total Score (0-30) All Obsessions & Compulsions Time required to complete the ratings: ________ minutes 2 OC Spectrum Symptoms Other Somatic obsessions* Related compulsions _____ Content involves bodily appearance _____ _____ _____ ____ _____ Content concerns the urge to pluck hair _____ Content concerns the urge to pick skin Related grooming compulsions Related dressing compulsions Related eating habits Related compulsions related to physical exercise _____ Trichotillomania _____ Skin picking Obsessions related to separation or union* Compulsions _____ Concerns about being separated from a close family member _____ Concerns about becoming or being too much like another person _____ Compulsions to prevent the loss of a close family member _____ Related compulsions _____ Content involves food or eating Tic-related Obsessions* _____ Staring rituals _____ Urge to repeat something you heard * As in the original Y-BOCS, do not include these obsessions and compulsions in the severity ratings. Specialized rated instruments should be employed to rate separation anxiety disorder, tic disorders, eating disorders, body dysmorphic disorder, and trichotillomania. They are included here to document OC spectrum symptoms for research purposes.