ER measurements / Ddx - Department of Radiological Sciences
advertisement
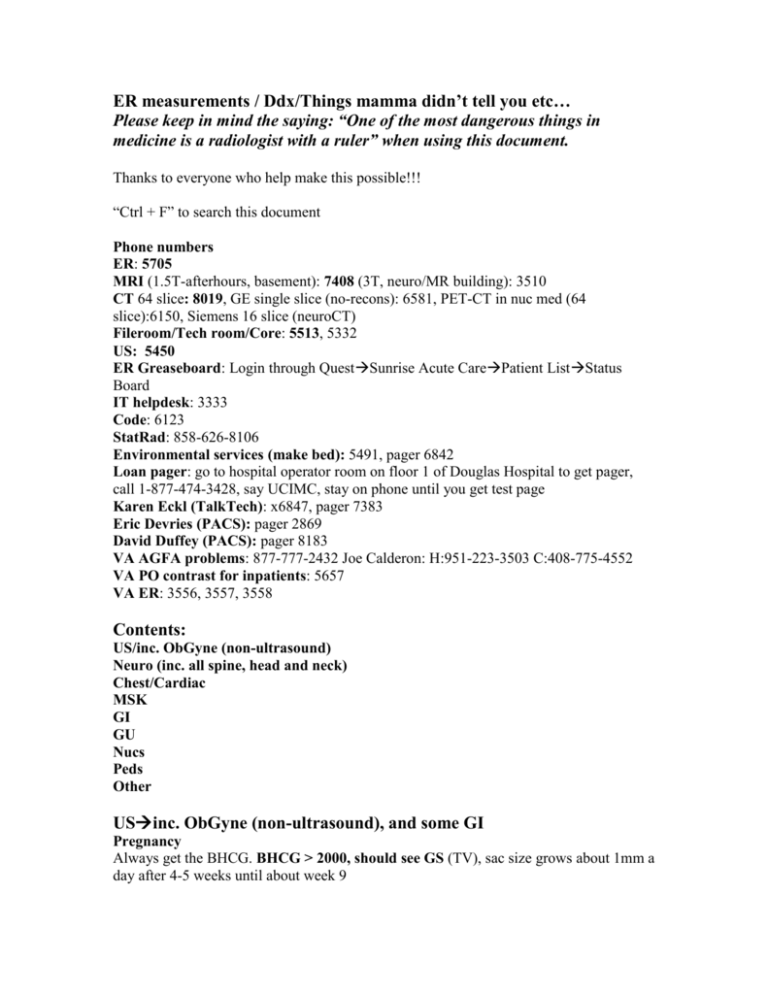
ER measurements / Ddx/Things mamma didn’t tell you etc… Please keep in mind the saying: “One of the most dangerous things in medicine is a radiologist with a ruler” when using this document. Thanks to everyone who help make this possible!!! “Ctrl + F” to search this document Phone numbers ER: 5705 MRI (1.5T-afterhours, basement): 7408 (3T, neuro/MR building): 3510 CT 64 slice: 8019, GE single slice (no-recons): 6581, PET-CT in nuc med (64 slice):6150, Siemens 16 slice (neuroCT) Fileroom/Tech room/Core: 5513, 5332 US: 5450 ER Greaseboard: Login through QuestSunrise Acute CarePatient ListStatus Board IT helpdesk: 3333 Code: 6123 StatRad: 858-626-8106 Environmental services (make bed): 5491, pager 6842 Loan pager: go to hospital operator room on floor 1 of Douglas Hospital to get pager, call 1-877-474-3428, say UCIMC, stay on phone until you get test page Karen Eckl (TalkTech): x6847, pager 7383 Eric Devries (PACS): pager 2869 David Duffey (PACS): pager 8183 VA AGFA problems: 877-777-2432 Joe Calderon: H:951-223-3503 C:408-775-4552 VA PO contrast for inpatients: 5657 VA ER: 3556, 3557, 3558 Contents: US/inc. ObGyne (non-ultrasound) Neuro (inc. all spine, head and neck) Chest/Cardiac MSK GI GU Nucs Peds Other USinc. ObGyne (non-ultrasound), and some GI Pregnancy Always get the BHCG. BHCG > 2000, should see GS (TV), sac size grows about 1mm a day after 4-5 weeks until about week 9 Please refer to the following images for “pseudosac” sign seen in ectopic, and “double decidual sign” or “intradecidual sign”universally present when MSD ≥10mm, is one of the earliest signs of nl pregnancy http://radiology.rsna.org/content/245/2/385.full http://radiopaedia.org/articles/double_decidual_sign Transvaginal MSD ≥ 8mm = yolk sac MSD ≥ 16mm = fetal pole = embryo CRL ≥ 5 mm = heat beat, heart beat may be seen as early as 1.5mm Transabdominal MSD ≥ 20mm = YS MSD ≥ 25mm = fetal pole Should be able to obtain FHR around 5 weeks (Bolded criteria above are most reliable and most important) Fetal heart rate (average nl120-160bpm), but is based on fetal age, measured on M-mode ultrasound, the lower limit of normal may be 90 bpm at 6 weeks or less, and 110bpm at greater then 6weeks, from 5 to 9 weeks the heart rate rapidly increases from 110 to 175 bpm then gradually decreased to 160-170bpm. Nl heart beat at 6 weeks is about 90113bpm. Fetal demise after T1 bradycardia most often occurs within the first week after detection of the brady; F/U recommended at 1 week; about 25% of T1 bradycardia will go on to demise http://radiology.rsna.org/content/236/2/643.full http://www.jultrasoundmed.org/cgi/content/abstract/14/6/431 Chart of nl fetal heart rates best on GA http://www.i-am-pregnant.com/encyclopedia/F/Fetal-Heart-Rate/ Minimum FHR based on fetal pole: 2mm embryo: 75 beats per minute 5 mm embryo: 100 beats per minute 10 mm embryo: 120 beats per minute 15 mm embryo: 130 beats per minute Coulam CB, Britten S, Soenksen DM. Early (34-56 days from last menstrual period) ultrasonographic measurements in normal pregnancies. Hum Reprod. 1996 Aug;11(8):1771-4. FYI: Note that nl heart rate for children 1-10yo is 70-120bpm, and HR may be 10bpm faster in women than men B-HCGafter 1 month, HCG doubles Q2d, peaks at 10-12w, then decreases to 22w, then increases again. BHCG 5000embryonic pole, 7000yolk sac, 10,000heart beat FYI only (not reliable): Week from the Last Menstrual Period Amount of HCG in mIU/ml 3 5 -50 4 3 - 426 5 19 - 7,340 6 1,080 - 56,500 7-8 7,650 - 229,000 9 - 12 25,700 - 288,000 13 - 16 13,300 - 254,000 17 - 24 4,060 - 165,400 25 - 40 3,640 - 117,000 Because of the wide variation in values, the test is not useful in establishing the gestational age of a pregnancy. http://www.obfocus.com/questions/qanda7.htm If an echogenic intracardiac focus (>90% in LV) is detected on fetal US, there is about a 1% risk for chromosomal abnormality, but this % is somewhat debatable, and most centers will recommend amniocentesis Echogenic fetal bowel when the bowel is brighter than the liver and as bright as bone in T2, worrisome for CF or chromosomal abn/aneuploidy (ex. Down’s)recommend amnio, T3 echogenic bowel is a common finding and of uncertain significance <20w GA, cannot reliably dx placenta previa, highest incidence during T2, many partial previas will resolve, but complete rarely does, overdistended bladder and myometrial contractions may give false positives, obtain post-void images; note a full bladder may under-dx cervical incompetence http://emedicine.medscape.com/article/404639-media Placental abnormalities (increase w/ C-sx, often seen w/ previa) Percretia(5%, worst, placenta penetrates entire uterine wall), incretia, accretia(75%) Pregnancy/Breastfeeding and Contrast Non-trauma pregnant patients need to sign a consent form for CT. IV iodine and IV gadolinium effects in humans are not fully understood, both cross the placenta, and should be avoided if possible. There is concern IV iodinated contrast may suppress neonatal thyroid function, and some recommend checking thyroid function in neonate in first week post-partum if iodinated contrast was given during pregnancy. The fetal thyroid starts trapping iodine by around 10-12w. http://www.ajronline.org/cgi/content/full/191/1/268 For both iodinated contrast and gadolinium based media in breast-feeding—it is thought to be generally safe to resume breast feeding right after the study due to the extremely low absorbed infant dose, but if the patient has any concerns, they may abstain for 24hrs http://www.acr.org/SecondaryMainMenuCategories/quality_safety/contrast_manual/Full Manual.aspx#page=65 Most important reference: ACR Contrast Manual (latest as on Oct. 2010 is V7): http://www.acr.org/SecondaryMainMenuCategories/quality_safety/contrast_manua l.aspx Four main recommendations for documentation in the radiology report for both iodinated and gad-based contrast per this manual in pregnant patients: 1. That information requested from the study cannot be acquired without the use of IV contrast or by using other imaging modalities. 2. That the information needed affects the care of the patient and fetus during the pregnancy. 3. That the referring physician is of the opinion that it is not prudent to wait to obtain this information until after the patient is no longer pregnant. 4. Obtain informed consent from patient if possible “Blighted ovum” = failed pregnancy Transcranial ultrasound after stroke for vasospasm: Lindegard ratio: MCA/ICA velocity Hyperemia 1.7 to 3, vasospasm >3 Nl non-pregnant US uterus(VA chart): 8 x 5 x 4cm Subchorionic hemorrhage Most is small, should be followed as is assoc. w/ high risk fetal loss, but is usually insignificant when small Important to ddx placental cotyleydons, chorionic plate indentations, myometrial contractions and venous lakes vs placental abruption which presents as an area of decreased placental enhancement “True placental abruptions were characterized by large, contiguous, and retroplacental and/or full-thickness areas of low enhancement that form acute angles with myometrium”. Especially look for this in trauma patients. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2716448/ Endometrium (VA Chart): Premenopausal Immediate postmenstrual 1-4mm Proliferative 4-8mm Secretory 8-14mm Postmenopausal Asymptomatic nl ≤ 8mm w/ hemorrhage nl ≤ 4mm w/ Tamoxifen and HRT stripe can be ≤ 8mm normally, but depends on type of HRT Ovary A dominant follicle in an ovulating woman is normally <3cm Suggestive of malignancyNodular soft tissue component, septal wall thickening, RI<0.4, pulsatility index <1 Asymptomatic ovarian cysts SRU 2009 Guidelines http://radiology.rsna.org/content/256/3/943.full Simple Unilocular cysts (inc. paraovarian, and cysts w/ a single <3mm septation or small wall calcification) In women of reproductive age: ≤3 cm: Normal physiologic findings; at the discretion of the interpreting physician whether or not to describe them in the imaging report; do not need follow-up. >3 and ≤5 cm: Should be described in the imaging report with a statement that they are almost certainly benign; do not need follow-up. >5 and ≤7 cm: Should be described in the imaging report with a statement that they are almost certainly benign; yearly follow-up with US recommended. >7 cm: Since these may be difficult to assess completely with US, further imaging with magnetic resonance (MR) or surgical evaluation should be considered. In postmenopausal women: ≤1 cm: Are clinically inconsequential; at the discretion of the interpreting physician whether or not to describe them in the imaging report; do not need follow-up. >1 and ≤7 cm: Should be described in the imaging report with statement that they are almost certainly benign; yearly follow-up, at least initially, with US recommended. Some practices may opt to increase the lower size threshold for follow-up from 1 cm to as high as 3 cm. One may opt to continue follow-up annually or to decrease the frequency of follow-up once stability or decrease in size has been confirmed. Cysts in the larger end of this range should still generally be followed on a regular basis. >7 cm: Since these may be difficult to assess completely with US, further imaging with MR or surgical evaluation should be considered. Hemorrhagic cysts (normally resolve in 8w): In women of reproductive age: 1. Cysts ≤3 cm: At the discretion of the interpreting physician whether or not to describe them in the imaging report; do not need follow-up. 2. Cysts >3 and ≤5 cm: Should be described in the imaging report; do not need follow-up. 3. Cysts >5 cm: Should be described in the imaging report; short-interval follow-up (6– 12 weeks) with US recommended to ensure resolution. While imaging in the follicular phase, on days 3–10 of the menstrual cycle, is optimal, the panel recognized that this is sometimes difficult to coordinate in clinical practice. Early post-menopausal (may still ovulate) Any hemorrhagic cyst early short-interval (6-12w follow-up) Late post-menopausal Any hemorrhagic cystsurgical exploration Ovary volume = 0.523 x width x length x thickness, normal average volume = 10mL If one ovary is 1.75 times larger than the other, think ovarian torsion, also look for peripheral follicles Stein-Leventhal (PCOD)—classic findings--numerous small (<1cm) peripheral cortical follicles (at least 5 in each ovary) w/ hyperechoic ovarian stroma, prominent fibrous capsule, both ovaries are enlarged Spleen size ≤ 13cm Common bile duct= measured at porta hepatis, 6mm max up to age 60, then add 1mm for each decade thereafter for upper limit of normal (ex. 7mm at 70yo) Brant and Helms Carotid Doppler for carotid artery stenosis Nl Doppler angle 40-60 degrees VA chart 2003 To detect slow flow: Decrease the PRF, use low wall filter, decrease Doppler angle, increase sampling area, lower frequency transducer Renal Doppler/Renal artery stenosis RI less than 0.8, elevated > 0.9 Main renal artery less than 200cm/sec, some say 150cm/s Nl RAR <3.5, if >, then stenosis may be >60% In RAS may see spectral broadening w/ or w/o flow reversal, absent diastolic flow may indicate stenosis >50% RI is not elevated is RAS, more commonly obstruction, ATN, etc… May be elevated in chronic RAS with CRI Liver length on ultrasound is measured saggittal R10length of the right lobe (VA), should be ≤ 15.5cm Caudate lobe is between IVC and portal vein on sagg ultrasound Left hepatic vein is seen on sagg US of left lobe 90% hemangiomas are hyperechoic w/o halo, most of the rest (“atypical hemangioma”) are hypo with hyper rim Gallbladder Fasting for at least 6hrs is recommended before exam, often can’t fast in ER cases Two major criteria: gallstones and sonographic Murphy’s Gallbladder wall thickness should be ≤ 3mm Common bile duct measured at porta hepatis should be ≤6mm up to 60yo, and thereafter increase by 1mm per decade (For example, upper limit of normal, in a 70yo is 7mm). Brant and Helms Main pancreatic duct ≤3mm Kidneys (L>R) (VA chart) Female:9.5-12cm Male: 10-12.5cm Pyloric Stenosis (CHLA measurements) Recent literature suggests an “olive” is palpable less than 50% of the time, and maybe this is generous (before reported as 80%) Baby is fed glucose water, and imaged w/ US. If pylorus is not seen due to overdistended antrum, place NGT Normal pylorus opens Q15min Post-operative pylorus is difficult to eval. Normal values Muscle wall thickness ≤3.5mm Pyloric channel length ≤16mm Pylorospasm: Muscle wall thickness or pyloric length measurements may overlap those accepted as positive for hypertrophic pyloric stenosis, to differentiate, image over a long period of time Journal of Ultrasound in Medicine, Vol 17, Issue 11 705-711, 1998 If there is suspicion for pyloric stenosis and the measurement values are at the upper limits of normal and close follow-up is usually recommended (us. w/in a few days) Germinal matrix/intraventricular hemorrhage in neonates I - subependymal and/or GM (less than 10% vent. volume), seen in caudothalamic groove II- intraventricular, less than 50% vent. volume (normal sized vent), overall good prog. III - IV, w/ > 50% of vent. volume (vent enlarged), 20% mortality IV-(some say this is now better termed hemorrhagic venous infarction, is Grade III w/ extent into cerebral hemispheres, 90% mortality Upper limits of normal abdominal/limb vasculature (VA chart) Abdominal aorta: 3cm Common iliac artery: 2cm Femoral artery:1.5cm Popliteal artery:1.0cm TIPS malfunction (VA chart) Peak shunt velocity <60cm/s or >200cm/s Change in peak shunt velocity >50cm/s MPV velocity <30cm/s Renal transplant rejection Donor ureter usually implanted to superolateral wall of bladder, donor renal vessels us. anastomosted to native iliac vessels Hypertrophy and increased C/M differentiation are normal findings, Dilatation confined to the renal pelvis/mild hydronephrosis may not be clinically significant, but should be followed and an etiology should be sought Lymphocoeles at 4-8 weeks after Sx, in 15% of Txs Urine Leak/urinoma often presents w/in 3w at UVJ, no septations unless infected Normal main renal artery velocity < 200cm/s Arteries have low resistance w/ brisk upstroke and nl RI from 0.6 to 0.8 ATN occurs in some extent in all cadaveric Txs, most common need for dialysis 2 weeks post transplant, non-specific imaging, may have increased RI Acute rejection-occurs in up to 40% in first few weeks Chronic rejection-occurs after 3 mos, most common cause of late graft loss Obstruction is rare, but when it occurs it is likely due to ischemic fibrosis at UVJ Renal artery thrombosis, very rare, seen in first month, most common from acute rejection w/ retrograde thrombosis, no renal flow on US Renal artery stenosis-most common vascular complication in up to 10% in first year, may be segmental w/ chronic rejection, PSV >200cm/s w/ turbulence, parvus tardus distally Venous thrombosis-acute pain, renal swelling, oliguria in first week, absent venous flow and reversal of flow in the renal artery Renal vein stenosis-spectral Doppler w/ 3-4X increased velocity across a select region indicates a hemodynamically significant stenosis http://www.learningradiology.com/lectures/facultylectures/usrenaltransplantppt_files/fra me.htm Hepatic transplant rejection Rejection in 50-70% of patients at some point after Tx Nl in first few days post-op: rapid upward systolic stroke but no diastolic flow Acute rejection-often nl imaging, may be heterogenous or decreased liver echotexture Conversion of hepatic vein waveform from triphasic to monophasic (not specific), but concerning Chronic rejection-increased periportal echogenicity Biliary complications as well as vascular thrombosis/stenosis-most w/in 3 months Often biliary strictures are at the anastomotic site HA thrombosis (#1 vascular comp.)—no flow at porta hepatic, hypoechoic blotchy infarcts seen at liver edges, may cause biliary ischemic strictures, the bile ducts in a Tx’d liver depend solely on HA blood, impending thrombosis may be seen with absence of diastolic flow, then dampened diastolic peak, then total loss of waveform HA stenosis-at anastomotic site-flow w/ spectral broadening/turbulence, distal tardus parvus, flow ≥ 2m/s at anastomosis (abn), look for pseudoaneurysm at anast. site Nl waveforms in right and left hepatic arteries = patent proper HA Biloma most common at anastomotic site. Biloma may also be caused by HA thrombosis. Portal Vein/IVC thrombosis/stenosis-rare, focal narrowing at anastomosis is nl Clinical sonography, a practical guide, Sanders et. al. 2006 http://radiographics.rsna.org/content/23/5/1093.full.pdf Nl portal vein diameter 8-12mm Portal vein thrombosis cavernous transformation Normal hepatic duct diameter3-6mm (some say 4mm is ULN), right and left hepatic ducts should be ≤2mm DVT The veins should be compressible to 2mm or less (each vein wall counts for 1mm), tech must perform compression if able, be careful w/ augmentation maneuvers in patients w/ a known DVT Normal testis measures about 5x3cm Thyroid Nl each lobe: 4x2x2 cm Isthmus: 4-6mm 10-40% of adult population has thyroid nodules Increased size of thyroid lesion does not correlate w/ increasing prob. of malignancy 4-33% of thyroid CA undergoes cystic degeneration Ultrasound may detect 2-3mm lesions Most often benign: eggshell calcification and a thin echolucent halo Features suggestive of malignancy: solid, hypoechoic, irregular margins, fine punctuate calcifications (papillary), note that although cancer is hypoechoic in >70% of cases, a hypoechoic nodule is statistically more likely to be benign A cold nodule with hypervascular periphery and hypovascular center suggests benignity except in Hashimoto’s thyroiditis, when a cold nodule is internally hypervascular, the chance of malignancy increases Only about 4% of thyroid cancers are hot 85% of thyroid nodules are cold, and 85% of cold nodules are benign Papillary carcinoma is more often less vascular than normal thyroid tissue Mets can be diffuse or focal. Focal mets often go to the lower pole and appear as solid hypoechoic well-defined non-calcified nodule, most cancer presents as a solid nodule Caution should be taken as to not rely on ultrasound features alone for malignancy http://emedicine.medscape.com/article/385301-imaging Pediatric hip Alpha angle normally >60o Graf Ultrasound Classification of Acetabula: Type I Normal acetabular morphology. Alpha angle greater than 60 degrees. Type II a Child less than three months of age with borderline acetabular morphology and nondisplaced femoral head. Alpha angle is 50 to 60 degrees, consistent with immature acetabulum. Vast majority of these children progress to normal by three months of age (96%). Repeat scanning at three months of age may be done to confirm this expected progression to normal. Type II b Same as II a, but child is greater than three months of age. These children need intervention, since by three months, immature acetabulum should no longer be present. Type II c Acetabulum is deficient with nondisplaced femoral head (becomes II d when decentering femoral head is present). Type III Type IV Alpha angle is less than 49 degrees. Intervention is required regardless of age. Acetabulum is deficient. Alpha angle is less than 49 degrees with subluxation of femoral head. Intervention is required regardless of age. Dislocated hip. Intervention warranted. A. The normal anatomy visualized on a pediatric hip ultrasound should include the following: 1. Cartilaginous femoral head. 2. Bony acetabulum. 3. Ilium, ischium, and pubic bones 4. Labrum. 5. Femoral head ossification centers if child is older. B. The abnormal anatomy visualized on a pediatric hip ultrasound could include the following: 1. Subluxation or dislocation of the femoral head. 2. Abnormal alpha angle. 3. Abnormal thickness of labrum. 4. Presence of pulvinar. 5. Asymmetry of the ossification centers. http://uvmrads.org/protocols/31-ultrasound/29-pediatric-hip-ultrasound-protocol-ddh Vesicoureteral Reflux VUR Grade I – reflux into non-dilated ureter Grade II – reflux into the renal pelvis and calyces without dilatation Grade III – mild/moderate dilatation of the ureter, renal pelvis and calyces with minimal blunting of the fornices Grade IV – dilation of the renal pelvis and calyces with moderate ureteral tortuosity Grade V – gross dilatation of the ureter, pelvis and calyces; ureteral tortuosity; loss of papillary impressions The younger the age of the patient and the lower the grade at presentation the higher the chance of spontaneous resolution. Most (approx. 85%) of grade I & II cases of VUR will resolve spontaneously. Approximately 50% of grade III cases and a lower percentage of higher grades will also resolve spontaneously http://en.wikipedia.org/wiki/Vesicoureteral_reflux, http://radiographics.rsna.org/content/20/1/155/F10.expansion.html (pictures) Neuro (inc. all spine, head and neck) (inc. all spine, head and neck) UCI MRI acute stroke technique: Most common (LASH/non-LASH, MRA head, MRA neck): the head and MRA head are done without contrast. Axial images are termed “the partitions.” Then a bolus of gad is given and the MRA neck is done. Then the 3D reconstructions with gadolinium are made. From the neck images, the MRA head 3D reconstructions are made, and added back to the MRA head study. So the second set of MRA head images are with gadolinium and reconstructed from the MRA of the neck. Please note if MR perfusion (uses gad) for stroke is to be performed, you cannot do MRA of the neck with gad, and you cannot do a contrast brain MRI (if the ordering clinician is on a “seek and destroy” mission, and not necessarily looking for stroke). You can do the MRA neck without gad, but it is often very noisy. However, I have seen a few turn out very well. >6 hrs ischemia bright on FLAIR Enhancement with high T2 in stroke pt suggests infarction less than 2w old Some NIR believe that if the stroke is not yet bright on FLAIR the brain is salvageable and not yet infarcted Predental space 3mm adult, 5 mm child Note normal pseudosubluxation of the cervical spine in a child (C2/C3 (40% of children), less at C3/4)—anterior displacement of C2 on C3 of ≤4mm, occurs in flexion only, reduces in extension http://www.wheelessonline.com/ortho/pseudosubluxation_of_the_c_spine http://www.orthobullets.com/spine/2048/pseudosubluxation-of-the-cervical-spine Prevertebral soft tissue normal values (get inspiratory extension views-unless severe trauma) ≤ 3mm at C3, be concerned if ≥ 5mm Adult: ≤ 7mm at C2, and ≤ 22mm at C6 Child: ≤ 14mm at C6 Note SCIWORA in a child (us. less than 8yo) (abn. not seen on plain films or CT) SCIWORA is due to the ligamentous flexibility and elasticity of the immature spine, greatest in C-spine, often will not present w/ deficit (maybe just initial tingling) until 48hrs later, get MRI http://www.wheelessonline.com/ortho/sciwora_syndrome_spinal_cord_injury_w_o_radio logic_abnormality Best temporal bone anatomy (I found e-anatomy to not be that great): http://headneckbrainspine.com (images a bit grainy) http://www.radsmd.com/coronalCTatlas3.htm (slow) Transtentorial herniation (3 types): Uncal-dilated pupil, duret, ips hemip, later eye down and out, C/L homo hemianop Central-suprasellar cistern Upward cerebellar-quadrigeminal cistern, us. from cerebellar mass/edema Flexion injury Narrowed disc space above involved vertebral body “Basal cisterns” (4) -suprasellar -paramesencephalic -ambient -prepontine Epiglottis Imaging may be false negative early in disease Obtain an extension radiograph w/ mouth closed Adult, normal thickness 3-5mm, >7mm is 100% sens/spec for epiglottitis, aryepiglottic fold > 4.5mm suspicious For all age patients highly specific and sensitive for epiglottitis: Epiglottic width/C3 vertebral body width > 0.5 Epiglottic width/epiglottic height > 0.6 Radiologic diagnosis of epiglottitis: Objective criteria for all ages. Rothrock et al. Ann Emerg Med. Sept.1990 Lateral radiograph of the neck demonstrates and enlarged epiglottis (red arrow) and thickening of the aryepiglottic folds (yellow arrow). There is also reversal of the normal lordotic curve in the cervical spine and slight dilatation of the hypopharynx. From learningradiology.com There is no completely reliable approach to the injured cervical spine http://www.ajnr.org/cgi/content/full/28/9/1819 Atlantooccipital dissociation (more common in children) --avoid C-spine flexion-Atlanto occipital condyle distance should be less than 5mm (some say 4mm or less) regardless of age Wackenheim’s Clival Line (picture below) The odontoid should be tangential to or below the line that extends along the dorsal clivus Harris Method Line along the posterior C2 body should be less than 12mm from basion and the basion to the tip of the dens should be less than 12mm (this is the BDI, basion to dens interval) http://w3.cns.org/university/pediatrics/Spinks_chapter_figures73108_Page_07.jpg Powers Ratio BC/OA If >1, then anterior subluxation, Ratio<0.55 is posterior translation http://www.wheelessonline.com/ortho/atlantooccipital_disassociation http://4.bp.blogspot.com/_zmXoIvqjSJw/TFb1TkM1SII/AAAAAAAAAKM/20bxSBgC S10/s400/%E5%9C%96%E7%89%871.jpg ICA dissection is most common in the cervical portion, 2cm from bifurcation (35-50yo) In intracranial ICA dissection, most patients are less than 30yo PAC-man/crescent sign—best seen on axial T1W The dark part is flow, bright part is the dissection intramural hematoma http://radiographics.rsna.org/content/28/6/1711/F29.expansion http://radiographics.rsna.org/content/28/6/1711.full Spinal enhancement Fibrosis in the spine enhances. A recurrent disc does not, unless it is imaged late. There may be enhancement around a synovial cyst (us. at facet) and type I Modic changes Spinal infection sparing the disc space = TB Disc space biggest at L4/5 Lines for determining basilar invagination Chamberlain’s (line from posterior hard palate to posterior lip of foramen magnum, abnormal if dens >3mm above line) http://www.raddaily.com/data/articles/neuro/skullchamberlain.jpg MacGregors (easier to use, line from posterior hard palate to base of occiput, abnormal if dens is >4.5mm above line) http://www.raddaily.com/whitepaperarticle.php?articleTitle=Lines+of+the+Skull+Base Pathologic spinal fracture—pathologic(met) vs non-path Paravertebral soft-tissue masses and infiltration of posterior elements are the most reliable signs of a malignant fracture. Pathologic fractures show more homogeneous replacement of the bone marrow. “Fluid sign” rarely occurs in metastatic fractures, in addition intravertebral air w/in the compressed vertebrae is more often associated with avascular necrosis benign compression, osteolytic mets (low T1, high T2) blastic (low T1, low T2). “Pseudocapsule” may be seen post-gap w/ spinal met http://radiology.rsna.org/content/225/3/730.full Bright on SWI phase images = iron/blood, dark=calcium, this is only good for small lesions and is unreliable in the basal ganglia. Also look for clot, on SWI phase or MAG images particularly in the Sylvian fissure. Make sure to check the coronal images for any extra-axial bleed in trauma patients. Best sequences for cord lesion: axial GRE and sagittal PD Measure neural foramina in L-spine on saggittal and C-spine on axial. Use GRE and/or T2. Note GRE artifacts often cause measurements to be incorrect. Subdural hematoma W/L: 90/40 or 90/50 Internal capsule blood supply Largest supply-> MCA M1 lenticulostriate (LTS) Anterior--LTS, recurrent Huebner off ACA (inf. half) Genu--LTS Posterior--LTS, ant choroidal off ICA (inf. half) Cerebellar tonsils > 5mm below the foramen magnum (ectopic tonsils) and/or pointedChiari I Sella turcica AP Length of 17mm Depth 13mm Width 15mm Investigate if depth exceeds length Cranial arteries/Circle of Willis segments—some segments are variable and there is disagreement on the number of segments for certain arteries ICA (4, some give up to 7) http://www.meddean.luc.edu/lumen/MedEd/neuro/neurovasc/navigation/iccerv.htm C1-cervical C2-petrous C3-cavernous C4-supraclinoid (gives rise to ophthalmic a., pcomm, ant. Choroidal MCA (3 or 4) (MCA is not part of COW) M1-horizontal (sphenoidal) M2-insular (Sylvian) M3-opercular M4-cortical (terminal) Some sources state there is no M4, and then the M3 is termed the “cortical” segment (M2/M3 segment more commonly bifurcates than trifurcates into main trunks (middle trunk not always present) ACA (5) A1-from ICA to AComm A2-from Acomm to bifurcation into pericallosal and callosamarginal, or to junction of rostrum and genu of CC, ascending A3-pericallosal (may anastomose w/ PCA), ascending, extends around genu until sharp posterior turn A4- horizontal, above CC, A4 and A5 separated by plane of coronal fissure A5- horizontal, above CC Practical neuroangiography. Pearse Morris, 2007. (Pericallosal) http://www.meddean.luc.edu/lumen/MedEd/neuro/neurovasc/navigation/peri.htm Callosomarginal often branches off of pericollasal (8=pericallosal, 9= callosomarginal) http://www.mdconsult.com/das/book/body/222994964-2/0/1611/59.html Best seen on a coronal view-the paired pericallosal arteries are midline, and give rise to the callosomarginals which deviate laterally then run anteriorly and are more dorsal than the pericallosal Recurrent a. of Huebner is variable in origin, most commonly off proximal A2, lateral A Comm or distal A1 segment PCA (3 or 4) P1-from basilar tip to PComm (part of COW) P2- courses laterally around midbrain to junction w/ post. choroidal a. P3-runs through lateral quadrigeminal cistern and divides into P4 P4-cortical branches P1 and P2 strokes cause infarcts in thalamus and midbrain. P3 and P4 cause cortical strokes (some sources say there is no P4, just P3) Some call P4 “cortical branches” Vertebral artery (4) V1-take off of subclavian to transverse foramen at C5 or C6 V2- from foramen transversarum of C5 or C6 to C2 V3- from C2 foramen transversarum, loops around posterior arch of C1, passes between atlas and occiput V4-intracranial segment from where is enters the dura to basilar a. Vertebral artery most commonly dissects at C1/C2 region (Segment 3), us. in young healthy individuals following minor trauma or spontaneous Most common neurological symptoms correlate w/ Wallenberg (lateral medullary syndrome), also HA, nuchal pain etc… Watershed infarct—most commoncortical border zone infarcts) between ACA and MCA, also MCA and PCA, less common“internal watershed” involves corona radiate/centrum semiovale (poorer prognosis) Us. from severe unilateral carotid stenosis, prolonged hypotension (bilateral), or carotid dissection (unilateral), aortic dissection (bilateral) http://www.radiologyassistant.nl/en/484b8328cb6b2 Internal Watershed—us. bilateral from hypotension, sometimes looks like “rosary/string of pearls” configuration http://radiopaedia.org/cases/iwi01 http://jnnp.bmj.com/content/78/8/907/F1.large.jpg http://missinglink.ucsf.edu/lm/ids_104_cns_injury/response%20_to_injury/Watershed.ht m Chronic watershed ACA/MCA and MCA/PCA http://www.mdconsult.com/das/article/body/2229908052/jorg=journal&source=&sp=21537242&sid=0/N/672988/1.html#f08001175005 Usually unilateral watershed is from severe carotid stenosis Flexion/extension plain film: Translation greater than 3mm in either flex or ext = considered unstable Cavernoma,= cavernous hemangioma, popcorn, dark ring Blood stages on MRI (T1/T2) Hyperacute --hours oxyHgb (low/high) Acute --days deoxy (low/low) w edema Subacute early --days4-7 IC metHgb (high/low) Subacute late --weeks EC metHgb (high/high) Chronic--years hemosiderin (low/low) slit, or greater than 2 weeks Blood is not bright on T1 until after one week Modic T1 T2 I low high (edema) II high high (fat) III low low (sclerosis) Klippel-Feil Syndrome (3 things)-short neck, low dorsal hairline, restricted neck mobility from segmentation anomaly w/ synostosis of cervical vertebrae often w/ block cervical vertebrae, decreased number cervical vertebrae. Often w/ other congenital anomalies and Sprengel’s deformity of scapula. K-F deformity only involves C-spine abn. #1parotid tumor is benign mixed/pleomorphic adenoma, #1 malignant is mucoepidermoid #1 submandibular is Warthin tumor Normal pressure hydrocephalus is a clinical diagnosis, may see narrow convexity sulci, transependymal edema, dilatation of temporal horns/atria/ventricles out of proportion to atrophy, T2 aqueductal flow void “flow void sign/hyperdynamic/pulsatile flow” = dark signal on T2 in the aqueduct http://emedicine.medscape.com/article/342827-imaging http://radiopaedia.org/articles/normal-pressure-hydrocephalus Hydrocephalus look for bowing/dilatation of the recesses of the third ventricle DVA was formerly “venous angioma”, see DVA look for associated cavernomathis is what causes problems (bleeds etc.) Sinovertebral nerve—cause of pain from annular tear Conus ends at L1/2 us. by 3 months of age Axial midbrain: Cerebral peduncles antcollici post to thisquad plate cistern post to this All holoprosencephaly have absent septum pellucidum TB of spine affects body>disc Spinal stenosisAP diameter cervical spine <12mm, <11.5 mm lumbar—these mm are debatable, a canal <10mm is usually considered stenosis. Some say AP diameter 1115mm=relative stenosis, less than 10mm on saggittal absolute stenosis ALL rupturesag MRI, look at anterior disc annulus, and for STS “Mastoid antrum” is largest mastoid air cell Aditus ad antrum is from the epitympanic recess or attic to the mastoid antrum Branchial cleft cyst, type 2 is most common Pharyngeal tonsils = adenoids, most superiorhttp://en.academic.ru/pictures/enwiki/71/Gray994-adenoid.png Palatine tonsil at level of uvula http://www.aafp.org/afp/2002/0101/p93.html BVORVOG + ISS = SS SOV is medial to superior rectus Dermoid/epidermoid most common congenital orbital lesion Holoprosencephaly(cortical mantle, no thalamic cleavage = fused thalami) vs hydrancephaly(no cortex) vs severe hydro (interhemispheric fissure) Toxo= diffuse parenchymal calcs Chest/Cardiac Pneumothorax increases with expiratory views Traumatic pseudoaneurysm vs normal ductus bump Ductus bump is smooth and convex w/o acute margins, both at isthmus region Aortic Dissection Stanford Type A = ascending only Stanford Type B = descending only DeBakey Type I = ascending + descending DeBakey Type II = ascending only DeBakey Type IIIa = descending only DeBakey Type IIIb = descending, including abdominal ***Asc. Requires surgical repair, asc. only is 60% of total Thoracic Aortic Aneurysm Recommendations, elective repair of asc aorta ≥ 5.5cm and desc at ≥6.5cm, and possibly at smaller size if other comorbidity (bicuspid valve, Marfan’s etc..). Generally, for both asc. and desc. ≥4cm = aneurysm The main pulmonary artery diameter should be <3cm on CT. Pulmonary artery diameter ≥ 3.5cm,95% chance of pulmonary HTN, mean pulmonary artery pressure for HTN is around 20mmHg Right lung segments (10 bronchopulmonary segments) A PALM Seed Makes Another Little Palm UPPER LOBE o o o apical posterior anterior MIDDLE LOBE o o lateral medial LOWER LOBE o o o o o superior medial basal anterior basal lateral basal posterior basal Left lung segments remember, the lingual is part of the left upper lobe (us. 8 bronchopulmonary segments-somewhat debated) ASIA ALPS (upper/lower) UPPER LOBE o o o o apical posterior anterior superior lingular inferior lingular LOWER LOBE o o o o superior posterior basal lateral basal anterior medial basal Lung collapse LOBAR COLLAPSE Right--> Upper—superior medially, Golden S Middle--over right heart border, triangle on lateral Lower--over right hemiD, posterior triangle over posterior sulcus on lateral Left--> Upper--anteriorly, luftschikle, may look like UL haziness, look for volume loss (lingulamedially/heart border, ant. triangle above oblique fissure): Lower--medial posterior behind heart, posterior triangle over posterior sulcus on lateral http://emedicine.medscape.com/article/353833-imaging (pics) http://www.radiology.co.uk/srs-x/tutors/collapse/left.htm Centrilobular pattern often spares the lung periphery Stages of sarcoid Chest films in sarcoidosis have been classified into four stages: 1. 2. 3. 4. Bilateral hilar lymphadenopathy Bilateral hilar lymphadenopathy + pulmonary disease Only pulmonary disease Irreversible fibrosis 1-2-3- lymph node sign, small nodules along fissures (specific), small perilymphatic nodules in mid and upper lung Persistent peripheral lung consolidationCOP/BOOP, eosinophilic pneumonia BOOP is COP when there is no known cause UIP—fatal, progressive, extensive fibrosis, IPF accounts for more than 60% of cases, UIP is IPF when there us no known cause Hypersensitivity pneumonitis Mosaic pattern, spares lung bases, centrilobular nodules http://www.radiologyassistant.nl/en/46b480a6e4bdc Upper lobes Cystic fibrosis EG Ankylosing spondylitis Allergic alveolitis/chronic extrinsic alveolitis Sarcoid Berylliosis Granulomatous disease (post-primary TB), histoplasmosis, sarcoid granulomas/micronodules Radiation Rx (dep. on site) Pneumoconiosis PMF Lower Lobes Mets LAM Scleroderma RA Dermatomyositis Lymphangitic spread Asbestosis IPF Tuberculosis Primary TB: Initial infection with consolidation, adenopathy and pleural effusion. Secondary TB: Post-primary or reactivation TB. This is the reactivation of the original infection. Usually located in the apical segments of upper lobes with cavitation Endobronchial spread: May occur in both primary and secondary TB, when the infection is not contained. Hematogenous spread (miliary TB): May occur in both primary and secondary TB, when the infection is not contained. http://www.radiologyassistant.nl/en/46b480a6e4bdc Miliary pattern--cocci, tb, thyroid mets Radiation pneumonitis seen 4-12w post therapy Radiation fibrosis after 6-12months post-therapy, stabilizes at 2yrs http://radiographics.rsna.org/content/20/1/83.full Post-pneumonectomy lung First 24hrs after sxair only Fills with fluid at rate of 2 rib spaces/day Hemithorax is 80-90% filled w/ fluid at end of 2w Should be completely opacified at around 4mo Maximum shift toward pneumonectomy side at 6-8mo, return to midline of previously shifted mediastinum is highly sensitive for late complication Air w/ in resection cavity after prior opacification suggests bronchopleural fistula (drop in fluid level by >2cm) or infection From learningradiology.com The right paratracheal stripe should be less than 4mm. If enlarged is most often due to regional adenopathy. #1 aortic arch anomaly is nl left arch w aberrant right subclavian #1 right aortic arch anomaly is right arch with aberrant left subclavian, both can cause dysphagia Fleischner criteria for pulmonary nodules Good to remember-->less than 4mmonly high risk for primary needs a FU at 12mo Fleischner Criteria Nodule Size (mm) Low risk patients High risk patients Less than or equal to 4 No follow-up needed. Follow-up at 12 months. If no change, no further imaging needed. >4 - 6 Follow-up at 12 months. If no change, no further imaging needed. Initial follow-up CT at 6 -12 months and then at 18 - 24 months if no change. >6 - 8 Initial follow-up CT at 6 -12 months and then at 18 - 24 months if no change. Initial follow-up CT at 3 - 6 months and then at 9 -12 and 24 months if no change. >8 Follow-up CTs at around 3, 9, and 24 months. Dynamic contrast enhanced CT, PET, and/or biopsy Same at for low risk patients Note.—Newly detected indeterminate nodule in persons 35 years of age or older. Low risk patients: Minimal or absent history of smoking and of other known risk factor. High risk patients: History of smoking or of other known risk factors. Information taken from www.radswiki.net Emphysema Centrilobular (#1)-proximal bronchioles, upper zones, smoking Panlobar-lower zones, @1AT exac by smoking Paraseptal-adjacent to pleural surface and fissures, smoking, subpleural blebs Giant cell looks similar to Takayasu Polyarteritis nodosa and aneurysms of renal a's Reverse bat wing: COP, chronic eosinophilic PNA, vasculitis, aspiration, contusion, infarction MSK Transcapular view is the “Y view” “Rim sign”-seen in posterior shoulder dislocation, distance from anterior glenoid to medial border of humeral head >6mm Normal AC joint 3-8mm with smooth continguous border inferiorly (<5mm vertical step-off), widening usually from FOOSH Normal coracoclavicular distance 11-13mm Acromioclavicular Joint Separation Grades Type Anatomy Radiographic findings Prognosis Stretching of AC ligament I AC joint is stable Only seen on stress views of injured and uninjured shoulders=widening of AC joint No instability Widening of AC joint but a normal coracoclavicular distance May require arthroplasty Sprain CC ligament intact Partial or complete rupture of AC ligament II Subluxation III IV Posterior V Inferior Partial, but not complete, disruption of CC ligament Stress films may still be required to demonstrate widening of both AC joint and CC space Disruption of both AC and CC ligaments Widening of both the AC and CC spaces on routine erect film AC and CC ligaments disrupted but coracoacromial ligament remains intact Distal end of clavicle lies inferior and posterior to acromion seen best on axillary view AC and CC ligaments disrupted Coracoacromial ligament remains intact Sternoclavicular separation occurs as well Marked widening of both the AC and CC space Sternoclavicular dislocation Internal fixation VI Distal end of clavicle displaced inferiorly and lodges in biceps and coracobrachialis m.muscles Distal end of clavicle comes to lie inferior to acromion This is chart is from learningradiology.com Normal scapholunate interval is less than or equal to 2mm, >2mm-suspicious, if ≥ 4mm, most would call scapholunate dissociation Physis closed-giant cell, chondroblastoma Fibrous dysphasia “ground glass” with bowing/other deformity Erosive osteoarthritis- gull wing, osteopenia Always say chondrmyxoid fibroma w/ NOF ACL runs lateral to medial Exostosis--rule of 10's PVNS--> knee, hip, elbow, ankle The sustentaculum tali is a projection off the calcaneus Foot fractures often missed: Anterior process of calcaneous and cuboid Myositis ossificans hot on bone scan, zonal phenomenon w/ peripheral rim calcification to help ddx from malignancy Malignant ST tumor--MFH/fibrosarc (#1), then liposarc JRAcarpal erosions, capitate the most MRI knee Look at saggittal PD and T2 are best for ligament and meninscal tears Medial knee-tibia is like a golf tee, lateral tibia is like a hockey stick Posterior meniscus should be bigger than anterior portion Tear should extent to articular surface Magic angle = when a structure is oriented 55 degrees to main magnetic field, T2 times increase 100X (increase bright signal artifact mainly seen in inf. patellar tendon and rotator cuff, ankle) Hip columns Most common injury is isolated posterior column Least common is isolated anterior column Line a–a1 establishes anterior (AC) and posterior (PC) columns. Anterior (AW) and posterior (PW) walls lie lateral to line b–b1 http://www.ajronline.org/cgi/content/full/182/6/1367 Calcaneal fracture Bohler’s angle is normally greater than 20 degrees, and less than 20 suspect calcaneal fracture http://www.joint-pain-expert.net/images/calcaneus_fracture2.jpg Salter Harris (SALTR = slipped, above, lower, through, raised) I- epiphyseal separation, physeal widening, ex. SCIFE II- metaphyseal + epiphyseal, most common SH fracture III – physis and epiphysis, ex. Tillaux, intra-articular IV – epiphysis, physis, metaphysic, intra-articular V – epiphysis crushed, us. NOT detected acutely AVN stages (2 diff’t classifications): Ficat femoral head AVN Stages Stage Clinical Features Early 0 Preclinical 0 I Preradiographic + II Precollapse + Transition: Radiographs 0 0 Diffuse Porosis, Sclerosis, Cysts Flattening, Crescent Sign III Collapse IV Osteoarthritis ++ +++ Broken Contour of Head Certain Sequestrum, Joint Space Normal Flattened Contour Decreased Joint Space Collapse of Head Enneking Osteonecrosis stages Stage I II III IV V VI Pain None None Occasional Limp Continuous Severe Radiographs Slight increased density Reactive rim Crescent sign Step off flattening Collapse Deformed Calcaneus is epiphyseal equivalent, intraosseus lipoma or unicameral bone cyst (common at metaphysis) Patella is largest sesamoid Pes anserinus (anteromedial proximal tibia) “Say Grace before SupTer” (Sartorius, gracilus, semitendinosis) Hand w sublaxation distally, think SLE or Jacoud (post RF) Hair on end skull-Thalessemia Cotton wool skull with thickening of iliopectineal line (ant column) is Pagets Chronic villonodular synovitis is giant cell tumor of tendon sheath Hemophilia-cystic changes on both sides of joint Malignant ST tumor--retroperitoneal, large, heterog T2 signal Fibrous histiocytoma is second most common ST tumor after lipoma T score < -2.5 = osteoporosis >2cm=NOF, <2cm fibrous cortical defect Morton neuroma darkT1 and T2, enhances brightly Hardware lucency = 2mm or more Adamantinoms/osseous fibrous dysplasia Hemophiliac arthropathy, sclerotic joint sn w no osteopenia, pseudotumor of hemophilia You do not need gadolinium for MRI in osteomyelitis Nidus (lucent area w/ surrounding reactive sclerosis)osteoid osteoma, osteoblastoma, LCH(EG), osteomyelitis (inc.Brodie’s) Fallen fragment unicameral bone cyst with pathological fracture, may be confused w/ sequestrum Sequestrum osteomyelitis (inc.Brodie’s) LCH (EG), metastases, radiation necrosis, fibrosarcoma, or FILE (Fibrosarcoma, Infection, Lymphoma, EG), may mimic osteoid osteoma, “button” in skull w/ difft differential Fluid/fluid level ABC, telangiectatic osteosarcoma, giant cell, chondroblastoma, fractured simple bone cyst, myositis ossificans, synovial sarcoma, mets (renal/lung) The following link offers a very good list of MSK differentials: http://home.caregroup.harvard.edu/departments/radiology/residency/teaching/differential/MSKDD x.doc GI Appendicitis Normal appendix in adult diameter ≤6mm, wall ≤3mm Look for inflamed adjacent fat, fluid, appendecolith Portal venous gas/air vs pnemobiliapneumobilia is normally > 2cm central from liver capsule, portal venous gas is usually more fine, linear, branching, may extend to liver capsule Liver Segments (8, 4a/b) http://www.radiologyassistant.nl/en/4375bb8dc241d ABDOMINAL TRAUMA INJURY GRADING SCALE ( from AAST)-inc. kidneys Spleen (either/or)—SPLENIC TRAUMA GRADING SCALE-Grade 1 -subcapsular hematoma <10% of surface area -capsular tear <1cm deep Grade 2 -Subcapsular hematoma 10-50% SA -intraparenchymal hematoma <5cm diameter -laceration 1-3 cm deep, not involving vessels Grade 3 -Subcapsular hematoma >50% SA or expanding and ruptured -subcapsular or parenchymal hematoma -Intraparenchymal hematoma >5cm or expanding -Laceration >3cm deep, or involving vessels Grade 4 -involves hilar vessels with devascularization >25% of spleen Grade 5 -shattered hilar vascular injury Liver---HEPATIC TRAUMA GRADING SCALE Grade 1 (either/or) -Subcapsular hematoma (SH) <1cm -Liver Laceration (LL) <1cm deep Grade 2 -SH or LL 1-3 cm Grade 3 -SH or LL >3cm Grade 4 -LL or SH >10cm Lobar destruction devascularization Grade 5 -Global destruction or devascularization Grade 6 -Hepatic avulsion Pancreas---PANCREATIC TRAUMA GRADING SCALE Grade 1 (either/or) -Minor contusion/hematoma w/o ductal injury -Superficial laceration w/o ductal injury Grade 2 (either/or) -Major contusion/hematoma w/o ductal injury or tissue loss -Major laceration w/o ductal injury or tissue loss Grade 3 -Laceration w/ distal transection or parenchymal injury w/ ductal injury Grade 4 -Proximal (to right of the SMV) transection or parenchymal injury, not involving the ampulla Grade 5 -Massive disruption of the pancreatic head -Advance one grade for multiple injuries up to Grade III Kidney (either/or)---RENAL TRAUMA GRADING SCALE Grade 1 -Hematuria with normal imaging studies -Contusions -Nonexpanding subcapsular hematomas Grade 2 -Nonexpanding perinephric hematomas confined to the retroperitoneum -Superficial cortical lacerations less than 1 cm in depth without collecting system injury Grade 3 -Renal lacerations greater than 1 cm in depth that do not involve the collecting system Grade 4 -Renal lacerations extending through the kidney into the collecting system -Injuries involving the main renal artery or vein with contained hemorrhage -Segmental infarctions without associated lacerations -Expanding subcapsular hematomas compressing the kidney Grade 5 -Shattered or devascularized kidney -Ureteropelvic avulsions -Complete laceration or thrombus of the main renal artery or vein http://radiographics.rsna.org/content/21/suppl_1/S201.figures-only In the groin region, the iliac vein is medial to the artery Upper limits of normal for adult lymph node stations (short axis)-non-thoracic specific Short gastric 6mm Retrocrural 6mm Retrocaval 6mm Paracardiac 8mm Mediastinal 10mm Gastrohepatic ligament 8mm Upper paraoartic 9mm Portocaval 8-10mm Portahepatic 7mm Lower paraaortic 11mm Axillary, neck, groin 15mm Please note that there is some discrepancy regarding these measurements, but the more important is to note which stations have the lower cut-offs (retrocrural, etc..) Malignant nodes may appear more round as opposed to oval and have loss of the normal fatty hilum Check out RECIST v1.1 http://radiology.ucsd.edu/radres/Education/journal_club/RECIST%201_1%20nodes.pdf http://radiology.rsna.org/content/180/2/319.full.pdf+html Duodenal ulcers>%w/ H. pylori, anterior and superolateral duodenal bulb Gastric ulcerslesser curvature/antrum, benign ulcers us. on posterior wall Distal left posterior wall of esophagusmost common location for Boerhaave syndrome Gastrografin (not used in babies/children) often given for esophageal perforation suspicion due to rapid absorption, however if it gets in lungs causes necrotizing pneumonia due to high osmolarity (barium can cause fibrosis), if Gastrografin study is negative but suspicion remains a barium swallow is then indicated, if barium gets into peritoneal cavity may cause peritonitis/granulomatous rxn , that is why Gastrografin is used in cases of suspect bowel perforation Fatty Liver CT HU difference of less than 18 between liver and spleen equals fatty liver w IV contrast Normal liver 50-75 HU non con Liver HU on non-con less than 40 mod/severe hepatic steatosis Large caudate PBC, PSC, Budd-Chiari, caudate is generally large in cirrhosis Ciliated hepatic foregut cyst--bright on T1, segment 4 only, <3cm Epithelial hemangioepthelioma Retroperitoneal fibrosis-autoimmune Sprue increase risk of SB lymphoma Tuberus sclerosis lymphangioma Infarction of bowl--lack of enhancement Carcinoid- TI, rectum Type 1 choledochal cyst, most common, ALL are at risk of developing cholangioCA Type III = choledochocoele Ameboema right colon BsC cholangitis and cancer PSC mild IHBD dilatation Santorini seal for symptomatic panc divisum Normal alpha fetal protein (AFP) level is <10mg/ml. 40% w/ liver cancer have normal AFP GU Adrenal adenoma, fast washout, greater than 50% at 10 min Size > 4cm usually cancer, also can do MR chemical shift #1cause of adrenal hemorrhage is septicemia, w/ AH, insufficiency is rare Urethral Injury Anterior urethra=bulbar and penile, Posterior = Memb-UG, P DIAGNOSED BY RGU Type 1- puboprostatic ligament rupture, prostate and bladder apex displaced superiorly, post urethra stretched/intact, Type 2-above UGD in prostatic segment, contrast in extraperitoeneal pelvis Type 3-membranous disrupted, most common type, tear extends down through the UGD, may include proximal bulbous, contrast in extraperitoeneal pelvis and perineum (contrast extrav us. at or above AND below UGD) Type 4-bladder neck injury extending to the anterior urethra Type 4A- bladder base injury with periurethral extravasation Type 5-Pure anterior urethral *CT does not allow distinction between Type II and III injuries, but may be suggestive drawing from http://myradnotes.wordpress.com/category/trauma/ Bulbous urethra is from external sphincter to penoscrotal junction Extraperitoneal bladder injury is most common Beware that sometimes extraperitoneal can look like intraperitoneal and sometimes there is a component of both (intra req. sx repair) Bladder injury Type 1- contusion (pt may have hematuria, but nl CT) Type 2- intraperitoneal rupture, sx emergency, direct blow to distended bladder ruptures dome Type 3- interstitial bladder injury, serosa intact, no extrav Type 4- Extraperitoneal rupture (80-90%); more common w/ pelvic fxs, rupture is us. due to laceration by bone fx frag, contrast into perivesicle space so called “molar tooth appearance” 4A-simple 4B-complex Type 5- Combined bladder injury http://radiographics.rsna.org/content/20/5/1373.full Prostate Nl dimension (StatDx) 3cm craniocaudal 4cm wide 2cm AP More precise = volume = 0.523 x length x width x thickness (1cc prostate tissue = 1g) Normal is about 20g in young man, enlargement is >40g StatDx Prostate CA is us.T2 low signal//hypoehoic in peripheral posterior prostate, but not always Prostate Specific Antigen There is no specific normal or abnormal PSA level, and there is no optimal level recommended for biopsy. It is nonspecific and may be elevated in BPH, UTI’s, prostatitis, etc.. However, the higher the PSA or if there is high velocity (increase by >0.75ng/ml in one year), or a low percent free PSA (<10%), the more likely the chance of cancer. Historically, 4ng/ml has been the upper limits of normal for PSA, but a lower cutoff (2.5ng/ml) should be used in younger patients. From published reports: normal prostate on exam + PSA <4 = 15% chance of cancer, PSA from 4-10 = 25% chance, and PSA >10 = 67%. Many believe that in prostate cancer patients with a PSA <10, there is less likelihood of capsular penetration or skeletal metastases http://www.webmd.com/prostate-cancer/guide/psa http://radiology.rsna.org/content/243/1/28.full Some use age-specifc PSA cut-offs: Age 40-50: 0-2.5 ng/ml Age 50-60: 0-3.5 Age 60-70: 0-4.5 Age 70-80: 0-6.5 Most common seminal vesicle lesion is a cyst Bosniak 1-simple, water density 2-thin septa, fine wall calc, <3cm, 18% chance of CA 2F- min enh of thin septa, min septal thickening, modular calc, totally intrarenal <3cm high density non-enh well-marginated 3- thickened irregular wall/septal enh, 33% 4-enhancing ST component, 92% A renal/ureteral stone/calculus >4mm is more unlikely to pass on its own. 90% of stones 4mm or less will pass on their own. The normal urinary bladder wall is ≤3mm when the bladder is well-distended The nl testis is 5 by 3 cm Nuclear Medicine HIDA Conjugated Bili should be less than 4 mg/dL, may give more radiopharm if jaundiced Patient should have fasted for at least 4hrs and less than 24hrs. If patient fasted <4hr or >24hr may not see GB Fasting >12 (or some say > 24hrs) and no GB seen, can give CCK Once radiotracer is seen in the bowel, morphine (0.04mg/kg/IV)can be given to aid in GB visualization Not seeing the GB on HIDA at 60 min-#1 cause= acute chole, other causes: improper fasting as above, acute acalculous chole, chronic chole, hepatic insuff., hyperalimentation, alcoholism, pancreatitis, hyperbilirubinemia, opioid abuse Nl study: Clear blood pool:15min EH bile ducts at:10-15min SB: 30-60min GB: <1hr Acute chole- non-visualization of the GB by 60 min. when bowel is seen Acalculous chole (10%) High M &M, failure to visualize GB, along w/ low EF (<35%) post-CCK Low EF post-CCK, high PPV for chronic acalculous chole, persistent GB activity w/o washout, us. see GB if wait long enough Chronic acalc> acute acalc Acute-Non-vis of GB at 1hr w/ vis of SB, morphine mat help in dx by decreasing false + Chronic alcalculous cholecystitis-GB EF <40%, high PPV Please note that HIDA cannot reliably distinguish calculous vs. acalculous and correlation is needed w/ ultrasound or CT Note sphincter of Oddi spasm/dysfunction Rim sign: complicated/gangrenous chole DDx’ing neonatal hepatitis vs biliary atresia-> may want to pre-treat with phenobarbital (5mg/kg/24h PO for 5 days prior to study) V/Q Perfusion imaging may be done first, and if no abnormalities are seen, the ventilation portion may be cancelled in some instances (ex. pregnancy) Modified PIOPED Criteria HIGH PROBABILITY SCAN ≥80% chance of PE o 2 or more large mismatched segmental defects or equivalent moderate/large defects with a normal x-ray o Any perfusion defect substantially larger than radiographic abnormality INTERMEDIATE PROBABILITY SCAN 20-79% o Multiple perfusion defects with associated radiographic opacities o Greater than 25% of a segment and less than 2 mismatched segmental perfusion defects with Normal radiograph. One moderate segmental One large or two moderate segmental One large and one moderate segmental Three moderate segmental o Difficult to characterize as high probability or low probability LOW PROBABILITY SCAN <20% o Nonsegmental defects-small effusion blunting costophrenic angle, cardiomegaly, elevated diaphragm, ectatic aorta o Any perfusion defect with substantially larger radiographic abnormality o Matched ventilation and perfusion defects with normal chest radiograph o Small subsegmental perfusion defects NORMAL o No perfusion defects *"Segmental Equivalent" Sizing: The moderate segmental defect is counted as 0.5 of a large segmental defect (two moderate sized segmental defects are therefore equivalent to one large segmental defect). All moderate and large defects can be than added up to result in total segmental equivalent units. (Example: 3 moderate segmental defects and 1 large = 2.5 segmental equivalents) *Note a solitary triple match in the mid or upper lung zone has a very low likelihood, while one in the lower lobe is intermediate *“Stripe sign” –very low probability *Pleural effusion w/ no other defect-very low probability *One moderate mismatch w/ no CXR abn. may be placed in high group if patient has cancer (controversial) Excellent resource: http://www.svhrad.com/DigLib/Pulmonary/Lung%20Scan/Interpretation%20of%20VQ% 20Scans%20for%20PE.htm GI bleed Most commonly use tagged RBC (other choice is SC—faster, but a little less sensitive) No patient prep Image 1min/frame for 1-2hrs False + = free tech, varices/hemangioma on blood pool, penile/uterine blush False - = low bleeding rate, venous bleed, tech. failure, cessation of bleed Nuclear cardiac stress test (VA) Stress images are over rest http://tomography.files.wordpress.com/2007/10/unlabelledmedyaleedu.gif Look at perfusion defects, wall motion, EDV, EF and raw data for artifacts (motion, gut) due to filtered backprojection Most commonly use sestamibi (have to use high stress dose/low rest dose) or thallium (more radiation, but different energies that don’t overlap with Tc-99, (so don’t need the high/low) Nl LVEDV is us. less than 120mL, but based on height/weight, Nl EF is about 50-75% Transient ischemic dilatation (TID), seen in stress images in patient’s with 3-vessel disease Ga> Indium for discitis Indium WBC don't see kidney, see bones. Octreotide see kidneys Peds—for more complete info please see the Cleveland Clinic training modules https://www.cchs.net/pediatricradiology/ Congenital heart disease (CHLA) Left atrial enlargement-mitral stenosis >regurg Width of main PA should equal supraaortic tracheal width Sinus venosus asd, papvc, vein must be redirected to left atrium ASD increased pulmonary vascularity, most close by 2-3mos VSD most common shunt defect assoc with syndromes and trisomies AV canal = endocardial cushion defect, in complete there is primum ASD, inlet VSD and common AV valve VSDs and hyperinflation PDAs increase size of LA and LV LA enlargement in VSD not ASD VSD in first few weeks, ASD in childhood or adolescence Coarctation more common in adults, short segment juxtaductal type Bicuspid aortic v in 85% of coarcts, often w poststenotic dilatation of asc aorta Intercostals #1-3 from thyrocervical trunk from the carotids HLHS has PDA and ASD and 75% w coarctation, does not present for a few days (3-5), right heart is dilated, Norwood (first stage is BT shunt-right subclavian artery to right PA), Glenn shunt (cavopulmonary), Fontan (fenestration between IVC and RA-later closed Round pna --> S. Pneumonia Neuroblastoma calcs, but no fat, Wilms can have fat, Nb more often goes to bones, from adrenal, ages 2-4 Wilma goes to lungs, renal vein to right atrium, Beyond 10 yrs old wilms=RCC NEC seen after 72hrs Submucosal->bubbly pneumatosis, subserosal->linear Blount’smedial depression of tibia Duodenal hematoma is child abuse Hutch diverticulum needs repair PIE = barotrauma, first 2-3day in neonate with ARDS Lymphangiomatosis/asia goes to bone/lung Chylothorax Big heart first few days = Ebsteins , tricuspid atresia Newborn kidney upper limit is 4cm MCDK look for UPJ obst on other side Discoid miniscus easily tears, seen in child Hepatoblastoma (tumor thrombus in kids is Wilma or hepatoblastoma) vs hemangioendothelioma (vascular) Permeative bone lesionEwing, LCH, lymphoma, osteosarcoma Peribronchial cuffing interstitial edema Surfactant deficiency/ARDS is babies less than 36 weeks and less than 2.5 kg TTN peaks at 24hrs higher w/ c-section or precipitous vag delivery, clears from periphery to center and top to bottom, treatment is CPAP Intussusceptions between 6 mo and 2 yrs, small bowel intussusception is surgical only Meconium aspiration, air block phenomenonPTX Ileal duplication is #1 duplication cyst Resect esophageal duplication due to ectopic gastric mucosa and higher risk of cancer Only tubular duplication cysts communicate with lumen Intralobar sequestration is 75%, venous drainage is through pulmonary system to LA, m=f, diagnosed after 20 yrs, hemoptysis, pneumonia Extralobar left CPA, males, can present as an adrenal mass, most symptomatic in first 6 months, 60% have other congenital anomalies Most sequestration ix excised to decrease infection rate Normal thymic echotexture=liver Valves and coronary arteries go with ventricles in transposition Other Outpatient contrast reaction prophylaxis (2 main protocols) ONE 1. Prednisone 50mg PO at 13hr, 7hr, and 1hr before exam plus 2. Diphenhydramine (Benadryl) 50mg IV, IM, or PO 1 hr before exam -ORTWO 1. Methylprednisolone (Medrol) 32mg PO at 12hr and 1hr before exam plus 2. Diphenhydramine (Benadryl) 50mg IV, IM, or PO 1 hr before exam Emergency Premedication IV steroids are NOT EFFECTIVE when administered less than 6hrs before exam Chose ONE of the following 3 protocols. Listed in order of decreasing desirability 1. Methylprednisolone sodium succinate (Solu-Medrol) 40mg OR hydrocortisone sodium succinate (Solu-Cortef) 200mg IVq4h until contrast study required plus diphenhydramine 50 mg IV 1hr prior to contrast injection*** most desired protocol 2. Dexamethasone sodium sulfate (Decadron) 7.5 mg or betamethasone 6.0 mg IV q4h until contrast study must be done in patent with known allergy to methylprednisolone, aspirin, or non-steroidal anti-inflammatory drugs, especially if asthmatic. Also diphenhydramine 50 mg IV 1 hour prior to contrast injection. 3. Omit steroids entirely and give diphenhydramine 50 mg IV. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/contrast_manual/Full Manual.aspx#page=9 Contrast extravasation Inflammatory response may not peak until 1-2d after extravasation Be careful in patients with atherosclerotic disease and children Monitor extravasation in dorsum of hand or feet even more carefully Always monitor for compartment syndrome (#1), and skin ulceration Raise limb to level of heart and may use cold or warm compressNote that these have not been associated w/ any type of more rapid recovery Keep patient in radiology dept. until you are satisfied, no further reaction with occur If severe reaction, ER or emergent surgical consult http://www.acr.org/SecondaryMainMenuCategories/quality_safety/contrast_manual/Full Manual.aspx#page=17 PD long TR short TE MRI gad stays in system for 7hrs Frequency:readout:chemical shift The following is an excellent chart developed by Dr. Wu at the VA for the order of optimal imaging modalities for endocrine tumor/disorders