Expanding Spectrum of Ciliopathy beyond the Airway
advertisement
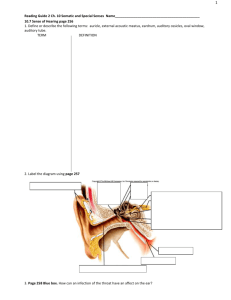
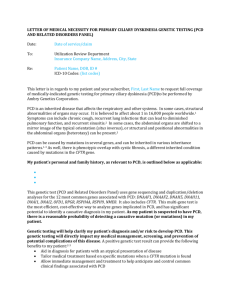
Expanding spectrum of ciliopathy beyond the airway Andrew Bush MB BS (Hons) MA MD FRCP FRCPCH Professor of Paediatric Respirology, Imperial School of Medicine at National Heart and Lung Institute; and Honorary Consultant Paediatric Chest Physician, Royal Brompton Hospital. Correspondence: Department of Paediatric Respiratory Medicine, Royal Brompton Hospital, Sydney Street, London SW3 6NP, UK. Tel: -207-351-8232 Fax: -207-351-8763 e mail:- a.bush@rbh.nthames.nhs.uk Abstract Primary ciliary dyskinesia (PCD)is characterised by chronic upper and lower respiratory tract infection, and in nearly 50% of cases, mirror image arrangement. This is the archetypal ciliary disease, but it is now clear that it is part of a wide spectrum. Clinical features now recogised as intrinsic components of PCD include heterotaxy and complex congenital heart disease, oesophageal disease and primary ciliary dyskinesia. It is dysfunction of motile cilia that is responsible for the clinical manifestations of PCD, but malfunction of primary and nodal cilia is also important. The complexities of ciliary structure and function are only beginning to be appreciated; primary cilia may have mechano- and chemosensory functions as well as possibly secretory, through the illunderstood process of intraflagellar transport. Dysfunction of nodal cilia is implicated in cystic disease in particular of the kidneys and liver. Ciliary dysfunction is important in the pathophysiology of retinitis pigmentosa, Jeune’s asphyxiating thoracic dystrophy, and complex neurodevelopmental, sketal and other multisystem syndromes. This review covers PCD, as well as acting as an introduction to the many complex conditions caused by underlying ciliary dysfunction. Keywords: cilia, heterotaxy, bronchiectasis, congenital heart disease, polycystic kidney disease, retinitis pigmentosa The initial description of ciliopathy was the triad of sinusitis, bronchiectasis and situs inversus (Kartagener’s syndrome). The structure and genetics of cilia, and the upper and lower airway manifestations of ciliopathy (primary ciliary dyskinesia, PCD) have been described in previous presentations and elsewhere [1,2]. It is clear that PCD is only the tip of the iceberg of ciliary diseases. The purpose of this presentation is briefly to review the standard manifestations of PCD; to review the expanding spectrum of other manifestations of PCD; and to discuss other diseases related to ciliary dysfunction. If nitric oxide was the molecule of the 1990s, cilia are clearly the structures of the new millennium. Nomenclature of the different types of cilia Primary cilia (which confusingly are not the root cause of PCD) are solitary structures widely distributed in epithelial cells. Their primary structure is nine outer doublets, but no inner pair. The structure may vary along the axoneme, and there may be regions with central singlets. They are probably mechano- or chemo-sensors, and are not motile. They arise from a proximal and distal centriole. They are found on the vast majority of non-mitotic cells in the body [3]. Nodal cilia overlap between primary and motile cilia. They are responsible for determining situs in the developing embryo [4]. They are structurally primary in type (no central pairs), but unlike other primary cilia, some are motile. There are also sensory cilia within the embryonic node. Motile cilia are responsible either for propelling unicellular organisms through liquids (e.g. chlamydomonas) or moving mucus along epithelial surfaces. These are the cilia which are abnormal in PCD. They are complex structure, with nine outer doublets and an inner pair, containing more than 200 proteins [5]. Key structures are the inner and outer dynein arms, which are mechanochemical ATPases, similar in function to myosin and kynesin, and radial spokes and nexin links. The complexity of these structures means that there are likely many PCD genes. Human locations of cilia are listed at http://members.global2000.net/bowser/cilialist.htm/; they are widely distributed in the plant and animal kingdoms. The human rods and cones of the retina, sperm tails and olfactory cells are related human structures. Intraflagellar transport In addition to the functions described above, the complex processes of intraflagellar transport are being discovered. The purpose of this complex process is not clear, but may relate to ciliary nutrition [6,7]. It has been suggested this may be a ciliary secretory function [8]. It is linked to ciliary signalling pathways via sonic hedgehog in particular [9], but this is also not well defined. ‘A’ and ‘B’ rafts are moved anterogradely to the ciliary tip, and retrogradely to the base of the cilia. Mutations in A and B raft genes lead to short, stumpy cilia. There is a link to Jeune’s asphyxiating thoracic dystrophy (below). PCD: airway manifestations The classical phenotype of PCD is of upper and lower airway disease, with, in around 50% of cases, mirror image arrangement. The presentation and diagnosis of PCD have been reviewed in detail [1,2], and are summarised in Tables 1 and 2 respectively. Absolutely essential in the diagnostic process is to ensure that ciliary abnormalities secondary to infection are not mis-diagnosed as PCD. If there is any doubt, and in atypical cases, testing should be repeated a few months later. Typically there are combinations of upper and lower airway disease; isolated cough is rarely due to PCD. The diagnosis is frequently delayed into adult life [10], probably because many of the symptoms (cough, rhinitis, chronic serous otitis media) are very common in otherwise normal children [11]. There is a spectrum; mild disease may be diagnosed in apparently well siblings after the finding of PCD in an index case [10]. This means that there is often substantial impairment of lung function [12]; stabilisation can be achieved [12, 13], but significant and sustained improvement is rare. Established bronchiectasis is frequently found in children diagnosed late. Thus diagnostic vigilance is essential, and this usually has to rely on a carefully focussed history and clinical examination. Treatment is empirical, and largely based on cystic fibrosis (CF) protocols. This is not logical, given the different pathophysiology (ciliary dysfunction versus airway surface dehydration [14]), and indeed, treatments such as rhDNase which are very effective in CF, may be useless or even harmful in other chronic chest conditions [15]. Lower respiratory tract treatment is by combinations of airway clearance techniques [13]; early on Staphylococcus aureus and Haemophilus influenza are common. Isolates of these orhanisms are treated with a 2-4 week course of an appropriate oral antibiotic such as Augmentin. Repeated isolates merit consideration of prophylactic antibiotics, and symptoms non-responsive to oral therapy are treated with intravenous antibiotic. Mucoid and nonmucoid strains of Pseudomonas aeruginosa and atypical Mycobacteris species are not usually seen until adult life. Most centres use eradication protocols for Pseudomonas similar to CF, and also use chronic suppressive nebulised antibiotics if infection has become established. Intravenous antibiotics are used as needed, usually a combination of an aminoglycoside and a third generation cephalosporin. The management of atypical Mycobacteria is complex in CF; there is even less evidence in PCD. The treatment of the upper airway complications is significantly different from what might be expected [16]. Secretory otitis media is treated conservatively – the placement of tympnostomy tubes almost invariably leads to prolonged otorrhea with no improvement of hearing. Long-term, improvement can be anticipated, and hearing loss is minimal [17]. If hearing is problematic in PCD patients, then a short period of the use of hearing aids may be needed, but these are usually able to be discarded in the teenage years. Sinusitis is also managed conservatively where possible. Nasal polyps are very rare in PCD, in my experience. The management of PCD has recently been reviewed in detail [1, 2]. PCD: more than just an airway disease The spectrum of PCD has been extended to include hydrocephalus (a rare manifestation), infertility, and heterotaxy and complex congenital heart disease [18]. Hydrocephalus is seen more commonly in animal models of PCD; there are cilia bathed in cerebrospinal fluid, but their function is not clear. Sperm tails may be immotile in men with PCD, but this is not inevitable [19]. There is said to be a higher prevalence of ectopic pregnancy in women with PCD due to immotility of cilia in the Fallopian tubes [20]. In terms of heterotaxy, a large series (n=337) of PCD patients [18], 46% had usual organ arrangement, 48% had mirror image, and 6% (21/337) had disorders of heterotaxy (including n=1 right isomerism with asplenia, n=11 left isomerism with polyspenia). Complex congenital heart disease was seen in 8 patients, and there was a 200-fold higher prevalence than normal of complex congenital heart diease in PCD with heterotaxy, an overall prevalence of one in fifty. Complex congenital heart disease was particularly common in the presence of outer dynein arm defects (especially DNAH1 and DNAI5). Therefore it is essential to remember PCD in the context of congenital heart disease with laterality disorder, and screen for PCD if there is the least suspicion of associated respiratory disorders. Taken together, the facts that nodal cilia are responsible for situs, and ciliary dysfunction affects cardiac structure, presumably due to motility effects during the development of the heart, one could speculate that other organ malpositions, in particular gastrointestinal malrotation, may be an effect of ciliary dysfunction. Indeed, malrotation is associated with right and left isomerism [21], and we have described malrotation and a gastrointestinal motility disorder in a cilipathy related condition, Jeune’s asphyxiating thoracic dystrophy (below). In this regard, the finding of disordered neural crest migration and Hirschprung’s disease in Bardet-Biedl syndrome lends support to the hypothesis that gastrointestinal motility disorders may in part be cilia related [22]. Another co-morbidity, which should prompt exclusion of PCD, is biliary atresia [23]. Although mild to moderate gastro-oesophageal reflux is common in many respiratory diseases, there seems to be an increased risk of really severe reflux, and other oesophageal disease, in PCD [24]. Whether there is an oesophageal motility disorder in PCD has yet to be determined. Spectrum of disorders of primary cilia As might be expected given their wide distribution, there are many manifestations of disorders of primary cilia. There is a wide spectrum of liver and kidney cystic syndromes [25], of varying disease severity, and retinal involvement, anosmia, obesity, ataxia and other central nervous system abnormalities, and skeletal dysplasias are all described as part of this spectrum. Many syndromes are rare and beyond the scope of this manuscript, the more important will briefly be described below and see Table [26]. Renal manifestations of ciliopathy include adult and juvenile onset polycystic kidney disease, and nephronophthisis. The mechanisms linking ciliary dysfunction and cyst formation are unknown, although the WNT signalling pathway is implicated [27]. There is also a fascinating link between kidney disease and bronchiectasis [28]. Polycystin is found in the human respiratory epithelium, although its function there is not known. In a comparison between nearly 100 adult polycystic kidney patients and 100 other renal disease patients, the prevalence of bronchiectasis was 37% in the polycystics versus 1: in the non-cystic kidney patients, p=0.0022. However, 13% prevalence of bronchiectasis in the control group is much higher than could be expected by chance. It has been suggested that this might be related to the newly described primary cilia in airway smooth muscle cells [29]. Whatever the explanation, it is suggested that bronchiectasis should be excluded in any renal patient with respiratory symptoms. Cilia connect the inner and outer retinal photoreceptor neurones. There are many syndromes which include retinitis pigmentosa, with involvement of other organ systems common. We are following a family in which the father has retinitis pigmentosa and the two children have PCD. A number of similarly poly-phenotypic kindreds have been described [30-2]. Jeune asphyxiating thoracic dystrophy is an autosomal-recessive chondrodysplasia characterized by short ribs and a narrow thorax, short long bones, inconstant polydactyly, and trident acetabular roof. It is closely related to the short rib polydactyly syndrome (SRP) type III, which is a more severe condition characterized by early prenatal expression and lethality and variable malformations. Jeune’s asphyxiating thoracic dystrophy has been known to be associated with abnormalities of situs. Recently, Jeune’s was found to be associated with abnormalities in the IFT80 gene on chromosome 3 [33]. This is a poorly understood gene, which is concerned in intraflagellar transport. More recently, a Jeune’s gene to was mapped to chromosome 11q14.3q23.1 in a 20.4 Mb region and identified as the cytoplasmic dynein 2 heavy chain 1 (DYNC2H1) gene [34]. DYNC2H1 is a component of a cytoplasmic dynein complex and is directly involved in the generation and maintenance of cilia. Polydactyly, renal degeneration and renal cysts have also been described in this condition. We have described a child with Jeune’s syndrome, malrotation and gut dysmotility, hypothesising that these last two features may be a feature of ciliopathy [35]. Ciliopathy: the future Clearly, ciliary disease has come a long way from the days of Kartagener! Ciliopathy is a rapidly expanding multisystem condition. We are good at investigating the function of motile cilia in the respiratory tract, but it cannot be assumed that anormalities in primary and nodal cilia are necessarily related to motile cilia. Indeed, patients with PCD and motile sperm have been described, underscoring the variability within cilia-like structures. We urgently need new tests of ciliary function, particularly primary cilia. In the meantime, when seeing a child with a multisystem disease, it is worth asking ‘could this be another ciliopathy?’ Table 1. Clinical manifestations of PCD Age Classical Manifestations Antenatal Mirror image arrangement on antenatal ultrasound (not diagnostic) Newborn period Respiratory distress Rhinitis Positive family history Childhood Atypical ‘asthma’ Chronic productive cough Bronchiectasis Severe gastro-oesophageal reflux Rhinosinusitis Chronic secretory otitis media After diagnosis in a relative As for childhood Male infertility Ectopic pregnancy Adulthood Non-Classical Manifestations Heterotaxy on antenatal ultrasound Complex congenital heart disease on ultrasound Heterotaxy Complex congenital heart disease Biliary atresia Oesophageal disease Table 2. Summary of diagnostic testing for PCD Screening for PCD Ciliary function Ciliary structure Ciliary culture [42] Genetic studies [5] Immunohistochemistry [43] Saccharine test [36] Radionuclide scanning [37] Nasal nitric oxide (less well established in young children) [38-40] Ciliary beat frequency and pattern [2] Transmission electron microscopy [2, 41] Only needed if clinical doubt Many genes as yet undiscovered Only limited availability Table 3: The common associations of clinical features in five ciliary dysfunction syndromes [44, 45] Disease Retinitis pigmentosa Renal cystic disease Polydactyly Situs inversus/isomerism Mental retardation/developmental delay Hypoplasia of the corpus callosum Dandy-Walker mallformation Posterior encephalocele Hepatic disease Total number of phenotypes in each disorder * In mice. BBS √ √ √ √ √ √ √ √* √ 8 OFD1 √ √ Senior-Loken √ √ √ √ √ √ √* 5 √ 5 Meckel Joubert √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ √ 9 9 References 1. Bush A, Chodhari R, Collins N, Copeland F, Hall P, Harcourt J, Hariri M, Hogg C, Lucas J, Mitchison HM, O'Callaghan C, Phillips G. Primary ciliary dyskinesia: current state of the art. Arch Dis Child. 2007; 92: 1136-40. 2. Barbato A, Frischer T, Kuehni CE, Snijders D, Azevedo I, Baktai G, et al. Primary ciliary dyskinesia: a consensus statement on diagnostic and treatment approaches in children. Eur Respir J. 2009; 34: 1264-76. 3. Wheatley DN, Wang AM, Strugnell GE.Expression of primary cilia in mammalian cells, Cell Biol. Int. 1996; 20: 73–81 4. Nonaka S, Shiratori H, Saijoh Y, Hamada H. Determination of left-right patterning of the mouse embryo by artificial nodal flow. Nature. 2002; 418: 96-9. 5. Leigh MW, Pittman JE, Carson JL, Ferkol TW, Dell SD, Davis SD, Knowles MR, Zariwala MA. Clinical and genetic aspects of primary ciliary dyskinesia/Kartagener syndrome. Genet Med. 2009; 11: 473-87. 6. Sloboda RD. Flagella and cilia: the long and the short of it. Curr Biol. 2009; 19: R1084-7. 7. Silverman MA, Leroux MR. Intraflagellar transport and the generation of dynamic, structurally and functionally diverse cilia. Trends Cell Biol. 2009; 19: 306-16. 8. Baldari CT, Rosenbaum J. Intraflagellar transport: it's not just for cilia anymore. Curr Opin Cell Biol. 2010; 22: 75-80. 9. Tran PV, Haycraft CJ, Besschetnova TY, Turbe-Doan A, Stottmann RW, Herron BJ, et al. THM1 negatively modulates mouse sonic hedgehog signal transduction and affects retrograde intraflagellar transport in cilia. Nat Genet. 2008; 40: 403-10. 10. Coren ME, Meeks M, Buchdahl RM, Morrison I, Bush A. Primary Ciliary Dyskinesia (PCD) in children - age at diagnosis and symptom history. Acta Paediatrica 2002; 91: 667-9. 11. Bush A, O’Callaghan C. Primary ciliary dyskinesia. Arch Dis Child 2002; 87: 363-5. 12. Ellerman A, Bisgaard H. Longitudinal study of lung function in a cohort of primary ciliary dyskinesia. Eur Respir J. 1997; 10: 2376-9. 13. Noone PG, Leigh MW, Sannuti A, et al. Primary ciliary dyskinesia: diagnostic and phenotypic features. Am J Respir Crit Care Med. 2004; 169: 459-67 14. Matsui H, Grubb BR, Tarran R, Randell SH, Gatzy JT, Davis CW, Boucher RC. Evidence for periciliary liquid layer depletion, not abnormal ion composition, in the pathogenesis of cystic fibrosis airways disease. Cell. 1998; 95: 1005-15. 15. Wills PJ, Wodehouse T, Corkery K, et al. Short-term recombinant human DNase in bronchiectasis. Effect on clinical state and in vitro sputum transportability. Am J Respir Crit Care Med 1996; 154: 413–417. 16. Hadfield PJ, Rowe-Jones JM, Bush A, Mackay IS. Treatment of otitis media with effusion in children with primary ciliary dyskinesia. Clin Otolaryngol 1997; 22: 302-6. 17. Majitha A, Fong J, Hariri M, et al. Hearing outcomes in children with primary ciliary dyskinesia – a longitudinal study. Int J Pediatr Otorhinolaryngol 2005; 69: 1061–4. 18. Kennedy MP, Omran H, Leigh MW, et al. Congenital heart disease and other heterotaxic defects in a large cohort of patients with primary ciliary dyskinesia. Circulation 2007; 115: 2814–2821 19. Jonsson MS, McCormick JR, Gillies CG, Gondos B. Kartagener's syndrome with motile spermatozoa. N Engl J Med. 1982; 307: 1131-3. 20. Halbert SA, Patton DL, Zarutskie PW, et al. Function and structure of cilia in the fallopian tube of an infertile woman with Kartagener’s syndrome. Hum Reprod 1997; 12: 55–8. 21. Ditchfield MR, Hutson JM. Intestinal rotational abnormalities in polysplenia and asplenia syndromes. Pediatr Radiol. 1998; 28: 303-6. 22. Tobin JL, Di Franco M, Eichers E, May-Simera H, Garcia M, Yan J, et al. Inhibition of neural crest migration underlies craniofacial dysmorphology and Hirschsprung's disease in BardetBiedl syndrome. Proc Natl Acad Sci U S A 2008; 105: 6714-9 23. Gershoni-Baruch R, Gottfried E, Pery M, Sahin A, Etzioni A. Immotile cilia syndrome including polysplenia, situs inversus, and extrahepatic biliary atresia. Am J Med Genet. 1989; 33: 3903. 24. Gemou-Engesaeth V, Warner JO, Bush A. New associations of primary ciliary dyskinesia syndrome. Pediatr Pulmonol 1993; 16: 9-12. 25. Ong AC, Wheatley DN. Polycystic kidney disease--the ciliary connection. Lancet. 2003 ; 361: 774-6. 26. Tobin JL, Beales PL.The nonmotile ciliopathies. Genet Med. 2009; 11: 386-402. 27. Lancaster MA, Louie CM, Silhavy JL, Sintasath L, Decambre M, Nigam SK, Willert K, Gleeson JG. Impaired Wnt-beta-catenin signaling disrupts adult renal homeostasis and leads to cystic kidney ciliopathy.Nat Med. 2009; 15: 1046-54 28. Marthin JK, Mortensen J, Pressler T, Nielsen KG. Pulmonary radioaerosol mucociliary clearance in diagnosis of primary ciliary dyskinesia. Chest. 2007; 132: 966-76. 29. Sieck GC, Qian Q. Characterization of primary cilia in human airway smooth muscle cells. Chest. 2009; 136: 561-70 30. Alessandri JL, Cartault F, Brayer C, Cuillier F, Rivière JP, Ramful D, Gubler MC. Renal cystic dysplasia, paucity of bile ducts, situs inversus, bowing of the femora in two siblings in the Reunion Island: a ciliopathy? Clin Dysmorphol. 2009; 18: 209-12 31. Moore A, Escudier E, Roger G, Tamalet A, Pelosse B, Marlin S, et al. RPGR is mutated in patients with a complex X linked phenotype combining primary ciliary dyskinesia and retinitis pigmentosa. J Med Genet. 2006; 43: 326-33 32. van Dorp DB, Wright AF, Carothers AD, Bleeker-Wagemakers EM. A family with RP3 type of X-linked retinitis pigmentosa: an association with ciliary abnormalities. Hum Genet. 1992; 88: 331-4. 33. Beales PL, Bland E, Tobin JL, Bacchelli C, Tuysuz B, Hill J, Rix S, Pearson CG, Kai M, Hartley J, Johnson C, Irving M, Elcioglu N, Winey M, Tada M, Scambler PJ. IFT80, which encodes a conserved intraflagellar transport protein, is mutated in Jeune asphyxiating thoracic dystrophy. Nat Genet. 2007; 39: 727-9. 34. Dagoneau N, Goulet M, Geneviève D, Sznajer Y, Martinovic J, Smithson S, et al. DYNC2H1 mutations cause asphyxiating thoracic dystrophy and short rib-polydactyly syndrome, type III. Am J Hum Genet. 2009; 84: 706-11 35. Hall T, Bush A, Fell J, Offiah A, Smith V, Abel R. Ciliopathy spectrum expanded? Jeune syndrome associated with foregut dysmotility and malrotation. Pediatr Pulmonol. Pediatr Pulmonol. 2009; 44: 198-201 36. Canciani M, Barlocco EG, Mastella G, et al. . The saccharin method for testing mucociliary function in patients suspected of having primary ciliary dyskinesia. Pediatr Pulmonol 1988; 5: 210–14 37. Marthin JK, Mortensen J, Pressler T, Nielsen KG. Pulmonary radioaerosol mucociliary clearance in diagnosis of primary ciliary dyskinesia. Chest. 2007; 132: 966-76. 38. Karadag B, James AJ, Gultekin E, Wilson NM, Bush A. Nasal and lower airway level of nitric oxide in children with primary ciliary dyskinesia. Eur Respir J 1999; 13: 1402-1406. 39. Baraldi E, Pasquale MF, Cangiotti AM, Zanconato S, Zacchello F. Nasal nitric oxide is low early in life: case study of two infants with primary ciliary dyskinesia. Eur Respir J. 2004; 24: 881-3. 40. Stehling F, Roll C, Ratjen F, Grasemann H. Nasal nitric oxide to diagnose primary ciliary dyskinesia in newborns. Arch Dis Child Fetal Neonatal Ed. 2006; 91:F233. 41. Escudier E, Couprie M, Duriez B, Roudot-Thoraval F, Millepied MC, Prulière-Escabasse V, Labatte L, Coste A. Computer-assisted analysis helps detect inner dynein arm abnormalities. Am J Respir Crit Care Med. 2002; 166: 1257-62. 42. Jorissen M, Willems T, Van der Schueren B, et al. Ultrastructural expression of primary ciliary dyskinesia after ciliogenesis in culture. Acta Otorhinolaryngol Belg 2000; 54: 343–56. 43. Fliegauf M, Olbrich H, Horvath J, et al. Mislocalization of DNAH5 and DNAH9 in respiratory cells from patients with primary ciliary dyskinesia. Am J Respir Crit Care Med 2005;171:1343–1349 44. Harris PC. Genetic complexity in Joubert syndrome and related disorders. Kidney Int. 2007; 72: 1421-3 45. Adams NA, Awadein A, Toma HS. The retinal ciliopathies. Ophthalmic Genet. 2007; 28: 11325.