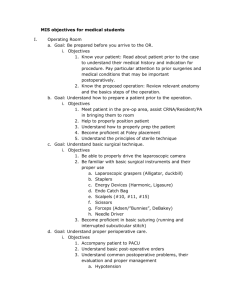
Rotation Specifics - Pediatrics House Staff
advertisement

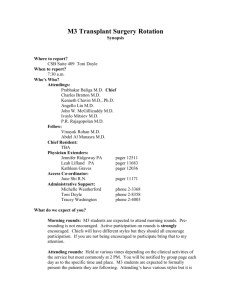
ROTATION SUMMARY GREEN TEAM & GREEN/RED NIGHT FLOAT Rotation Contacts and Scheduling Details Rotation Director: John Kerner, M.D. 750 Welch Road, Suite 116 pager: 1-3078 e-mail: jkerner@stanfordmed.org Administrator: Carmen Kimberling Carmenk@stanford.edu (6500 723-5070 Introduction The pediatric gastroenterology core rotation provides an opportunity for the resident to develop an understanding of the pathophysiology, clinical manifestations, and management of complex common and unusual disorders of the gastrointestinal tract, liver, and pancreas. Emphasis will be placed on the performance of a detailed and focused history and physical examination and the interpretation of laboratory, imaging studies, and G-I procedures (e.g., upper endoscopy, colonoscopy). Following completion of the rotation, residents will be able to initiate initial evaluation and management of these complex patients. Weekly Schedule - Inpatient Time Monday Pre-round 0700-0800 Morning Report 0800-0830 or 8 -9 GI/Liver Mtg 750 Welch, Ste 116 0830 ROUNDS 900 Tuesday Pre-round Morning Report Wednesday Pre-round Morning Report Thursday Pre-round Morning Report ROUNDS ROUNDS ROUNDS Friday Pre-round Grand Rounds (8:00-9:00) ROUNDS 11-1200 Patient Care Patient Care Patient Care 1200-1300 1300-1800 1700 Conference Patient Care Sign-out Conference Patient Care Sign-out Conference Patient Care Sign-out Weekly Schedule – Outpatient Monday Tuesday 8:00-9:00 am 8:00-8:30 am G-I/Liver Morning Report Meeting 750 Welch Rd. Suite 116 Wednesday 7:30 am – 8:30 am 1st Weds. each month Multidisciplinary Conference with Radiology and Peds Surgery …………………. Patient Care Chairman’s Rds Conference Patient Care Sign-out Patient Care Conference Patient Care Sign-out Thursday 8:00-8:30 am Morning Report Friday 8:00-9:00 am Grand Rounds 9 am – noon G-I Clinic 9 am – 12 noon Consults/ Directed Reading 8:00-8:30 am Morning Report 9:00 am – 12:00 pm G-I Clinic Inpatient Consults/Directed Reading Inpatient Consults/ Directed Reading …………………… 10 am - 12 noon+ Nutrition Support Last updated 6/10 Rounds Admin Conference room (basement LPCH) Noon Conference Noon Conference Noon Conference Noon Conference 12:00 pm – 1 pm G-I Teaching Seminar/ Path Conference once a month 1:00 pm – 5:00 pm G-I Clinic 1:00 pm – 5:00 pm G-I Clinic G-I Clinic (SCVMC)* 1:00 pm – 5:00 pm G-I Clinic …………………… 1:00 pm – 5:00 pm G-I Clinic 1st and 3rd Thursday of each month: 1:30 pm – 5:30 pm G-I Clinic (PAMF)** *Attending: Dr. Manuel Garcia/Dr. Missy Hurwitz. The GI clinic at SCVMC can accommodate one additional physician (Fellow or Resident) per session. When the Fellow is scheduled to be at VMC, residents should attend GI Urgent Clinic. Residents are responsible for asking the Fellow his/her schedule for VMC at the start of the rotation. **Attending: Dr. Dorsey Bass + 11-1 on the 2nd Wednesday of each month Rotation Specifics Orientation Residents should receive sign-out before beginning the rotation so they are well versed with the patients on the first day. Interns are expected to arrive at the hospital with enough time to pre-round on their patients before Morning Report. Your supervisors will arrive by 7am on Intern Switch Day to help orient you to the service. The Senior Resident on the Team should hold a brief session on the first day of the rotation to discuss how Rounds will be conducted and expectations for presentations, pre-rounding, notes and interaction with medical students and attendings. Rounds The Green team is comprised of the Gastroenterology and Liver service and each team typically has their own Fellow and Attending; rounds are conducted independently. The Green team is composed of an intern, supervising junior resident and physician assistant. The Senior Resident leads rounds. During the weekdays, the team is expected to walk round to see patients and discuss the plan with the family and the nursing staff. Patient distribution is as follows: The Transplant PAs primary responsibility is to the surgical services and surgical patients. If 2 PAs are on service and available they should be able to cover both the transplant surgical and medical patients up to 16 (dependent on surgical acuity). -Exceptions to above: If both PAs are required in the operating room or if the combined transplant surgical/medical service >8pts with one PA sick/PTO/conference/in OR the residents or fellows will cover the post transplant medical patients. When combined GI/pre transplant census is high (>10pts) the intern will cap at 10, the junior resident will take on 2 additional patients, and patients above that will go to PAs(pre txp) and/or fellows(GI). The PAs should be responsible for any of those patients they take on for the entire day or longer if necessary until the census decreases. They will primarily take on pre transplant patients who have completed the evaluation process and remain hospitalized or those that are readmitted post evaluation. When the team census is > 12 and the PA’s are unable to take on the remainder of patients (due to their patient load or if large volume of GI patients), the GI fellows and attendings will assist the residents in completing those Last updated 6/10 work assignments that involve large time commitments with low learning potential (ie discharge preparation and paper-work, etc). -In times of low census for the combined GI/Liver team, to maximize the learning experience the intern will have a minimum of 5 patients to include the post transplant readmits (especially if surgical census is high). Patient placement is as follows: PRE TRANSPLANT ADMISSIONS: o Please admit them to the LIVER TXP service, not GI. Please activate the Liver or Small Bowel transplant evaluation plan which will help you with the labs needed for work up. You do not need to repeat labs that have already been obtained at an outside facility EXCEPT HIV and blood type(2 are required but only 1 must be done here if already performed at outside hospital). ALL patients need echos regardless of presence of murmur unless one has been obtained at outside facility. Only obtain consults from services as needed based on patient’s PMH. The PA will serve as the liaison between the Green Team and the surgical Transplant team. They will ensure all the required tests and studies are ordered for transplant evaluation. If an incoming evaluation is known ahead of time they will initiate the order set for the Green team. POST TRANSPLANT READMISSIONS: o The PA will admit and activate the order set for any post transplant patient that arrives to the floor prior to 1600. If staffing/timing allows, the PA will perform the H&P on ER or clinic patients prior to admission, but if not, will initiate order set and the PM resident will verify meds/diet and activate the order set. Please admit under the LIVER TXP service. Activating the post txp readmit plans (liver in place, SB to follow soon) will save you time since most of the medications and standard labs are part of the plan. The Green team is not responsible for surgical patients and should defer all calls to the transplant fellow/attending if they are contacted regarding these patients when the transplant PA is not available. Clinic GI clinic is held Monday and Thursday mornings and every afternoon. Interns will be exposed to a balanced variety of outpatient management issues by the completion of the rotation. The GI Clinic operates like other traditional clinics. The resident will take the initial History and Physical then present that patient to the Attending. The Attending and resident will then see the patient together and the resident will be responsible for dictating the management plan. Residents are encouraged to keep track of the patients they see in clinic and follow-up on the outstanding laboratory results. Also, residents should “sign-out” all patients seen in Urgent Clinic to the Fellows as they will follow-up lab studies on these patients. Residents are expected to see patients with all types of diagnoses and in various stages of treatment. It is not practical nor beneficial from an educational perspective to seek out only new diagnoses. Pagers The Green Team will have a team text pager and phone to facilitate communication. Sign-out, Call Schedule & Evening Communication Expectations The PA will sign out to the dayshift junior/intern(Junior’s preference) at 1600. The PA will update the sign out in Cerner each day. This will include any major changes to the care plan, any major problems that occur during the day and any labs/studies or issues that needs to be closely followed overnight. The PA will also be available for signout or concerns from the night team. M-F AM Sign Out: If there are significant events that require extensive communication, to save time in the am the NF intern can email the covering PA (mmerrill@lpch.org, lkjelson@lpch.org). The PA will call or be available to be called before 0615 or after 0645 for verbal sign out. Weekend/Holiday Sign Out: The PA will provide a detailed sign out via email to the junior/intern on medical patients to the weekend team on Friday evening and leave updated sign-out in Cerner system. The covering interns/residents from the weekend will maintain a signout that will be emailed to the PA at the end of the weekend. Last updated 6/10 The weekend covering PA is responsible for both adult and pediatric surgical patients on the weekends and is not available to follow medical patients on the weekend. Weekend Rounds Patients will be divided into two teams for weekend call: General Pediatrics/Cards-Pulm (Blue/Yellow) and RenalRheum/GI (Red/Green). On Saturday, each team will round with two interns or residents and one supervisor. Members of the team who are post-call (varies by call schedule – it may be an intern or supervisor) leave after rounds are completed. The on-call team will always include one team member from a regular daytime weekday team. The supervisor who oversees both teams will be one of the supervisors of the daytime weekday teams (Blue, Yellow, Red, and Green) plus the Resident Reserve who regularly fills in for Continuity Clinic absences. Night Team The Night Team usually consists of two interns and a senior supervising resident. The interns often will cover night call responsibilities of the Ward team they were on in the previous block to maintain continuity. The Night Team arrives at 5 pm for interns and 6 pm for supervisors and receives sign-out from the daytime teams. As time progresses, Night Teams will know the service better. Therefore, sign-out should be relatively quick and concise— focusing on new admissions and new developments for existing patients. On the Wards and Oncology, the Night Team or Night Float will work all day on Sunday and 14-hour shifts Monday until Thursday. On Sundays, it is expected that the Night Team interns will pre-round and write notes on their patients (with the help of the Saturday on-call intern) and then round with the attendings, starting at 8:30. The Night Team should use this Sunday call to better acquaint themselves with the attendings and the patients on their teams. During their weekday calls, the Night Team is only responsible for pre-rounding on and writing notes for the new patients who they admitted during the previous night. At 7:00 each morning (Monday through Friday) supervisors from each team will meet with the Night Team supervisor to sign out new patients and important overnight events. Interns should provide written sign-out to the daytime teams and give verbal sign out to the daytime interns about new admissions and overnight events. As part of our educational curriculum, we hold Evening Report each night at 10 pm in the Housestaff Lounge. These reports, led by overnight pediatric hospitalists, will focus on acute ‘on call’ issues. The sessions will be very flexible and will include bedside teaching, practical skills, and physical exam rounds. Resident Roles and Responsibilities The PL-1 and PL-2 assigned to G-I/Liver Transplant will be responsible for the day-to-day management of all medical patients followed by either the G-I service or the Liver Transplant Service (except those followed in the PICU and except for any liver or liver/small bowel transplant patients followed by the Pediatric Liver Physician’s Assistant). Intern: Primary physician for all medical patients on the G-I or Liver Transplant Service except as stated above. Responsibilities: Write up and dictate history, physical, and treatment plan on all service admissions in consultation with the PL-2 and G-I or Liver Transplant Attending (it is unnecessary to leave the written note in the chart as long as you print out your dictation and place it in the chart prior to leaving the hospital) Write all of the orders on G-I and Liver Transplant medical patients. Arranging for all special diagnostic tests. Maintenance of charts, including daily progress notes, growth charts, and lab results on all patients. In general, progress notes should be written at the earliest after morning rounds, but preferably later in the day when results of laboratory tests, cultures, radiologic studies, etc. are available. If a significant change in the patient’s status, requiring a change in management occurs after the daily progress note is written, an addendum must be written. Keeping parents and patients apprised of progress, lab results, new developments, etc. Discharge summaries must be dictated on all patients within 48 hours of discharge. Face sheets must be completed at the time of discharge. As the primary physician, the intern is responsible for knowing each of his/her patients in detail including past medical history and relevant psychosocial history. Rounds: Last updated 6/10 Interns will be responsible for presenting their patients in detail at Work Rounds in the morning and briefly presenting a review of the status and treatment plan of the intern’s patients to the on-call residents on Evening Sign-Out Rounds. Interns will be expected to have rounded on their inpatients prior to morning work rounds so they will be able to present an up-to-date clinical summary and appropriate latest labwork. Presentation should be succinct: reviewing each patient in appropriate detail by active problems with a presentation of assessment and plan for each problem. New patient admissions will be presented formally and in detail. Additional teaching rounds will be arranged between the Attending, Fellow, and Housestaff. Outpatient Clinic: The inpatient residents are not expected to attend outpatient clinic. The intern on the outpatient portion of the rotation is expected to function according to the outpatient GI selective (see other portion of manual) Supervising Resident: Direct supervision of the PL-1 for all medical inpatients on the G-I or liver transplant service (except as stated before) An admission history and physical is to be dictated on each medical patient on the services above by a resident (If a sub-I dictates a note, a resident is required to write a complete H&P for the chart). Supervising proper maintenance of the patients’ charts on the above services. The PL-2 will lead morning Work Rounds, focusing on all active problems for each patient. The PL-2 will perform G-I consultations as requested by the G-I Attending only if the service is extremely light. PA Roles and Responsibilities In an effort to improve communication between the residents and PAs, the PA will be available to meet with the intern and junior resident at the beginning of their rotation if they have any questions. They can go over the PA role and also orient them to the established order sets for transplant evaluations/readmissions. They can be reached at any time via pager or cellphone (Melanie 799-8591; Lynn 644-7059). If at any time the night float has questions about sign out or concerns about the patients they can call the covering PA-there is someone always available unless in the OR. Primarily, the residents are not responsible for the post transplant patients Monday-Friday 0700-1600. The PA reports to the fellow or attending physician regarding these patients. For the patients on the Liver team that the PA follows, the PA will be allowed the same autonomy as that of a supervisory resident. It is understood that the supervisory residents will play a large role in caring for these children during nights, weekends, and during the day in cases of emergencies; however it is not necessary for supervisory residents to confirm physical exams or labs of these patients prior to rounds. The PA will identify themselves to the nurse taking care of the patient each morning that they are to be the primary contact for any issues. Please defer any questions from the nurses or consulting services (aside from matters that require emergent response) to the responsible PA. FACULTY PRECEPTORS John Kerner, M.D. Manuel Garcia, M.D. Dorsey Bass, M.D. Eric Sibley, M.D. Ken Cox, M.D. William Berquist, M.D. Ricardo Castillo, M.D. Missy Hurwitz, M.D. Clare Wilson, M.D. James Lue, M.D. Brandy Lu, M.D. For the inpatient service, one of the above attendings will be responsible for GI inpatients and all consults; Liver Transplant patients, Small Bowel Transplant patients, or combined Liver-Small Bowel Transplant patients will be covered by a separate attending. There will be 1-2 fellows on inpatient service, depending on the schedule (if there are 2, they will parallel the patient load of each attending). Evaluation and Feedback The methods of evaluation for the Green Team Ward Rotation will consist: Global Rating Scales –MedHub Resident Evaluations, Faculty Evaluations, Rotation Evaluations These evaluation tools will be included in each resident’s portfolio. Last updated 6/10 Resident performance (including knowledge base, diagnostic skills, and ability to formulate a plan of management) is evaluated during the inpatient experience and by a written examination modeled after the ABP certifying examination. Feedback should be provided by the supervisor to intern on a regular basis, but at least weekly. The focus of feedback will be on competency-based goals and objectives. The senior resident should request feedback from the attending on a weekly basis. At the end of the rotation an end-of-rotation feedback session will be conducted by the supervising resident and attending. Each Junior resident will give an oral presentation either on an “AAP Top Ten List” topic or a journal article of particular relevance or a relevant case presentation with discussion. Faculty evaluation of the presentation will be added to the resident’s portfolio. Each resident will keep a journal recording a running list of the diagnoses of all inpatients and outpatients seen so the faculty can help assure there is a broad exposure to Pediatric G-I cases over the course of the rotation. References Each resident will receive a folder including: 1. A CD with current articles on all aspects of pediatric G-I, liver, nutrition, and transplantation. 2. Listing of all faculty and ancillary staff, including phone and pager numbers. 3. A review article on Failure to Thrive and on Parenteral Nutrition. 4. A Pediatric Formula Guide and supplementary information on nutrition assessment.. Last updated 6/10 Competency-based Goals and Objectives Goal 1. Be able to recognize the physical signs of underlying acute or chronic liver disease. Resident Objectives: Describe the clinical findings (signs and symptoms of liver disease) Instructional Strategies Abdominal exams comparing liver and spleen exams with Attending exam Assessment of Competency Medhub Direct observation ACGME Competency Goals MK Appreciate petechiae, jaundice, encephalopathy Describe the laboratory findings in liver disease. Clinical rounds Medhub Direct observation MK Name the 5 main etiologies for liver disease. Clinical rounds Read Chronic Viral Hepatitis, Hochman (Peds in Review Article). Clinical rounds Patient care Read Managing Liver Failure (DA Kelley) Medhub Direct observation MK Medhub Direct observation MK Patient Care NeoReviews 2001: Nutritional Management of Neonatal and Infant Liver Disease Prep 2009 Q#49&97 Patient care Discussions with supervising resident Transplant Slide Show Medhub Direct observation MK Medhub Direct observation MK PC SBP SBP MK Describe the pathophysiology of liver failure and appropriate management strategies for the complications thereof including ascites, coagulopathy and encephalopathy. Explain the unique nutritional needs of patients with liver failure and apply strategies to meet those needs. List indications for transfer to an intensive care setting. Describe the process by which a child gets listed for liver transplant and factors that effect their placement on the list. PA verbal feedback Attend transplant discussion conference Goal 2. Understand the work-up and management for failure to thrive from a gastroenterologist viewpoint. Resident Objectives: Define failure to thrive. Last updated 6/10 Instructional Strategies Review article: Failure to Thrive from a Gastroenterologist Perspective Assessment of Competency Medhub Direct observation ACGME Competency Goals MK Obtain detailed nutritional histories. Define the initial GI work-up for a child with failure to thrive including the screening labs for Celiac Disease, IBD and Cystic Fibrosis. Analyze malabsorption patterns from serum and stool. Explain indications for admission. Brainstorm key insightful questions you may add to the history taking. Reflect on questions Attendings inquire about on History. Article Read Childhood Malabsorption Article (Peds in Review, M. Pietzak) Review Dr. Kerner’s Malabsorption powerpoint Patient care Discussion with Attendings Medhub Direct observation ICS PC Medhub Direct observation MK Medhub Direct observation MK Medhub Direct observation MK SBP PC Goal 3. Know the major causes of chronic diarrhea and the steps in diagnosis and management. Resident Objectives: Define acute versus chronic diarrhea. Instructional Strategies Review MMWR Managing Acute Gastroenteritis. Generate a differential diagnosis for the major causes of chronic diarrhea (Infectious, IBD, Malabsorption). Prep 2009 Q#193 Read AGE in Industrialized Countries Read Inflammatory Bowel Disease (J. Hayms) Sabery article Name the screening labs and studies for the major differential diagnoses. Define the initial pharmacologic management of patients with inflammatory bowel disease. Bass/Mian Assessment of Competency Medhub Direct observation ACGME Competency Goals MK Medhub Direct observation MK MK Medhub Direct observation Medhub Direct observation MK Goal 4. Understand the differences in conjugated and unconjugated hyperbilirubinemia, the corresponding etiologies and management. Resident Objectives: Define conjugated and unconjugated hyperbilirubinemia. Instructional Strategies Review Sahar Rooholamani’s neonatal cholestasis powerpoint. Read Neonatal Cholestasis (Peds in Review, F. Suchy’s) Patient care Last updated 6/10 Assessment of Competency Medhub Direct observation ACGME Competency Goals MK Differentiate breast feeding and breast milk jaundice, onset, and management. Explain the rationale for the expedient work-up of direct hyperbilirubinemia and indications for initiating a work-up. Define the initial work-up of conjugated hyperbilirubinemia incuding the ndications for and interpretation of results of lab tests, ultrasound, HIDA scan, and biopsy. Define steps to optimize nutritional management in patients with hyperbilirubinemia. Review Sahar Rooholamani’s neonatal cholestasis presentation. Read Guidelines for Infantile Cholestasis (J Ped Gastro) Medhub Direct observation MK Berquist case Review Sahar Rooholamani’s presentation. Medhub Direct observation MK PC Review Sahar Rooholamani’s presentation. Medhub Direct observation MK Medhub Direct observation MK PC Patient care Goal 5. Learn the approach to diagnosis and management of acute GI Bleeds. Resident Objectives: Define upper versus lower GI bleed and explain how to differentiate these. Generate a differential diagnosis by age for acute GI bleed. Specify at least three major etiologies and explain how to differentiate among the conditions. Instructional Strategies Patient care Observe gastric lavage on patient Read Lower GI Bleeding in Children. (Pediatric Emergency Care, A. Leung) Assessment of Competency Medhub Direct observation ACGME Competency Goals MK PC Medhub Direct observation MK Medhub Direct observation MK PC Read Gastroesophageal Variceal Hemorrhage (Medical Progress, Sharara) Patient care Prep 2009 Q#29 Specify the management of an acute GI Bleed. Take into account IV access, indicated laboratory studies and frequency of repeat labs, dietary status, assessment of resources, vital sign monitoring and medications (see below). Last updated 6/10 Patient care List indications for Protonix and Octreotide in the setting of acute GI bleed. Read Octreotide Therapy for Acute GI Bleed (J Pedatr Gastro) Medhub Direct observation MK Goal 6. Understand basic nutritional requirements by age. Recognize the varying nutritional needs of patients with chronic illness and gastrointestinal pathology and recommend appropriate dietary modifications. Resident Objectives: Initiate optimal TPN for neonate. Instructional Strategies Review NICU guide on parenteral nutrition. Review TPN orders with supervising Initiate optimal TPN for child. Review Drs. Hurwitz and Kerner’s TPN chapter. Medhub Direct observation MK PC Describe the recommended monitoring while advancing TPN. Explain the considerations in advancement of dextrose, amino acids, and intralipids Describe the complications of long term parenteral nutrition and strategies to prevent these complications. Review LINKS TPN pathway Nutritional Support Team discussion Medhub Direct observation MK PC Review Drs. Hurwitz and Kerner’s TPN chapter. Patient care Prep 2009 Q#17 Attend nutritional support team meeting Medhub Direct observation MK PC Medhub Direct observation SBP Utilize the multidisciplinary nutritional resources available to LPCH patients including nutritionist, nutritional support team and pharmacist. State the caloric requirements by age. Define allergic colitis and describe your management approach to including formula choice. Name a standard infant and pediatric formula. Recognize the major components and differences in infant Last updated 6/10 Nutritional support team Patient care Check calories provided in patients on TPN and observe child’s growth pattern. Prep 2009 Q#1&94 Review Dr. Kerner’s Pediatric Formula Guide Article on Allergic colitis? Patient care Read Enteral Nutrition Article (Serrano) Assessment of Competency resident/Attending ACGME Competency Goals MK PC Medhub Direct observation MK Medhub Direct observation MK Medhub Direct observation MK versus pediatric formulas including calorie and osmotic load differences. Describe the basic composition of specialized pediatric formulas, Viovenex and Peptamen. Explain how to address the unique nutritional challenges in patients with short bowel syndrome. Describe the importance of the length of bowel and functional anatomy in design of nutritional strategy and prognosis. Review Dr. Kerner’s Pediatric Formula Guide Review Dr. Kerner’s Pediatric Formula Guide Patient care PBLI = practice based learning and improvement ICS = interpersonal and communication skills P= professionalism MK= medical knowledge PC= patient care SBP = systems based practice Last updated 6/10 Medhub Direct observation MK Medhub Direct observation MK PC